Abstract
In the mnemonic model of PTSD, the current memory of a negative event, not the event itself determines symptoms. The model is an alternative to the current event-based etiology of PTSD represented in the DSM. The model accounts for important and reliable findings that are often inconsistent with the current diagnostic view and that have been neglected by theoretical accounts of the disorder, including the following observations. The diagnosis needs objective information about the trauma and peritraumatic emotions, but uses retrospective memory reports that can have substantial biases. Negative events and emotions that do not satisfy the current diagnostic criteria for a trauma can be followed by symptoms that would otherwise qualify for PTSD. Predisposing factors that affect the current memory have large effects on symptoms. The inability-to-recall-an-important-aspect-of-the-trauma symptom does not correlate with other symptoms. Loss or enhancement of the trauma memory affects PTSD symptoms in predictable ways. Special mechanisms that apply only to traumatic memories are not needed, increasing parsimony and the knowledge that can be applied to understanding PTSD.
Keywords: autobiographical memory, gender, neuroticism, dissociative amnesia, trauma
This paper is a about posttraumatic stress disorder (PTSD) and more specifically about its assumed etiology. We evaluate basic theoretical assumptions underlying the PTSD diagnosis and present an alternative model. By its current diagnostic criteria in the U.S.A., which we refer to as the DSM, (i.e., the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, American Psychiatric Association, 2000) and by the World Health Organization (2006), the diagnosis of PTSD requires the occurrence of a traumatic event. However, in practice, the diagnosis does not involve measuring the occurrence of an actual event, only the patient’s report of the event at least one month, and sometimes years, after the event occurred. The memory report, in practice, is not questioned (McNally, 2003b). We examine the implications of a diagnosis based on a pathogenic memory rather than a pathogenic event. The change has major consequences: the event, which is not measured during diagnosis, treatment, and research, is removed from its etiological status and is replaced by the memory of the event, which is measured. One can then ask what kinds of memories are associated with PTSD, what events and emotions are present in them, and what individual difference measures describe the people that produce these kinds of memories. Table 1 summarizes the six key diagnostic criteria for PTSD, which we will refer to throughout this work.
Table 1.
Requirements for PTSD.
|
Note: source: American Psychiatric Association (2000, pp. 467–468)
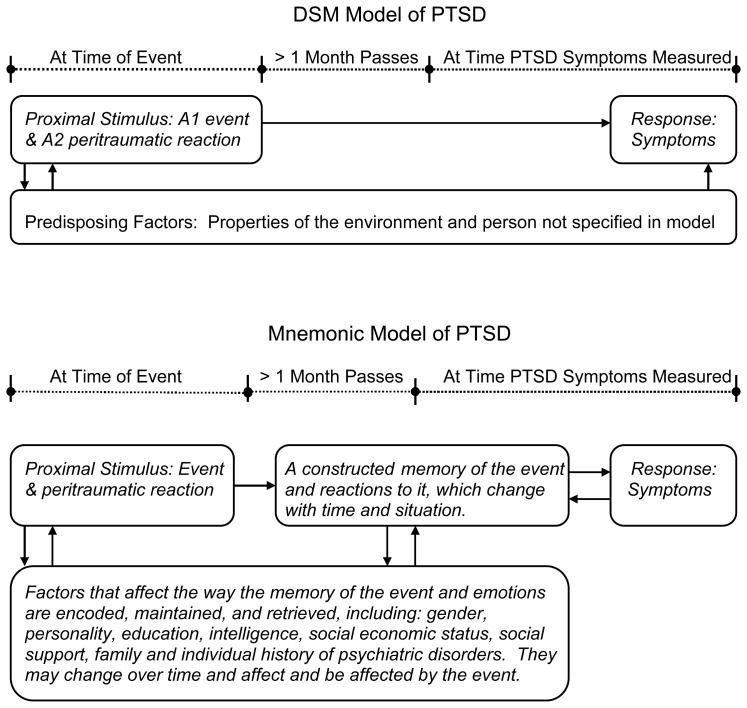
The Mnemonic Model
Although the current DSM is not intended to provide a model of the etiology of the diagnostic categories, there is a causal model inherent in the DSM diagnostic criteria of PTSD. It is a stimulus – response model. As shown in the top of Figure 1, there is an A1 event and an A2 immediate reaction to the event. The proximal stimulus, that is, the event and the immediate reaction, cause the later B, C, and D symptom response. By design, the DSM acknowledges, but is not specific about, predisposing conditions. According to the diagnosis and the model shown in the top of Figure 1, PTSD is a psychiatric diagnosis that depends on a special kind of external event and immediate, almost reflexive, reactions to it, making it different from all other diagnoses, with the possible exception of addictions, in that it relies on known external events.
Figure 1.
Contrasting models of PTSD.
The mnemonic model is shown at the bottom of Figure 1. It adds one component to the model at the top of the figure: a memory. A negative event occurs to a person. This produces changes in the person, which we describe through the concept of memory. The memory is not fixed, but changes over time due to factors that characterize all memories in all people, factors related to individual differences among people, factors related to extremely stressful events, and factors related to the current goals and concerns of the person. There is no partial or complete, indelible memory of the initial encoding that can be recovered. There is only a selective, current memory that is produced differently at different times and that can be changed. The interaction between the characteristics of the event and the processes of remembering determines whether PTSD will follow; the symptoms derive from the memory, not from the event per se. Thus, our general theoretical understanding of memory and emotion can be used to predict the nature of the traumatic memory and how it generates PTSD symptoms. The event has an effect that can be studied. Our point simply is that this effect is mediated by memory. The mnemonic model is not an attack on the reality of PTSD as a clinical disorder. There are many insightful critiques that reformulate the symptoms of PTSD in ways other than a psychopathology (e.g., Summerfield, 1999; 2001; Young, 1995), but our model is not one of them.
Our mnemonic model offers a new framework for the understanding of PTSD and is a basic change from the way theories of PTSD have been formulated. As Dalgleish (2004, p. 253) notes, “in clinician/clinical researcher stakeholder terms a theory of PTSD should offer an account of the symptoms of the disorder and their treatment.” Whereas, “the basic science/pure theorist stakeholder has an altogether different set of expectations of a theory.… Pure theorists are more motivated to broaden theoretical horizons from disorder-specific, microtheoretical approaches (such as those that focus only on PTSD) to… models that embrace various psychopathological and nonpsychopathological presentations.… Ideally, the theories should offer up unique, tightly prescribed, and falsifiable empirical predictions. For the pure theorist/basic scientist, then, the limitations inherent in current theories of PTSD are frustrating.” Two issues are critical here. First, existing theories of PTSD ‘offer an account of the symptoms of the disorder’ that is an account of PTSD as described in the current diagnosis, whereas we are challenging aspects of the diagnosis. Second, the existing theories of PTSD are ‘microtheoretical approaches’ formulated to account for just PTSD, whereas our starting assumption is one of no special mechanisms for PTSD, just normal memory functioning in extreme situations. Because of these differences, our model cannot be directly compared to clinical theories of PTSD operating at a more detailed level of analysis, even though many of them involve memory (e.g., Foa & Rothbaum, 1998; Foa, Zinbarg, & Olasov-Rothbaum, 1992; Brewin, Dalgleish, & Joseph, 1996; Ehlers & Clark, 2000; Mineka & Zinbarg, 1996, 2006; for authoritative reviews see Brewin & Holmes, 2003 and Dalgleish, 2004). Because of our broader scope, details are not known and we term our attempt a model rather than a formal detailed theory as is common for the clinical theories of PTSD.
According to the mnemonic model, PTSD is developed and maintained though the explicit memory of a particular event (or series of events). We focus on explicit memory (i.e., conscious voluntary and involuntary recall) because the evidence suggests that it plays a central role and because this focus provides an easily testable model. This position does not preclude implicit memory processes from contributing to some of the symptoms of PTSD. Thus, increasing the availability of the memory of the stressful event by making it more self-defining will increase PTSD symptoms; decreasing the availability of the memory through pharmacological interventions, neuropsychological damage, or other means will decrease symptoms. Moreover, memory, including memory for traumatic events, is constructive; memory reports cannot give pure, unbiased access to the event at encoding. The constructive nature of memory is in the service of the current attitudes, goals, and concerns of the individual, and is affected by standard individual differences measures such as gender, intelligence, dissociation, neuroticism and other aspects of personality, and applies as strongly to the remembering of subjective states, such as emotions, as to the remembering of more objectively observable information.
Given these claims, it remains an empirical question as to the types of events that can lead to a memory associated with B, C, and D symptoms (see Table 1) in a particular individual and to the particular negative emotions that will be part of the memory. To examine the logic of the A criteria, we accept the B, C, and D symptoms (except for a suggested modification of one aspect of the C symptoms offered later); that is, consistent with the literature, we assume that many people show the cluster of B, C, and D symptoms. However, we question that events with A1 and A2 characteristics are the only events followed by this complex of symptoms. If memory, rather than a specific type of event and specific emotional reactions to it, is the mechanism leading to PTSD, it becomes unacceptable to operate with a priori categories of events and a priori emotional reactions to them, as in the DSM model. What events, in which people, lead to the formation and maintenance of maladaptive memories becomes an empirical question.
By emphasizing memory, we in no way deny the reality of the traumatic event, the usefulness of studying the traumatic event, or the losses caused by the event, which outlast the event itself in ways that do not rely on human memory. Consider a concrete example. A tornado destroys a person’s home, injures him physically restricting his mobility, scatters his friends removing his social supports, destroys the church from which he gains much of his emotional strength, and destroys his place of work changing his present and future economic status. The event is real and losses suffered by the person remain long after the tornado is past. Such losses have an extremely important effect on the individual’s psychological well being, however they are not the focus of the diagnostic criteria of the DSM, nor our model, and will be considered only briefly in relation to meta-analyses of factors contributing to PTSD.
The Hypotheses Derived from the Models
The following formal hypotheses all begin with the name of the model that generated them. The four hypotheses of the DSM model are counter to the first four hypotheses of the mnemonic model. We will show considerable support for the mnemonic model hypotheses, but not for the DSM model.
DSM – Memory (implied)
Memory for traumatic events, and for the emotions at the time of the event, is accurate and unchanging, although sometimes incomplete. Otherwise one would not allow retrospective reports of the A criteria to be used without questioning their validity.
Mnemonic – Memory
Memories for traumatic events and for the emotions at the time of the event change over time, as do all other memories. The changes that occur can often be understood using theories from research in cognition, emotion, and personality.
DSM – A1 (implied)
By definition, only A1 events cause PTSD symptoms. If there is no A1 event, by definition, the identical symptoms are Adjustment Disorder symptoms (American Psychiatric Association, 2000, p. 467), in which case, they should usually last less than six months, should not have an onset delayed by more than three months and have other differences from PTSD symptoms (American Psychiatric Association, 2000, p. 679–683). The DSM therefore implies a discontinuity in the frequency and severity of the PTSD that follows A1 versus non-A1 events.
Mnemonic – A1
Memory for both A1 and non-A1 events can lead to PTSD symptoms. What kinds of events are most effective in producing memories associated with PTSD symptoms is an empirical question, but, a priori, it is unlikely that it will be only the set of A1 events specified in the DSM.
DSM – A2 (implied)
By definition, A2 peritraumatic emotions are needed to cause PTSD symptoms. The DSM therefore implies a discontinuity in the frequency and severity of the PTSD that follows A2 versus non-A2 emotions.
Mnemonic – A2
Memory for both A2 and non-A2 peritraumatic emotions can lead to PTSD symptoms. Which particular peritraumatic emotions are most effective in producing PTSD symptoms is an empirical question, but, a priori, it is unlikely that it will be exactly the set of A2 emotions specified in the DSM.
DSM – C3
The C3 symptom is “an inability to recall an important aspect of the trauma” (American Psychiatric Association, 2000, p. 468).
Mnemonic – C3
According to what is known about memory in general and tunnel memory in stressful events, important aspects of the trauma should be better recalled. Thus, the C3 symptom should be poorly correlated with the remaining PTSD-symptoms.
Mnemonic – Gender
Because of gender differences in emotional autobiographical memories, woman will be more likely than men to develop PTSD symptoms for the same negative event. The DSM model makes no specific prediction.
Mnemonic – Neuroticism
Neuroticism is an interrelated set of tendencies that should increase the negative affect and availability of a memory of a very negative event, magnifying its impact and maintaining it over long periods. For that reason, level of neuroticism will be positively related to level of PTSD symptoms. The DSM model makes no specific predictions.
Mnemonic – Amnesia
The following hypotheses are all variants of the idea that symptom severity should vary systematically with the availability of the memory; in the extreme, if we could remove the memory completely we could prevent PTSD from developing or continuing. We exclude psychogenic amnesia, repression, and dissociation, because these are partial and temporary, thus allowing the memory to have effects, and because their psychogenic nature can lead to circular arguments. We include the following four specific hypotheses: Mnemonic – Organic Amnesia, Mnemonic – Pharmacologically Induced Amnesia, Mnemonic – Childhood Amnesia, and Mnemonic – Self-Relevance Memory Enhancement. The DSM Model makes no specific predictions beyond changes in some of the reliving symptoms that depend on having a conscious memory.
Methodological Considerations
Before reviewing the evidence for the mnemonic versus DSM model, some theoretical and methodological issues need to be discussed including how to test the models, the quality of the evidence available, and the two kinds of measures of PTSD.
Testing the Models
How can we test the DSM and mnemonic models of PTSD? Because the event is crucial, the ideal test for the DSM model would be to have a neutral observer present as people experience a variety of very negative events, interview the people, and record the nature of the events and the emotional reactions to them while the events are taking place. Based on the neutral observer’s reports, the events would be classified as A1 events or not and the peritraumatic emotions as A2 or not. PTSD symptoms would be examined after one month or later. We know of no such test. In some cases, the A1 criterion could be established from independent records of the traumatic event, replacing the independent observer, but the A2 criterion, by necessity, must be based on retrospective measures if a neutral observer is not present or online measures are not taken.
A major advantage for testing the mnemonic model is that we have measurements of the memory of the event made at the same time as measurements of PTSD symptoms and so data already exist to test it. For the DSM model, on the other hand, the actual event and peritraumatic reactions to it, not the memory, matter and so these same memories must be viewed as retrospective reports, or indirect measures, of an earlier event rather than the data that are needed by the DSM model. We will note the problems with retrospective reports as we proceed.
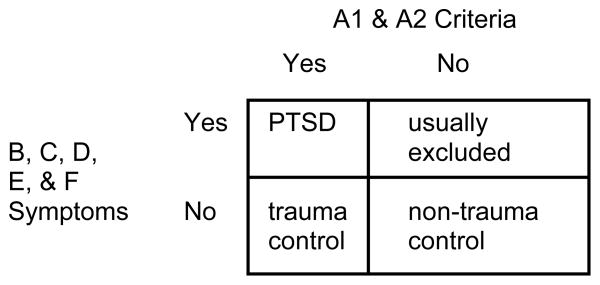
Missing evidence
The existing evidence is not ideal for our analyses, though we will use it to argue our points. Research on PTSD in large part uses the official diagnosis to set inclusion and exclusion criteria for participants. “The existence of an official taxonomy also has become an unintended straightjacket, as most researchers have limited themselves to the DSM criteria rather than investigating diverse sets of criteria” (Clark, Watson, & Reynolds, 1995, p. 123). Thus, the literature does not have all the data we would like to have for our analyses. As shown in Figure 2, there are people with and people without B, C, D, E, and F symptoms sufficient for a diagnosis of PTSD, and there are people with and people without the A1 and A2 criteria. All four cells of the two by two array defined by this situation are not equally well represented in the literature. People with the A1, A2, B, C, D, E, and F criteria have PTSD. People with or without A1 and A2 criteria but without B, C, D, E, and F symptoms are control participants. However, people without the A1 and A2 criteria but with the B, C, D, E, and F symptoms are usually excluded from much of the literature because they do not meet the inclusion criteria for PTSD, the inclusion criterion for the regular control group, and are not considered as a separate control group. We find and use some reports of such individuals from case studies and from researchers, who want to extend the diagnosis, but they remain an understudied group for our purposes, and so our data are not ideal. This is a serious problem for the field in general and the DSM model, in particular, since one cannot logically decide on whether the A1 and A2 criteria can be empirically justified without including all four cells of Figure 2, that is, without having groups with and without the A1 and A2 criteria.
Figure 2.
A categorization of people with and without PTSD criteria and symptoms.
Furthermore, to test the DSM model, we need a study that considers a very wide range of negative events, measures peritraumatic emotions to them when they take place, and then assesses PTSD symptoms at least one month after the event. No such study exists. This is true even if we allow retrospective reports of the A1 and A2 criteria. Thus, although our review here supporting the Mnemonic – A1 and Mnemonic – A2 hypotheses may be limited, it does not have to overcome any empirical support for the DSM – A1 and DSM – A2 hypotheses.
Two kinds of measures of PTSD
A dichotomous measure of PTSD is needed for diagnosis, because for clinical purposes a person either has PTSD or not. This measure depends on having the A1, A2, E, F, and at least one B, three C, and two D symptoms. Each judgment of a symptom is a binary decision on what in most cases is conceptually a continuous scale. The other is a continuous measure of PTSD symptom severity consisting of the sum of a participant’s rating scale responses to the 17 B, C, and D symptoms from the DSM. Most researchers prefer the continuous scale to the dichotomous one for good psychometric and theoretical reasons. PTSD is viewed as a continuum with a break made for diagnosis. Terms like sub-clinical, mild, moderate, or severe often modify PTSD in the literature. Moreover, because the B, C, and D scales are highly correlated, it is virtually impossible to get high PTSD severity scores without getting the right number of B, C, and D symptoms. Empirically, if one sets the cut off correctly on a PTSD scale and checks for A, E, and F symptoms then one gets a high concordance with the dichotomous measure (e.g., Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Davidson et al., 1997). Because of this, most research uses the continuous scale of PTSD severity. The two measures are confounded with two measurement methods. The dichotomous scale is usually obtained by clinicians using a structured interview. The continuous scale is often obtained by having a participant fill in a paper and pencil test. Here we use PTSD to imply the clinician administered dichotomous scale and PTSD symptoms and PTSD symptom severity to imply a continuous rating scale that may have been administered without a clinician’s supervision.
In the following, we question the DSM model and offer support for the mnemonic model under the four headings of Trauma versus Negative Event, Event versus Person, Event versus Memory, and Event with No Memory. To ensure our ability to generalize from experimental studies to studies for extreme events, especially for those results that may conflict with intuition or clinical insight, we support the general literature on memory and emotion with studies of memory for trauma, where such studies are available.
Trauma versus Negative Event
Several studies have shown a positive relation between trauma severity (measured according to the A1 and A2 criteria) and level of reliving, avoidance, and arousal symptoms (e.g., Brewin, Andrews & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003). However, these findings do not demonstrate that A1 and A2 characteristics are necessary for the development of PTSD; events that do not satisfy the A1 and A2 trauma criterion also may be followed by reliving, avoidance, and arousal symptoms at a level that would qualify for the PTSD-diagnosis, as predicted by the mnemonic model (Mnemonic A1 – Mnemonic A2).
In order to test the hypothesis, implied by the DSM, that A1 and A2 event characteristics are necessary for the development of PTSD, we logically have to examine the sequelae of negative events that do not satisfy the A1 and A2 trauma criteria. If such stressful, but non-traumatic, events show an ability to generate reliving, avoidance, and arousal symptoms at a level that would qualify for the PTSD-diagnosis, the hypothesis is falsified. Of course, one could still restrict PTSD using the A1 and A2 criteria, but some scientific justification should be given for the restriction. We first address the sequelae for stressful events that do not satisfy the A1 criterion. We review findings showing that such events nonetheless can be followed by PTSD symptoms. Second, we show that there is no evidence for the assumption underlying the A2 criterion that fear, horror, and helplessness at the time of the event are necessary for the development of PTSD symptoms – that is, it has not been demonstrated that PTSD symptoms cannot evolve in response to other negative emotional states.
The A1 event
According to criterion A1, only events “that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others” (American Psychiatric Association, 2000; p. 467) qualify as a traumatic event. According to most interpretations (e.g., Kilpatrick et al., 1998), simple bereavement (such as death of one’s spouse in old age) does not qualify for the A1 trauma criterion, nor does being bullied without physical injury or threats to physical integrity. If the A1 trauma criterion is a prerequisite for PTSD symptoms, we should not expect such events to cause the B, C, and D symptoms at levels qualifying for PTSD. However, this is contradicted by the data.
Examples of non-A1 events that cause PTSD symptoms severe and long enough to qualify for a PTSD diagnosis if the A criteria were met include: bullying at work without threats to physical integrity (Mikkelsen & Einarsen, 2002), death of a spouse among older adults (Elklit & O’Connor, 2005), stalking that does not meet the A1 criterion (Pathé & Mullen, 1997), discovering a spouse’s affair or having a miscarriage (Helzer, Robins & McEvoy, 1987), “18 months of persistent ‘dumping’ of work” on the patient by a superior (Scott & Stradling, 1994, p. 72), the sudden threatened or actual dissolution of a marriage, illegal acts and arrests of the patient’s teenage children, or the collapse of adoption arrangements (Burstein, 1985). In defence of the DSM model, one could argue that any of the particular positive case of PTSD in response to non-A1 events just listed could be over diagnosing that would disappear with stricter application of the B through F DSM criteria. This potential critique cannot be used with the studies that follow, which compare PTSD symptom severity as these scales are applied uniformly to all participants in a study, nor can it be applied to the Posttraumatic Stress Disorder Field Trial study that ends this section.
Another source of evidence that the A1 trauma criterion is not necessary for the development of reliving, avoidance, and arousal symptoms qualifying for PTSD comes from studies that compare PTSD symptom severity following A1 to non-A1 stressors. Solomon and Canino (1990) used a structured interview to study 543 victims who were selected because they were exposed to flooding and/or dioxin contamination in the St. Louis area or were outside the impact area, and 912 victims who were exposed to extensive flooding and deadly mudslides in Puerto Rico or were outside the impact area. In addition to measuring PTSD symptoms, they also assessed exposure to ordinary life events, not qualifying as A1 traumas (e.g., job loss, move, and money problems) to “empirically examine the PTSD sequelae of environmental stressors that include both ordinary and extraordinary events” (p. 228). In order to test the relevance of the criteria A1, both the common stressful events and stressors fulfilling the A1 criteria (flood/mudslide or flood/dioxin disaster exposure) were entered as predictors of PTSD in an ANCOVA, which controlled for the effects of lifetime predisaster PTSD symptomatology. In the St. Louis sample, the results showed that some of the ordinary stressful events related more closely to PTSD symptoms than did the A1 traumatic events. Disaster exposure in and of itself did not significantly predict the level of PTSD symptoms. In the Puerto Rican sample, disaster exposure did relate to increased levels of PTSD symptoms. However, “breaking up with a best friend” and “having to take someone into one’s house” and “other upsetting events” (p. 231) were more strongly associated with PTSD than disaster exposure.
Similarly, Street and Arias (2001) investigated the role of physical abuse (e.g., used a knife), which could qualify as an A1 symptom, and psychological abuse, which could not, on the severity of PTSD in battered women. Scales measuring physical and psychological abuse both predicted symptom severity when they were each the only predictors in a multiple regression, but when both were entered together, only psychological abuse remained significant.
Mol et al. (2005) randomly sampled adults from a family practice population. Given the health care system in the Netherlands, this sampling produced a representative sample of the general population. Participants filled out a checklist of very negative events, added ones not on the list, and then nominated and dated the worst event they had experienced. Keeping this event in mind, they filled out a 17-item PTSD symptom checklist. Only participants who nominated one and only one worst event that had occurred before the calendar year of the testing, and thus more than one month earlier, were included. Mol et al. obtained 284 adults who specified a worst event that was a A1 trauma (e.g., sudden death of a loved one including murder and suicide, sexual abuse, disaster, war) and 519 whose worst event was a non-A1 life event (e.g., non sudden or unspecified death of a love one, relational problems, problems with study or work such as unemployment, chronic illness). The groups did not differ on age, gender, education, or history of other stressful events. The average A1 event occurred 18 years earlier versus 12 years for the non A1 event.
In general, the PTSD symptoms to the A1 and non-A1 event were similar, and when all respondents were included, not statistically different even with a large sample. Thus, overall A1 events did not produce more PTSD symptoms than non-A1 events counter to what would be expected from the DSM – A1 hypothesis. In analyses correcting for demographic variables or limited to events within the last 30 years, symptoms for non-A1 events were statistically higher. This finding was opposite to what was expected, and the authors reported trying to refute it, post hoc, without success. They tried analyzing the data in several different ways including using only PTSD scores above the 90th percentile of the combined A1 and non A1 groups’ scores, comparing events that occurred in five-year strata, assigning sudden death of a loved to the non-A1 events, assigning all deaths to the A1 events, and examining each of the 17 symptoms that made up the PTSD scale separately. Only three categories of A1 events had mean PTSD severity scores above all non-A1 categories: child physical or sexual abuse, adult sexual abuse, and adult physical abuse. In addition, there were no differences between A1 and non-A1 events regarding the rankings of the 17 PTSD symptoms. Given the large representative sample and the consistency with the other results just reported, it seems safe to conclude that non-A1 events caused PTSD symptoms as severe as the A1 events and somewhat more severe under some analyses.
The Kilpatrick et al., (1998) study reported results of the Posttraumatic Stress Disorder Field Trial, a study specifically designed to investigate several key issues that were under consideration when possible changes in the diagnostic criteria for PTSD were being considered in a working group of the American Psychiatric Association. Like all studies, this one has limitations, but it is the study initiated by the American Psychiatric Association to suggest changes in the description of PTSD in the DSM III and cannot be faulted for misapplying the DSM criteria. One of the issues that the PTSD field trial addressed was the role of the A criteria for the development of PTSD symptoms. The participants were interviewed about exposure to “high-magnitude stressor events” at any time during their life (i.e., completed rape, other sexual assault, serious physical assault, other violent crime, homicide death of family members or close friends, serious accidents, natural or man made disasters, and military combat, p. 812) and about exposure to “low-magnitude stressor events” during the past year (p. 813) which included 11 events that were excluded from criterion A in the DSM version current at the time (e.g., non-violent death of family or friend, chronic illnesses, and relationship conflicts). PTSD diagnoses were based on structured interviews. Returning to Figure 2, an ideal population to test the role of the A1 stressor would have about half of the sample with and half without the A1 stressor. A systematic comparison of the probability of these two stressor types for being associated with PTSD symptoms was hampered by the fact that the large majority of participants (72%) reported exposure to both high and low magnitude events and by a substantial variability in the number of stressful events reported across the participants.
Among 66 participants who reported no high magnitude events during their lives and one or more low-magnitude events within the last year, 8 (12%) were found to be positive cases of PTSD, except for the A criteria. The 8 low-magnitude events were 6 deaths or serious illnesses, one divorce, and once case of being fired. Given the care with which the assessments were done, the 12% prevalence is strong evidence that was taken in diagnosis and is inconsistent with the authors’ conclusion that “these data indicated that PTSD occurred extremely rarely in the absence of high-magnitude events” (p. 818). Moreover, the great majority of participants with high-magnitude events also reported low magnitude events, rendering it hard to determine the relative effects of the two categories of stressors in general.
In summary, there is evidence from both self-report and interview studies that the A1 trauma criterion need not be met for PTSD symptoms to follow. However, it is unclear to what extent A1 events (or a subset of such events) may nonetheless increase the probability of PTSD relative to other events. For example, Mol et al. (2005) found that physical abuse (adult) and sexual and physical abuse (child) had the highest PTSD scores of all events. Among the life events, the category of relational problems had the highest score. Tentatively, this might suggest the importance of some social factors cutting across the current A1 versus non-A1 distinction. At the present, we simply do not have the relevant studies to decide on such possibilities. Thus, future research should study the aftermath of a range of negative events (as in Mol et al., 2005), should include measures of symptom severity, and should obtain measures of symptoms and event characteristics both through interviews and self-reports, to ensure convergence of findings across different measurements. Because of a multitude of potential interacting factors, this issue calls for substantial amounts of research before firm conclusions can be made. In general, the results reviewed in this section challenge the DSM – A1 hypothesis and are consistent with the Mnemonic – A1 hypothesis.
The A2 emotions
The DSM diagnosis specifies “the person’s response involved intense fear, helplessness, or horror.” (Criterion A2, American Psychiatric Association, 2000; p. 467). While it makes intuitive sense that strong emotion is associated with traumas, very little work has been done to examine whether the experience of fear, horror or helplessness are necessary preconditions for PTSD or whether PTSD symptoms may follow from events involving other intense negative emotions, such as anger, shame, and guilt (McNally, 2003a, b). Moreover, in the studies that have been done, the assessment of emotional reactions usually comes well after the event, when the assessment of PTSD is made and so is based on a retrospective judgement that we will note is subject to many post-event factors. We begin, however, at a more general level. Following basic theoretical and empirical research on emotion and memory, we argue that it is unlikely that PTSD symptoms would result from only the three specific negative emotional states currently required.
At a theoretical level, there are two general views of emotion. One is the dimensional view in which all emotions are characterized by two dimensions, valence and intensity or arousal (Russell, 1980; Russell & Carroll, 1999) or positive and negative affect (Watson & Tellegen, 1985). Within this view, the more recent vector model reduces the complexity further by considering valence as a binary, positive or negative, value so that degree of positive or negative valence is proportional to intensity (Bradley, Greenwald, Petry, & Lang, 1992; Bradley, & Lang, 1999). The other view is that each emotion has unique properties that cannot be easily accounted for by two dimensions (Levine & Pizarro, 2004). This view often includes the assumption that there are only a few basic emotions (Ekman, 1992; Izard, 1992). Most classifications of basic emotions include fear, whereas horror is rarely included, and helplessness is never included (see Ortony & Turner, 1990; Power & Dalgleish, 1997, for reviews). Thus, neither theoretical view privileges the A2 emotions.
Little is known about how particular emotions affect memory. Most studies of the effects of emotions on memory use only one emotion making comparisons among emotions impossible (Levine & Pizarro, 2004). Recently, research has been conducted using more than one emotion and varying both valence and intensity. Both dimensions are important, though intensity has the larger effect on most properties of autobiographical memory (Talarico, LaBar, & Rubin, 2004). However, we still have very little knowledge of the unique effects of individual emotions beyond the effects attributable to their intensity and valence.
The only possible explanation we could think of for privileging the A2 emotions is that they are supported in part by animal models based on fear conditioning and learned helplessness following fearful situations. Such conditioning models have proved very useful for understanding anxiety disorders in general and PTSD in particular (e.g., Foa, Zinbarg, & Olasov-Rothbaum, 1992; Mineka & Zinbarg, 1996, 2006). If this is the underlying motivation for the A2 emotions then the following issues should be considered. First, conditioning models should be found for a range of non-A2 negative emotions where there may be possible animal models (e.g., anger and disgust). Second, the possibility of extrapolating existing conditioning models to non-A2 emotions should be considered. Third, the range of possible human emotions involved in PTSD should not be limited to ones for which there are well-developed conditioning models.
In short, it seems premature from basic science to argue that the A2 emotions have a privileged status; doing so takes a strong theoretical stance on the nature of emotions that contradicts existing and well-established emotion theories. By including one emotion (fear) that is considered as basic in almost all theories, one emotion (horror) that is rarely included in this category and one (helplessness) that never is, the current diagnosis denies a special role for basic emotions. By assuming a small set of unique emotions, it denies the value of dimensional models. One alternative, which seems theoretically more reasonable and better empirically supported than the current A2 list, would be to assume initially that the current intensity of a negative emotion is what matters and then examine which, if any, negative emotions are especially effective in producing PTSD symptoms. Another alternative, to which we now turn, would be to examine which particular emotions have been shown to lead to B, C, and D symptoms.
Given the strong claims in the A2 section of the diagnosis and the lack of evidence in the general emotion literature for a privileged status of fear, horror, and helplessness, one might have expected to find considerable support in the PTSD literature to justify the A2 criterion. However, we could discover no evidence suggesting that negative emotional states other than fear, horror, and helplessness are not followed by PTSD symptoms. Two problems pervade the literature on peritraumatic emotions. One is the use of retrospective measurements of emotions, which decreases the accuracy of the reports of peritraumatic emotions and makes the difference between peritraumatic emotions and current emotions less clear. The other problem is that in most studies, either no emotions or only A2 emotions have been measured – leaving it unresolved whether other negative emotional states were present and might lead to similar reactions.
First, we examine fear. If reactions to fearful situations are the key to PTSD, one might expect PTSD to be most related to other fear related disorders such as panic and phobia disorders, but this is not the case (Cox, Clara, & Enns, 2002). However, in studies that measure fear retrospectively, fear is generally related to PTSD symptoms. Basoglu and colleagues have found positive correlations between retrospective measures of peritraumatic fear and PTSD symptoms among Turkish earthquake survivors (Basoglu, Salcioglu & Livanou, 2002; Basoglu, Kilic, Salcioglu, & Livanou, 2004; Kilic & Ulusoy, 2003; Livanou, Basoglu, Salcioglu, & Kalender, 2002; Salcioglu, Basoglu & Livanou, 2003). Similar findings have been reported for persons hospitalized for burns (Van Loey, Maas, Faber & Taal, 2003), among persons seeking mental health assistance after a terrorist attack (Tucker, Pfefferbaum, Nixon, & Dickson, 2000), among victims of violent crime (Brewin, Andrews & Rose, 2000), among victims of motor vehicle accidents (Ehlers, Mayou & Bryant, 1998), and among military health care workers exposed to an air disaster (Epstein, Fullerton & Ursano, 1998). A few studies have measured, but failed to find, an effect of retrospective reports of peritraumatic fear (Palmer, Kagee, Coyne, DeMichele, 2004; Roemer, Orsillo, Borkovec & Litz, 1998). Thus, with a few exceptions, retrospective assessment of peritraumatic fear appears to be associated with severity of PTSD symptoms. This finding has multiple possible interpretations. It is consistent with (1) the intensity of retrospective reports of one and only one A2 emotion (fear) being correlated with PTSD symptoms, or with (2) several negative A2, and possibly non-A2, emotions being related to PTSD symptoms, or with (3) any negative emotion being related to PTSD symptoms.
For the other two A2 emotions, helplessness and horror, the evidence is scarce and ambiguous. Tucker et al. (2000) found effects of peritraumatic helplessness on PTSD symptoms. Roemer, Orsillo, Borkovec and Litz (1998) found no significant correlation between PTSD and reports of horror, but did find a correlation with reports of helplessness and numbness during the event. Brewin et al., (2000) found a positive correlation between reports of horror and helplessness and PTSD symptoms, whereas Palmer et al., (2004) found no effects of either horror or helplessness. Thus, one of the A2 emotions (fear) seems more relevant than the other two.
Very few studies have examined the possible effects of negative emotional states other than the ones listed in the A2 criterion, though these data are needed to decide on whether the current A2 emotions are special. Exploratory studies show that many emotions may be associated with PTSD symptoms (e.g., Bernat, Ronfeldt, Calhoun & Arias, 1998; Berntsen & Rubin, 2007; Brewin et al., 2000; Grey, Holmes & Brewin, 2001; Silver & Iacono, 1984). Unfortunately, only a few studies were designed to disentangle the relative importance of different, but coexisting, peritraumatic emotions.
The strongest case for non-A2-emotions leading to increased PTSD symptoms can be made for shame, guilt, and anger. In Vietnam veterans, commission or exposure to atrocities, implicating shame, predicts PTSD or PTSD severity beyond other combat exposure, implicating fear (Beckham, Feldman, & Kirby1998; Yehuda, Southwick, & Giller, 1992). In addition, studies have investigated the role of shame directly. Street and Arias (2001) found that shame was more relevant than guilt in a sample of battered women, correlating.47 with PTSD symptom severity compared to.21 for guilt. Andrews, Brewin, Rose, and Kirk (2000) found that both shame and anger correlated with PTSD symptom severity at 1 and 6 months after a violent crime. Both emotions predicted PTSD symptoms (with control for degree of injury) at the 1 month delay, and shame also did so at the 6 months delay. Riggs, Dancu, Gershuny, Greenberg, and Foa (1992) found that anger measured one week after a crime predicted PTSD severity scores in female victims of physical or sexual assault, measured at one month, independent of measures of guilt and life threat. In the studies mentioned here, comparable measures of fear, horror, and helplessness were not included along with the measures of shame, guilt, or anger and so comparisons and possible interactions cannot be reported.
Ehlers, Mayou, and Bryant (1998) measured initial anger reactions to a motor vehicle accident shortly after it occurred and they also measured anger related to intrusive recollections 3 months and 1 year after the accident when PTSD symptom severity was measured. Initial anger reactions predicted PTSD symptom severity at 3 months and 1 year (r =.25 and.20). The 3 month assessment of anger related to intrusive recollections predicted PTSD symptom severity at 3 months and 1 year (r =.37 and.35) and the 1 year assessment of anger correlated with PTSD symptom at 1 year (r =.47). The fact that the size of the correlations increases over time may suggest emotions play more of a role in maintaining, than in initially forming, PTSD symptoms. Partial correlations showed that neither injury severity nor perceived threat during the accident accounted for these correlations. Thus, anger, shame and guilt appear to be especially important in maintaining symptoms. To draw more firm conclusions, future studies should measure a range of emotions as close to the event as possible and whenever symptoms are measured in order to separate the role of emotions in causing and maintaining PTSD. This should be done for a variety of events because different events would be likely to involve different emotions.
Strong support for the effect of non-A2 emotions was found in Kilpatrick et al.’s (1998) Posttraumatic Stress Disorder Field Trial study, the study designed by a working group of the American Psychiatric Association to investigate such issues, although this interpretation was not made by the authors as evidence against the A2 criteria. An orthogonal factor analysis based on retrospective data on initial emotional and other subjective responses to high-magnitude events (i.e., events satisfying the A1 criterion) yielded five factors that together accounted for 62% of the variance. Factor I accounted for 39% of the variance. It had nine items that were not emotions per se (i.e., dizziness, chest pain, shortness of breath, hot flashes, physical numbing, nausea/gastrointestinal, choking, sweating, and fear of going crazy or losing control of emotions.). As indicated by the name given to this factor by the authors, “panic/physiological arousal” many of these variables relate to panic and high arousal and thus may be related to fear as well as to other high arousal emotions and disgust. However, the items more directly related to fear, horror, and helplessness (i.e., scared, trembling or shaking, fear of death or serious injury, helplessness, confusion, and surprise) loaded on Factor II, which accounted for 8% of the variance. Factor III, which accounted for 6% of the variance, had three items: embarrassment, guilt and violated trust. Factor IV, which accounted for 5% of the variance, had three items: anger, disgust and sadness. Factors V, which accounted for 4% of the variance had three items, all associated with numbing and unreality. Thus, despite the fact that the Factor II, which related to fear and helplessness, had seven items, it accounted for less of the variance than the two factors addressing the non-A2 emotions of anger, disgust, embarrassment, guilt, sadness, and violated trust, which combined had six items.
More central to the relation of different emotions to PTSD symptoms is that when participants with and without current PTSD were compared on the five factors, the PTSD-group scored higher on all five factors (all ps<.001; no detailed statistics were given for each factor). Similar comparative analyses were conducted for participants with and without lifetime PTSD. We calculated the R2 based on the F-values in Kilpatrick et al. (1998, p. 820). In ranked order, the R2’s were.27 for embarrassment/guilt/violated trust (Factor III), and.26 for panic/physiological arousal (Factor I), and.25 for unreality/emotional numbing/detached as if in a dream (Factor V), and.24 for fear, helplessness and confusion (Factor II) and.14 for anger, disgust and sadness (Factor IV). Thus, the factor on which the non-A2 emotions of embarrassment, guilt, and violated trust loaded accounted for at least as much of the variance regarding the presence versus absence of life time PTSD as did the factor on which the A2 emotions loaded. The factor on which the non-A2 emotions of anger, disgust and sadness loaded also accounted for substantial variance. In addition, the importance of non-A2 emotions may have been underestimated here, because Kilpatrick et al. (1998) based their analyses of emotion on reactions to a set of ‘high-impact events’ only, many of which by their nature have fear as a major emotional component.
In summary, two points should be made. First, there is no evidence for the claim that fear, horror, and helplessness at the time of the event are necessary for the development of PTSD. The evidence generally supports a central role for fear in the development of PTSD symptoms, whereas mixed evidence is found for horror and helplessness. In addition, several studies suggest that a multitude of intense negative emotions, not limited to fear, horror and helplessness, contribute to PTSD, with most evidence for shame and anger. Second, research on the A2 emotions is hampered not only by a paucity of studies that have systematically examined the potential effects of emotions other than the ones listed under the A2 trauma criterion but also by the retrospective nature of the assessment of emotion. Most studies do not report on non-A2 emotions and almost all report the peritraumatic emotion remembered at the time of the measurement of the B, C, and D symptoms, and never the peritraumatic emotion itself. The study that comes closest to reporting peritraumatic emotion (Ehler’s et al., 1998) suggests that emotions play more of a role in maintaining than in initially forming PTSD symptoms. In agreement with our view, Harvey, Brewin, Jones, and Kopelman (2003) argue that the evidence that intense peritraumatic emotion is essential for PTSD is “not yet compelling” (p. 669). Thus, it appears methodologically and theoretically misguided to place the emphasis on the emotional reaction at the time of the event. A more promising strategy is to analyse which emotions are associated with the maintenance and retrieval of the traumatic memory, and how such emotions relate to PTSD symptoms over time. In general, the results reviewed in this section challenge the DSM – A2 hypothesis and are consistent with the Mnemonic – A2 hypothesis.
Event versus Person
The key theoretical question here is whether there are measures of individual differences that contribute to PTSD and, if so, whether these effects can be reasonably accounted for through the mechanism of memory formation and maintenance. Two recent, major meta-analyses have examined many factors related to PTSD: Brewin, Andrews, and Valentine, (2000) and Ozer, et al. (2003). Brewin, et al. (2000) reviewed the following factors, which we present ranked by their weighted average r’s: lack of social support,.40; life stress,.32; trauma severity,.23; adverse childhood other than previous trauma,.19; low intelligence,.18; low SES,.14, childhood abuse,.14; family psychiatric history,.13; female gender,.13; other previous trauma,.12; psychiatric history,.11; lack of education,.10; younger age,.06; and minority status,.05. Ozer, et al. (2003) found: peritraumatic dissociation,.35; perceived support, −.28; perceived life threat,.26; peritraumatic emotions,.26; prior trauma,.17; prior adjustment,.17; and family history of psychopathology,.17. Here we focus on studies of gender and neuroticism because they are particularly relevant to the mnemonic model (i.e., the Mnemonic Gender and Mnemonic Neuroticism hypotheses) and in spite of considerable data on these topics they are absent from one or both of the major meta-analyses. At the end of this section, we review findings related to other predisposing factors and their combined effects and discuss how they can be accounted for in our mnemonic model.
Gender
Methodologically gender has one major advantage: Gender does not change with a trauma, eliminating the problem of retrospective reporting. Gender should be important for several reasons. It is well documented that women are more prone to depression than males (e.g., Hankin & Abramson, 2001; Kuehner, 2003), that they are more prone to almost all anxiety disorders (Howell, Castle, & Yonkers, 2006), and show higher levels of general anxiety (e.g., Egloff & Schmulke, 2004) and neuroticism (Costa, & McCrae, 1992; for cultural variation see Costa, Terracciano, & McCrae, 2001). Because PTSD is an anxiety disorder, it seems reasonable to expect a greater prevalence of PTSD among females than males. Thus, in general, being female is a risk factor for PTSD. In terms of the mnemonic model, depression, anxiety, and neuroticism should all help maintain and enhance memory for an extremely stressful event. Nonetheless, one of the major meta-analysis of PTSD “omitted consideration of demographic factors such as gender, education, and ethnicity, as none of these factors is plausibly implicated in the psychological process of trauma response” (Ozer,, et al., 2003, p. 55). In the following, we briefly explain the relevance of gender in relation to our mnemonic model of PTSD, and then we consider the empirical evidence for a relation between gender and PTSD.
Neurobiological and behavioral evidence show that men and women differ regarding memories for emotional events (Cahill et al., 2001; Cahill, Uncapher, Kilpatrick, Alkire & Turner, 2004). Cahill (2003) speculated that sex-differences in brain activity during the processing of emotional episodes may be causally related to the greater prevalence of PTSD and clinical depression among women. Few studies have been conducted to examine gender differences at the behavioral level of autobiographical memory. Even though some of these studies have found little or no gender differences on some measures (e.g., Rubin, Schulkind & Rahhal, 1999), others have found reliable effects of gender, especially on emotion. For example, Davis (1999) showed that women recalled more childhood memories about emotional events and had faster access to such memories than males. This effect was not found for childhood memories of non-emotional events. Seidlitz and Diener (1998) found that women recalled more memories than men when requested to recall as many positive and negative experiences as possible within a short time period. Bauer, Stennes and Haight (2003) found that women’s narratives of personal events after age seven contained more references to emotions and other internal states than did men’s narratives. Herlitz, Nilsson and Backman (1997) found better performance among women than men on a number of different laboratory, episodic memory tasks, also when controlling for the women’s higher verbal abilities. They found no gender differences on tasks involving semantic memory, primary memory and priming. Pillemer, Wink, DiDonato and Sanborn (2003) found that older women provided more descriptions of specific episodes when interviewed about life changes even though they did not provide longer narratives than the male participants (see Fivush, 1998 and Nelson & Fivush, 2004 for gender differences on socialization regarding the use of autobiographical memory).
If these findings of non-traumatic events in men and women hold for memory of a traumatic event, women would be more inclined to think and talk about the event than men. Because women have easier access to the emotional memory, they may suffer more from intrusions and nightmares related to the trauma and may be more inclined to use the traumatic memory as a reference point for understanding themselves and the world, leading to maladaptive attributions (Berntsen & Rubin, 2006a). Being female is also a risk factor for neuroticism (Costa, & McCrae, 1992) and depression (e.g., Hankin & Abramson, 2001). Access to negative autobiographical memories is increased in depression though the memories are less specific (Williams, 1996). Neuroticism similarly increases access to emotionally negative autobiographical information, as we will discuss in the next section. Thus, some of the effects of gender on memory for the traumatic event may be mediated by neuroticism and depression. As we argue next, gender differences in PTSD are substantial.
Kesssler, Sonnega, Bromet, Hughes, and Nelson (1995), using DSM-III-R definitions, noted that in a representative sample of 5877 U.S.A. adults, 10% of the females and 5% of the males reported having PTSD sometime in their life. In contrast, there were differences in the frequency of reported traumas in the opposite direction with 60% of the men reporting at least one trauma compared with 51% of the women. Thus, the conditional probability of getting PTSD given that a trauma is reported is even higher in women (20%) than in men (8%), a ratio of 2.4 to 1.0. Moreover, there are differences in the kind of traumas experienced. To provide a more controlled estimate of the effects of gender on the likelihood of developing PTSD, we searched the literature for all studies allowing us to calculate the number of male and female participants and the percentage of each who had PTSD to the same nominal trauma, so that the findings could not be caused by the types of traumas encountered by males and females, respectively. We excluded all studies that included sexual assault with other kinds of assault. To produce the average percentages in Table 2, we weighted each study by its total number of participants, rather than averaging men and women separately because we did not want variations in the proportion of men and women in each study to have an effect on the results. When the type of trauma is controlled, general plays a substantial role with an odds ratio of 2.6 to 1.0, similar to the 2.4 to 1.0 ratio in Kessler et al., (1995) and the 2.0 to 1.0 ratio in Tolin and Foa (2006).
Table 2.
Studies with specific A1 events reporting percent of men and women with PTSD.
| First Author | Year | Event | n | Percent with PTSD |
Odds ratio | r | ||
|---|---|---|---|---|---|---|---|---|
| f | m | f/m | ||||||
| War and Terrorism Related Events | ||||||||
| Abenhaim | 1992 | Bombing, attack in France | 254 | 19 | 17 | 1.14 | 1.18 | 0.03 |
| Jehel | 2003 | Bombing in a Paris subway | 32 | 35 | 13 | 2.65 | 3.56 | 0.25 |
| North | 2005 | Bombing in Nairobi | 227 | 35 | 26 | 1.36 | 1.56 | 0.09 |
| Bombing in Oklahoma City | 182 | 34 | 20 | 1.74 | 2.13 | 0.17 | ||
| Verger | 2004 | Bombings in France | 196 | 38 | 23 | 1.65 | 2.05 | 0.16 |
| North | 1994 | Mass shootings | 126 | 36 | 20 | 1.90 | 2.46 | 0.17 |
| Blanchard | 2004 | September 11, 2001 | ||||||
| Albany, NY | 504 | 12 | 11 | 1.06 | 1.07 | 0.01 | ||
| Augusta, GA | 336 | 9 | 3 | 2.84 | 3.03 | 0.10 | ||
| Fargo, ND | 516 | 4 | 2 | 2.20 | 2.26 | 0.06 | ||
| DeLisi | 2003 | September 11, 2001 | 1009 | 24 | 13 | 1.78 | 2.03 | 0.14 |
| Pulcino | 2003 | September 11, 2001 | 988 | 10 | 5 | 2.06 | 2.18 | 0.10 |
| Schuster | 2001 | September 11, 2001 | 524 | 50 | 37 | 1.35 | 1.70 | 0.13 |
| Bleich | 2003 | Terrorism, Israel | 509 | 16 | 2 | 6.75 | 7.86 | 0.24 |
| Thapa | 2005 | Terrorism, Nepal | 290 | 59 | 50 | 1.19 | 1.47 | 0.09 |
| Wolfe | 1999 | Veterans, Gulf War | ||||||
| On return to U.S.A. | 2942 | 8 | 3 | 2.67 | 2.81 | 0.07 | ||
| 18–24 months later | 2313 | 16 | 7 | 2.29 | 2.53 | 0.09 | ||
| Natural Disasters and Related Events | ||||||||
| Parslow | 2006 | Bushfire | 2085 | 7 | 3 | 2.59 | 2.71 | 0.10 |
| Green | 1990 | Dam collapse | 120 | 31 | 23 | 1.35 | 1.50 | 0.08 |
| Bödvarsdóttir | 2004 | Earthquake in Iceland | 52 | 26 | 17 | 1.59 | 1.80 | 0.11 |
| Basoglu | 2002 | Earthquake in Turkey | 1000 | 53 | 33 | 1.61 | 2.29 | 0.19 |
| Basoglu | 2004 | Earthquake (epicenter) | 530 | 31 | 13 | 2.38 | 3.01 | 0.22 |
| Basoglu | 2004 | Earthquake (not epicenter) | 420 | 17 | 4 | 4.25 | 4.92 | 0.17 |
| Chang | 2005 | Earthquake in Taiwan | 252 | 41 | 20 | 1.95 | 2.56 | 0.21 |
| Livanou | 2002 | Earthquake in Turkey | 1027 | 71 | 46 | 1.54 | 2.87 | 0.22 |
| Yang | 2003 | Earthquake in Taiwan | 663 | 15 | 6 | 2.62 | 2.91 | 0.15 |
| Steinglass | 1990 | Flood in USA | 66 | 23 | 10 | 2.36 | 2.77 | 0.18 |
| Ironson | 1997 | Hurricane Andrew | 173 | 36 | 25 | 1.44 | 1.69 | 0.11 |
| Norris | 2001 | Hurricane Andrew (black) | 133 | 23 | 20 | 1.18 | 1.23 | 0.20 |
| Norris | 2001 | Hurricane Andrew (white) | 134 | 19 | 6 | 3.29 | 3.84 | 0.04 |
| Norris | 2001 | Hurricane Paulina, Mexico | 198 | 44 | 14 | 3.04 | 4.63 | 0.33 |
| Caldera | 2001 | Hurricane in Nicaragua | 496 | 7 | 2 | 3.19 | 3.35 | 0.08 |
| Steinglass | 1990 | Tornado in USA | 39 | 35 | 5 | 6.60 | 9.62 | 0.37 |
| Madakasira | 1987 | Tornado in USA | 111 | 62 | 62 | 1.00 | 1.00 | 0.00 |
| Motor Vehicle Accidents | ||||||||
| Blanchard | 1996 | Motor vehicle accident | 158 | 45 | 26 | 1.74 | 2.36 | 0.18 |
| Ehlers | 1998 | Motor vehicle accident | 888 | 29 | 18 | 1.59 | 1.83 | 0.13 |
| Freedman | 2002 | Motor vehicle accident | 197 | 14 | 20 | .71 | .66 | −0.08 |
| Frommberger | 1998 | Motor vehicle accident | 152 | 31 | 11 | 2.82 | 3.62 | 0.25 |
| Ursano | 1999 | Motor vehicle accident: | ||||||
| 1 month later | 122 | 52 | 19 | 2.76 | 4.65 | 0.35 | ||
| 3 months later | 99 | 31 | 20 | 1.53 | 1.76 | 0.12 | ||
| 6 months later | 99 | 22 | 14 | 1.60 | 1.77 | 0.13 | ||
| Medical and Other Events | ||||||||
| Defide | 1999 | Burn injury | 31 | 44 | 59 | 0.75 | 0.55 | −0.13 |
| Epstein | 1998 | Healthcare workers, disaster | 311 | 17 | 11 | 1.51 | 1.62 | 0.08 |
| Stukas | 1999 | Heart transplant & caregivers | 300 | 24 | 12 | 2.06 | 2.39 | 0.16 |
| Landolt | 2002 | Parents, child diagnosed | 73 | 24 | 22 | 1.09 | 1.12 | 0.02 |
| Murphy | 1999 | Parents, 4months after violent death of child | 261 | 40 | 14 | 2.86 | 4.10 | 0.26 |
| Murphy | 2002 | Parents, 5 years after violent death of child | 173 | 28 | 13 | 2.22 | 2.68 | 0.18 |
| Olley | 2005 | Patients, HIV diagnosis | 149 | 19 | 5 | 4.22 | 4.98 | 0.19 |
| Fullerton | 2004 | Rescue workers, plane crash | 116 | 22 | 16 | 1.42 | 1.54 | 0.06 |
| Brent | 1995 | Suicide of peer | 146 | 12 | 0 | - | - | 0.26 |
| Total n/Weighted average | 21,722 | 23 | 13 | 2.27 | 2.63 | 0.13 | ||
To provide a comparison to the other meta-analysis of gender as a PTSD risk factor, we followed Brewin et al’s. (2000) methods and calculated an r for each study. We did this by first calculating a chi-square for each study and we averaged r’s across studies in same way Brewin et al. did. As seen in Table 2, our average r was.13, which is the same value obtained in the Brewin et al. meta-analysis. Thus, in terms of r, our data are similar, but the implications we draw are different. From the simplest, most direct reporting of the data, which is the percentage of people who get a diagnosis of PTSD, we find that over twice as many women get the diagnosis as men, given the same nominal trauma. The odds ratio, which is more commonly reported in studies of disease, is over 2.5. From the series of calculations of turning percentages into a chi-square and then into a correlation, we find that less than 2% of the variance is explained by gender. Thus, according to the calculated correlation of r =.13, we find that gender has a small effect. Following the more straightforward analysis based on the frequencies, we find that gender has a big effect, namely more than a two to one difference. This discrepancy in the implications caused by reporting different statistics on the same data is not a problem unique to PTSD, in part, because different measures have different statistical properties (Fleiss, 1994; Rosenthal, 1994).
Neuroticism
Personality variables were not examined in the two major meta-analyses of PTSD (Brewin et al., 2000; Ozer et al., 2003; Watson, Gamez, & Simms, 2005), even though personality variables have been shown to influence exposure to traumatic events as well as post-event symptoms (e.g., Bowman, 1999; Lauterbach & Vrana, 2001). In general, personality factors interact with the phenomenology of autobiographical memory (Rubin & Seigler, 2004). Neuroticism is especially relevant in relation to our mnemonic model of PTSD for the following reasons. Neuroticism is a measure of general negative affectivity – such as worry, anxiety, and depression – that is identifiable early in life and shows longitudinal stability (e.g., Bowman, 1999; Martin, 1985). Neuroticism has been shown to affect level of PTSD symptoms. For example, Lauterbach and Vrana (2001) reported a moderate relationship between PTSD severity and trauma intensity for participants low in neuroticism whereas a strong relationship was found between trauma intensity and PTSD severity for participants high in neuroticism. One possible explanation, suggested by Lauterbach and Vrana, is that neuroticism magnifies the impact of the traumatic event (also see Bowman, 1999). If neuroticism acts as such a “magnifier,” according to the mnemonic model, it is likely to do so through autobiographical memory. This agrees with findings showing that higher scores on a neuroticism scale are associated with increased access to emotionally negative information, notably, emotionally negative information that is perceived as self-related (Martin, 1985; Teasdale & Green, 2004). Such negative self-focus has been considered a possible explanation for the observation that higher levels of neuroticism increases vulnerability to depression (Martin, 1985).
At a more general level, we included neuroticism here: because it is often measured in relation to PTSD; because some researchers have claimed that neuroticism is one of the most important predisposing factors for PTSD (e.g., Bowman, 1999); because neuroticism is an important theoretical concept related to PTSD (Weisæth, 2002) and other anxiety disorders (Watson, et al., 2005). We therefore assembled all the studies that we could find reporting on a relationship between neuroticism and PTSD that used the same traumatic events for all people so that the results could not be caused by people, who vary on neuroticism, varying in systematic ways on the type of traumas they report. In Table 3 we display all the studies we found along with an uncorrected r statistic as calculated in the Brewin et al. (2000) meta-analysis1.
Table 3.
Studies with specific A1 events reporting correlations with neuroticism.
| First Author | Year | Event | n | r |
|---|---|---|---|---|
| Chung | 2005 | Airplane, train crash | 148 | .40a |
| .36b | ||||
| Lewin | 1998 | Earthquake in Australia | 515 | .43c |
| McFarlane | 1988 | Bushfire disaster, firefighters | 45 | .20 |
| Parslow | 2006 | Bushfire disaster, residents | 2085 | .12d |
| Brodaty | 2004 | Holocaust survivors | 100 | .41 |
| Fauerbach | 2000 | Medical, burn survivors | 70 | .41 |
| Kelly | 1998 | Medical, HIV | 61 | .50 |
| Sembi | 1998 | Medical, stroke | 61 | .64 |
| Holeva | 2001 | Medical, traffic accidents | 265 | .44 |
| Engelhard | 2003 | Pregnancy loss | 118 | .25 |
| Watson | 2005 | Veterans, Gulf War | 573 | .44 |
| Casella | 1990 | Veterans, Vietnam, high combat | 46 | .61 |
| Hyer | 1994 | Veterans, Vietnam with PTSD | 52 | .32 |
| Davidson | 1987 | Veterans, WWII/Korean | 24 | .39 |
| Total n/Weighted average | 1415 | .43 | ||
IES intrusion scale, not included in the total n or average.
IES avoidance scale, not included in the total n or average.
IES, not included in the total n or average.
Not included in the total n or average, see footnote 1.
The effects of neuroticism are reliable with a weighted average of.43. As with most predisposing conditions considered in the two major meta-analyses we use for comparison, few studies include truly prospective measures. Even though neuroticism is a personality factor and is generally found to be stable through life, for Table 3, all but two of the studies measured neuroticism after the trauma; raising the possibility that neuroticism could be affected by the severity of PTSD as well as affecting it. Both the studies that measure neuroticism prior to the trauma (Engelhard, Van den Hout, & Kindt, 2003, and the Parslow et al., 2006 once it was corrected for its extreme marginals) had r’s of about.25, which are much smaller than the average of the other studies. Thus, the concern, about traumatic events affecting neuroticism, is well founded. More prospective studies are needed, and especially ones that continue to track neuroticism scores at several points after the stressful event.
If we do not restrict ourselves to prospective studies in order to provide a fair comparison with the two major meta-analyses, which make no such restrictions, we would use the weighted average r of.43. If we restrict ourselves to just the prospective studies, r would be.25. Either way the effect of neuroticism is large. The weighted average rs for factor in Brewin et al. (2000) that are.25 or larger are.40 for lack of social support and.32 for life stress. For Ozer et. al (2003) they are.35 for peritraumatic dissociation, −.28 for perceived support,.26 for perceived life threat, and.26 for peritraumatic emotions. Moreover, unlike Brewin et al. (2000), Ozer et al. (2003) statistically corrected r’s for studies that reported PTSD as a dichotomous as opposed to a continuous variable, which increased the corrected r’s by a minimum factor of 1.25 (Hunter and Schmidt, 1990). Thus, Ozer et al.’s (2003) findings are inflated compared to Brewin et al.’s and ours whenever a dichotomous PTSD variable is used.
We could find no study for which greater neuroticism resulted in statistically significant lower frequency or lower severity of PTSD. Given its theoretical importance and the large number of studies that measure neuroticism and PTSD including those we did not include because they did not involve the same traumatic event for all people, it is surprising that neuroticism has not received more attention in current theories of PTSD. However, it does have a central role to play in the mnemonic model of PTSD as a magnifier of memory for negative events.
Other predisposing factors
What other individual difference factors should be important according to our mnemonic model? Education and intelligence should help protect against PTSD by providing more cognitive resources for problem solving activity to conceptualize traumatic events in ways that reduce negative affect in their memories. Social economic status (SES) should help protect against PTSD by providing more economic resources to lessen the aftermath of some traumatic events and thus the current memory of them. Similarly, social support should help protect against PTSD by providing people help to reconceptualize the trauma and ease current concerns caused by the trauma. Sharing negative events with others has been found to enhance the pace with which negative affect fades over time, in contrast to some private forms of rehearsal (Ritchie et al., 2006). In terms of the mnemonic model, a personal history of psychiatric problems would indicate modes of thought conducive to producing and maintaining a highly available, negative memory. Family history could function through the inheritance of such biases in cognitive and emotional processes, through their early learning, through reduced social support, or insecure attachment (Conway, Singer, & Tagini, 2004). For education, intelligence, SES, social support, individual history of psychiatric or adjustment problems, and a family history of such problems, Brewin et al. report weighted r’s in the expected direction of.14,.18,.14,.40,.11, and.13. Ozer et al. report corrected weighted r’s for social support, individual history of psychiatric or adjustment problems, and a family history of such problems of.28,.17, and.17. The effects, while not large in all studies reviewed, are reliable. We could find no study for which those with more education, more intelligence, more social support, less individual or family history of psychiatric problems had statistically significant higher frequency or higher severity of PTSD.
Combinations of predisposing factors
The meta-analyses of PTSD, because of the varied data they must summarize, must keep the effects of each variable independent. Because different studies measure different variables, in meta-analyses the individual effects cannot be easily combined in a multiple regression or other statistical ways to measure their combined effects. Thus, when taken together, the variables tied to the person as opposed to the event could provide a much larger contribution than any one of them taken by itself, and “the sum of pre-trauma factors might then outweigh the apparently larger impact of trauma severity” (Brewin et al., 2000, p. 756). In general, the results reviewed in this section support the Mnemonic – Gender hypothesis and the Mnemonic – Neuroticism hypothesis.
Event versus Memory
The A1 and A2 criteria of the PTSD diagnosis refer to the objective content of the traumatic event and the person’s emotional reaction to the event as it was occurring (American Psychiatric Association, 1994). However, in most cases, there is no access to the A1 and A2 criteria except later through the person’s memory. Since the beginning of modern cognitive psychology (e.g., Bartlett, 1932) memory has been viewed as constructive, with distortions made through schemata (see Rubin, 1995 for a review). Personal memory is prone to error and distortion, often in systematic ways. This observation also holds for memories of traumatic events (e.g., van Giezen, Arensman, Spinhoven and Wolters, 2005). In the following, we review three common sources of distortion and biases in memory for emotional events that are especially relevant for PTSD (tunnel memory, observer memory, and current goals and attitudes) and we show how such distortions apply to memory for trauma. We also show how certain reactions (often labeled as peritraumatic dissociation) that are assumed to take place at the time of the event as a trauma-specific response may be more parsimoniously explained in terms of general reconstructive memory processes at the time of recall (see also Candel & Merckelbach, 2003, for a critical review).
Tunnel memory
The notion of tunnel memory refers to a narrowing of attention and memory so that, compared to a neutral situation, the most central parts of an emotionally arousing situation are better remembered, and the peripheral parts are remembered less well (Safer, Christianson, Autry, & Österlund, 1998). Tunnel memory for autobiographical events is only found for a range of intensely negative emotions, not for intensely positive emotions (Berntsen, 2002; Talarico, Berntsen, & Rubin, unpubl. ms.).
Consistent with the idea of tunnel memory, several studies have shown that, while memory for peripheral details are reduced by high levels of arousal, memory for central details are facilitated (e.g., Burke, Heuer, & Reisberg, 1992; Christianson & Loftus, 1991; Christianson, Loftus, Hoffman, & Loftus, 1991; Wessel & Merckelbach, 1994; see Christianson, 1992, for a review). This effect has been found in both the laboratory and naturalistic studies, such as studies on memory for crimes and among asylum seekers, in which the life threatening nature of the event and the type and intensity of negative emotion are in the A1 and A2 range (e.g., Herlihy, Scragg & Turner, 2002; Steblay, 1992; Yuille & Cutshall, 1986)
In this context, empirical studies of tunnel memory directly contradict one of the DSM symptoms. In the autobiographical memory literature, central details are defined as important for the emotional reaction and for the gist of the event (e.g., Berntsen, 2002; Christianson & Loftus, 1990). Thus, central details are important parts of the event, by definition. Tunnel memory is therefore the opposite of one of the symptoms: C3 – the inability to recall an important aspect of the trauma (American Psychiatric Association, 1994, p. 428). The theoretical motivation for the C3 is the idea of dissociative amnesia – i.e., the assumption that voluntary memory of the traumatic event is impaired (e.g., Brewin & Holmes, 2003). However, studies have repeatedly demonstrated that memories for trauma are coherent (Berntsen, Willert, & Rubin, 2003; Kihlstrom, 2006; Porter & Birt, 2001; Porter & Peace, 2007; Rubin, Feldman, & Beckham, 2003) and that dissociative amnesia is rare among trauma victims suffering from PTSD (see Merckelbach, Dekkers, Wessel, & Roefs, 2003a, 2003b, for original work and reviews).
Following research on tunnel memory, we therefore predicted that the C3 would not be related to other PTSD symptoms. How can we test empirically whether the C3 symptom really fits with the other symptoms? One way is to examine how the C3 item fares in studies of the statistical structure of the PTSD symptoms. There are numerous investigations of the contribution to the underlying factor structure of the 17 symptoms that make up the DSM PTSD diagnosis. In many cases, these studies report the loadings of the 17 items corresponding to the PTSD symptoms on the best models found or hypothesized. To test whether the C3 symptom is as useful a contributor to the underlying factor structure as are the other symptoms, we examined it loadings in these studies.
For a study to be considered here, the C3 item included in the study had to refer to forgetting important parts of the stressful event, not just to poor memory in general, poor memory for the event in general, or poor memory for certain things about the event (e.g., Breslau, Davis, Andreski, & Peterson, 1991). Some of the factor analyses were exploratory and were intended only to describe the data; most were confirmatory intended to test various models that had 2, 3, or 4 factors. The studies report a variety of statistics, but all studies that report results for individual items report the loading of each item on the factor on which it had the highest loading for exploratory factor analyses or on the factor that the best fitting model predicted it would load, and often provide no further information on each item. Table 4 therefore reports, for each study we could find that included an item for each symptom, the following information: the first author and year of the study, the number of participants, a brief description of the participants, the PTSD test used, the number of factors used, the loading of the C3 item and the range of all other items on the factor on which each item was predicted to fit best or on which it loaded the highest, and the rank of the C3 item loading from best (1) to worst (17).
Table 4.
Factor analyses of PTSD symptoms reporting a C3 item.
| Study |
Participants |
Test | Factors | Maximum Loadings C3 (others) | C3 rank | ||
|---|---|---|---|---|---|---|---|
| First Author | Year | n | Description | ||||
| Asmundson | 2000 | 349 | routine medical patients | PCL-C | 4 | .67 (.55–.85) | 14 |
| Asmundson | 2003 | 427 | male UN peacekeepers, | PCL-M | 4 | .56 (.33–.87) | 15 |
| 321 | with chronic back pain | 2 | .56 (.42–1.07) | 16 | |||
| without chronic back pain | PCL-M | 4 | .62 (.22–.90) | 16 | |||
| 2 | .61 (.63–1.16) | 17 | |||||
| Baschnagel | 2005 | 748 | undergraduates, 1 month post 9/11 for 9/11 events | PDS | 4 | .35 (.51–.83) | 17 |
| 705 | undergraduates, 3 months post 9/11 for 9/11 | PDS | 4 | .60 (.49–.84) | 14 | ||
| Buckley | 1998 | 217 | survivors of MVA, 49% PTSD | CAPS | 2 | .32 (.47–.80) | 17 |
| Cordova | 2000 | 142 | woman who had breast cancer | PCL-C | 3 | .41 (.47–.95) | 17 |
| Davidson | 1997 | 241 | war, rape, or hurricane trauma | D-F | 2 | .63 (.73–.90) | 17 |
| D-S | 2 | .82 (.77–.89) | 15 | ||||
| 67 | of 241 with current PTSD | D-F | 6 | .56 (.57–.84) | 17 | ||
| D-S | 6 | .79 (.60–.84) | 7 | ||||
| DuHamela | 2004 | 236 | bone marrow transplantation | PCL-C | 4 | .56 (.22–.76) | 13 |
| Kilpatrickb | 1998 | 528 | help seeking & community | SCID | 2 | .43 (.52–.77) | 17 |
| King | 1998 | 524 | male veterans, 70% had PTSD | CAPS | 4 | .27 (.51–.77) | 17 |
| Maes | 1998a | 130 | hotel fire, 55 car crash, 23%PTSD | ||||
| exploratory, oblique | CIDI | 3 | .49 (.37–.79) | 13.5 | |||
| exploratory, orthogonal | 3 | .48 (.41–.70) | 14 | ||||
| confirmatory, based on DSM-III | 3 | .37 (.43–.56) | 17 | ||||
| 1998b | exploratory, oblique | 2 | .49 (.32–.71) | 13 | |||
| exploratory, orthogonal | 2 | .48 (.36–.69) | 15 | ||||
| exploratory, 42 with PTSD only | 2 | .39 (.04–.78) | 14 | ||||
| confirmatory | 2 | .39 (.37–.65) | 16 | ||||
| confirmatory, 130 fire only | 2 | .38 (.42–.63) | 17 | ||||
| Palmieri | 2005 | 1,218 | women in sexual harassment lawsuit | PCL-C | 4 | .45 (.72–.90) | 17 |
| Shelby | 2005 | 148 | women who had breast cancer | PCL-C | 4 | .38 (.23–.84) | 15 |
| PCL-C | 3 | .44 (.28–.87) | 11 | ||||
| Simms | 2002 | 948 | deployed, first sample | PCL-M | 4 | .54 (.45–.89) | 15 |
| 948 | deployed, second sample | PCL-M | 4 | .49 (.61–.80) | 17 | ||
| 1,799 | not deployed in Gulf War | PCL-M | 4 | .40 (.59–.83) | 17 | ||
| 419 | of 1,896 deployed with A criteria | PCL-M | 4 | .47 (.63–.84) | 17 | ||
| Stewart | 1999 | 284 | substance-abusing women | PSS | 4 | .86 (.39–.86) | 1.5 |
| Tayor | 1998 | 103 | motor vehicle accidents | SCID | 2 | .17 (.42–.75) | 17 |
| 419 | UN peacekeepers | PSS | 2 | .44 (.46–.88) | 17 | ||
| Ventureyra | 2002 | 113 | outpatients with PTSD, 31 controls | PCSS | 3 | .08 (.07–.92) | 16 |
Notes: The lowest rank is 17. The following abbreviations are used for the PTSD tests: CAPS, Clinicial-Administered PTSD Scale, (Blake, et al., 1995); CIDI, Composite International Diagnostic Interview, (Smeets, Smeets, & Dingemans, 1993). DIS, modified Diagnostic Interview Schedule (Robins, Helzer, Croughan, & Ratcliff, 1981); PCL-C. PCL-M, PCL-S (Weathers, Litz, Huska, & Keane, 1994; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996); PDS, Posttraumatic Diagnostic Scale, (Foa, Cashman, Jaycox, & Perry, 1997); PSS PTSD Symptom Scale (Foa, Riggs, Dancu, & Rothbaum, B1993) ; SCID, Structured Clinical Interview for the DSM-III-R (Spitzer, Williams, & Gibbon, 1987).
DuHamel et al. (2004) data included 110 of 111 participants in Smith et al. (1999).
Kilpatrick et al. (1998) used both the SCID and the DIS.
As shown in Table 4, the C3 criterion in the majority of analyses had a rank of 15, 16, or 17 and it had a rank at or above the median rank of 9 in only two analyses. It often had the lowest loading, often much lower and out of the range of the rest of the items, which was noted explicitly in a few of the studies. One study not shown in Table 4 (Foa, Riggs, & Gershuny, 1995) started out with all 17 items and then removed the C3 item because it loaded as the only item on a fourth factor and without it there were three theoretically relevant factors. When the C3 item did not have the absolute lowest loading, it usually had one of the lower loadings. This occurs with a variety of 2, 3, 4 and 6 factor solutions and with populations that vary widely in the severity of their trauma and gender. In the Stewart, Conrod, Pihl, and Dongier (1999) study, however, the C3 is tied for the highest loading. The participants were selected for this study because of substance abuse, not PTSD, which offers an alternative explanation for the correlation of the severity of their problems with remembering central parts of the event and other PTSD symptoms than the underlying factor structure of PTSD symptoms. In the Stewart et al. (1999) study, the C3 loaded on a factor with avoiding thoughts (C1) and avoiding reminders (C2) of the trauma, which suggests that substance abuse may be in part an attempt to avoid the memory. Thus, as expected from the empirical work on tunnel memory, except in a sample in which people were selected for substance abuse rather than PTSD symptoms or events, the C3 item is an outlier from the perspective of correlating in a theoretically expected way with other symptoms. This finding has been overlooked by the current diagnosis of PTSD and by other accounts of this disorder, many of which base their theory on the assumption of trauma specific reactions at the time of the event that lead to impaired and fragmented memories (see Dalgleish, 2004, for a overview). Such accounts predict the C3 symptom to correlate well with the other symptoms of PTSD, contrary to the evidence reviewed here. Our review contradicts hypotheses DSM – C3 and supports hypothesis Mnemonic – C3.
Observer memory
Autobiographical memories may be recalled from two different perspectives: Field memories in which the person remembers the scene from his or her original point of view and observer memories in which the person remembers the scene as an observer would, often seeing him- or herself in the memory image. The distinction dates back at least to Freud (1899/1953), who used observer memory as evidence of constructive memory. Nigro and Neisser (1983) who coined these terms found that field memories were slightly more common and more recent than observer memories. Events associated with self-awareness (e.g., “giving an individual public presentation,” p. 475) and fear (“walking or running from threatening situation,” p. 475) were more frequently remembered from an observer perspective. Robinson and Swanson (1993) found that a voluntary shift from field to observer memories led to reduced affect associated with the memories, but that shifting from observer to field perspective had no effect on affect (see Berntsen & Rubin, 2006b, for a replication and extension).
Recent research has documented that memories recalled from a field perspective are generally experienced as more emotional and contain more information on emotional and other subjective states as compared to observer memories. This pattern has been found both in studies where perspective has been manipulated and in studies in which the relation between memory characteristics and naturally occurring field/observer perspective has been examined (see Berntsen & Rubin, 2006b, for a review). Recollecting from an observer perspective may therefore be a way to reduce reliving of stressful emotion (and even of chronic pain, McNamara, Benson, McGeeney, Brown, & Albert, 2005) at the time of recall. If so, observer perspective may in such cases reflect an avoidance attempt – a need to distance oneself from emotionally painful memories. Studies on reliving qualities of traumatic memories lend some support to this possibility (see Berntsen & Rubin, 2006b for a review).
Observer and tunnel memory in the out-of-body experience
The use of observer perspective as a memory strategy serving to defend the person against strong emotional reliving of the unpleasant memory may offer an alternative explanation of the clinical notion of out-of-body experiences. In the clinical literature, out-of-body experience is frequently described as an aspect of peritraumatic dissociation in which, at the time of the traumatic event, the person feels that he or she is mentally leaving his or her body and observing the stressful event from a distance (e.g., van der Hart, van der Kolk, & Boon, 1998; Ozer & Weiss, 2004). Two observations suggest that alternative views should be considered. First, although the out-of-body experience is reported as occurring at the time of the event, it is always a retrospective report of how an event is recalled. Second, out-of-body experiences occur in many non-traumatic situations such as meditation and relaxation (for a review see Blackmore, 1987) and in epileptic seizures (Blanke et al., 2005). One alternative interpretation, that is consistent with the mnemonic model, is that reports of out-of-body experiences may not be indications of peritraumatic dissociation at the time of the event but of constructive memory processes serving to dampen emotional reliving at the time of recall.
In addition, tunnel memory may facilitate reports of out-of-body experiences and also account for why it tends to occur in situations of extremely intense negative emotions. According to the literature on tunnel memory just reviewed, people recalling a very negative event often have few details with which to anchor their own location. Therefore, they may remember the event as if they are floating context free, that is, in an out-of-body experience. Thus, the later out-of-body-experience report may come from a lack of encoding of information needed to construct a memory from a particular perspective as opposed to a floating ambiguous perspective (Blackmore, 1984, 1987). This claim of fewer details leading to an observer perspective is consistent with the empirical literature. People who experience an event without visual input tend to remember it from an observer perspective (Rubin, Burt, & Fifield, 2003), and as initially noted by Freud (1899/1953), older memories tend to be recalled more often from an observer perspective (e.g., Nigro & Neisser, 1983; Rice, Talarico & Rubin, 2005; Robinson & Swanson, 1993). The combination of distancing oneself from an event and impoverished peripheral details might lead to a perception of an out-of-body-experience at the time of the event, but this needs to be tested, not assumed. Moreover, it would be caused by mundane cognitive processes.
In general, peritraumatic dissociation is often assumed to play an important causal role for the development of PTSD. For example, in Ozer et al.’s (2003) meta-analysis, peritraumatic dissociation was found to be one of the major predictors for PTSD. However, peritraumatic dissociation is not measured at the time of the trauma, but later usually at the time of diagnosis. The shortest delays obtained in some research studies occur when assessment occurs in an emergency room after medical needs have been met, but this is still a retrospective report of what occurred at the trauma taken in surroundings that were very different from the trauma itself, often after some medications have been administered to relieve suffering. Questions to the patient about the trauma are likely to be of the form ‘how did you feel then’ rather than ‘how do you feel now’ To the extent retrospective reports of peritraumatic dissociation reflect observer memory, tunnel memory, and related reconstructive processes at recall, the causal role of peritraumatic dissociation for the development of PTSD (e.g., Ozer & Weiss, 2004) is questioned. According to the mnemonic model, it is the current memory, which involves what retrospectively appears to be peritraumatic dissociation, that is important.
Current goals and attitudes
The idea that memory is reconstructed to take into account the individual’s goals and current concerns is a basic tenant of research on memory and cognition (Bartlett, 1932; James, 1890; Neisser, 1967) social cognition (Greenwald, 1980) as well as Freud’s (1901/1960) analyses of memory distortions. Goals and attitudes are central to the dynamic and reconstructive nature of autobiographical memory (for reviews see Conway & Pleydell-Pearce, 2000; Conway, 2005). Research has shown that such reconstructions take place both for the factual parts of the event (corresponding to the A1 trauma criterion) and for memory for emotional reactions (corresponding to the A2 trauma criterion).
Ratings of prior emotional states are prone to error and reconstruction (Christianson & Safer, 1996; Levine, 1997). This observation is especially relevant in relation to the extensive use of retrospective reports of peritraumatic emotion in the PTSD literature and diagnosis. In a radical interpretation, prior emotional states are not remembered at all but constructed from higher order knowledge at retrieval (James 1890; see Christianson & Safer, 1996, for an overview). A less radical position would be to assume that emotions are retained in a fashion similar to other kinds of sensory and perceptual information and that they are subject to similar forgetting, though with their own forgetting rate (Rubin, 2005, 2006). This implies that memories for all sorts of emotional events lose intensity over time. However, this reduction interacts with a number of factors. Ratings of emotional intensity generally decrease more rapidly for negative than for positive events – a phenomenon known as the fading affect bias (Walker, Vogl, & Thompson, 1997; see Walker, Skowronski & Thompson, 2003, for a review). However, this bias not found for dysphoric people (Walker, Skowronski, Gibbons, Vogl, & Thompson, 2003) and is also countered by the perceived self-importance of the event as well as certain forms of private rehearsal, such as involuntary memories (Berntsen, 1996), that help to maintain the emotional intensity associated with negative events (Ritchie et al., 2006). In addition, several studies have demonstrated systematic reconstructive errors in memory for prior emotional states as a function of the person’s present attitudes (see Levine & Safer, 2002, for a review).
Many studies of flashbulb memories (i.e., memories for the personal context for the reception of surprising and important news) have used a similar test-retest methodology and typically demonstrated considerable inconsistencies between the memory descriptions produced at the first and the second recording (e.g., Talarico & Rubin, 2003). Thus, although flashbulb memories seem to be more durable than memories for mundane events when tested at long delays (Berntsen & Thomsen, 2005) studies of flashbulb memories document that personal memory of highly emotional events is prone to error and distortion. Memory for traumatic events is no exception. Van Giezen, Arensman, Spinhoven and Wolters (2005) reviewed seventeen studies in which memories for traumatic events, assaults, or war zone exposure, had been tested at two occasions. In all seventeen studies, inconsistencies between the two reports were identified. Furthermore, in three out of nine reports of war zone exposure, an interaction was found with higher PTSD symptom severity associated with more amplifications of the memory (also see Dohrenwend, 2006).
For example, Roemer, Litz, Orsillo, Ehlich and Friedman (1998) studied the memory of 460 U.S. soldiers who had served in a peacekeeping mission in Somalia. They were asked twice to report the frequency with which they had been exposed to very stressful experiences related to peacekeeping duty while in Somalia: once within the first year of their return to the US and once 1 to 3 years later. On average, soldiers demonstrated a significant increase in their frequency reports of stressful events from the first to the second report. But soldiers with PTSD increased their frequency score significantly more than soldiers without PTSD. Similarly, Southwick, Morgan, Nicolaou, and Charney (1997) studied 59 veterans of Operation Desert Storm. The veterans were asked whether they had experienced 19 different potential traumatic stressors during the war that were specific events not subject to broad interpretation (e.g., seeing others killed or wounded, firefights, unit ambushed, observing the death of a close friend). They completed the questionnaire 1 month and 2 years after their return from the Gulf War. At the 2 year test, their PTSD symptoms were measured. There was a correlation of.32 between PTSD symptom score and the number of responses on the trauma questionnaire changing from “no” at the first report to “yes” at the second report. In a non-combat situation, Schwarz, Kowalski, and McNally (1993) studied changes in memory and emotional reactions 6 and 18 months after a school shooting. Although the study included only a dozen participants, forcing conclusions to be tentative, the relations among PTSD symptom severity and increases in the severity of the memory for the event were large and often statistically significant. Qin et al. (2003) studied memory consistency for the September 11th terrorist attack among individuals with and without a history of PTSD. Memory reports were obtained 1 month after the event and again 10 month after the event. It was found that at 10 months after the event, the PTSD-group overestimated their 1 month report of worry in response to the attack whereas the non-PTSD group did not. In contrast, Porter and Peace (2007) found no relation between PTSD symptoms and trauma memory consistency in a study with undergraduates.
In general, “effect sizes for trauma severity in retrospective studies are significantly greater than in prospective studies” (Brewin et al., 2000, p.755). If memory were accurate, and if the event were the major cause then the effect sizes should be equivalent. The reported differences, however, are consistent with current levels of PTSD symptoms causing the original event to be remembered as more severe. These findings seriously question the common assumption that positive correlations between retrospective assessments of A1 and A2 trauma severity and levels of PTSD symptoms imply that trauma severity is causally related to level of PTSD. What can be concluded is merely the existence of a positive association between PTSD and trauma severity in memory, with the possibility that this relation is caused by the current state of distress as well as by the past objectively viewed reality of the traumatic event. In general, the results reviewed in this section challenge the DSM – Memory hypothesis and support the Mnemonic – Memory hypothesis.
Event with No Memory
In this section, we review evidence showing that level of PTSD symptoms vary systematically with the availability of the traumatic memory. This pattern is found even in cases where the unavailability of a trauma memory indicates that a more severe traumatic event occurred. Our review includes the following four sections: Organic Amnesia, Pharmacologically Induced Amnesia, Childhood Amnesia and Self-Relevance Memory Enhancement.
Organic amnesia
According to the mnemonic model, individuals with Traumatic Brain Injury (TBI) would be less likely to show symptoms of PTSD to the extent that the TBI involves amnesia for the traumatic event. As we will review here, the literature supports this prediction. Although individuals with Traumatic Brain Injury (TBI) may suffer from PTSD, several studies show that they are less likely to be diagnosed with PTSD than individuals without TBI for similar events (mostly road traffic accidents, for reviews, see Harvey, Brewin, Jones & Kopelman, 2003; Gil, Caspi, Ben-Ari, & Klein, 2006; Klein, Caspi, & Gil, 2003). This is particularly noteworthy since the diagnosis of TBI has many overlapping symptoms with PTSD (e.g., Parker, 2002), which should increase the likelihood of a coexistence of the two diagnoses, other things being equal, and since TBI indicates severe physical injury at the time of the event – a risk factor for PTSD (American Psychiatric Association, 2000; Blanchard, Hickling, Taylor, Loos, Forneris, & Jaccard, 1996; Frommberger, et al., 1998; Urano, et al., 1999).
The prevalence of PTSD among individuals with TBI shows substantial variability across studies. As reviewed by Harvey et al. (2003) and Klein et al. (2003) studies of PTSD in TBI populations tend to fall in two classes: one showing an extremely low prevalence of PTSD among individuals with TBI and another suggesting that PTSD may be as common, though not higher, for people with as without TBI. For example, a very low prevalence of PTSD (0–4%) was found in four studies reviewed by Harvey et al. (2003). In the remaining studies, which involved eight different TBI samples, prevalence of PTSD ranged 14–48%. For both categories, the stressor was either motor vehicle accidents or a range of mixed events.
One possible explanation of this variability, consistent with the mnemonic model, concerns presence versus absence of a memory for the traumatic event. Even though many individuals with TBI suffer from amnesia for the injury event, this is not always the case (Klein et al., 2003). At the same time, very few studies on the co-existence of PTSD and TBI have carefully examined whether the participants are actually amnesic with regard to the injury event. Such studies (involving largely survivors of road traffic accidents) lend strong support to our prediction that the presence of PTSD varies systematically with availability of the traumatic memory. Using a detailed memory questionnaire administered four times, including once within 24 hours of the injury, Gil, Caspi, Ben-Ari, Koren and Klein (2005) found that at the 24-hour interview, 55 of their participants with TBI had a good memory for the traumatic event and 65 had a poor memory. They found that 23% of the participants with a good memory at the initial testing had PTSD but only 6% of the participants with a poor or no memory had PTSD. Caspi, Gil, Ben-Ari, Koren, Aaron-Peretz, and Klein (2005) replicated these findings in a retrospective study, in which participants were interviewed 2.9 years after the injury (range 1 month to 5 years). Based on responses to a memory questionnaire, roughly 40% of their brain injured participants were classified as having good memory for the event and 60% as having a poor or no memory for the traumatic event. Caspi et al. found that 33% of the participants who had a good memory for the event had PTSD but only 8% of their participants who had no or a poor trauma memory had PTSD. In both the prospective and the retrospective study, the probability of having PTSD was roughly four times higher for participants with a good memory for the injury.
If explicit memory of an event were the only cause of PTSD for that event, one would expect no PTSD in the group with poor or no memory in both studies. However, this assumes the memory loss was complete, which is not reported, and that the PTSD was for the initial trauma and not for later events such as regaining consciousness in a hospital or wondering whether they would be rescued. For the prospective study, decreases in retrograde amnesia with time also need to be considered.
Other studies with less extensive testing of the injury-event memory have also found a higher prevalence of PTSD among participants with a traumatic memory for the injury event compared to participants without such memory (Turnbull, Cambell & Swann, 2001; Bombardier et al., 2006, but see Greenspan et al., 2006). Similarly, patients with post traumatic amnesia of greater than one hour have fewer PTSD symptoms than those with shorter post traumatic amnesia, even though we can assume that the traumatic event was more severe among the former (Feinstein, Hershkop, Ouchterlony, Jardine, & McCullagh, 2002).
Organic amnesia for the traumatic event is indicative of severe physical injury. Physical injury is generally an important risk factor for the development of PTSD, as documented by studies on general injuries in motor vehicle accidents (Blanchard, Hickling, Taylor, Loos, Forneris, & Jaccard, 1996; Frommberger, et al., 1998; Urano, et al., 1999) as well as in other domains. Regarded in isolation, this could be taken as evidence for the idea that severe traumatic events cause PTSD, consistent with the DSM model. However, the fact that the event severity does not show this effect in the case of TBI with organic amnesia, indicates that event severity per se though important is not crucial. Event severity may play a role only to the extent that it affects memory. Thus, the findings on organic amnesia in TBI support the central assumption of the mnemonic model that PTSD is caused by having a traumatic memory rather than by having had a traumatic event per se.
Nonetheless, although rare, individuals with TBI who have no explicit trauma memory may get the diagnosis of PTSD (Klein et al, 2003). Several explanations have been suggested, all of them consistent with the mnemonic model (see Harvey et al., 2003, for a review). Notably, some individuals with amnesia for the injury event develop PTSD symptoms in response to pseudo-memories of the trauma. For example, Bryant (1996) reports two case studies of patients who were amnesic for their motor vehicle accidents. Both patients nonetheless had delayed onset PTSD with vivid intrusive images about the accidents, based on information from police reports. In both cases, the person pictured himself at the scene of the accident (e.g., seeing himself bleeding in the front seat of the car) in the intrusive images, which therefore can be considered as an implanted or false memory of the event. Such cases can be seen as a parallel to individuals who develop traumatic flashbacks in response to allegedly implanted memories of child sexual abuse that they later retract (de Rivera, 1997) or people who develop PTSD symptoms after a traumatic memory has been recovered. For instance, McNally, Perlman, Ristuccia, and Clancy (2006) note that when children fail to understand at the time of events that what occurred was childhood sexual abuse and then later remember and reinterpret the events as adults, they are often more traumatized as adults and realizing the severity of what happened to them than they were as children.
Pharmacologically induced amnesia
Following the mnemonic model, a pharmacological intervention that disrupts the consolidation of the traumatic memory immediately after a traumatic event would reduce the level of PTSD by rendering the memory less accessible. If memories are formed by processes in many systems, including emotion, (Rubin, 2006) then the whole memory need not be affected, only component processes or their integration, especially if what is affected is the effects of negative emotions. The consolidation of memories of emotionally stressful events is enhanced by the release of epinephrine. However, this effect may be abolished by the β-adrenergic blocker propranolol (e.g., Cahill, Pham, & Setlow, 2000; see Pitman & Delahanty, 2006, for a review). To examine whether propranolol would also reduce subsequent PTSD symptoms, Pitman et al. (2002) conducted a double blind study with participants recruited from a general hospital emergency room. Within six hours of their traumatic event, they were given propranolol or a placebo and continued this treatment four times daily for ten days. None of the 8 propranolol patients were classified as having physiological responses to script-driven imagery when tested three months after their traumatic event, whereas 8 of 14 placebo patients were. A similar study was conducted by Vaiva et al. (2003). They found significantly lower levels of PTSD symptom severity in individuals treated with propranolol as compared to the controls, when examined two months after their traumatic event, despite the fact that the two groups had experienced equally stressful events. More recently, Brunet, Orr, Tremblay, Robertson, Nader, and Pitman (in press) have demonstrated that propanolol given after memory retrieval during script driven imagery reduced physiological responses during later script driven imagery. The studies reported in this paragraph all have small numbers of participants and are in the early stages of what could be a very exciting area of research, but for our current theoretical purposes, though promising, they must be taken with caution.
Childhood amnesia
An ability to remember personal events is critical for the ability to develop PTSD in response to experiencing traumatic events, according to the mnemonic model. Following this model, we should therefore expect the prevalence of PTSD symptoms among adults for events experienced in childhood to show the same developmental pattern as childhood amnesia. That is, we should expect events experienced during the first three years of life to be rarely associated with later PTSD symptoms (although they may cause other types of emotional problems) and we should expect a steady increase in level of PTSD symptoms up to age 7, after which an asymptote should be reached (Rubin, 2000). Alternatively, it has been suggested that cognitive and emotional factors that may counteract the development of PTSD symptoms become increasingly sophisticated throughout childhood. These include the capability to talk about and thus share the traumatic experiences with others, the ability to control emotions and/or inhibit unwanted thoughts and memories (e.g., see Berntsen & Rubin, 2006c, Salmon & Bryant, 2002; Scheeringa & Zeanah, 2001; Vogel & Vernberg, 1993, for further discussion). Following this line of reasoning, we should expect a reverse developmental pattern.
Berntsen and Rubin (2006c) addressed this issue by examining autobiographical memories and PTSD symptoms as a function of age at the time of the events. They interviewed a large sample of older Danes about memories and PTSD symptoms in relation to events experienced during the German occupation of Denmark in World War II. In a second study, a large sample of younger Danes answered the same questions in relation to self-nominated stressful events sampled from the entire life span. In both studies, a clear pattern was observed with respect to the relation between the development of long-term posttraumatic reactions and age at the time of the traumatic event. For participants who were 7 years or younger at the time of their most traumatic event, positive correlations were found between their age at the time of their most traumatic event and current levels of posttraumatic reactions, vividness of the stressful memories, and how central the traumatic event was seen to be to the person’s life story and identity. For participants who were above age 7 at the time of their most traumatic event, no such relations were found. Thus, as predicted by the mnemonic model, the developmental pattern of PTSD symptoms was parallel to the developmental pattern of childhood amnesia (e.g., Rubin, 2000). These findings largely agree with the few PTSD studies that have examined age-related effects of traumas encountered in early childhood (e.g., Green, Grace & Vary, 1991; Sigal & Weinfeld, 2001; Vogel & Vernberg, 2003). –
Self-relevance memory enhancement
We have reviewed evidence showing, as predicted by the mnemonic model, that PTSD symptoms decrease when availability to the traumatic memory decreases. Here we review evidence showing that PTSD symptoms increase when availability of the traumatic memory increases. According to the mnemonic model there should be a positive correlation between level of PTSD symptoms and the degree to which the traumatic memory is seen as central to the person’s life story and identity and serves as a cognitive reference point for the organization of other experiences (Berntsen & Rubin, 2006a). This prediction is counter to the widespread assumption that PTSD is associated with a trauma memory that is hard to access, because it is poorly integrated into the person’s knowledge of him- or herself and the world (see Dalgleish, 2004, for review). Findings from an accumulating number of studies support the prediction derived from the mnemonic model. Berntsen and Rubin (2006a) introduced the Centrality of Event Scale (CES) measuring the extent to which a traumatic memory forms a central component of personal identity, a turning point in the life story and a reference point for everyday inferences. The CES has consistently shown positive correlations with PTSD severity (r’s ranging from.35 to.51) across a number of studies involving different populations (Berntsen & Rubin, 2006a, 2006c, 2007). This positive relationship persists even when controlling for anxiety, depression, dissociation, and self-consciousness (Berntsen & Rubin, 2007). For a discussion of self-defining autobiographical memories see Conway, Singer, and Tagini (2004).
In general, the results reviewed in this section challenge the DSM – Memory hypothesis and support the hypotheses Mnemonic – Organic Amnesia, Mnemonic – Pharmacologically Induced Amnesia, Mnemonic – Childhood Amnesia, and Mnemonic – Self-Relevance Memory Enhancement. Under all four headings we have shown that level of PTSD symptoms vary in predictable ways with the availability of the traumatic memory. Merely encountering a traumatic event with no subsequent memory for the event is unlikely to generate PTSD symptoms, as shown in the first three sections. The perceived self-relevance of the traumatic memory is positively related to level of PTSD, as reviewed in the last section. Thus, the findings contradict the assumption that event severity is the key causal factor for the development of PTSD and support the central assumption of the mnemonic model that PTSD is causally related to having a traumatic memory.
Discussion
The mnemonic model is able to account for important and reliable findings in research on PTSD that any theory of PTSD should account for but that are inconsistent with the current diagnostic view and that have been partly or completely neglected by most theoretical accounts of the disorder. These findings include the following: Trauma-like events that do not satisfy the A1 criterion and common stressful life events can be followed by PTSD symptoms (the Mnemonic – A1 hypothesis favored over the DSM – A1 hypothesis). Events that are associated with emotions other than the A2 criterion emotions of fear, horror, and helplessness can be followed by PTSD symptoms (the Mnemonic – A2 hypothesis favored over the DSM – A2 hypothesis). Over twice as many women as men develop PTSD after the same traumatic event (supporting the Mnemonic – Gender hypothesis). Neuroticism has large correlations with PTSD (supporting the Mnemonic – Neuroticism hypothesis). The C3 symptom of the diagnosis – the inability to recall an important aspect of the trauma – correlated poorly with other PTSD symptoms (challenging the DSM – C3 hypotheses and supporting the Mnemonic – C3 hypothesis). The most direct evidence for the role of the memory of the stressful event as a causal agent is the observation that eliminating, or enhancing, the memory in various ways changed PTSD symptom severity. Evidence for this claim was reviewed in the Organic Amnesia, Mnemonic – Pharmacologically Induced Amnesia, and Mnemonic – Mnemonic – Childhood Amnesia, Mnemonic – Self-Relevance Memory Enhancement. All of these findings were predicted by the mnemonic model, and most are inconsistent with the DSM model.
In addition, the mnemonic model can identify sources of reconstructive errors and biases that are usually overlooked by PTSD theorists and practitioners who take their starting point in trauma-specific reactions, such as peritraumatic dissociation (supporting the Mnemonic – Memory hypothesis). The identification of such reconstructive memory errors and biases has important practical and theoretical implications. The PTSD diagnosis is based on the patient’s memory for the trauma and peritraumatic emotions, not on independent observations of the traumatic event and independent observations of the patient’s emotional reactions to it at the time of the event, for which reason knowledge of reconstructive memory errors is crucial. Finally, the mnemonic model is consistent with the fact that only a minority of people who experience the same traumatic event develops PTSD. In the following we summarize four specific advantages that the mnemonic model has for the understanding of PTSD under the following headings: 1) Trauma-specific mechanism are not invoked, 2) Providing a framework for understanding individual differences, 3) Providing a testable model, 4) Consistency with practice. We finally discuss some disadvantages that our model has as compared to the current DSM model.
Trauma-specific mechanism are not invoked
A major advantage of a memory-based, rather than event-based, approach is the possibility of making better connections between research on PTSD and basic research on memory and emotion. With the exception of conditioning based models (Foa, et al., 1992; Mineka & Zinbarg, 1996, 2006), most theoretical approaches to PTSD leave PTSD isolated from many fields of research that could add to the understanding of this disorder. The idea that memory, and not the event, should be the center of our understanding of PTSD has led to a view that accounts for more of the existing observations as reviewed here. It also has the potential of developing new testable ideas of PTSD that would enlarge our understanding of this disorder by making connections between specific characteristics of the disorder and findings in basic research on memory and emotion.
Consistent with the mnemonic model, we have shown that memory processes leading to PTSD symptoms are not instigated by a specific class of traumatic events, such as events that satisfy the A1 and A2 criteria. We have argued that many highly negative events may potentially cause such reactions mediated by memory. Although certain classes of negative events are associated with higher risks of PTSD than others, according to our model, it is the way such events are processed and represented in memory that is the central causal mechanism, not the event per se. Our understanding of these processes therefore can draw upon theories of the general interplay between affect and memory instead of referring to hypothetical trauma-specific memory mechanisms, for which there is poor evidence (e.g., Geraerts et al., 2007; Kihlstrom, 2006; Porter & Birt, 2001; Shobe & Kihlstrom, 1997).
Basing our work on general rather than special memory mechanisms led us to reconsider the C3 symptom: the inability to recall an important aspect of the trauma (American Psychiatric Association, 1994, p. 428). We argued, this symptom is counter to what would be expected based on the literature on memory in general and we showed that it was very poorly correlated with the rest of the symptoms, as predicted from the mnemonic model. We also have argued that certain aspects of what is conventionally classified as peritraumatic dissociation are better accounted for in terms of memory distortions reflecting the current level of distress.
In general, there are major advantages of avoiding trauma-specific mechanism. Given a wide range of data to account for, it is easier to falsify mechanisms. If general mechanisms fail to work in the extreme conditions of trauma, then they will have to be modified and trauma research will lead to advances in general theory. In addition, the tendency for the study of PTSD to break off and loose contact with the wealth of data and theory available to it is lessened.
Providing a framework for understanding individual differences
Replacing the central role played by the event per se by the event as reconstructed in memory ascribes an active role to predisposing personality and demographic factors that are likely to influence both the initial perception of the event as well as the event as construed retrospectively in memory. Here, we reviewed the effects of two such variables, namely gender and neuroticism. Both variables were predicted to play a central role. These predictions were made based on reviews of the general literature of emotion and memory in relation to these variables.
Our prediction regarding gender was made in spite of the fact that gender was left out of one of the two major meta-analysis of predisposing factors for PTSD (Ozer et al., 2003) and seen to have minor effects in the other (Brewin et al., 2000). Our prediction regarding neuroticism was made despite the fact that this personality variable was left out of both meta-analyses. In our meta-analysis of gender, we found that women were more than twice as likely than men to develop PTSD in response to the same categories of events. Given this effect of gender and the amount of studies showing it, it is surprising that major theories of PTSD (e.g., Brewin, Dalgleish, & Joseph, 1996; Ehlers & Clark, 2000, for a review see Dalgleish, 2004) have devoted little attention (if any at all) to the fact that women are considerable more at risk for developing this disorder than men. Changing the framework for the understanding of PTSD in the direction that we suggest here can potentially help to remedy this oversight. Likewise, our meta-analysis of neuroticism consistently showed substantial associations between neuroticism and PTSD with an average r of.43 across the included studies. By considering the interplay between neuroticism and memory for affect, our mnemonic model was able to suggest possible explanations of this effect. Other factors that are known to be associated with PTSD, such as lack of social support or lower intelligence, may also be accounted for within our model.
Providing a testable model
As noted in the introduction, a major problem with the DSM model is that it defies testing. A cluster of B, C, D, E, and F symptoms can only be classified as PTSD, if preceded by an event fulfilling the A-criteria. As illustrated by Figure 2, because most research on PTSD have used the official diagnosis to set inclusion and exclusion criteria, B, C, D, E, and F symptoms in response to other stressful events are greatly understudied. The DSM also assumes experiences and emotional reactions at the time of the event to be decisive for the development of the disorder, but the literature is only able to provide indirect testing of this claim in the form a retrospective reports because the event itself is not measured as it occurs.
In contrast, claims made by the mnemonic model are testable. In the introduction, we described six classes of hypotheses for which we have reviewed evidence. The most direct evidence for the mnemonic model was the findings that level of PTSD symptoms vary systematically with the availability of the traumatic memory, as evidenced by studies of organic amnesia in traumatic brain injury, childhood amnesia, pharmacologically induced amnesia and memory enhancement through self-relevance. This research suggests that PTSD is unlikely to occur if the traumatic memory is unavailable. This research also suggests that PTSD-symptoms can occur in response to memory for events that are merely believed to have occurred but (in rare cases) never happened or happened in other ways than remembered (McNally, 2003a, b).
Consistency with practice
Among the advantages of the mnemonic model is its consistency with current practice of diagnosis and therapy. PTSD is diagnosed based on the patient’s memory for the trauma and not on independent observations of the traumatic event and independent observations of the patients emotional reactions to it at the time of the event. Some common therapeutic strategies for treating PTSD include changing the memory of the traumatic event. Often a key interpretation of the event is changed that need not contradict what is believed to actually have happened (Foa, Hearst-Ikeda, & Perry, 1995). Patients may be told that they did not have time to do anything to prevent an accident or that they were too young at the time of the event to be in any way responsible for the actions of an adult. Another more drastic therapeutic strategy is to change the central facts of an intrusive memory to be less stressful in order to alleviate this symptom (Hackmann, 1998; Smucker, Dancu, Foa, E. B., & Niederee, 1995). “The alternative target representations created only have to be positive, highly memorable, and attention-grabbing in the presence of negative cues. They are not required to be more consistent with the facts, more rational, or even physically possible” (Brewin, 2006, p. 777). Thus, a victim of childhood sexual abuse might change his or her memory so that the abuse in the intrusive memory was stopped before it could occur. Unless the memory was thought to have a causal role in maintaining PTSD symptoms, such therapies would make little practical and theoretical sense. Repeated exposure to traumatic memories that allow habituation to emotional reactions, as in script guided imagery, can also been seen as changing memory representations. Thus, clinical practice in relation to PTSD is in better agreement with the mnemonic model than with the DSM model.
Limitations
One important limitation of the mnemonic model of PTSD is that it does not provide an operationalization of PTSD for diagnostic purposes. Our present goal has been to develop a framework for understanding PTSD at a theoretical level. Although this may eventually form the basis for generating diagnostic guidelines, such development is beyond the scope of the present article. We are also aware that a risk of solipsism is inherent to the mnemonic model. By considering the disease only as a product of the current memory (as this memory is shaped by the event and predisposing factors characterizing the person), the model involves no necessary reference to objective events with specified, verifiable characteristics. However, as we have argued, the same problem pertains to the DSM model because the A1 and A2 criteria are assessed on the basis of retrospective memory reports, which reflects the identical subjective reality. One could also argue that removing the A criteria increases the risk for overdiagnosing. However, this potential problem is not limited to the mnemonic model. As pointed out by McNally (2003b), because the DSM-IV criteria also include secondhand exposure to traumatic events, a negotiable range of emotional events may count as traumatic stressors.
Concluding comments
The mnemonic model is a movement away from the toxic event metaphor that currently dominates the DSM. We appreciate the political and practical advantages of this metaphor. However, from a scientific point of view, it seems that progress in PTSD research is now better served by a shift to the framework we propose. Our approach is to view PTSD as an extreme of human memory and emotion that results after a highly negative event. We wish to oppose the tendency to devise theories and explanations that just cover PTSD and in contrast, we include as much knowledge as we can from the study of memory and emotion in general. In short, pursuing the current DSM model of PTSD is less likely to lead to scientific progress in the understanding of human suffering after strongly negative events than rethinking PTSD in terms of the mnemonic model.
Acknowledgments
We wish to thank Amanda Miles, Anne Stærk Jacobsen and Jennifer Labrecque for their help; Jeannie Beckham, Michelle Feldman Dennis, Heather Rice and Tim Strauman for their comments on the manuscript; Bo Sommerlund for statistical consultation; Martin Conway, John Kihlstrom and four anonymous reviewers for helping us to clarify our points and suggesting new tests of our model; and the Danish Research Council for Culture and Communication and National Institute of Mental Health grant R01 MH066079 for funding.
Three studies were listed in Table 3, but not included, in calculating the averages. Two did not report a PTSD measure, but used the IES, which covers a subset of PTSD symptoms. The third (Parslow, Jorm, & Christensen, 2006) reported means on the EPQ-R neuroticism scale (Eysenck, Eysenck, & Barrett, 1985) measured prior to the trauma for the PTSD and non PTSD groups of 6.55 (SD = 3.36) and 4.71 (SD = 3.36), which is a difference of greater than a half standard deviation. About 5% of the sample had PTSD; there were 104 participants in the PTSD group compared to 1,981 in the non-PTSD group. This severely limited the value of r calculated and produced a value that was much lower than the other values obtained. In particular, if the means and standard deviations in the Parslow et al. study did not change but there were only 104 participants in the non-PTSD group, the r would increase to.27, which would be in the range of the other studies.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/rev
Contributor Information
David C. Rubin, Duke University
Dorthe Berntsen, Aarhus University.
Malene Klindt Johansen, Aarhus University.
References
- Abenhaim L, Dab W, Salmi LR. Study of civilian victims of terrorist attacks (France 1982–1987) Journal of Clinical Epidemiology. 1992;45:103–109. doi: 10.1016/0895-4356(92)90002-5. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Andrews B, Brewin CR, Rose S, Kirk M. Predicting PTSD symptoms in victims of violent crime: The role of shame, anger, and childhood abuse. Journal of Abnormal Psychology. 2000;109:69–73. doi: 10.1037//0021-843x.109.1.69. [DOI] [PubMed] [Google Scholar]
- Asmundson GJG, Frombach I, McQuaid J, Pedrelli P, Lenox R, Stein MB. Dimensionality of posttraumatic stress symptoms: A confirmatory factor analysis of DSM-IV symptom clusters and other symptom models. Behaviour Research and Therapy. 2000;38:203–214. doi: 10.1016/s0005-7967(99)00061-3. [DOI] [PubMed] [Google Scholar]
- Asmundson GJG, Wright KD, McCreary DR, Pedlar D. Post-traumatic stress disorder symptoms in United Nations peacekeepers: An examination of factor structure in peacekeepers with and without chronic pain. Cognitive Behaviour Therapy. 2003;32:26–37. doi: 10.1080/16506070310003648. [DOI] [PubMed] [Google Scholar]
- Bartlett FC. Remembering: A study in experimental and social psychology. Cambridge: Cambridge University Press; 1967. Original work published 1932. [Google Scholar]
- Baschnagel JS, O’Connor RM, Colder CR, Hawk LW., Jr Factor structure of posttraumatic stress among Western New York undergraduates following the September 11th terrorist attack on the World Trade Center. Journal of Traumatic Stress. 2005;18:677–684. doi: 10.1002/jts.20076. [DOI] [PubMed] [Google Scholar]
- Basoglu M, Kilic C, Salcioglu E, Livanou M. Prevalence of posttraumatic stress disorder and comorbid depression in earthquake survivors in Turkey: An epidemiological study. Journal of Traumatic Stress. 2004;17:133–141. doi: 10.1023/B:JOTS.0000022619.31615.e8. [DOI] [PubMed] [Google Scholar]
- Basoglu M, Salcioglu E, Livanou M. Traumatic stress responses in earthquake survivors in Turkey. Journal of Traumatic Stress. 2002;15:269–276. doi: 10.1023/A:1016241826589. [DOI] [PubMed] [Google Scholar]
- Bauer PJ, Stennes L, Haight JC. Representation of the inner self in autobiography: Women’s and men’s use of internal states language in personal narratives. Memory. 2003;11:27–42. doi: 10.1080/741938176. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: Relationship to combat exposure, symptom severity, guilt, and interpersonal violence. Journal of Traumatic Stress. 1998;11:777–785. doi: 10.1023/A:1024453618638. [DOI] [PubMed] [Google Scholar]
- Bernat JA, Ronfeldt HM, Calhoun KS, Arias I. Prevalence of traumatic events and peritraumatic predictors of posttraumatic stress symptoms in a nonclinical sample of college students. Journal of Traumatic Stress. 1998;11:645–664. doi: 10.1023/A:1024485130934. [DOI] [PubMed] [Google Scholar]
- Berntsen D. Involuntary autobiographical memories. Applied Cognitive Psychology. 1996;10:435–454. [Google Scholar]
- Berntsen D. Tunnel memories for autobiographical events: Central details are remembered more frequently from shocking than from happy experiences. Memory & Cognition. 2002;30:1010–1020. doi: 10.3758/bf03194319. [DOI] [PubMed] [Google Scholar]
- Berntsen D, Rubin DC. The centrality of event scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behaviour Research and Therapy. 2006a;44:219–231. doi: 10.1016/j.brat.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, Rubin DC. Emotion and vantage point in autobiographical memory. Cognition & Emotion. 2006b;20:1193–1215. [Google Scholar]
- Berntsen D, Rubin DC. Flashbulb memories and posttraumatic stress reactions across the life-span: Age-related effects of the German occupation of Denmark during WWII. Psychology and Aging. 2006c;21:127–139. doi: 10.1037/0882-7974.21.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, Rubin DC. When a Trauma Becomes a Key to Identity: Enhanced Integration of Trauma Memories Predicts Posttraumatic Stress Disorder Symptoms. Applied Cognitive Psychology. 2007;21:417–431. [Google Scholar]
- Berntsen D, Thomsen DK. Personal memories for remote historical events. Accuracy and clarity for flashbulb memories related to WWII. Journal of Experimental Psychology: General. 2005;134:242–257. doi: 10.1037/0096-3445.134.2.242. [DOI] [PubMed] [Google Scholar]
- Berntsen D, Willert M, Rubin DC. Splintered memories or vivid landmarks? Qualities and organization of traumatic memories with and without PTSD. Applied Cognitive Psychology. 2003;17:675–693. [Google Scholar]
- Blackmore S. A psychological theory of out-of-body experiences. Journal of Parapsychology. 1984;48:201–218. [Google Scholar]
- Blackmore S. Where am I?: Perspectives in imagery and the of out-of-body experience. The Journal of Mental Imagery. 1987;11:53–66. [Google Scholar]
- Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Forneris CA, Jaccard J. Who Develops PTSD from Motor Vehicle Accidents. Behaviour Research and Therapy. 1996;34:1–10. doi: 10.1016/0005-7967(95)00058-6. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Kuhn E, Rowell DL, Hickling EJ, Wittrock D, Rogers RL, Johnson MR, Steckler DC. Studies of the vicarious traumatization of college students by the September 11th attacks: Effects of proximity, exposure and connectedness. Behaviour Research and Therapy. 2004;42:191–205. doi: 10.1016/S0005-7967(03)00118-9. [DOI] [PubMed] [Google Scholar]
- Blanke O, Mohr C, Michel CM, Pascual-Leone A, Brugger P, Seeck M, Landis T, Thut G. Linking out-of-body experience and self processing to mental own-body imagery at the temporoparietal junction. The Journal of Neuroscience. 2005;25:550–557. doi: 10.1523/JNEUROSCI.2612-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich A, Gelkopf M, Solomon Z. Exposure to terrorism, stress-related mental health symptoms, and coping behaviors among a nationally representative sample in Isreal. American Medical Association. 2003;290:612–620. doi: 10.1001/jama.290.5.612. [DOI] [PubMed] [Google Scholar]
- Bödvarsdóttir I, Elklit A. Psychological reactions in Icelandic earthquake survivors. Scandinavian Journal of Psychology. 2004;45:3–13. doi: 10.1111/j.1467-9450.2004.00373.x. [DOI] [PubMed] [Google Scholar]
- Bombardier CH, Fann JR, Temkin N, Esselman PC, Pelzer E, Keough M, Dikmen S. Posttraumatic stress disorder symptoms during the first six months after traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences. 2006;18:501–508. doi: 10.1176/jnp.2006.18.4.501. [DOI] [PubMed] [Google Scholar]
- Bowman L. Individual differences in posttraumatic distress: Problems with the DSM-IV model. Canadian Journal of Psychiatry. 1999;44:21–33. doi: 10.1177/070674379904400103. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Greenwald MK, Petry MC, Lang PJ. Remembering pictures: pleasure and arousal in memory. Journal of Experimental Psychology: Learning, Memory, & Cognition. 1992;18:379–390. doi: 10.1037//0278-7393.18.2.379. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Lang PJ. Affective norms for English words (ANEW): Instruction manual and affective ratings. Gainsville, FL: University of Florida, The Center for Research in Psychophysiology; 1999. Tech. Rep. No. C-1. [Google Scholar]
- Brent DA, Perper JA, Moritz G, Liotus LBS, Richardson D, Canobbio RBS, Schweers J, Roth C. Posttraumatic stress disorder in peers of adolescent suicide victims: Predisposing factors and phenomenology. American Academy of Child & Adolescent Psychiatry. 1995;34:209–215. doi: 10.1097/00004583-199502000-00016. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Brewin CR. Understanding Cognitive Behaviour Therapy: A Retrieval Competition Account. Behaviour Research and Therapy. 2006;44:765–784. doi: 10.1016/j.brat.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Rose S. Fear, helplessness, and horror in posttraumatic stress disorder: Investigating DSM-IV criterion A2 in victims of violent crime. Journal of Traumatic Stress. 2000;13:499–509. doi: 10.1023/A:1007741526169. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Dalgleish T, Joseph S. A dual representation theory of posttraumatic stress disorder. Psychological Review. 1996;103:670–686. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003;23:339–376. doi: 10.1016/s0272-7358(03)00033-3. [DOI] [PubMed] [Google Scholar]
- Brodaty H, Joffe C, Luscombe G, Thompson C. Vulnerability to post-traumatic stress disorder and psychological morbidity in aged Holocaust survivors. International Journal of Geriatric Psychiatry. 2004;19:968–979. doi: 10.1002/gps.1195. [DOI] [PubMed] [Google Scholar]
- Brunet A, Orr SP, Tremblay J, Robertson K, Nader K, Pitman RK. Effects of post-retrieval propanolol on psychophysiologic responding during subsequent script driven traumatic imagery in post-traumatic stress disorder. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2007.05.006. in press. [DOI] [PubMed] [Google Scholar]
- Bryant RA. Posttraumatic stress disorder, flashbacks, and pseudomemories in closed head injury. Journal of Traumatic Stress. 1996;9:621–629. doi: 10.1007/BF02103671. [DOI] [PubMed] [Google Scholar]
- Buckley TC, Blanchard EB, Hickling EJ. A confirmatory factor analysis of posttraumatic stress symptoms. Behaviour Research and Therapy. 1998;36:1091–1099. doi: 10.1016/s0005-7967(98)00076-x. [DOI] [PubMed] [Google Scholar]
- Burke A, Heuer F, Reisberg D. Remembering emotional events. Memory and Cognition. 1992;20:277–290. doi: 10.3758/bf03199665. [DOI] [PubMed] [Google Scholar]
- Burstein A. Posttraumatic stress disorder. The Journal of Clinical Psychiatry. 1985;4:300–301. [PubMed] [Google Scholar]
- Cahill L. Sex- and hemisphere-related influences on the neurobiology of emotionally influenced memory. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2003;27:1235–1241. doi: 10.1016/j.pnpbp.2003.09.019. [DOI] [PubMed] [Google Scholar]
- Cahill L, Haier RJ, White NS, Fallon J, Kilpatrick L, Lawrence C, Potkin SG, Alkire MT. Sex-related difference in amygdale activity during emotionally influenced memory storage. Neurobiology of Learning and Memory. 2001;75:1–9. doi: 10.1006/nlme.2000.3999. [DOI] [PubMed] [Google Scholar]
- Cahill L, Pham CA, Setlow B. Impaired memory consolidation in rats produced by β-adrenergic blockade. Neurobiology of Learning and Memory. 2000;74:259–266. doi: 10.1006/nlme.1999.3950. [DOI] [PubMed] [Google Scholar]
- Cahill L, Uncapher M, Kilpatrick L, Alkire MT, Turner J. Sex-related hemispheric lateralization of amygdale function in emotionally influenced memory: An fMRI investigation. Learning & Memory. 2004;11:261–266. doi: 10.1101/lm.70504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldera T, Palma L, Penayo U, Kullgren G. Psychological impact of the Hurricane Mitch in Nicaragua in a one-year perspective. Social Psychiatry and Psychiatric Epidemiology. 2001;36:108–114. doi: 10.1007/s001270050298. [DOI] [PubMed] [Google Scholar]
- Candel I, Merckelbach H. Peritraumatic dissociation as a predictor of post-traumatic stress disorder: A critical review. Comprehensive Psychiatry. 2003;45:44–55. doi: 10.1016/j.comppsych.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Caspi Y, Gil S, Ben-Ari IZ, Koren D, Aaron-Peretz J, Klein E. Memory of the traumatic event is associated with increased risk for PTSD: A retrospective study of patients with traumatic brain injury. Journal of Loss and Trauma. 2005;10:319–336. [Google Scholar]
- Casella L, Motta RW. Comparison of characteristics of Vietnam veterans with and without posttraumatic stress disorder. Psychological Reports. 1990;67:595–605. doi: 10.2466/pr0.1990.67.2.595. [DOI] [PubMed] [Google Scholar]
- Chang CM, Connor KM, Lai TJ, Lee LC, Davidson JRT. Predictors of posttraumatic outcomes following the 1999 Taiwan earthquake. Journal of Nervous and Mental Disease. 2005;193:40–46. doi: 10.1097/01.nmd.0000149217.67211.ab. [DOI] [PubMed] [Google Scholar]
- Christianson S-Å. Emotional stress and eyewitness memory: A critical review. Psychological Bulletin. 1992;112:284–309. doi: 10.1037/0033-2909.112.2.284. [DOI] [PubMed] [Google Scholar]
- Christianson S-Å, Loftus EF. Remembering emotional events: The fate of detailed information. Cognition and Emotion. 1991;5:81–108. [Google Scholar]
- Christianson S-Å, Loftus EF. Some characteristics of people’s traumatic memories. Bulletin of the Psychonomic Society. 1990;28:195–198. [Google Scholar]
- Christianson S-Å, Loftus EF, Hoffmann H, Loftus GR. Eye fixation and memory for emotional events. Journal of Experimental Psychology: Learning, Memory and Cognition. 1991;17:693–701. doi: 10.1037//0278-7393.17.4.693. [DOI] [PubMed] [Google Scholar]
- Christianson S-Å, Safer MA. Emotional events and emotions in autobiographical memories. In: Rubin DC, editor. Remembering our past: Studies in autobiographical memory. Cambridge UK: Cambridge University Press; 1996. pp. 218–243. [Google Scholar]
- Chung MC, Dennis I, Easthope Y, Werrett J, Farmer S. A multiple-indicator multiple-cause model for posttraumatic stress reactions: Personality, coping, and maladjustment. Psychosomatic Medicine. 2005;67:251–259. doi: 10.1097/01.psy.0000155675.56550.5f. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: Challenges to the current system and future directions. Annual Review of Psychology. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- Conway MA. Memory and the self. Journal of Memory and Language. 2005;53:594–628. [Google Scholar]
- Conway MA, Pleydell-Pearce CW. The construction of autobiographical memories in the self-memory system. Psychological Review. 2000;107:261–288. doi: 10.1037/0033-295x.107.2.261. [DOI] [PubMed] [Google Scholar]
- Conway MA, Singer JA, Tagini A. The self and autobiographical memory: Correspondence and coherence. Social Cognition. 2004;22:491–529. [Google Scholar]
- Cordova MJ, Studts JL, Hann DM, Jacobsen PB, Andrykowski MA. Symptom structure of PTSD following breast cancer. Journal of Traumatic Stress. 2000;13:301–319. doi: 10.1023/A:1007762812848. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI): Professional manual. Odessa, Fl: Psychological Assessment Resources; 1992. [Google Scholar]
- Costa PT, Jr, Terracciano A, McCrae RR. Gender differences in personality traits across cultures: robust and surprising findings. Journal of Personality and Social Psychology. 2001;81:332–331. doi: 10.1037/0022-3514.81.2.322. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Clara IP, Enns MW. Posttraumatic stress disorder and the structure of common mental disorders. Depression and Anxiety. 2002;15:168–171. doi: 10.1002/da.10052. [DOI] [PubMed] [Google Scholar]
- Dalgleish T. Cognitive approaches to posttraumatic stress disorder: The evolution of multirepresentational theorizing. Psychological Bulletin. 2004;130:228–260. doi: 10.1037/0033-2909.130.2.228. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Book SW, Colket JT, Tupler LA, Roth S, David D, Hertzberg M, Mellman T, Beckham JC, Smith RD, Davison RM, Katz R, Feldman ME. Assessment of a new self-rating scale for posttraumatic stress disorder. Psychological Medicine. 1997;27:153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Davidson J, Kudler H, Smith R. Personality in chronic post-traumatic stress disorder: A study of the Eysenck inventory. Journal of Anxiety Disorders. 1987;1:295–300. [Google Scholar]
- Davis PJ. Gender differences in autobiographical memory for childhood emotional experiences. Journal of Personality and Social Psychology. 1999;76:498–510. doi: 10.1037//0022-3514.76.3.498. [DOI] [PubMed] [Google Scholar]
- DeLisi LE, Maurizio A, Yost M, Papparozzi CF, Fulchino C, Katz CL, Altesman J, Biel M, Lee J, Stevens P. A survey of New Yorkers after the Sept. 11, 2001, terrorist attacks. American Journal of Psychiatry. 2003;160:780–783. doi: 10.1176/appi.ajp.160.4.780. [DOI] [PubMed] [Google Scholar]
- de Rivera J. The construction of false memory syndrome: The experience of retractors. Psychological Inquiry. 1997;8:271–292. [Google Scholar]
- Difede J, Barocas D. Acute instrusive and avoidant PTSD symptoms as predictors of chronic PTSD following burn injury. Journal of Traumatic Stress. 1999;12:363–369. doi: 10.1023/A:1024788812393. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychological Bulletin. 2006;132:477–495. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuHamel KN, Ostroff J, Ashman T, Winkel G, Mundy EA, Keane TM, Morasco BJ, Vickberg SMJ, Hurley K, Burkhalter J, Chhabra R, Scigliano E, Papadopoulos E, Moskowitz C, Redd W. Construct validity of the Posttraumatic Stress Disorder Checklist in cancer survivors: Analyses based on two samples. Psychological Assessment. 2004;16:255–266. doi: 10.1037/1040-3590.16.3.255. [DOI] [PubMed] [Google Scholar]
- Egloff B, Schmukle SC. Gender differences in implicit and explicit anxiety measures. Personality and Individual Differences. 2004;36:1807–1815. [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology. 1998;10:508–519. doi: 10.1037//0021-843x.107.3.508. [DOI] [PubMed] [Google Scholar]
- Ekman P. Are there basic emotions? Psychological Review. 1992;99:550–553. doi: 10.1037/0033-295x.99.3.550. [DOI] [PubMed] [Google Scholar]
- Elklit A, O’Connor M. Post-traumatic stress disorder in a Danish population of elderly bereaved. Scandinavian Journal of Psychology. 2005;46:439–445. doi: 10.1111/j.1467-9450.2005.00475.x. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, Kindt M. The relationship between neuroticism, pre-traumatic stress and post-traumatic stress: A prospective study. Personality and Individual Differences. 2003;35:381–388. [Google Scholar]
- Epstein R, Fullerton C, Ursano R. Posttraumatic stress disorder following an air disaster: A prospective study. American Journal of Psychiatry. 1998;155:934–938. doi: 10.1176/ajp.155.7.934. [DOI] [PubMed] [Google Scholar]
- Eysenck SBG, Eysenck HJ, Barrett P. A revised version of the psychoticism scale. Personality and Individual Differences. 1985;6:21–29. [Google Scholar]
- Fauerbach JA, Lawrence JW, Schmidt CW, Munster AM, Costa PT. Personality predictors of injury-related posttraumatic stress disorder. Journal of Nervous and Mental Disease. 2000;188:510–517. doi: 10.1097/00005053-200008000-00006. [DOI] [PubMed] [Google Scholar]
- Feinstein A, Hershkop S, Ouchterlony D, Jardine A, McCullagh S. Posttraumatic amnesia and recall of a traumatic event following traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences. 2002;14:25–30. doi: 10.1176/jnp.14.1.25. [DOI] [PubMed] [Google Scholar]
- Fivush R. Gendered narratives: Elaboration, structure and emotion in parent-child reminiscing across the preschool years. In: Thompson CP, Herrmann DJ, Bruce D, Read JD, Payne DG, editors. Autobiographical memory: Theoretical and applied perspectives. Mahwah, NJ: Lawrence Erlbaum Associates Inc; 1998. pp. 79–103. [Google Scholar]
- Fleiss JL. Measures of effect size for categorical data. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage Foundation; 1994. pp. 245–260. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Hearst-Ikeda D, Perry K. Evaluation of a brief cognitive-behavioral program for the prevention of chronic PTSD in recent assault victims. Journal of Clinical and Consulting Psychology. 1995;63:948–955. doi: 10.1037//0022-006x.63.6.948. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Riggs DS, Gershuny BS. Arousal, numbing, and intrusion: Symptom structure of PTSD following assault. American Journal of Psychiatry. 1995;152:116–120. doi: 10.1176/ajp.152.1.116. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive behavioral therapy for PTSD. NewYork: Guilford Press; 1998. [Google Scholar]
- Foa EB, Zinbarg RE, Olasov-Rothbaum B. Uncontrollability and unpredictability in post-traumatic stress disorder: an animal model. Psychological Bulletin. 1992;112:218–238. doi: 10.1037/0033-2909.112.2.218. [DOI] [PubMed] [Google Scholar]
- Freedman SA, Gluck N, Tuval-Mashiach R, Brandes D, Peri T, Shalev AY. Gender differences in responses to traumatic events: A prospective study. Journal of Traumatic Stress. 2002;15:407–413. doi: 10.1023/A:1020189425935. [DOI] [PubMed] [Google Scholar]
- Freud S. Screen memories. In: Strachey J, editor. Sigmund Freud: Collected papers. Vol. 6. London: Hogarth Press; 18991953. pp. 43–63. [Google Scholar]
- Freud S. The Standard Edition of the Complete Psychological Works of Sigmund Freud. Vol. 6. London: The Hogarth Press; 19011960. The psychopathology of everyday life. [Google Scholar]
- Frommberger UH, Stieglitz RD, Nyberg E, Schlickewei W, Kuner E, Berger M. Prediction of posttraumatic stress disorder by immediate reaction to trauma: A prospective study in road traffic accident victims. European Archives of Psychiatry and Clinical Neuroscience. 1998;248:316–321. doi: 10.1007/s004060050057. [DOI] [PubMed] [Google Scholar]
- Fullerton CS, Ursano RJ, Wang L. Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. American Journal of Psychiatry. 2004;161:1370–1376. doi: 10.1176/appi.ajp.161.8.1370. [DOI] [PubMed] [Google Scholar]
- Geraerts E, Kozaric-Kovacic D, Merckelbach H, Peraica T, Jelicic M, Candel I. Traumatic memories of veterans: Not so special after all. Consciousness and Cognition. doi: 10.1016/j.concog.2006.02.005. in press. [DOI] [PubMed] [Google Scholar]
- Gil S, Caspi Y, Ben-Ari IZ, Klein E. Memory of the traumatic event as a risk factor for the development of PTSD: Lessons from the study of traumatic brain injury. CNS Spectrums. 2006;11:603–607. doi: 10.1017/s1092852900013651. [DOI] [PubMed] [Google Scholar]
- Gil S, Caspi Y, Ben-Ari IZ, Koren D, Klein E. Does memory of a traumatic event increase the risk for Posttraumatic Stress Disorder in patients with traumatic brain injury? A prospective study. American Journal of Psychiatry. 2005;162:963–969. doi: 10.1176/appi.ajp.162.5.963. [DOI] [PubMed] [Google Scholar]
- Green B, Korol M, Grace MC, Vary MG. Children and disaster. Age, gender, and parental effects on PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:945–951. doi: 10.1097/00004583-199111000-00012. [DOI] [PubMed] [Google Scholar]
- Green BL, Lindy JD, Grace MC, Gleser GC, Leonard AC, Korol M, Winget C. Buffalo Creek survivors in the second decade: Stability of stress symptoms. American Journal of Orthopsychiatry. 1990;60:43–54. doi: 10.1037/h0079168. [DOI] [PubMed] [Google Scholar]
- Greenspan AI, Stringer AY, Phillips VL, Hammond FM, Goldstein F. Symptoms of post-traumatic stress: Intrusion and avoidance 6 and 12 months after TBI. Brain Injury. 2006;20:733–742. doi: 10.1080/02699050600773276. [DOI] [PubMed] [Google Scholar]
- Greenwald AG. The totalitarian ego: Fabrication and revision of personal history. American Psychologist. 1980;35:603–618. [Google Scholar]
- Grey N, Holmes E, Brewin CR. Peritraumatic emotional “hot spots” in memory. Behavioural and Cognitive Psychotherapy. 2001;29:367–372. [Google Scholar]
- Hackmann A. Working with images in clinical psychology. In: Bellack AS, Hersen M, editors. Comprehensive clinical psychology. Vol. 6. New York: Elsevier; 1998. pp. 301–318. [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Brewin CR, Jones C, Kopelman MD. Coexistence of posttraumatic stress disorder and traumatic brain injury: Towards a resolution of the paradox. Journal of the International Neuropsychological Society. 2003;9:663–676. doi: 10.1017/S1355617703940069. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Robins LN, McEvoy L. Posttraumatic stress disorder in the general population: Findings of the Epidemiologic Catchment Area Survey. New England Journal of Medicine. 1987;317:1630–1634. doi: 10.1056/NEJM198712243172604. [DOI] [PubMed] [Google Scholar]
- Herlihy J, Scragg P, Turner S. Discrepancies in autobiographical memories--Implications for the assessment of asylum seekers: Repeated interviews study. British Medical Journal. 2002;324:324–327. doi: 10.1136/bmj.324.7333.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herlitz A, Nilsson LG, Backman L. Gender differences in episodic memory. Memory & Cognition. 1997;25:801–811. doi: 10.3758/bf03211324. [DOI] [PubMed] [Google Scholar]
- Holeva V, Tarrier N. Personality and peritraumatic dissociation in the prediction of PTSD in victims of road vehicle accidents. Journal of Psychosomatic Research. 2001;51:687–692. doi: 10.1016/s0022-3999(01)00256-2. [DOI] [PubMed] [Google Scholar]
- Howell HB, Castle DJ, Yonkers KA. Anxiety disorders in women. In: Castle DJ, Kulkami J, Abel KM, editors. Mood and anxiety disorders in women. New York: Cambridge University Press; 2006. pp. 59–74. [Google Scholar]
- Hunter JE, Schmidt FL. Dichotomization of continuous variables: The implications for meta-analysis. Journal of Applied Psychology. 1990;75:334–349. [Google Scholar]
- Hyer L, Braswell L, Albrecht B, Boyd S, Boudewyns P, Talbert S. Relationship of NEO-PI to personality styles and severity of trauma in chronic PTSD victims. Journal of Clinical Psychology. 1994;50:699–707. doi: 10.1002/1097-4679(199409)50:5<699::aid-jclp2270500505>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Ironson G, Wynings C, Schneiderman N, Baum A, Rodriguez M, Grennwood D, Benight C, Antoni M, LaPerriere A, Huang HS, Klimas N, Fletcher MA. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosomatic Medicine. 1997;59:128–141. doi: 10.1097/00006842-199703000-00003. [DOI] [PubMed] [Google Scholar]
- Izard CE. Basic emotions, relations among emotions, and emotion – cognition relations. Psychological Review. 1992;99:561–565. doi: 10.1037/0033-295x.99.3.561. [DOI] [PubMed] [Google Scholar]
- James W. The principles of psychology. 1–2. New York: Henry Holt and Co; 1890. [Google Scholar]
- Jehel L, Paterniti S, Brunet A, Duchet C, Guelfi JD. Prediction of the occurrence and intensity of post-traumatic stress disorder in victims 32 months after bomb attack. European Psychiatry. 2003;18:172–176. doi: 10.1016/s0924-9338(03)00043-9. [DOI] [PubMed] [Google Scholar]
- Kelly B, Raphael B, Judd F, Kernutt G, Burnett P, Burrows G. Posttraumatic stress disorder in response to HIV infection. General Hospital Psychiatry. 1998;20:345–352. doi: 10.1016/s0163-8343(98)00042-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kihlstrom JF. Trauma and memory revisited. In: Uttl B, Ohta N, Siegenthaler AL, editors. Memory and emotion. Interdisciplinary perspectives. Malden, MA: Blachwell; 2006. pp. 259–291. [Google Scholar]
- Kilic C, Ulusoy M. Psychological effects of the November 1999 earthquake in Turkey: An epidemiological study. Acta Psychiatrica Scandinavica. 2003;108:232–238. doi: 10.1034/j.1600-0447.2003.00119.x. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick P, Roth S, Van der Kolk B. Posttraumatic stress disorder field trial: Evaluation of the PTSD construct – Criteria A through E. In: Widiger TA, Frances AJ, Pincus HA, Ross R, First MB, Davis W, Kline M, editors. DSM-IV Sourcebook. Vol. 4. Washington, DC: American Psychiatric Association; 1998. pp. 803–846. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Klein E, Caspi Y, Gil S. The relation between memory for the traumatic event and PTSD. Evidence from studies of traumatic brain injury. 2003;48:28–33. doi: 10.1177/070674370304800106. [DOI] [PubMed] [Google Scholar]
- Kuehner C. Gender differences in unipolar depression: An update of epidemiological findings and possible explanations. Acta Psychiatrica Scandinavica. 2003;108:163–174. doi: 10.1034/j.1600-0447.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Ribi K, Laimbacher J, Vollrath M, Gnehm HE, Sennhauser FH. Brief report: Posttraumatic stress disorder in parents of children with newly diagnosed Type 1 diabetes. Journal of Pediatric Psychology. 2002;27:647–652. doi: 10.1093/jpepsy/27.7.647. [DOI] [PubMed] [Google Scholar]
- Lauterbach D, Vrana S. The relationship among personality variables, exposure to traumatic events, and severity of posttraumatic stress symptoms. Journal of Traumatic Stress. 2001;14(1):29–45. [Google Scholar]
- Levine LJ. Reconstructing memory for emotions. Journal of Experimental Psychology, General. 1997;126:165–177. [Google Scholar]
- Levine LJ, Pizarro DA. Emotion and memory research: A grumpy overview. Social Cognition. 2004;22:530–554. [Google Scholar]
- Levine LJ, Safer MA. Sources of bias in memory for emotions. Current Directions in Psychological Science. 2002;11:169–173. [Google Scholar]
- Lewin TJ, Carr VJ, Webster RA. Recovery from post-earthquake psychological morbidity: Who suffers and who recovers? Australian and New Zealand Journal of Psychiatry. 1998;32:15–20. doi: 10.3109/00048679809062701. [DOI] [PubMed] [Google Scholar]
- Livanou M, Basoglu M, Salcioglu E, Kalender D. Traumatic stress responses in treatment-seeking earthquake survivors in Turkey. The Journal of Nervous and Mental Disease. 2002;190:816–823. doi: 10.1097/01.NMD.0000041958.58852.1D. [DOI] [PubMed] [Google Scholar]
- Madakasira S, O’Brien KF. Acute posttraumatic stress disorder in victims of a natural disaster. Journal of Nervous and Mental Disease. 1987;175:286–290. doi: 10.1097/00005053-198705000-00008. [DOI] [PubMed] [Google Scholar]
- Maes M, Delmeire L, Schotte C, Janca A, Creten T, Mylle J, Struyf A, Pison G, Rousseeuw PJ. Epidemiologic and phenomenological aspects of post-traumatic stress disorder: DSM-III-R diagnosis and diagnostic criteria not validated. Psychiatry Research. 1998a;81:179–193. doi: 10.1016/s0165-1781(98)00095-x. [DOI] [PubMed] [Google Scholar]
- Maes M, Delmeire L, Schotte C, Janca A, Creten T, Mylle J, Struyf A, Pison G, Rousseeuw PJ. The two-factorial symptom structure of post-traumatic stress disorder: Depression—avoidance and arousal—anxiety. Psychiatry Research. 1998b;81:195–210. doi: 10.1016/s0165-1781(98)00094-8. [DOI] [PubMed] [Google Scholar]
- Martin M. Neuroticism as a predictor toward depression: A cognitive mechanism. Personality and Individual Differences. 1985;6:353–365. [Google Scholar]
- McFarlane AC. The aetiology of post-traumatic stress disorders following a natural disaster. British Journal of Psychiatry. 1988;152:116–121. doi: 10.1192/bjp.152.1.116. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology. 2003a;54:229–252. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Remembering trauma. Cambridge: Harvard University Press; 2003b. [Google Scholar]
- McNally RJ, Perlman CA, Ristuccia CS, Clancy SA. Clinical characteristics of adults reporting repressed, recovered, or continuous memories of childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2006;74:237–242. doi: 10.1037/0022-006X.74.2.237. [DOI] [PubMed] [Google Scholar]
- McNamara P, Benson E, McGeeney B, Brown A, Albert ML. Modes of remembering in patients with chronic pain: Relation to current pain. The Journal of Nervous and Mental Diseases. 2005;193:53–57. doi: 10.1097/01.nmd.0000149219.04841.f5. [DOI] [PubMed] [Google Scholar]
- Merckelbach H, Dekkers T, Wessel I, Roefs A. Amnesia, flashbacks, nightmares, and dissociation in aging concentration camp survivors. Behavior Research and Therapy. 2003a;41:351–360. doi: 10.1016/s0005-7967(02)00019-0. [DOI] [PubMed] [Google Scholar]
- Merckelbach H, Dekkers T, Wessel I, Roefs A. Dissociative symptoms and amnesia in Dutch concentration camp survivors. Comprehensive Psychiatry. 2003b;44:65–69. doi: 10.1053/comp.2003.50011. [DOI] [PubMed] [Google Scholar]
- Mikkelsen EG, Einarsen S. Basic assumptions and symptoms of post-traumatic stress among victims of bullying at work. European Journal of Work and Organizational Psychology. 2002;11:87–111. [Google Scholar]
- Mineka S, Zinbarg R. Conditioning and ethological models of anxiety disorders: Stress-in-Dynamic-Context Anxiety models. In: Hope DA, editor. Nebraska Symposium on Motivation, 1995: Perspectives on anxiety, panic, and fear. Lincoln, NE: University of Nebraska Press; 1996. pp. 135–210. [PubMed] [Google Scholar]
- Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. 2006 doi: 10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- Mol SSL, Arntz A, Metsemakers JFM, Dinant GJ, Vilters-Van Montfort PAP, Knottnerus JA. Symptoms of post-traumatic stress disorder after non-traumatic events: Evidence from an open population study. British Journal of Psychiatry. 2005;186:494–499. doi: 10.1192/bjp.186.6.494. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Braun T, Tillery L, Cain KC, Johnson LC, Beaton RD. PTSD among bereaved parents following the violent deaths of their 12- to 28-year-old children: A longitudinal prospective analysis. Journal of Traumatic Stress. 1999;12:273–291. doi: 10.1023/A:1024724425597. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Johnson LC, Lohan J. The aftermath of the violent death of a child: An integration of the assessments of parents’ mental disorders and PTSD during the first 5 years of bereavement. Journal of Loss and Trauma. 2002;7:203–222. [Google Scholar]
- Neisser U. Cognitive psychology. New York: Appleton-Century-Crofts; 1967. [Google Scholar]
- Nelson K, Fivush R. The emergence of autobiographical memory. A social cultural developmental theory. Psychological Review. 2004;111:486–511. doi: 10.1037/0033-295X.111.2.486. [DOI] [PubMed] [Google Scholar]
- Nigro G, Neisser U. Point of view in personal memories. Cognitive Psychology. 1983;15:467–482. [Google Scholar]
- Norris FH, Perilla JL, Ibañez GE, Murphy AD. Sex differences in symptoms of posttraumatic stress: Does culture play a role? Journal of Traumatic Stress. 2001;14:7–27. [Google Scholar]
- North CS, Pfefferbaum B, Narayanan P, Thielman S, McCoy G, Dumont C, Kawasaki A, Ryosho N, Kim YS, Spitznagel EL. Comparison of post-disaster psychiatric disorders after terrorist bombings in Nairobi and Oklahoma City. British Journal of Psychiatry. 2005;186:487–493. doi: 10.1192/bjp.186.6.487. [DOI] [PubMed] [Google Scholar]
- North CS, Smith EM, Spitznagel EL. Posttraumatic stress disorder in survivors of a mass shooting. American Journal of Psychiatry. 1994;151:82–88. doi: 10.1176/ajp.151.1.82. [DOI] [PubMed] [Google Scholar]
- Olley BO, Zeier MD, Seedat S, Stein DJ. Post-traumatic stress disorder among recently diagnosed patients with HIV/AIDS in South Africa. AIDS Care. 2005;17:550–557. doi: 10.1080/09540120412331319741. [DOI] [PubMed] [Google Scholar]
- Ortony Andrew, Turner Terence J. What’s basic about basic emotions? Psychological Review. 1990;97:315–331. doi: 10.1037/0033-295x.97.3.315. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Weiss DS. Who develops posttraumatic stress disorder? Current Directions in Psychological Science. 2004;13:169–172. [Google Scholar]
- Palmer SC, Kagee A, Coyne JC, DeMichele A. Experience of trauma, distress, and posttraumatic stress disorder among breast cancer patients. Psychosomatic Medicine. 2004;66:258–264. doi: 10.1097/01.psy.0000116755.71033.10. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Fitzgerald LF. Confirmatory analysis of posttraumatic stress symptoms in sexually harassed women. Journal of Traumatic Stress. 2005;18:657–666. doi: 10.1002/jts.20074. [DOI] [PubMed] [Google Scholar]
- Parker RS. Recommendations for the revision of DSM-IV diagnostic categories for co-morbid posttraumatic stress disorder and traumatic brain injury. NeuroHabilitation. 2002;17:131–143. [PubMed] [Google Scholar]
- Parslow RA, Jorm AF, Christensen H. Associations of pre-trauma attributes and trama exposure with screening positive for PTSD: Analysis of a community-based study of 2085 young adults. Psychological Medicine. 2006;36:387–395. doi: 10.1017/S0033291705006306. [DOI] [PubMed] [Google Scholar]
- Pathé M, Mullen PE. The impact of stalkers on their victims. British Journal of Psychiatry. 1997;170:12–17. doi: 10.1192/bjp.170.1.12. [DOI] [PubMed] [Google Scholar]
- Pillemer DB, Wink P, DiDonato TE, Sanborn RL. Gender differences in autobiographical memory styles of older adults. Memory. 2003;11:525–532. doi: 10.1080/09658210244000117. [DOI] [PubMed] [Google Scholar]
- Porter S, Birt AR. Is traumatic memory special? A comparison of traumatic memory characteristics with memory for other emotional life experiences. Applied Cognitive Psychology. 2001;15:101–118. [Google Scholar]
- Porter S, Peace KA. The scars of memory. A prospective, longitudinal investigation of the consistency of traumatic and positive emotional memories in adulthood. Psychological Science. 2007;18:435–441. doi: 10.1111/j.1467-9280.2007.01918.x. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Delahanty DL. Conceptually driven pharmacologic approaches to acute trauma. CNS Spectrums. The international Journal of Neuropsychiatric medicine. 2005;10:99–106. doi: 10.1017/s109285290001943x. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Sanders KM, Zusman RM, Healy AR, Cheema F, Lasko NB, Cahill L, Orr SP. Pilot study of secondary prevention of posttraumatic stress disorder with Propranolol. Biological Psychiatry. 2002;51:189–192. doi: 10.1016/s0006-3223(01)01279-3. [DOI] [PubMed] [Google Scholar]
- Power M, Dalgleish T. Cognition and emotion: From order to disorder. Hove: Psychology Press; 1997. [Google Scholar]
- Pulcino T, Galea S, Ahern J, Resnick H, Foley M, Vlahov D. Posttraumatic stress in women after the September 11 terrorist attacks in New York City. Journal of Women’s Health. 2003;12:809–820. doi: 10.1089/154099903322447774. [DOI] [PubMed] [Google Scholar]
- Qin J, Mitchell KJ, Johnson MK, Krystal JH, Southwick SM, Rasmusson AM, Allen ES. Reactions to and memories for the September 11 terrorist attack in adults with posttraumatic stress disorder. Applied Cognitive Psychology. 2003;17:1081–1097. [Google Scholar]
- Rice HJ, Talarico JM, Rubin DC. Images of the past: An examination of visual perspective use during autobiographical memory retrieval. Poster session presented at the annual meeting of the North Carolina Cognition Group; Winston-Salem, NC. 2005. Feb, [Google Scholar]
- Riggs DS, Dancu CV, Gershuny BS, Greenberg D, Foa E. Anger and post-traumatic stress disorder in female crime victims. Journal of Traumatic Stress. 1992;5:613–625. [Google Scholar]
- Ritchie TD, Skowronski JJ, Wood SE, Walker WR, Vogl RJ, Gibbons JA. Event self-importance, event rehearsal, and the fading affect bias in autobiographical memory. Self and identity. 2006;5:172–195. [Google Scholar]
- Robins LN, Helzer JE, Croughan J. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Robinson JA, Swanson KL. Field and observer modes of remembering. Memory. 1993;1:169–184. doi: 10.1080/09658219308258230. [DOI] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, Ehlich PJ, Friedman MJ. Increases in retrospective accounts of war-zone exposure over time: The role of PTSD symptom severity. Journal of Traumatic Stress. 1998;11:597–605. doi: 10.1023/A:1024469116047. [DOI] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM, Borkovec TD, Litz BT. Emotional response at the time of a potentially traumatizing event and PTSD symptomatology: A preliminary retrospective analysis of the DSM-IV criterion A-2. Journal of Behavior Therapy. 1998;29:123–130. doi: 10.1016/s0005-7916(98)00007-x. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York: Russell Sage Foundation; 1994. pp. 231–244. [Google Scholar]
- Rubin DC. Memory in oral traditions: The cognitive psychology of epic, ballads, and counting-out rhymes. New York: Oxford University Press; 1995. [Google Scholar]
- Rubin DC. The distribution of early childhood memories. Memory. 2000;8:265–269. doi: 10.1080/096582100406810. [DOI] [PubMed] [Google Scholar]
- Rubin DC. A basic-systems approach to autobiographical memory. Current Directions in Psychological Science. 2005;14:79–83. doi: 10.1177/0963721416631955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC. The Basic-Systems Model of Episodic Memory. Perspectives on Psychological Science. 2006;1:277–311. doi: 10.1111/j.1745-6916.2006.00017.x. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Burt CDB, Fifield SJ. Experimental manipulations of the phenomenology of memory. Memory & Cognition. 2003;31:877–886. doi: 10.3758/bf03196442. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Feldman ME, Beckham JC. Reliving, emotions, and fragmentation in the autobiographical memories of veterans diagnosed with PTSD. Applied Cognitive Psychology. 2003;18:17–35. [Google Scholar]
- Rubin DC, Schulkind MD, Rahhal TA. A study of gender differences in autobiographical memory: Broken down by age and sex. Journal of Adult Development. 1997;6:61–71. [Google Scholar]
- Rubin DC, Siegler IC. Facets of personality and the phenomenology of autobiographical memory. Applied Cognitive Psychology. 2004;18:913–930. [Google Scholar]
- Russell JA. A circumplex model of affect. Journal of Personality & Social Psychology. 1980;39:1161–1178. [Google Scholar]
- Russell JA, Carroll JM. On the bipolarity of positive and negative affect. Psychological Bulletin. 1999;125:3–30. doi: 10.1037/0033-2909.125.1.3. [DOI] [PubMed] [Google Scholar]
- Safer MA, Christianson S-Å, Autry MW, Österlund K. Tunnel memory for traumatic events. Applied Cognitive Psychology. 1998;12:99–117. [Google Scholar]
- Salcioglu E, Basoglu M, Livanou M. Long-term psychological outcome for non-treatment-seeking earthquake survivors in Turkey. The Journal of Nervous and Mental Disease. 2003;191:154–160. doi: 10.1097/01.NMD.0000054931.12291.50. [DOI] [PubMed] [Google Scholar]
- Salmon K, Bryant RA. Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review. 2002;22:163–188. doi: 10.1016/s0272-7358(01)00086-1. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH. A relational perspective on PTSD in early childhood. Journal of Traumatic Stress. 2001;14:779–815. doi: 10.1023/A:1013002507972. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Stein BD, Jaycox LH, Collins RL, Marshall GN, Elliot MN, Zhou AJ, Kanouse DE, Morrison JL, Berry SH. A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine. 2001;345:1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- Schwarz ED, Kowalski JM, McNally RJ. Malignant memories: Post-traumatic changes in memory in adults after a school shooting. Journal of Traumatic Stress. 1993;6:545–553. [Google Scholar]
- Scott MJ, Stradling SG. Post-traumatic stress disorder without the trauma. British Journal of Clinical Psychology. 1994;33:71–74. doi: 10.1111/j.2044-8260.1994.tb01095.x. [DOI] [PubMed] [Google Scholar]
- Seidlitz L, Diener E. Sex differences in the recall of affective experiences. Journal of Personality and Social Psychology. 1998;74:262–271. doi: 10.1037//0022-3514.74.1.262. [DOI] [PubMed] [Google Scholar]
- Sembi S, Tarrier N, O’Neill P, Burns A, Faragher B. Does post-traumatic stress disorder occur after stroke: A preliminary study. International Journal of Geriatric Psychiatry. 1998;13:315–322. doi: 10.1002/(sici)1099-1166(199805)13:5<315::aid-gps766>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Shelby RA, Golden-Kreutz DM, Andersen BL. Mismatch of posttraumatic stress disorder (PTSD) symptoms and DSM-IV symptom clusters in a cancer sample: Exploratory factor analysis of the PTSD Checklist-Civilian Version. Journal of Traumatic Stress. 2005;18:347–357. doi: 10.1002/jts.20033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shobe KK, Kihlstrom JF. Is traumatic memory special? Current Directions in Psychological Science. 1997;3:70–74. [Google Scholar]
- Sigal JJ, Weinfeld M. Do children cope better than adults with potentially traumatic stress? A 40-year follow-up of Holocaust survivors. Psychiatry: Interpersonal & Biological Processes. 2001;64:69–80. doi: 10.1521/psyc.64.1.69.18236. [DOI] [PubMed] [Google Scholar]
- Silver SM, Iacono CU. Factor-analytic support for DSM-III’s post-traumatic stress disorder for Vietnam veterans. Journal of Clinical Psychology. 1984;40:5–14. doi: 10.1002/1097-4679(198401)40:1<5::aid-jclp2270400102>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Smeets RM, Smeets RMR, Dingemans PMAJ. Composite International Diagnostic Interview, Version 1.1, Interviewers Version, Dutch translation. World Health Organization; Geneva: 1993. [Google Scholar]
- Smith MY, Redd W, DuHamel K, Vickberg SJ, Ricketts P. Validation of the PTSD Checklist-Civilian Version in survivors of bone marrow transplantation. Journal of Traumatic Stress. 1999;12:485–499. doi: 10.1023/A:1024719104351. [DOI] [PubMed] [Google Scholar]
- Smucker MR, Dancu C, Foa EB, Niederee JL. Imagery rescripting: A new treatment for survivors of childhood sexual abuse suffering from posttraumatic stress. Journal of Cognitive Psychotherapy. 1995;9:3–17. [Google Scholar]
- Solomon SD, Canino GJ. Appropiateness of DSM-III-R criteria for posttraumatic stress disorder. Comprehensive Psychiatry. 1990;31:227–237. doi: 10.1016/0010-440x(90)90006-e. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Morgan A, Nicolaou AL, Charney DS. Consistency of memory for combat-related traumatic events in veterans of Operation Desert Storm. American Journal of Psychiatry. 1997;154:173–177. doi: 10.1176/ajp.154.2.173. [DOI] [PubMed] [Google Scholar]
- Spitzer R, Williams J, Gibbon M. Structured Clinical Interview for DSM-III-R, Version NP-V. NY: New York State Psychiatric Institute, Biometrics Research Department; 1987. [Google Scholar]
- Steblay NM. A meta-analytic review of the weapon focus effect. Law & Human Behavior. 1992;16:413–424. [Google Scholar]
- Steinglass P, Gerrity E. Natural disasters and post-traumatic stress disorder: Short-term versus long-term recovery in two disaster-affected communities. Journal of Applied Social Psychology. 1990;20:1746–1765. [Google Scholar]
- Stewart SH, Conrod PJ, Pihl RO, Dongier M. Relations between posttraumatic stress symptoms dimensions and substance dependence in a community-recruited sample of substance-abusing women. Psychology of Addictive Behaviors. 1999;13:78–88. [Google Scholar]
- Street AE, Arias I. Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims. 2001;16:65–78. [PubMed] [Google Scholar]
- Stukas AA, Dew MA, Switzer GE, DiMartini A, Kormos RL, Griffith BP. PTSD in heart transplant recipients and their family caregivers. Journal of Consultation Liaison Psychiatry. 1999;40:212–221. doi: 10.1016/s0033-3182(99)71237-5. [DOI] [PubMed] [Google Scholar]
- Summerfield D. A critique of seven assumptions behind psychological trauma programmes in war-affected areas. Social Science & Medicine. 1999;48:1449–1462. doi: 10.1016/s0277-9536(98)00450-x. [DOI] [PubMed] [Google Scholar]
- Summerfield D. The invention of post-traumatic stress disorder and the social usefulness of a psychiatric category. British Medical Journal. 2001;322:95–98. doi: 10.1136/bmj.322.7278.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talarico JM, LaBar KS, Rubin DC. Emotional intensity predicts autobiographical memory experience. Memory & Cognition. 2004;32:1118–1132. doi: 10.3758/bf03196886. [DOI] [PubMed] [Google Scholar]
- Talarico JM, Rubin DC. Confidence, not consistency, characterizes flashbulb memories. Psychological Science. 2003;14:455–461. doi: 10.1111/1467-9280.02453. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Green HAC. Ruminative self-focus and autobiographical memory. Personality and Individual Differences. 2004;36:1933–1943. [Google Scholar]
- Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Social Psychiatry and Psychiatric Epidemiology. 2005;40:672–679. doi: 10.1007/s00127-005-0943-9. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in truama and postruamatic stress disorder: A quantitiative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tucker P, Pfefferbaum B, Nixon SJ, Dickson W. Predictors of post-traumatic stress symptoms in Oklahoma City: Exposure, social support, peri-traumatic responses. The Journal of Behavioral Health Services and Research. 2000;27:406–416. doi: 10.1007/BF02287822. [DOI] [PubMed] [Google Scholar]
- Turnbull SJ, Campbell EA, Swann IJ. Post-traumatic stress disorder symptoms following a head injury: Does amnesia for the event influence the development of symptoms? Brain Injury. 2001;15:775–785. doi: 10.1080/02699050110034334. [DOI] [PubMed] [Google Scholar]
- Ursano RJ, Fullerton CS, Epstein RS, Crowley B, Kao TC, Vance K, Craig KJ, Dougall AL, Baum A. Acute and chronic posttraumatic stress disorder in motor vehicle accident victims. American Journal of Psychiatry. 1999;156:589–595. doi: 10.1176/ajp.156.4.589. [DOI] [PubMed] [Google Scholar]
- Vaiva G, Ducrocq F, Jezequel K, Averland B, Lestavel P, Brunet A, Marmar CR. Immediate treatment with propranolol decreases posttraumatic stress disorder two months after trauma. Biological Psychiatry. 2003;54:947–949. doi: 10.1016/s0006-3223(03)00412-8. [DOI] [PubMed] [Google Scholar]
- Van der Hart O, van der Kolk BA, Boon S. Treatment of dissociative disorders. In: Bremner JD, Marmar CR, editors. Trauma, memory and dissociation. Washington, DC: American Psychiatric Press; 1998. pp. 253–283. [Google Scholar]
- Van Giezen AE, Arensman E, Spinhoven P, Wolters G. Consistency of memory for emotionally arousing events. Clinical Psychology Review. 2005;25:935–953. doi: 10.1016/j.cpr.2005.04.011. [DOI] [PubMed] [Google Scholar]
- Van Loey NEE, Maas CJM, Faber AW, Taal LA. Predictors of chronic posttraumatic stress symptoms following burn injury: Results of a longitudinal study. Journal of Traumatic Stress. 2003;16:361–369. doi: 10.1023/A:1024465902416. [DOI] [PubMed] [Google Scholar]
- Ventureyra VG, Yao S-N, Cottraux J, Note I, De Mey-Guillard C. The validation of the Posttraumatic Stress Disorder Checklist Scale in posttraumatic stress disorder and nonclinical subjects. Psychotherapy and Psychosomatics. 2002;71:47–53. doi: 10.1159/000049343. [DOI] [PubMed] [Google Scholar]
- Verger P, Dab W, Lamping DL, Loze JY, Deschaseaux-Voinet C, Abenhaim L, Rouillon F. The psychological impact of terrorism: An epidemiologic study of posttraumatic stress disorder and associated factors in victims of the 1995–1996 bombings in France. American Journal of Psychiatry. 2004;161:1384–1389. doi: 10.1176/appi.ajp.161.8.1384. [DOI] [PubMed] [Google Scholar]
- Vogel JM, Vernberg EM. Part I: Children’s psychological responses to disasters. Journal of Clinical Child Psychology. 1993;22:464–484. [Google Scholar]
- Walker WR, Skowronski JJ, Gibbons JA, Vogl RJ, Thompson CP. On the emotions that accompany autobiographical memories: Dysphoria disrupts the fading affect bias. Cognition and Emotion. 2003;17:703–723. [Google Scholar]
- Walker RW, Vogl RJ, Thompson CP. Autobiographical memory: Unpleasantness fades faster than pleasantness over time. Applied Cognitive Psychology. 1997;11:399–413. [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Watson D, Tellegen A. Toward a consensual structure of mood. Psychological Bulletin. 1985;98:219–235. doi: 10.1037//0033-2909.98.2.219. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, Keane TM. The PTSD Checklist (PCL) 1994 Unpublished scale available from the National Center for PTSD. [Google Scholar]
- Weisæth L. The European history of psychotraumatology. Journal of Traumatic Stress. 2002;15:443–452. doi: 10.1023/A:1020909620364. [DOI] [PubMed] [Google Scholar]
- Wessel I, Merckelbach H. Characteristics of traumatic memories in normal subjects. Behavioural & Cognitive Psychotherapy. 1994;22:315–324. [Google Scholar]
- Williams JMG. Depression and the specificity of autobiographical memory. In: Rubin DC, editor. Remembering our past: Studies in autobiographical memory. Cambridge: Cambridge University Press; 1996. pp. 244–267. [Google Scholar]
- Wolfe J, Erickson DJ, Sharkansky EJ, King DW, King LA. Course and predictors of posttraumatic stress disorder among Gulf War Veterans: A prospective analysis. Journal of Consulting and Clinical Psychology. 1999;67:520–528. doi: 10.1037//0022-006x.67.4.520. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic criteria for research. Geneva: World Health Organization; 1992. [Google Scholar]
- Yang YK, Yeh TL, Chen CC, Lee CK, Lee IH, Lee LC, Jeffries KJ. Psychiatric morbidity and posttraumatic symptoms among earthquake victims in primary care clinics. General Hospital Psychiatry. 2003;25:253–261. doi: 10.1016/s0163-8343(03)00022-7. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Southwick SM, Giller EL. Exposure to atrocities and severity of chronic posttraumatic stress disorder in Vietnam combat veterans. American Journal of Psychiatry. 1992;149:333–336. doi: 10.1176/ajp.149.3.333. [DOI] [PubMed] [Google Scholar]
- Young A. The harmony of illusions: Inventing Post-Traumatic Stress Disorder. Princeton: Princeton University Press; 1995. [Google Scholar]
- Yuille JC, Cutshall JL. A case study of eyewitness memory of a crime. Journal of Applied Psychology. 1986;71:291–301. [PubMed] [Google Scholar]