You are working in a community emergency department in proximity to a destination ski resort. You have treated the following patients, all of whom need to fly home tomorrow:
an 8-year-old with otitis media (OM),
a 22-year-old snowboarder with an ankle fracture, which has been reduced and casted,
a 65-year-old with a mild chronic obstructive pulmonary disease (COPD) exacerbation—oxygen saturation of 93% on room air,
a 52-year-old with angina,
a 45-year-old with menorrhagia and symptomatic anemia, and
an 18-year-old with a rib fracture and a small traumatic pneumothorax.
Which of these patients are fit for air travel?
The commercial aircraft cabin, which is pressurized to approximately 8000 ft above sea level, is a physiologically different environment compared with the ground. The cabin at that altitude is hypoxic relative to the ground atmosphere because of the decreased PO2. Also, at this decreased pressure, gaseous volumes increase, according to Boyle’s law, in which volume is inversely proportional to pressure. It is these 2 variables that account for a large proportion of illnesses that occur or worsen in flight. Knowledge of how altitude physiology can worsen illnesses can allow you to predict which of your patients are not fit for air travel.
Air travel prognosis
The 8-year-old with OM
The gas within the middle ear expands when the aircraft cabin climbs to altitude and automatically vents via the eustachian tube. At altitude the space within the middle ear is in equilibrium with the decreased atmospheric pressure. As the plane descends and atmospheric pressure increases, the middle ear equalizes by air ascending via the eustachian tube. If there is edema or blockage of the eustachian tube, such as with an upper respiratory tract infection (URTI) or OM, the passenger will be unable to equalize the pressure in the middle ear. With landing, the gaseous bubble within the middle ear will continue to decrease in size as the atmospheric pressure increases, essentially creating a vacuum effect and pulling at the tissues of the middle ear. The tympanic membrane (TM), the most malleable of these tissues, will be pulled inward, causing pain. With enough pressure difference, the TM might rupture.1 For this reason, it is advised that passengers with URTI or OM do not fly.
If the passenger chooses to fly, however, there are certain maneuvers to aid in equalizing the pressures across an edematous eustachian tube. One hour before descent, an oral anti-inflammatory can be taken to decrease swelling in the area. Also, an oral decongestant, such as pseudoephedrine, (in children 12 years or older) can aid in decreasing inflammation of the oro-pharynx. Topical nasal decongestants might also be of some benefit. Finally, the passenger can try techniques to aid in increasing the patency of the eustachian tube, such as yawning, swallowing, or performing a Valsalva maneuver.2 Children can be encouraged to blow into a small straw or balloon, as this action has a Valsalva effect. Infants can be fed during descent to promote stretching and straightening of the eustachian tube.
Patients with URTI or OM should be medically exempt from air travel. They should be informed of the likelihood of pain in the ear with landing and of the potential complication of a perforated TM. Those who insist on flying should be advised of the various ways to increase eustachian tube patency.
The 22-year-old snowboarder with an ankle fracture, which has been reduced and casted
A fracture that is casted is at risk of compartment syndrome due to the swelling associated with the injury and the confined space of the cast. The usual risk of swelling is increased in travelers with extremity fractures that cannot be kept elevated in the aircraft. Furthermore, the hypoxic environment causes venodilation, leading to increased venous pooling and increasing the risk of swelling and compartment syndrome. Finally, in certain passengers for whom the seat edge presses directly against the popliteal fossa, there can be compression of the popliteal vein, leading to even further pooling of blood in the leg. For this reason, any cast (lower or upper extremity) applied for a fracture that is less than 48 hours old must be bivalved before flight.3 A safe alternative would be to splint the injury in a 3-sided splint.
The 65-year-old with a mild COPD exacerbation; oxygen saturation of 93% on room air
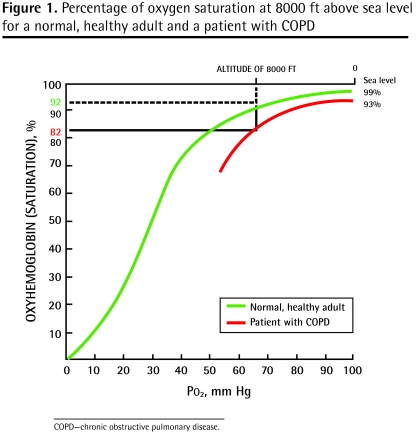
Patients with COPD often have lower baseline oxygen saturation, particularly during an exacerbation of their disease. Even those who are asymptomatic with a baseline saturation of 93% will encounter difficulties in flight. Breathing air at 8000 ft (ie, the cabin pressure in flight) is equivalent to breathing 15% oxygen at sea level.4 This hypoxic aircraft environment will cause a decrease in your patient’s PaO2 (Figure 1). A normal, healthy adult will desaturate to approximately 92% to 93% in flight. This COPD patient will desaturate to approximately 82% in flight and is likely to experience symptoms of hypoxia.
Figure 1.
Percentage of oxygen saturation at 8000 ft above sea level for a normal, healthy adult and a patient with COPD
Patients who have low baseline oxygen saturation should have supplemental oxygen in flight. This can be arranged through the airline. (The airline usually requires at least 48 hours’ notice.) Given that airlines can usually only provide oxygen up to 4 L/min by nasal prong, patients requiring oxygen at 4 L/min on the ground who do not achieve a saturation better than 95% are not fit to fly by commercial aircraft.
A patient is allowed to bring his or her own portable oxygen concentrator (7 brands are approved by Transport Canada) as long as it is not adjusted to its maximum level on the ground. The patient must bring a sufficient number of fully charged batteries for the duration of the flight as well as any unanticipated delays, as the portable oxygen concentrator cannot be plugged into the seat electrical outlet.5
The 52-year-old with angina
Angina at sea level is brought on by reduced oxygen delivery to myocardial tissue. The hypoxic cabin environment means a further reduction in oxygen delivery. Those who are able to perform usual activities without angina (New York Heart Association classes I and II) are considered generally safe to fly. Those who experience angina with minimal exertion or at rest might become symptomatic with the reduced cabin oxygen. These patients should travel with supplemental oxygen.
Air travel for a patient with New York Heart Association class IV angina is recommended only if it is medically necessary and if the patient is accompanied by a physician (eg, traveler returning home).
It should be noted that if there is evidence of myocardial ischemia (eg, electrocardiogram changes or positive cardiac marker results), elective travel should be delayed by at least 6 weeks.6
The 45-year-old with menorrhagia and asymptomatic anemia
A passenger with anemia (ie, hemoglobin less than 85 to 90 g/L, depending on the airline) cannot fly without supplemental oxygen. Despite normal ground-level saturation (ie, each molecule of hemoglobin is fully saturated with oxygen), the total oxygen-carrying capacity is decreased. When combined with the hypoxia of altitude, the total oxygen delivery to end organs will be decreased and might result in symptoms such as chest pain, shortness of breath, and light-headedness.
This patient will need a transfusion so that her hemoglobin levels are greater than 90 g/L, or you will have to request supplemental oxygen in flight from the airline’s medical desk.1
The 18-year-old with a rib fracture and a small traumatic pneumothorax
A pneumothorax is a contraindication to flight.1 As the cabin pressure decreases with ascent, the volume of extrapleural gas will increase. This expanded gas bubble can further compress the lung, and there is potential for the pneumothorax to evolve into a tension pneumothorax.
Patients are required to wait 2 weeks after the resolution of the pneumothorax before flying. A chest radiograph should be completed to document the resolution.
Conclusion
These examples highlight common medical conditions that might seem stable when assessed in the emergency department but that can become problematic in the aircraft environment. Many airlines have medical forms available on their websites to assist you in identifying potentially problematic medical conditions. You might be asked to complete this form in order to medically clear your patient for air travel. Any uncertainty about prognosis for air travel should be cleared with the airline’s medical department. Most major airlines have physicians on duty to assist you in making decisions regarding fitness for air travel.
Interested in assessing patients’ fitness for air travel or in the management of in-fight emergencies? We invite you to participate in Onboard Medical Emergencies, a course offered by the McGill University Health Centre Continuing Education Office at the Air Canada Training Centre in Montreal, Que, on December 9, 2009. For more information, please visit www.OnboardME.com.
Certain illnesses or injuries, including certain chronic conditions, might make a person unfit for air travel. Knowledge of certain absolute and relative contraindications to air travel can make the travel experience safer for your patient and reduce in-flight emergencies.
Emergency Files is a quarterly series in Canadian Family Physician coordinated by the members of the Emergency Medicine Committee of the College of Family Physicians of Canada. The series explores common situations experienced by family physicians doing emergency medicine as part of their primary care practice. Please send any ideas for future articles to Dr Robert Primavesi, Emergency Files Coordinator, at robert.primavesi@muhc.mcgill.ca.
Further reading and resources
For physicians
Aerospace Medical Association, Medical Guidelines Task Force. Medical guidelines for airline travel. 2nd ed. Aviat Space Environ Med 2003;74(5 Suppl):A1–19. Available from: www.asma.org/pdf/publications/medguid.pdf
Ross D, Essebag V, Sestier F, Soder C, Thibeault C, Tyrrell M, et al. Assessment of the cardiac patient for fitness to fly: flying subgroup executive summary. Can J Cardiol 2004;20(13):1321–3.
Transport Canada [website]. Hypoxia and hyperventilation. Ottawa, ON: Transport Canada; 2008. Available from: www.tc.gc.ca/CivilAviation/cam/tp13312-2/section2/hypoxia.htm
For patients
Air Canada [website]. Health tips. Dorval, QC: Air Canada; 2009. Available from: www.aircanada.com/en/travelinfo/onboard/healthtips.html
British Airways [website]. Medical information. Harmondsworth, UK: British Airways; 2009. Available from: www.britishairways.com/travel/healthmedinfo/public/en_gb
World Health Organization [website]. International travel and health. Geneva, Switz: World Health Organization; 2005. Available from:http://whqlibdoc.who.int/publications/2005/9241580364_chap2.pdf
Aerospace Medical Association. Medical guidelines for airline passengers. Alexandria, VA: Aerospace Medical Association; 2002. Available from: http://www.asma.org/publications/paxguidelines.doc
BOTTOM LINE
Environmental and physiological changes that occur during a flight might cause an exacerbation of a passenger’s underlying medical condition.
Hypobaric hypoxia in the reduced cabin pressure at altitude will lead to a decrease in oxygen saturation, affecting patients with existing respiratory and cardiac conditions and those with anemia.
Gas expansion on ascent and reduction during descent (according to Boyle’s law) will cause problems in body cavities where there is air trapping (ie, barotitis, barosinusitis, tension pneumothorax, bowel obstruction).
Physicians who are uncertain about a patient’s fitness for air travel should contact the medical desk of the patient’s airline.
POINTS SAILLANTS
Les changements environnementaux et physiologiques qui se produisent en vol peuvent causer une exacerbation des problèmes médicaux sous-jacents d’un passager.
L’hypoxie hypobare due à la pression réduite en altitude dans la cabine entraînera une baisse de la saturation en oxygène pouvant affecter des patients ayant des problèmes respiratoires et cardiaques existants, ainsi que ceux qui font de l’anémie.
L’expansion des gaz lors du décollage et leur réduction durant l’atterrissage (selon la loi de Boyle) causeront des problèmes dans les cavités corporelles où l’air est captif (p. ex. barotite, barosinusite, pneumothorax sous tension, obstruction intestinale).
Les médecins qui ont des incertitudes quant à l’aptitude d’un patient à voyager par avion devraient communiquer avec le bureau médical de la compagnie d’aviation du patient.
Footnotes
Competing interests
Drs Carvalho and Poirier are Co-Directors of the Onboard Medical Emergencies course.
References
- 1.Aerospace Medical Association, Medical Guidelines Task Force. Medical guidelines for airline travel. Aviat Space Environ Med. (2nd ed) 2003;74(5 Suppl):A1–19. [PubMed] [Google Scholar]
- 2.Cummin ARC, Nicholson AN. Aviation medicine and the airline passenger. New York, NY: Oxford University Press; 2002. pp. 132–5. [Google Scholar]
- 3.Martin T. Aeromedical transportation. 2nd ed. Surrey, UK: Ashgate; 2006. p. 166. [Google Scholar]
- 4.British Thoracic Society Standards of Care Committee. Managing passengers with respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2002;57(4):289–304. doi: 10.1136/thorax.57.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Transport Canada [website] Carriage of portable oxygen concentrators for passenger use on board aircraft. Ottawa, ON: Transport Canada; 2007. [Accessed 2009 Aug 21]. Available from: www.tc.gc.ca/civilaviation/imsdoc/acs/700/700-002.htm. [Google Scholar]
- 6.Ross D, Essebag V, Sestier F, Soder C, Thibeault C, Tyrrell M, et al. Assessment of the cardiac patient for fitness to fly: flying subgroup executive summary. Can J Cardiol. 2004;20(13):1321–3. [PubMed] [Google Scholar]