Abstract
Background:
The anatomical and morphological differences and high-flexion daily activities in the Asian population have since ever prompted for development of customized knee replacement systems. INDUS knee system has advantages both of high-flex designs and is developed by keeping the anatomical variations of the native population in mind. The purpose of this study is to analyze the 2-year follow-up results using the INDUS prosthesis.
Materials and Methods:
Two hundred and ninety-seven knees in 276 patients were prospectively analyzed. There were 65 men (72 knees) and 211 (225 knees) women with a mean age of 64.56 years. Two hundred and forty-five knees had primary osteoarthritis, 48 knees had rheumatoid arthritis, and four knees had post-traumatic arthritis. Clinical parameters, including the Knee Society scores (knee score and function score), range of motion, post-operative anterior knee pain, and complications were recorded. Pre- and post-operative serial radiographs were analyzed for limb alignment, component positioning, and evidence of loosening.
Results:
The patients were followed-up for an average of 2.59 years (range, 2–3.3 years). The mean knee score and the mean function score were significantly improved from a pre-operative value of 39.4 points and 46.7 points to a post-operative value of 87 points and 86 points, respectively (P value <0.05). Two hundred and thirty four knees had no anterior knee pain while 63 knees had mild to moderate pain, but none of the patients requested any intervention for the same. Of the 276 patients (297 knees), 79 knees had flexion above 140°, 167 had a flexion range of 130–140°, 27 had a flexion range of 100–130°, and 24 knees had a flexion < 100°, with the mean range of movement being 132.9°. Improvements in the range of movement were retained over time and a total of 205 patients (224 knees, 75.7%) could squat or sit cross-legged at the final follow-up. The mean tibiofemoral angle was 8.5°±6.9° of varus pre-operatively and 5.4°±2.2° of valgus (3–7° of valgus) at the final follow-up, with no loss of alignment noted in any case. One knee underwent revision for late infection while another knee had periprosthetic supracondylar fracture treated with plate fixation.
Conclusions:
Use of the INDUS knee prosthesis has a favorable short-term outcome, with a mean range of 135° flexion and excellent knee scores.
Keywords: Backside wear, high flexion, INDUS knee
INTRODUCTION
Total joint replacement is the technologically advanced solution for arthritic pain. However, a search for a better functional and durable prosthesis still continues. The original total condylar design was very successful in terms of pain relief and durability, but the average post-operative flexion achieved was only around 90–95°.1–7 Even though this may be enough for most of the daily activities in the western world,8 Asians, and particularly Indians, require a higher flexion for most of their daily social habits and customs.9 In 1978, the posterior stabilized condylar prosthesis was introduced, as a modification of the total condylar prosthesis, by Insall et al.10 In this prosthesis, a post and cam mechanism was used to achieve femoral rollback. The average flexion achieved by this prosthesis was 107–115°.10–14 Similarly, cruciate retaining designs achieve a flexion of around 110–112°.15,16 Although this was a significant improvement, it was not enough for daily habits like cross-legged sitting and squatting that are so common in the Indian subcontinent. In recent times, a number of additional design modifications have been introduced to achieve this goal.17,18 This increase in flexion however brings with it the fear of loosening and excessive wear.19 Moreover, most modern knee designs are modular, which results in backside wear.20 Current design trends are focusing on shortening the radii of curvature; such shortening, in turn, thickens the posterior femoral condyle and increases the height of the posterior-stabilized box, both of which require removal of more bone. The end results may be excessive wear, increased patellofemoral complications, and difficult revisions.
The INDUS prosthesis is designed so as to keep the thickness of the posterior condyle equivalent to the thickness of the distal condyle. Also, the cam and post have been placed in such a way that the removal of the box in the center is much less; hence, patellofemoral complications are much lower.
The purpose of this study is to analyze the 2 year follow-up results using the INDUS prosthesis. This prosthesis has been in use at six centers since August 2005.
MATERIALS AND METHODS
This study was approved by the institutional ethical committee of the hospital. The implant design was approved and funded by Division of Science and Technology (DST). Three hundred and seventy-eight primary total knee arthroplasties in 343 patients using the INDUS knee prosthesis were prospectively enrolled in this study that was conducted at six centers. The surgeries were performed from August 2005 to October 2006. Three patients died (four knees) in the first year of surgery due to unrelated causes. Seventeen patients were lost to follow-up (23 knees). For the purpose of reporting the short-term results, we excluded 47 patients with less than 2 years of follow-up (54 knees). Thus, a total of 297 knees (276 patients) were available for review. A demographic detail of patients from different centers is shown in Table 1. There were 65 men (72 knees) and 211 (225 knees) women. The mean age was 64.56 years (49–91). Two hundred and fifty-five patients underwent unilateral total knee replacement (TKR) and 21 patients underwent bilateral TKR at an average interval of 2.4 months (range, 1–3 months). The diagnosis was primary osteoarthritis in 245 knees (82.49%, 14 bilateral), rheumatoid arthritis in 48 knees (16.16%, seven bilateral), and post-traumatic arthritis in four (1.34%) knees. The patients were followed-up for an average of 2.59 years (range, 2–3.3 years).
Table 1.
Demographic details from different centers
| Variables | No. of patients | Mean age (years) | Male/female (no of knees) | Mean BMI | Mean follow-up (years) |
|---|---|---|---|---|---|
| Center 1 | 166 (178 knees) | 64.7 | 27/139 | 28.5 | 3.16 |
| Center 2 | 25 (31 knees) | 61.32 | 4/21 | 27.4 | 2.65 |
| Center 3 | 19 (19 knees) | 66.26 | 6/13 | 26.3 | 2.58 |
| Center 4 | 32 (34 knees) | 66.5 | 13/19 | 23.9 | 2.56 |
| Center 5 | 23 (24 knees) | 62.74 | 11/12 | 27.6 | 2.56 |
| Center 6 | 11 (11 knees) | 64.91 | 4/7 | 24.1 | 2.5 |
| Total | 276 (297 knees) | 64.56 | 72/225 | 26.3 | 2.66 |
The mean body mass index from all the centers was 26.5.
The implant
The ethnic anatomical and cultural variations in the Indian population have prompted the need for development of the INDUS Knee.21 It is a posterior cruciate substituting design where femoral rollback occurs by a post and cam mechanism [Figure 1]. The radius of curvature of the posterior condyle of the femoral component (J curve) has been reduced, thereby increasing the posterior condylar offset. The total thickness remains the same. The original offset is reproduced. This helps in gaining more femoral rollback and more flexion. A 4° slope is incorporated in the tibial insert and a 3° slope in the metal base plate to aid in increase of flexion22 [Figure 2]. The above two design modifications allow maximal flexion at the knee. The deep flexion achieved prompted certain novel modifications in the post and cam mechanism to offer stability and to allow for rotational freedom in deep flexion. A third joint was designed between the post and the cam, with the post engaging the cam at around 80° of flexion and thereafter acting like a load bearing surface in deep flexion. The articulating surface of the post is convex and that of the cam is concave thus allowing a more congruent surface for allowing load transfer and the rotation to occur [Figure 3] as the post does not impinge on the side walls of the box during rotations. This rotational freedom is necessary to prevent wear of the post and hence loosening and osteolysis of the tibial component.23 Also, as the bar of the cam articulates with the post at a lower level, the jumping distance is increased to 16 mm, another feature to assist in enhanced stability. The posterior edges of the tibial polyethylene insert are chamfered to avoid impingement in deep knee flexion. There is an anterior cutout in the tibial polyethylene insert to accommodate the patellar tendon during deep flexion [Figure 4]. The tibia is monoblock and hence backside wear is reduced to a minimum.20 The tibial polyethylene insert has a deep dish design to prevent point loading and polywear [Figure 4]. Introduction of the post and cam mechanism involves removal of extra bone from the intercondylar region of the femur to accommodate the box. This results in bone loss.10,13,24 In the INDUS design, the femoral box is designed so as to cut minimal bone. Thus, INDUS knee also incorporates the bone sparing principle. A thorough anatomic study of the Indian knee joints was done before designing the components. The components are made in sizes that are more suited to the Indian population. The various sizes were designed in accordance with the suggestions of Vaidhya et al.21 and by analyses of 100 computerized tomography scans in 50 patients (independent unpublished data) The femoral components are separate for the right and left, with an anatomic deep trochlear design for better patellar tracking and avoiding the patellar clunk syndrome.25,26 The intercondylar box of the femoral component is kept open to enable nailing in case of periprosthetic fractures. The patella is a single peg anatomic design [Figure 5]. In conclusion, the INDUS knee is designed to be a high-flexion, bone sparing and anatomic design suitable for the native population. The prosthesis is Gamma irradiated in vacuum to increase the longevity of the polyethylene.27
Figure 1.

INDUS a posterior stabilized design to increase femoral rollback
Figure 2.
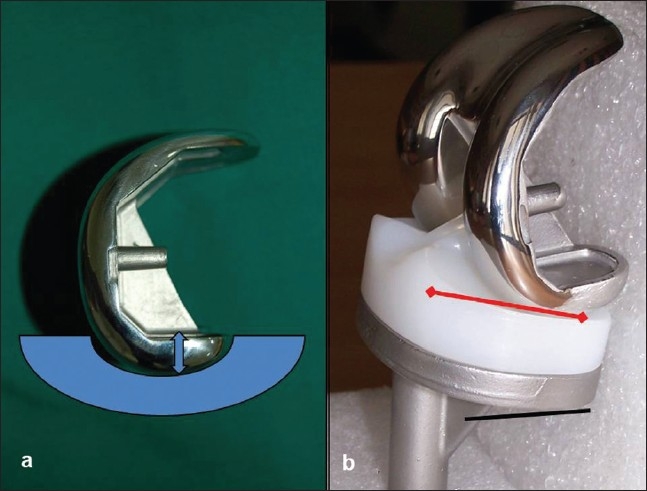
INDUS Hiflex features. (a) An improved J curve (thicker posterior condyle) increases the posterior offset. (b) The tibial component having total slope of 70 with 40 in the base plate (black line) and 30 in the insert (red arrow)
Figure 3.
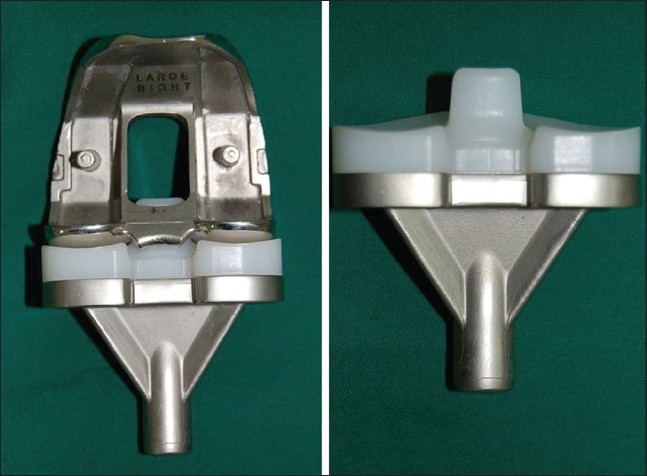
The post and cam conform mediolaterally to form a third joint allowing enhanced rotational congruency
Figure 4.

Monoblock tibial component with deep dish design and anterior cut out in insert (arrow) to accommodate the patellar tendon during deep knee flexion
Figure 5.
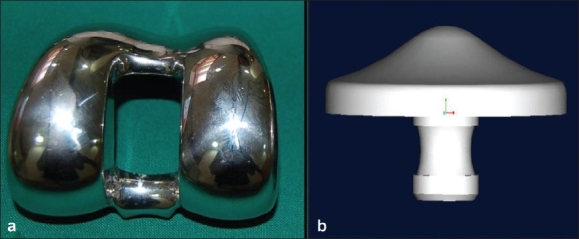
(a) Anatomical trochlear design with open intercondylar box. (b) single peg anatomical patella
Operative procedure
Before the operation, full-length weight-bearing radiographs were obtained showing the hip, knee, and ankle joints. The angles of the femoral and tibial cuts and the desired position of the femoral entry hole were planned before surgery. An anterior midline incision measuring 12–14 cm was followed by a medial parapatellar arthrotomy. All the components were cemented after pulsed lavage and drying of the cut bone ends and pressurization of the cement. Patelloplasty rather than patellar resurfacing was performed in 111 knees when the articular cartilage was found to be healthy, erosion was <20% and when patellar tracking was good especially in younger patients. It consisted of a peripatellar synovectomy, electrocautery of the patellar rim to provide partial denervation, and removal of osteophytes. The remaining patellae were resurfaced. All patients received prophylactic antibiotics. Prophylactic antibiotics were given one night before and 45 min before surgery. Intravenous antibiotics were continued for 3 days after surgery. They wore compression stockings for 2 weeks. A drain was used for 24 h. Active quadriceps-strengthening exercises and range of motion were commenced immediately post-operatively and continuous passive motion (CPM) machine was not used. Weight-bearing was allowed from the second post-operative day. Knee flexion was allowed as guided by the pain tolerance of the patient.
The patients were reviewed at 6 weeks, 3 months, 6 months, 1 year, and annually thereafter. Clinical parameters, including the Knee Society scores (KSS),28 range of motion, post-operative clinical anterior knee pain and complications were recorded. The KSS was evaluated in two parts: first, the knee score involving the clinical knee findings, and, second, the function score analyzes functional mobility of the patient. In addition, patients were asked to squat or sit cross-legged at follow-up. Pre-operative factors affecting the post-operative range of movement were also analyzed, including flexion contracture, deformity, and range of movement. No subjective parameter was recorded.
Pre- and post-operative weight bearing radiographs included anteroposterior, lateral, and full-length anteroposterior scanogram films and a skyline patellar view. These were assessed for limb alignment, component positioning, and the presence and location of radiolucent lines at the bonecement interface.
Statistical comparisons of the pre-operative and post-operative clinical scores (categorical variable) were made with the use of chi-square analysis. Correlations between the pre-operative and post-operative ranges of flexion (continuous variable) were investigated with the paired t-test. The level of statistically significant difference was set at P = 0.05.
RESULTS
The patients were followed-up for an average of 2.59 years (2–3.3 years). A change in values of different variables from all the six centers is shown in Table 2. Pre-operatively, the mean knee score was 39.4 ± 11.4 points and the mean function score was 46.7 ± 17.4 points. Both scores showed significant improvement at final follow-up [Table 3]. At the last follow-up, the clinical anterior knee pain scores were grade 0 (no pain) in 234 knees (78.79%), grade 1 (mild pain) in 35 knees (11.78%), and grade 2 (moderate pain) in 28 knees (9.43%); none were grade 3 (severe pain). None of the patients requested a revision because of anterior knee pain. A total of 205 patients (224 knees, 75.7%) could squat or sit cross-legged at the final follow-up. Pre-operatively, the mean flexion contracture was 10.3° (range, 0–30°), the mean maximum flexion was 114.83° (60–140°), and the mean range of movement was 106.2° (45–150°). At the last follow-up, the mean flexion contracture was 3.19° (0–10°), the mean maximal flexion angle was 136.14° (90–160°), and the mean range of movement was 132.10° (85–160°). These outcomes represent a statistically significant improvement [Table 3]. Of the 276 patients (297 knees), 79 (26.6%) knees had flexion above 140°, 167 (56.23%) had a flexion range of 130–140°, 27 (9.09%) had a flexion range of 100–130° and 24 (8.08%) knees had flexion <100°. Improvements in the range of movement were retained over time [Figure 6]. No clunks or crepitus were heard.
Table 2.
Pre- and post-operative data of all the centers
| Variables | Flexion deformity (degrees) | Range of motion (degrees) | Total knee score | Total functional score | ||||
|---|---|---|---|---|---|---|---|---|
| Variables | ||||||||
| Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | |
| Center 1 | 11.01 | 3.37 | 102.67 | 133 | 38.39 | 93.9 | 43.89 | 91.43 |
| Center 2 | 10.48 | 2.58 | 101.13 | 134.84 | 39.77 | 93.16 | 46.61 | 87.45 |
| Center 3 | 8.95 | 1.84 | 107.89 | 133.42 | 38.79 | 84.68 | 47.74 | 84.47 |
| Centre 4 | 12.06 | 3.09 | 103.82 | 133.24 | 40.5 | 84.71 | 49.65 | 84.41 |
| Center 5 | 11.88 | 4.17 | 108.54 | 131.25 | 38.25 | 85.25 | 49.04 | 84.79 |
| Center 6 | 10 | 4.09 | 113.64 | 127.27 | 41.18 | 83.82 | 43.55 | 83.73 |
| Total | 10.73 | 3.19 | 106.28 | 132.17 | 39.48 | 87.58 | 46.74 | 86.04 |
Table 3.
Comparison of pre-operative and post-operative clinical variables
| Variable | Pre-operative (mean ± SD) | Post-operative (mean ± SD) | P value |
|---|---|---|---|
| Knee score* | 39.4 ± 11.4 | 87.5 ± 7.16 | <0.05 |
| Function score* | 46.7 ± 17.4 | 86 ± 9.30 | <0.05 |
| Flexion deformity# | 10.7° | 3.19° | 0.041 |
| Terminal flexion# | 117.9° | 135.4° | 0.028 |
| Range of motion# | 106.2° | 132.1° | 0.034 |
P values are for chi-square test,
P values are for paired t-test
Figure 6.

Lateral radiograph of the knee of three year follow up of INDUS knee showing maintaining optimal flexion
A complete set of radiographs of 285 knees out of 297 were available for analysis at final follow-up [Figures 7 and 8].
Figure 7.

Clinical pre-operative photograph (a) of a 62 yrs old patient with severe genuvarum with OA. Clinical photograph (b) of same patient 30 months follow-up shows good deformity correction. Pre-operative scanogram (c) and post-operative scanogram (d) of the same patient shows good correction
Figure 8.

Pre-operative radiographs antero-posterior view (a) and lateral view (b) of the knee of 71 years old patient shows severe OA with genu varum. Post-operative lateral radiograph (c) show range of flexion achieved and clinical photographs (d) shows the range of flexion at 28 months follow-up
The mean tibiofemoral angle was 8.5° ± 6.9° of varus (32° of varus to 18° of valgus) pre-operatively and 5.4° ± 2.2° of valgus (3°–7° of valgus) at final follow-up. No change in alignment was observed at any post-operative radiological examination. Radiolucent lines were observed in 58 knees. All were seen below the tibial base plate beginning at around 1 year of follow-up and were non-progressive. There was no evidence of loosening of the tibial component. There were no cases of femoral radiolucency.
One knee underwent a two-stage revision because of late infection with Staphylococcus aureus, which was identified 7 months after surgery. In another knee, a peri-prosthetic supracondylar fracture of the femur occurred 17 months after operation, and this was treated successfully with open reduction and plate fixation. The femoral component remained well fixed.
DISCUSSION
Achieving maximal knee flexion improves the patient satisfaction and knee performance. However, conventional knee arthroplasty before high-flex designs rarely allows for knee flexion beyond 120°.29,30 The newer high-flexion knee replacement prostheses have reported a higher flexion achieved post-operatively, within a range of 130–135° of flexion.31,34 The INDUS knee is an indigineously researched and designed knee prosthesis that achieves a mean flexion of 135° without compromising on stability and polyethylene wear and with minimal bone resection.
Component sizing and proper placement of the components is key to the success of knee arthroplasty.35,36 Component oversizing in the anteroposterior dimension alters the delicate balance in flexion extension gap, resulting in flexion tightness post-operatively because of increased tension in the quadriceps mechanism36 whereas oversizing in the mediolateral dimension affects the patellar tracking and wound closure.37 The risk of component oversizing with the other available implants is especially present in Indians and other Asian subpopulations that are known to have a smaller build and stature as compared with the western population.21,38,39 INDUS knee is based on careful assessment of anthropometric data from the Indian patients thus reducing the risk of oversizing.
A number of modifications have been made in the post and cam mechanism of the INDUS knee to enhance flexion and increase stability in deep flexion. Han et al.40 reported a high incidence of loosening of the femoral component in a retrospective series of 72 knees using the Legacy posterior stabilized–flex total knee replacement. At a mean follow-up of 32 months, aseptic loosening of the femoral component was found in 27 (38%) cases, with 15 (21%) requiring revision at a mean of 23 months. They concluded that the high rate of loosening was associated with weight bearing at maximum flexion and inadequate support of the posterior condyle of the prosthesis. However, in the INDUS knee, the modified post and cam functions as a load-bearing third joint and lend support to the posterior condyles during deep flexion. Our follow-up is short, but we still have had no cases of mechanical loosening of either of the components.
Lack of rotational freedom of the post in the femoral box has been cited as a reason for causing polywear and osteolysis.23 In INDUS, the post does not impinge on the side walls of the box during rotations hence addressing this issue.
Most modern implants are modular. However, with modularity comes the problem of backside wear, which often occurs in amounts enough to cause osteolysis and loosening.20 To avoid these problems, a monoblock design was preferred for the INDUS knee.
Introduction of the post and cam mechanism involves removal of extra bone from the intercondylar region of the femur to accommodate the box. This results in bone loss.10,13,24 In the INDUS design, modifications in the post and cam mechanism allow for less bone removal thus preserving bone stock.
For conventional implants, the range of movement following TKRs is reported to be approximately 110°10–16 and few patients can flex beyond 120°.41–43 The excellent range of movement observed in this study is consistent with the kinematic advantages of high-flexion implants demonstrated in several biomechanical studies.17,18,31–34
The introduction of high-flexion prosthesis has raised concerns that the increased flexion which enables patients to squat or sit cross-legged may compromise the long-term results.19 There is also concern regarding loosening of the implant caused by design modifications requiring removal of more bone from the posterior femoral condyles and the intercondylar area.19,44 However, our study shows favorable results, with mean values of 135° flexion and excellent total and function KSS. No revisions for aseptic loosening were required. There were no incidents of instability or dislocation in the deep flexion. No patient requested revision because of anterior knee pain on deep flexion.
The limitations of this study include a limited number of patients with a short follow-up. However, the prospective nature of our study allows us to follow these patients and we should be able to identify and correct any problems seen with our new design. We have more than 95% follow-up and we will report on medium and longer term results as they become available.
In the present series, total knee arthroplasty with the INDUS knee prosthesis resulted in an excellent range of motion and good functional outcome, and the durability of the prosthesis is promising.
Acknowledgments
We would like to acknowledge Dr. Sancheti Parag K, Dr. Shyam Ashok, Dr. Dhariwal Qaed, Dr. Patil Surendra for their contribution in analyzing the data and preparation of the manuscript.
We the authors have received financial assistance from Department of Science and Technology, Govt. of India.
Footnotes
Source of Support: Science and Technology, Govt. of India
Conflict of Interest: None.
REFERENCES
- 1.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 2.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis: A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173–80. [PubMed] [Google Scholar]
- 3.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–65. [PubMed] [Google Scholar]
- 4.Insall J, Ranawat CS, Scott WN, Walker P. Total condylar knee replacement: Preliminary report 1976. Clin Orthop Relat Res. 2001;388:3–6. doi: 10.1097/00003086-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty: Pros and cons based on five- to ten-year follow-up observations. Clin Orthop Relat Res. 1986;205:93–9. [PubMed] [Google Scholar]
- 6.Ranawat CS, Boachie-Adjei O. Survivorship analysis and results of total condylar knee arthroplasty: Eight- to 11-year follow-up period. Clin Orthop Relat Res. 1988;226:6–13. [PubMed] [Google Scholar]
- 7.Ranawat CS, Rose HA. Clinical and radiographic results of total-condylar knee arthroplasty: A 3- to 8-year follow-up. In: Ranawat CS, editor. In Total- Condylar Knee Arthroplasty: Techniques, Results, and Complications. New York: Springer; 1985. pp. 140–8. [Google Scholar]
- 8.Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture. 2000;12:143–55. doi: 10.1016/s0966-6362(00)00060-6. [DOI] [PubMed] [Google Scholar]
- 9.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: Range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–8. doi: 10.1097/00004356-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: A modification of the total condylar design: Two to four-year clinical experience. J Bone Joint Surg Am. 1982;64:1317–23. [PubMed] [Google Scholar]
- 11.Maloney WJ, Schurman DJ. The effects of implant design on range of motion after total knee arthroplasty: Total condylar versus posterior stabilized total condylar designs. Clin Orthop Relat Res. 1992;278:147–52. [PubMed] [Google Scholar]
- 12.Ranawat CS, Luessenhop CP, Rodriguez JA. The press-fit condylar modular total knee system: Four-to-six-year results with a posterior-cruciate-substituting design. J Bone Joint Surg Am. 1997;79:342–8. doi: 10.2106/00004623-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Scott WN, Rubinstein M, Scuderi GJ. Results after knee replacement with a posterior cruciate-substituting prosthesis. J Bone Joint Surg Am. 1988;70:1163–73. [PubMed] [Google Scholar]
- 14.Stern SH, Insall JN. Posterior stabilized prosthesis: Results after follow-up of nine to twelve years. J Bone Joint Surg Am. 1992;74:980–6. [PubMed] [Google Scholar]
- 15.Martin SD, McManus JL, Scott RD, Thornhill TS. Press-fit condylar total knee arthroplasty: 5- to 9-year follow-up evaluation. J Arthroplasty. 1997;12:603–14. doi: 10.1016/s0883-5403(97)90132-7. [DOI] [PubMed] [Google Scholar]
- 16.Ritter MA, Campbell E, Faris PM, Keating EM. Long-term survival analysis of the posterior cruciate condylar total knee arthroplasty: A 10-year evaluation. J Arthroplasty. 1989;4:293–6. doi: 10.1016/s0883-5403(89)80029-4. [DOI] [PubMed] [Google Scholar]
- 17.Argenson JN, Komistek RD, Mahfouz M, Walker SA, Aubaniac JM, Dennis DA. A high flexion total knee arthroplasty design replicates healthy knee motion. Clin Orthop Relat Res. 2004;428:174–9. doi: 10.1097/01.blo.0000148948.79128.76. [DOI] [PubMed] [Google Scholar]
- 18.Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, et al. Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: An in vitro robotic experimental investigation. J Bone Joint Surg Am. 2004;86:1721–9. doi: 10.2106/00004623-200408000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Ranawat CS. Design may be counterproductive for optimizing flexion after TKR. Clin Orthop Relat Res. 2003;416:174–6. doi: 10.1097/01.blo.0000093028.56370.46. [DOI] [PubMed] [Google Scholar]
- 20.Conditt MA, Thompson MT, Usrey MM, Ismaily SK, Noble PC. Backside wear of polyethylene tibial inserts: Mechanism and magnitude of material loss. J Bone Joint Surg Am. 2005;87:326–31. doi: 10.2106/JBJS.C.01308. [DOI] [PubMed] [Google Scholar]
- 21.Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000;15:79–85. doi: 10.1016/s0883-5403(00)91285-3. [DOI] [PubMed] [Google Scholar]
- 22.Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H. The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:193–6. doi: 10.1007/s00167-004-0557-x. [DOI] [PubMed] [Google Scholar]
- 23.Mikulak SA, Mahoney OM, dela Rosa MA, Schmalzried TP. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am. 2001;83:398–403. doi: 10.2106/00004623-200103000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Vince KG. Principles of condylar knee arthroplasty: Issues evolving. Instr Course Lect. 1993;42:315–24. [PubMed] [Google Scholar]
- 25.Beight JL, Yao B, Hozack WJ, Hearn SL, Booth RE., Jr The patellar “clunk” syndrome after posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1994;299:139–42. [PubMed] [Google Scholar]
- 26.Hozack WJ, Rothman RH, Booth RE, Jr, Balderston RA. The patellar clunk syndrome: A complication of posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1989;241:203–8. [PubMed] [Google Scholar]
- 27.Collier MB, Engh CA, Jr, McAuley JP, Ginn SD, Engh GA. Osteolysis after total knee arthroplasty: Influence of tibial baseplate surface finish and sterilization of polyethylene insert: Findings at five to ten years postoperatively. J Bone Joint Surg Am. 2005;87:2702–8. doi: 10.2106/JBJS.E.00074. [DOI] [PubMed] [Google Scholar]
- 28.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–4. [PubMed] [Google Scholar]
- 29.Ranawat AS, Rossi R, Loreti I, Rasquinha VJ, Rodriguez JA, Ranawat CS. Comparison of the PFC Sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: Short-term results. J Arthroplasty. 2004;19:35–9. doi: 10.1016/j.arth.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Ranawat CS, Flynn WF, Jr, Deshmukh RG. Impact of modern technique on long-term results of total condylar knee arthroplasty. Clin Orthop Relat Res. 1994;309:131–5. [PubMed] [Google Scholar]
- 31.Gandhi R, Tso P, Davey JR, Mahomed NN. High-flexion implants in primary total knee arthroplasty: A meta-analysis. Knee. 2009;16:14–7. doi: 10.1016/j.knee.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 32.Kim YH, Choi Y, Kwon OR, Kim JS. Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses: A prospective, randomized study. J Bone Joint Surg Am. 2009;91:753–60. doi: 10.2106/JBJS.H.00805. [DOI] [PubMed] [Google Scholar]
- 33.Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS. The PFC Sigma RP-F TKA designed for improved performance: A matched-pair study. Orthopedics. 2006;29:S49–52. [PubMed] [Google Scholar]
- 34.Bin SI, Nam TS. Early results of high-flex total knee arthroplasty: Comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–5. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 35.Goldberg VM, Figgie HE, 3rd, Figgie MP. Technical consideration in total knee surgery: Management of patellar problems. Orthop Clin North Am. 1989;20:189. [PubMed] [Google Scholar]
- 36.Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty: Pros and cons based on five- to ten-year follow-up observations. Clin Orthop Relat Res. 1986;205:93–9. [PubMed] [Google Scholar]
- 37.Krackow KA. The technique of total knee arthroplasty. St Louis: CV Mosby; 1990. [Google Scholar]
- 38.Hoaglund FT, Low WD. Anatomy of the femoral neck and head, with comparative data from Caucasians and Hong Kong Chinese. Clin Orthop Relat Res. 1980;152:10–6. [PubMed] [Google Scholar]
- 39.Saikia KC, Bhuyan SK, Rongphar R. Anthropometric study of the hip joint in Northeastern region population with computed tomography scan. Indian J Orthop. 2008;42:260–6. doi: 10.4103/0019-5413.39572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89:1457–61. doi: 10.1302/0301-620X.89B11.19840. [DOI] [PubMed] [Google Scholar]
- 41.Anouchi YS, McShane M, Kelly F, Jr, Elting J, Stiehl J. Range of motion in total knee replacement. Clin Orthop Relat Res. 1996;331:87–92. doi: 10.1097/00003086-199610000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty: Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–3. doi: 10.1302/0301-620x.84b1.12432. [DOI] [PubMed] [Google Scholar]
- 43.Dennis DA, Komistek RD, Colwell CE, Jr, Ranawat CS, Scott RD, Thornhill TS, et al. In vivo anteroposterior femorotibial translation of total knee arthroplasty: A multicenter analysis. Clin Orthop Relat Res. 1998;356:47–57. doi: 10.1097/00003086-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 44.Ritter MA. High-flexion knee designs: More hype than hope? In the affirmative. J Arthroplasty. 2006;21:40–1. doi: 10.1016/j.arth.2006.02.088. [DOI] [PubMed] [Google Scholar]


