Abstract
Background
Standard recommendations for skin care for patients with atopic dermatitis stress the importance of skin hydration and the application of moisturizers. However, there is little objective data to guide recommendations regarding the optimal practice methods of bathing and emollient application.
Objective
This study quantified cutaneous hydration status after various combination bathing and/or moisturizing regimens.
Methods
Four bathing/moisturizer regimens were evaluated in ten subjects, five pediatric subjects with atopic dermatitis and five subjects with healthy skin. The regimens consisted of bathing alone without emollient application, bathing and immediate emollient application, bathing and delayed application, and emollient application alone. Each regimen was evaluated in all subjects, utilizing a cross-over design. Skin hydration was assessed with standard capacitance measurements.
Results
In atopic dermatitis subjects, emollient alone yielded a significantly (p<0.05) greater mean hydration over 90 min (206.2% baseline hydration) than bathing with immediate emollient (141.6%), bathing and delayed emollient (141%), and bathing alone (91.4%). The combination bathing and emollient application regimens demonstrated hydration values at 90 minutes not significantly greater than baseline. Atopic dermatitis subjects had a decreased mean hydration benefit compared to normal skin subjects.
Conclusions
Bathing without moisturizer may compromise skin hydration. Bathing followed by moisturizer application provides modest hydration benefits, though less than that of simply applying moisturizer alone.
Introduction
Historically, there have been tremendous variations in “expert recommendations” for optimal bathing practices in atopic dermatitis (AD) management. In 1872, Hebra1 recommended frequent bathing three to four times daily, as an intervention for eczema. In 1964, Scholtz2,3 advanced the concept that bathing may negatively impact individuals with AD. His “Scholtz regimen” advocated bathing avoidance and the application of a lipid-free lotion at least once a day per patient preferences4,5.
AD guidelines have not provided consistent recommendations regarding optimal bathing and emollient application frequencies. A consensus conference on pediatric AD6 recommended daily bathing with immediate application of topical medications followed by emollient, and Canadian guidelines7 emphasized bathing at least once daily and also recommended immediate application of moisturizer. An international consensus conference8 recommended applying emollient at least twice daily but did not discuss bathing. The National Institute9 for Health and Clinical Excellence recommended “emollients frequently and in large quantities, particularly after bathing or washing” but did not provide a bathing recommendation. American Academy of Dermatology guidelines10 did not address bathing although “emollients are a standard of care, steroid-sparing, and useful for both prevention and maintenance therapy.”
The concept of “soak and smear” has been discussed by Gutman et al11, advocating daily bathing followed by immediate smearing of a topical steroid ointment during intensive therapy and an emollient during maintenance. Both Gutman’s recommendation of daily bathing and Scholtz’s prohibition of bathing have been reported to be highly effective by each respective author. Notably, neither study utilized controls and the subjects were new patients to both providers, raising the question of whether the improvement was due to the assumption of care by a new skilled dermatology provider or the bathing intervention itself.
There have been several studies addressing objective measurement of interventions to the skin. Most notably, Grove12 demonstrated that subjects with normal skin maintained an increase in skin hydration up to 12 hours post-emollient application. Voegeli13 reported that washing the skin decreased hydration. However, previous research has not quantitatively analyzed the effect of bathing and subsequent emollient usage on skin hydration or studied the effect on AD subjects. This study attempts to provide objective evidence of the hydration effect of such regimens, to supplement published clinical experience and to guide recommendations regarding optimal bathing and emollient application strategies.
Materials and methods
Study subjects
Ten volunteer subjects (6 females and 4 males) participated. Five pediatric subjects had history and physical findings consistent with mild to moderate AD6(range: 11–16 yrs). Five subjects had history and physical examination findings of healthy skin(range: 8–30 yrs). The measurements were performed between April June in an air conditioned room (23.2±1.6°C, relative humidity 42±2.4). Bath temperature was 33.9±1.2°C. None of the subjects bathed, applied moisturizer, or applied medication for at least three hours before measurements were taken.
The study protocol was approved by both the University of California San Diego and Rady Children’s Hospital San Diego Institutional Review Boards. Adult subjects provided informed consent. Pediatric subjects and their parent provided informed assent and consent, respectively.
Instrument
The Nova Dermal Phase Meter (DPM) 9003 (Nova, Gloucester, MA) obtains impedance based capacitance readings by integrating measurements from varying frequencies of alternating current. The screen displays hydration values in arbitrary Nova units, directly related to the capacitance14. It was set on measurement mode dl0, giving instantaneous readings as the probe made contact with the skin. Mean coefficient of variation is ~20%15.
All measurements were repeated with a Scalar MY-707S Moisture Checker (Scalar Corp., Tokyo, Japan) which measures superficial skin conductance16.
Test Procedure
This was a crossover study. Over two visits, patients received four treatment regimens (Table 1), one randomly17 selected regimen to each arm on each day. Subjects were measured with a minimum of one day between visits.
Table 1.
Description of the four treatment regimens
| Treatment Regimen | Description |
|---|---|
| A | 10 min bath. No moisturizer |
| B | 10 min bath. Immediate moisturizer application |
| C | 10 min bath. Delayed (30 min post-bathing) moisturizer application |
| D | No bath (10 min wait period). Immediate moisturizer application |
Three of the regimens involved bathing of an arm for 10 minutes, followed by dab drying with towels, and then immediate moisturizer application, delayed application of moisturizer 30 min later, or no emollient application. The fourth treatment regimen consisted of a 10 min period of no intervention (“no bathing”) followed by immediate moisturization.
The observation time period for each treatment regimen was 120 min after intervention with bathing or non-bathing. Bathing was accomplished by placing an entire arm in a large basin, filled with tap water to approximately 5 cm above the elbow crease. No bath products were used. A commercial emollient was utilized (Cetaphil™ cream), applied with nitrile gloves, from the hand to 5 cm above the elbow crease. Guidelines for stratum corneum hydration measurement18 were followed with subjects resting for 20 min before baseline measurements were taken on the upper third of the volar forearm.
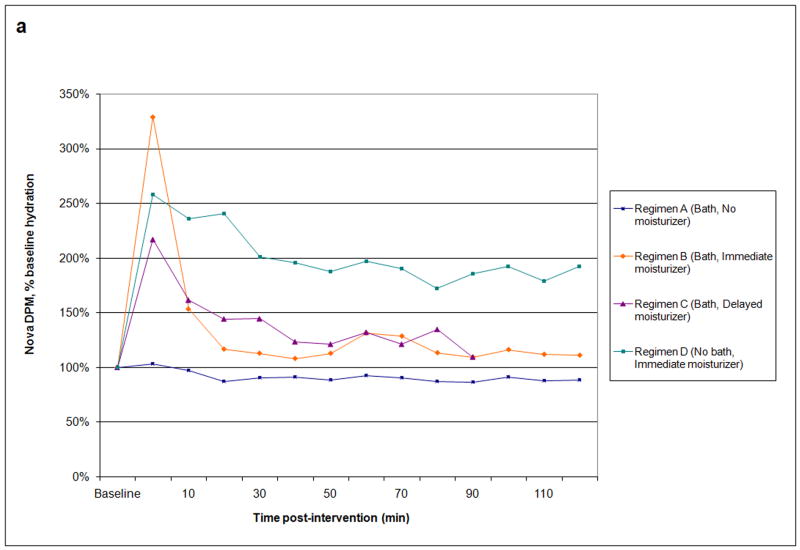
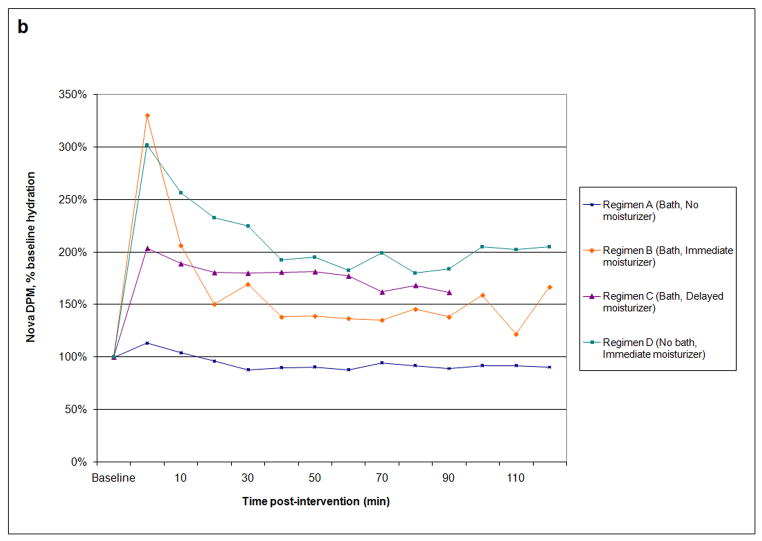
The time was limited by practical considerations of efficient utilization of study facilities and patient patience, with subjects remaining sitting in the room during the entire study period. This gave post-intervention results lasting 120 min for three of the four regimens. However, the bathing and delayed moisturizer regimen only had 90 min of post-intervention data due to the fact that moisturization was not performed until 30 min post-bathing. Thus, while the complete data set is presented in Fig. 1, data analysis was only performed for the 90 min post-intervention time period for which all regimens contained data.
Results
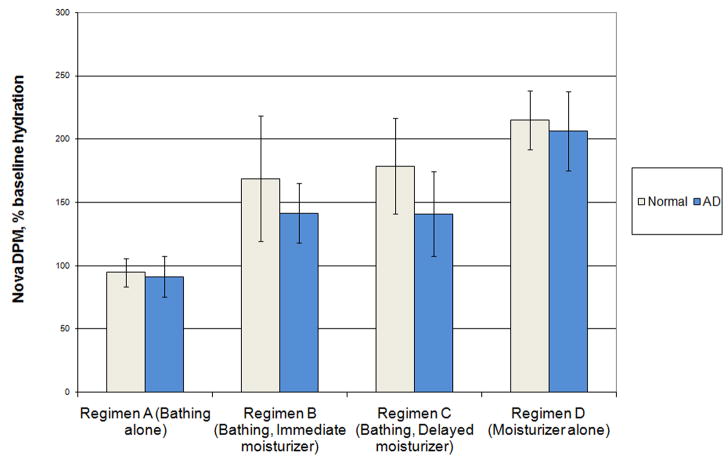
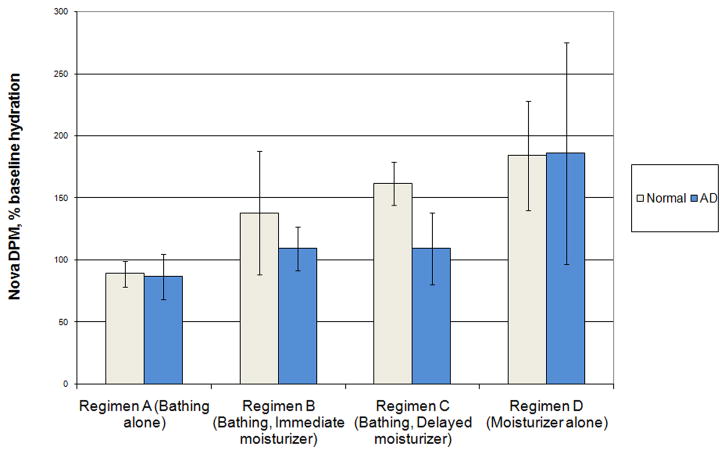
Outcome measures are presented in Table 2. Percent baseline hydration vs. time is graphed for AD subjects (Fig. 1a) and normal skin subjects (Fig. 1b). Bar graphs compare the treatment regimens by mean hydration over 90 min (Fig. 2) and final hydration at 90 min (Fig. 3).
Table 2.
Nova DPM, % baseline hydration. SD in parentheses. 95% CI in brackets.
| AD | Normal skin | |||
|---|---|---|---|---|
| Mean hydration | Final hydration @ 90 min | Mean hydration | Final hydration @ 90 min | |
| Regimen A (Bathing alone) | 91.4% (13.0) [75.2–107.6] | 86.6% (14.9) [68.1–105.1] | 94.6% (9.0) [83.4–105.8] | 89% (8.5) [78.5–99.5] |
| Regimen B (Bathing, Immediate moisturizer) | 141.6% (18.9) [118.1–165.1] | 109.4% (14.2) [91.7–127.1] | 168.8% (39.9) [119.3–218.3] | 138% (40.1) [88.3–187.7] |
| Regimen C (Bathing, Delayed moisturizer) | 141% (26.8) [107.7–174.3] | 109.2% (23.3) [80.2–138.2] | 178.6% (30.5) [140.7–216.5] | 161.6% (13.9) [144.3–178.9] |
| Regimen D (Moisturizer alone) | 206.2% (25.1) [175.1–237.3] | 186.0% (72.2) [96.4–275.6] | 215% (18.7) [191.8–238.2] | 184.2% (35.6) [140 228.4] |
In AD subjects, bathing without moisturization resulted in decreased hydration content, measured as capacitance, throughout the observation period, with a final hydration value 87% of baseline (Fig. 3). All regimens utilizing moisturizer, either immediately after bathing, 30 minutes after bathing, or applied to dry skin, increased hydration at all time points (Fig. 1a) Emollient application without bathing yielded a significantly greater (p<0.05) mean hydration (206%) and peak hydration (329%) compared to all other regimens. In addition, the last hydration value at 90 min (186%) (Fig 3) was significantly greater (p<0.05) than bathing without emollient application, though not significantly different from the two combination bathing and moisturizing regimens, utilizing paired t-tests.
The application of moisturizer immediately after bathing, as compared to delayed application 30 minutes later, showed no statistical differences in mean or last hydration values.
The mean hydration and last hydration values for the AD subjects differed significantly from the normal group’s values (p<0.05; data not shown).
Results using the Scalar conductive device were consistent with the Nova DPM 9003.
Discussion
This study showed that distinct bathing and moisturizing regimens influence skin hydration status, and that the effects are dynamic through the 90 minute observation period. Bathing without the application of moisturizer was shown to decrease skin hydration below baseline levels, as previously reported13. In atopic subjects, bathing followed by emollient application increased hydration status, initially to a high level, though with decreased effect over time such that 90 minutes post-application the end point hydration was not significantly greater than baseline. Emollient application alone provided the greatest average hydration benefit for patients with AD.
This study indicated no statistical difference in mean hydration status between immediate and delayed moisturization regimens despite guidelines6,7 recommending immediate moisturizer application post-bathing. There was a short term hydration peak at 5 min after immediate moisturizing that was not present with delayed moisturizing. However, measurement of the hydration peak may have been confounded by ionic compounds within water or emollient possibly remaining on the skin surface as the Nova DPM 9003 utilizes impedance based capacitance. This was minimized by pat drying after both bathing and emollient application, before measurements were made. In addition, Grove12 demonstrated that emollients do not retain conductivity after drying for one hour.
Individuals with AD had compromised cutaneous hydration compared to normal individuals when their skin was treated in similar ways. Examining the combination bathing and moisturizing regimens, AD subjects had decreased mean hydration benefits as compared to subjects with normal skin (Fig. 2). Even more striking, AD subjects did not retain moisture as well as individuals with normal skin, and by the end of the 90 min study had a smaller hydration benefit from bathing and moisturization (Fig. 3). Recent studies showing fillagrin mutations as a cause of ichthyosis vulgaris and risk factor for AD raise the question if genotypic differences may impact the response to different treatment regimens.
This study has limitations that may restrict how its conclusions impact recommendations on optimal bathing practices in individuals with AD, including a small sample size. Future studies might forego the comparison of non-atopic subjects, as it is the atopic group that most requires guidance from medical professionals. The instrument utilized to measure cutaneous hydration was the Nova DPM which measures impedance based capacitance, with results repeated with the Scalar Moisture Checker which measures conductance. Other measures of stratum corneum function such as transepidermal water loss may yield further insight. This study only measured skin hydration and was not designed to analyze bathing and/or emollient clinical benefits beyond hydration status. This study utilized only a single emollient cream. Emollients that contain stratum corneum lipids such as ceramide19 and/or other components may yield even greater skin hydration. Bathing may have cutaneous effects beyond hydration, such as decreasing cutaneous antigens and microbes that may contribute to inflammation and pruritus. In addition, it may impact the penetration of anti-inflammatory medications.
This study attempts to bring an evidence-basis to decision making on skin care regimens for individuals with AD. The study showed clear benefits of emollient application on skin hydration, either after bathing, or without bathing. Bathing followed by emollient application does not decrease skin hydration, in contrast to bathing without emollient application. Guidelines stressing emollients immediately after bathing, while reasonable for convenience and ease of structuring skin care regimens, do not appear to significantly improve skin hydration over delayed application of moisturizer. Recommendations to apply emollients frequently, including application at times other than after bathing seem appropriate.
It would be useful to study the effects of bathing and/or emollient usage over a longer time period, assessing longer post-intervention time-points, and the effects of different emollients or bath/moisturizer regimens. Utilizing objective and subjective scoring of AD severity to measure the impact of these skin care regimens in combination with standardized prescription regimens would be useful.
Acknowledgments
Special thanks to Ann Funk, RN for her help and enthusiasm.
Supported in part by a grant from the GCRC Program, M01 RROO827, National Center for Research Resources, National Institutes of Health.
References
- 1.Hebra F. Traite des maladies de la peau. Paris: Masson; 1872. pp. 567–72. [Google Scholar]
- 2.Scholtz J. Management of atopic dermatitis. A preliminary report. Calif Med. 1964;100(2):103–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Scholtz J. Management of atopic dermatitis. Calif Med. 1965;102(3):210–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Ayres S, Mihan R. Atopic dermatitis Success or failure with the Scholtz regimen. The Australas J Dermatol. 1967;9(1):16–22. doi: 10.1111/j.1440-0960.1967.tb01146.x. [DOI] [PubMed] [Google Scholar]
- 5.Tompkins R. Scholtz regimen. Arch Dermatol. 1978;114:1099. [PubMed] [Google Scholar]
- 6.Eichenfield LF, Hanifin JM, Luger TA, et al. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol. 2003;49(6):1088–95. doi: 10.1016/s0190-9622(03)02539-8. [DOI] [PubMed] [Google Scholar]
- 7.Lynde C, Barber K, Claveau J, et al. Canadian Practical Guide for the Treatment and Management of Atopic Dermatitis. [Accessed May 19, 2008];J Cutan Med Surg. doi: 10.1007/s10227-005-8080-3. Available at http://www.springerlink.com/content/r5432000056r2748/ [DOI] [PubMed]
- 8.Ellis C, Luger T, Abeck D, et al. International consensus conference on atopic dermatitis II (ICCAD II): clinical update and current treatment strategies. Br J Dermatol. 2003;148(Supp 63):3–10. doi: 10.1046/j.1365-2133.148.s63.1.x. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence. Atopic eczema in children: management of atopic eczema in children from birth up to the age of 12 years. National Institute for Health and Clinical Excellence; [Accessed May 19, 2008]. Available at: www.nice.org.uk/CG057. [Google Scholar]
- 10.Hanifin J, Cooper K, Ho V, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (AAD)/American Academy of Dermatology Association “Administrative Regulations for Evidence-Based Clinical Practice Guidelines”. J Am Acad Dermatol. 2004;50(3):391–404. doi: 10.1016/j.jaad.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Gutman A, Kligman A, Sciacca A, et al. Soak and Smear. A Standard Technique Revisited. Arch Dermatol. 2005;141:1556–9. doi: 10.1001/archderm.141.12.1556. [DOI] [PubMed] [Google Scholar]
- 12.Grove G. The effect of moisturizers on skin surface hydration as measured in vivo by electrical conductivity. Curr Ther Res. 1991;50(5):712–9. [Google Scholar]
- 13.Voegeli D. The effect of washing and drying practices on skin barrier function. J Wound Ostomy Continence Nurs. 2008;35(1):84–90. doi: 10.1097/01.WON.0000308623.68582.d7. [DOI] [PubMed] [Google Scholar]
- 14.Distante F, Beradesca E. Hydration. In: Berardesca E, Elsner P, Wilhelm K, Maibach H, editors. Bioengineering of the Skin: Methods and Instrumentation. New York: CRC Press; 1995. pp. 8–9. [Google Scholar]
- 15.Clarys P, Barel A, Gabard B. Non-invasive electrical measurements for the evaluation of the hydration state of the skin: comparison between three conventional instruments - the Corneometer, the Skicon, and the Nova DPM. Skin Research and Technology. 1999;5:14–20. [Google Scholar]
- 16.Asano-Kato N, Fukagawa K, Tsubota K, et al. Quantitative evaluation of atopic blepharitis by scoring of eyelid conditions and measuring the water content of the skin and evaporation from the eyelid surface. Cornea. 2001;20:255–259. doi: 10.1097/00003226-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Armer P, Bower E, Bernice B, et al. A Million Random Digits with 100,000 Normal Deviates. Glencoe: The Rand Corporation; 1955. [Google Scholar]
- 18.Berardesca E. EEMCO guidance for the assessment of stratum corneum hydration: electrical methods. Skin Research and Technology. 1997;3:126–132. doi: 10.1111/j.1600-0846.1997.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 19.Chamlin SL, Kao J, Frieden IJ, et al. Ceramide-dominant barrier repair lipids alleviate childhood atopic dermatitis: Changes in barrier function provide a sensitive indicator of disease activity. J Am Acad Dermatol. 2002;47:198–207. doi: 10.1067/mjd.2002.124617. [DOI] [PubMed] [Google Scholar]