Abstract
Objective
To review the clinical presentation and CT and MRI findings in patients with high clinical suspicion of non-accidental trauma (NAT); to examine associations between imaging findings and neurological long-term outcome in abused children.
Patients and Methods
A retrospective review of 57 cases of non-accidental trauma (NAT) from a single institution was performed. Neuroimaging studies (CT and MRI) were reviewed by a senior neuroradiologist, a neuroradiology fellow and a radiology resident. Clinical history and physical findings including retinal examination, imaging and follow-up assessment documents were reviewed.
Results
Mean time between arrival that CT and MRI imaging was 2.9 hours and 40.6 hours respectively. The most common clinical presentation (47%) was mental status changes. The most common neuroimaging finding was subdural hemorrhage, seen in 86% of patients. In 47 cases in which both MRI and CT was performed, there was one case of suspected non-accidental trauma missed on head CT. CT detected signs of global ischemia in all 11 of the patients that died (CT mean time performed after arrival = 1.1 hours). MRI detected additional signs of injury in patients who ended up with mild to moderate developmental delay.
Conclusion
CT was able to detect evidence of non-accidental head injury in 56 out of 57 abused children included in our cohort and predicted severe neurological injury and mortality. MRI was useful in detecting additional evidence of trauma which can be helpful in risk stratification for neurological outcomes as well as providing confirming evidence of repeated injury.
Keywords: Non-accidental trauma, neuroimaging, CT, MRI, developmental outcomes
Introduction
Head injury is the most common cause of death in abused children under the age of two. Incidence of inflicted traumatic brain injury in the United States is estimated to be 17 per 100,000 person-years, with males more frequently affected than females.1,2 Shaken baby syndrome or non-accidental trauma (NAT) is characterized by a combination of intracranial injuries, retinal hemorrhages and bone fractures.3 Because the child’s head-to-torso ratio is much higher than that of an adult, angular biomechanical forces, which cause acceleration-deceleration, are magnified in the pediatric head trauma.5 Apnea with resultant hypoxia may result from diffuse brainstem injury further magnifying the insult.6 Secondary brain injury can occur causing diffuse swelling and loss of cerebral blood flow autoregulation creating further hypoxic damage. In many children, the brain injury is likely multifactorial and includes shaking, impact, and hypoxic ischemic damage, in part related to delay in seeking medical care.
The initial clinical presentation of abusive head trauma can be highly variable and includes irritability, vomiting, apnea, seizures and obtundation.7,8 The history provided by the parents or caregivers is often vague and changes with time.9 Some typical examples include: choking with feeding, fall from height, sibling induced injury, and cyanosis. Physical exam can be useful, especially as far as detection of bruising, fractures and retinal hemorrhages, but does not always indicate the possibility or extent of intracranial injury.10 Radiology can play an important role in the detection of non-accidental head injury itself as well as provide confirming additional evidence of extracranial NAT (classic metaphyseal lesions, posterior rib fractures, scapular fractures, etc.)11
The combination of history, physical exam and radiologic findings is therefore crucial in raising the possibility and establishing the diagnosis of non-accidental head injury. Neuroimaging evaluation in the setting of NAT usually consists of head computed tomography (CT) and increasingly, brain magnetic resonance imaging (MRI). These different modalities can provide complimentary information in establishing the diagnosis of non-accidental head injury. Although there have been reports of head CT and brain MRI findings in the context of NAT, findings of CT and MR examinations in the same set of NAT patients have not, to our knowledge, been reported in the literature. Furthermore, there have been no reports investigating the association of neuroimaging findings and long term clinical outcomes in the setting of non-accidental head injury.
The aim of our study was two-fold:
Retrospective review of clinical presentation and spectrum of imaging findings on CT and MRI in a cohort of 57 patients with high clinical suspicion for NAT.
Investigation of associations between CT and MRI findings and long-term clinical outcome in these patients.
Patients and Methods
After obtaining Institutional Review Board approval, we reviewed the medical and radiologic records of 57 patients investigated for suspected non-accidental head injury over the past 13 years. Cases of suspected non-accidental head injury were identified through a review of Child Abuse Review Committee case lists, log books and interesting case books. All of these cases were evaluated by the “Child Protection Team” at our institution. The preponderance of evidence and final disposition strongly supported that the cranial injuries of this cohort of 57 patients were secondary to abuse. Equivocal cases and cases in which alternative diagnoses were made or entertained were excluded. All patients underwent neuroimaging studies and skeletal surveys. Ophthalmologic exam was documented in all but 4 patients. Only patients with imaging evidence of head injury including skull fractures were included. Patients presenting with other isolated axial or isolated appendicular injuries were excluded.
Neuroimaging studies (CT and MRI) were reviewed by a senior neuroradiologist (PCS), a neuroradiology fellow (MP) and a radiology resident (BRF) in a consensus fashion. To limit bias towards the opinion of the more senior reader, the junior members of the team were asked to express an opinion first. CT images were specifically examined for skull fractures, intracranial hemorrhage, extra-axial fluid collections and loss of gray white matter differentiation. MRI images were specifically examined for intracranial hemorrhage, extra-axial fluid collections, blood of different ages, restricted diffusion and edema.
The noncontrast CT protocol was performed in axial mode with 2 second gantry rotation time and gantry tilt parallel to nasion and occipital condyles. Kvp = 120, mA = 140, and DFOV = 15 cm. All CT scans performed with soft tissue algorithm reconstructions, slice thickness of 5 mm, as well as bone algorithm reconstructions, slice thickness of 2.5 mm. Patients were imaged on a 1.5T MR unit (GE Healthcare, Milwaukee, Wis). Thirty-eight of the 48 patients who had MRI examinations presented between 2001–2007 and underwent a standard pediatric protocol brain MR examination before and after administration of intravenous contrast (Magnevist; Bayer HealthCare Pharmaceuticals, Wayne, NJ), which included the following sequences: axial and sagittal T1 (spin-echo [SE] TR/TE 470/12); axial T2 (fast spin-echo TR/TE 3000–5000/100); axial fluid-attenuated inversion recovery (T2-weighted, TR/TE 11000/140); axial diffusion-weighted (SE-echo-planar imaging b-value 0–1000 directions 9); and axial, coronal, and sagittal postcontrast T1 SE. The slice thickness is for the MR sequences was 5 mm with a gap of 0.5 mm. Prior to 2001, the remaining 10 patients had axial and sagittal T1 weighted imaging, axial T2 weighted imaging and axial, coronal, and sagittal postcontrast T1 SE with similar parameters as listed above but without a DWI sequence. Pertinent extracranial imaging reports such as skeletal surveys or abdominal CT’s, performed during the NAT workup were also reviewed. These were specifically scrutinized for posterior rib fractures, metaphyseal extremity fractures and solid organ injuries; any other significant findings were also noted.
Presenting history as provided by the caretaker and physical exam findings were noted. Mortality rates during initial hospitalization were also recorded. Medical records were reviewed to determine long term outcome of patients. Thirty-nine of the surviving 46 patients had followup visits with either neurology or neurosurgery with documentation of the patient’s interval neurologic development and physical examination. Mildly impaired patients had some learning delays and/or mild tone or strength abnormality but were ambulatory. Moderately impaired patients had severe cognitive learning disabilities requiring special educational needs and/or significant motor impairment. Severely impaired children were unable to learn and were nonambulatory with severe cerebral palsy. Associations between neuroimaging findings and long term outcome categories were also examined.
Results
A total of 57 children were identified with a high clinical suspicion of non-accidental head injury between 1994 and 2007 at our institution. Ages varied from 0.5 months weeks to 39 months, with a mean age of 8.5 months. A total of 37 males and 20 females were included in this cohort. Twenty-five (47%) of the patients presented with mental status changes, 17 (32%) of the patients presented with respiratory distress, 10 (19%) of the patients presented with seizures with the remaining 5 patients (9%) presenting with fall.
CT findings
Fifty-six of the 57 patients underwent head CT as part of their initial work-up. Forty-eight of the patients had a head CT on initial presentation. The remaining eight patients underwent head CT between 10 to 48 hours following presentation (mean = 20.6 hours). The remaining one child was admitted for further workup after having dedicated outpatient knee plain film radiographs taken which revealed metaphyseal bucket handle fractures of the left distal femur and proximal tibia following a reported fall. Skeletal survey revealed a parietal skull fracture. As the patient was neurologically asymptomatic, the patient went straight to MRI which confirmed the skull fracture but was otherwise negative.
CT imaging revealed the presence of subdural hematomas in 49 patients, ischemic injury in 17 patients, subarachnoid hemorrhage in 12 patients and parenchymal hemorrhage in 3 patients. Skull fractures were encountered in 15/56 patients (27%), a similar percentage to previously reported data.8,12,13 Twelve of the 49 subdural hematomas had associated skull fractures. Out of the 12 patients with subarachnoid hemorrhage, 10 also had subdural hemorrhages. Eleven of these 12 patients had evidence of retinal hemorrhage; the twelfth patient died from diffuse anoxic injury before a retinal exam could be performed. All 11 patients who died had CT evidence of global ischemic injury (average mean time between arrival and performance of head CT was 1.1 hours). Five of these 11 patients presented with mental status changes and 6 patients presented with respiratory distress. One patient had signs of diffuse axonal injury.
MR findings
Forty-eight of the 57 patients had brain MRI examinations. Average mean time between patient arriving at the hospital and MRI examination was 40.6 hours (range = 8 to 240 hours). Of the 9 patients that did not undergo MRI, 4 of the patients were unstable and died; the remaining 5 patients that only had CT examinations presented prior to the year 2000, reflecting differences in referral pattern and/or availability of MRI. Subdural hemorrhage was detected in 44 of the 48 patients with 12 of these presenting with blood products of different ages. Fifteen of the patients had evidence of ischemia and 8 patients had subarachnoid hemorrhage. Three patients had intraparenchymal hemorrhage with another four patients exhibiting evidence of diffuse axonal injury. All 4 patients with DAI had accompanying subdural hemorrhages. Three of the 4 patients with DAI also had subarachnoid hemorrhage.
Combined CT & MRI Findings
Forty-seven of the patients underwent both CT and MRI examinations with the results shown in Table 1.
Table 1.
Neuroimaging Findings in 47 Patients
| Findings | CT | MRI |
|---|---|---|
| Hemorrhage | ||
| SDH | 44 | 44 |
| SAH | 8 | 8 |
| Parenchymal | 3 | 3 |
| Repeated hemorrhage | - | 12 |
| Ischemia | 12 | 15 |
| DAI | 1 | 4 |
In the patients undergoing both CT and MRI, both modalities detected the same number of subdural, subarachnoid and parenchymal hemorrhages. In 12/40 patients with subdural hematomas undergoing MRI, hemorrhage of different ages was detected, strengthening the case for non-accidental head trauma. MRI detected additional findings of NAT not seen on CT in 6 patients including 3 cases of DAI and 3 cases of ischemia. Figure 1 demonstrates one of the cases in which ischemia remained occult on the initial head CT but was detected on the diffusion weighted imaging.
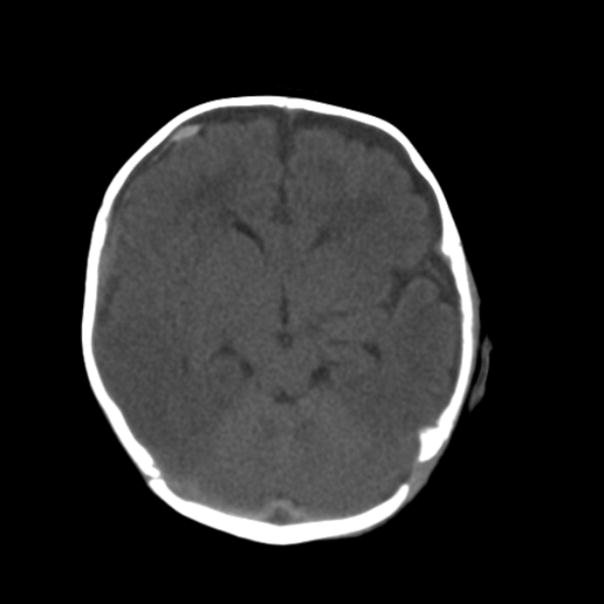
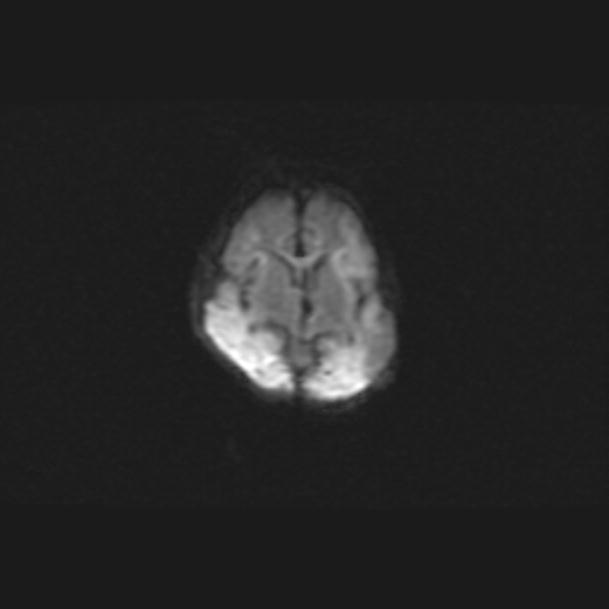
Figure 1.
Figure 1A. Noncontrast head CT in a child with high clinical suspicion of child abuse shows right frontal subdural hematoma but no evidence of ischemia. Figure 1B. Diffusion weighted MR sequence (ADC maps showed corresponding low signal) in the same patient demonstrates ischemia in bilateral parietal lobes not detected on the initial head CT.
Extracranial Findings
Retinal hemorrhages were detected in 45/53 patients which is in accordance with previously published data.8,12,13 The skeletal survey was positive for fractures in 31 out of the 57 patients (54%). Extracranial radiologic findings included rib fractures (8 patients), other skeletal fractures (10 patients) or a combination of both rib and extremity fractures (2 patients) which is similar to previously reported data.8 In seven patients (12%) with imaging evidence of intracranial injury, the skeletal survey and retinal exam was negative; these results are consistent with previously reported findings.14
Long-term Outcomes
Of the 46 surviving patients, 7 were lost to long-term followup. Long term follow up information was available on the remaining 39 patients, with length of follow up ranging from 1 to 129 months (mean = 28.2 months). Seventeen patients (34%) had normal development, 17 patients (34%) had mild to moderate impairment, 5 patients (10%) had severe impairment and 11 patients (22%) died.
In the 17 patients with normal development, neuroimaging findings at time of diagnosis included 2 isolated skull fractures, 13 subdural hematomas, 1 contusion injury and 1 subdural hemorrhage with associated DAI. In the group of 17 patients with mild to moderate neurological impairment, there were 15 patients with subdural hemorrhage: 4 of these patients also had subarachnoid hemorrhage, three had evidence of ischemia, and one had a parenchymal contusion. In the remaining 2 patients, one had parenchymal bleed and the other subarachnoid hemorrhage and contusion injury. In the five patients with severe impairment, 4 demonstrated signs of ischemia and one had an extensive hemorrhagic contusion.
Out of the 4 patients with evidence of DAI on diffusion weighted images one was lost to follow-up, one died, and one was noted to have moderate developmental delay on follow-up with a right sided hemiparesis. The fourth patient with DAI and subdural hemorrhage had no definite neurologic sequelae at 4 months post injury, at which point the patient was 5 months old; the patient was lost to follow up after this point, limiting definitive evaluation for neurological outcome.
Discussion
Noncontrast CT of the head is usually the initial radiologic examination of suspected acute non-accidental head trauma. The head CT also often precedes other investigative techniques for NAT and is relatively accessible and quick to perform. CT is very sensitive in detecting skull fractures as well as blood and can also assess for brain edema and ischemic changes.
Hemorrhage in the setting of non-accidental head trauma can be extra-cerebral such as a subdural hematoma or subarachnoid hemorrhage. True epidural hematomas are uncommon and are usually associated with skull fractures. Subdural hematomas result from injury to the bridging cortical veins and are often located in the interhemispheric fissure or infratentorially. Intra-axial cerebral hemorrhages are often associated with diffuse axonal shearing injuries and often located at grey/white matter interfaces or in white matter tracts such as the corpus callosum. A typical finding of global ischemia is the diffuse loss of grey-white matter differentiation with decreased attenuation in the cortex. The “reversal sign” refers to the relative sparing of thalami, basal ganglia, cerebellum and brainstem, which therefore appears bright.
In our series of patients, CT was important not only in identifying the possibility of NAT but also detecting evidence of ischemia in patients with poor prognosis. All 11 patients who died had imaging signs of global ischemia on CT. Five of the surviving patients had severe developmental delay as well as severe hemiparesis (1) and quadriparesis (4); all five had evidence of complicated CNS injury on CT including focal ischemia (2), global ischemia (2) or extensive hemorrhagic contusions (1).
Our results indicate that CT is quite robust both in terms of raising the clinical suspicion and/or confirming the clinical diagnosis of non-accidental head trauma. Our findings also suggest that CT as a stand alone test can predict poor prognosis in terms of death and severe neurologic sequelae in the more severely injured patients. However, MRI can still be useful in these patients by detecting blood products of different ages and and suggesting signs of repetitive inflicted trauma; these findings were present in 12 of the 44 patients who presented with subdural hematomas.
In our series of patients, CT missed injury in one patient out of 57 seen on the MRI exam performed two weeks later which demonstrated bilateral subacute parenchymal hematomas. MRI was able to detect parenchymal injuries in 6 patients not seen on CT including DAI and smaller areas of focal ischemia/brain edema not seen on CT. These findings were more commonly seen in children who ended up with mild to moderate developmental delay indicating that these additional MRI findings may have prognostic importance. Interestingly CT, which is generally considered less sensitive than MR for detecting extra-axial fluid collections, did not miss any of the subdural hematomas in this study which may in part be due to heightened scrutiny by the imaging readers.
MR imaging is always indicated when non-accidental intracranial trauma is suspected and the head CT is negative as MRI can detect the more subtle signs of child abuse such as DAI15,16,17. The MR imaging protocol should include T2-weighted images, FLAIR images, gradient-echo images, T1-weighted spin echo images in different planes and diffusion weighted images. Substances which alter susceptibility, such as hemosiderin, are easily detected on gradient-echo images and this sequence is therefore helpful in detecting older shear injuries and small petechial hemorrhages. FLAIR imaging can be helpful in detecting subarachnoid hemorrhage. Diffusion weighted imaging (DWI) is helpful in acutely assessing the presence and extent of early ischemic injury, as well as foci of diffuse axonal injury.
This study demonstrates that MRI is helpful in detecting additional findings in the subsection of patients that ended up with mild to moderate developmental delay. Out of the 15 children with mild to moderate developmental delay, 13 had both CT and MR. Additional imaging findings were present on the MRI examination in 5 of the 13 patients including parenchymal contusion (2), ischemia (2) and parenchymal hemorrhage (1).
In the setting of suspected non-accidental head trauma, skeletal survey and dilated retinal examination should be performed as they may provide crucial confirming evidence for NAT which was certainly the case in our population with 45 of 53 patients demonstrating retinal hemorrhages and 31 of the 57 patients exhibiting skeletal fractures. The presence and degree of retinal hemorrhage is predictive of underlying neurologic injury.18,19 Different theories for retinal hemorrhages have been proposed including increase in ocular pressure secondary to increases in either intracranial pressure or intrathoracic pressure, direct damage to the retina caused by shaking and tracking of subdural or subarachnoid blood through the optic sheath.12 However, it is important to note that retinal hemorrhages are not specific and must be placed in the context of the clinical history; differential includes neonatal birth trauma, motor vehicle accidents, leukemia, infection and blood disorders.20
Our study has a number of strengths. The 57 patients reviewed is one of the larger groups of patients evaluated with suspected NAT. Furthermore, our institutions’ guidelines for investigation of suspected child abuse including skeletal surveys in all patients and retinal exams in all but 5 patients offers a comprehensive data base of both clinical data and radiologic findings. Eighty-two percent of the patients underwent both CT and MRI allowing comparison of the two modalities which is the highest in the published literature.
Patient selection in this study is somewhat biased and reflects the institution’s referral pattern as a tertiary care center in the fields of trauma, neonatology, pediatric neurology and neurosurgery. The fact that the institution is located in a college town of modest size as opposed to a large city also introduces a level of bias in population selection, but may result in higher rates of long term follow-up which provides important information when investigating prognostic indicators. One inherent weakness of the study is its retrospective nature which might have resulted in incomplete identification of patients as no inclusive registry was maintained during the time period studied. The neurological outcome assessment of the cohort is not standardized using specific clinical criteria and the time periods of follow-up varied. Although a prospective study with set follow-up times would allow for a more thorough evaluation of the relationship between radiologic findings and clinical outcome, we believe that our reported cohort provides important information regarding the utility of neuroimaging techniques in the assessment of patients suspected of non-accidental trauma.
Conclusion
Non-accidental head trauma must always be suspected in a child presenting with an incoherent clinical history, abnormal head imaging or additional physical findings particularly since the presenting complaints are usually nonspecific. The most common clinical presentation in our population was mental status changes seen in 47% of the patients followed by respiratory distress seen in 32% of the patients. The most common radiologic finding was subdural hematoma found in 49 of the 57 patients followed by ischemia seen in 20 of the 57 patients. CT is the initial method of choice for the work-up of suspected child abuse and is extremely useful for the detection of inflicted intracranial injuries with few critical findings missed in our population. In addition, CT was useful in predicting poor prognosis and outcomes in patients with severe neurological injury from nonaccidental head injury. In the setting of suspected child abuse, MRI should be performed as an adjunct to CT and is particularly useful in detecting the possibility of blood products of different ages further increasing diagnostic certainty of child abuse. MRI was also helpful in detecting additional evidence of injury including small areas of ischemia and diffuse axonal injury which were not evident on CT and may provide additional prognostic information for less severely injured children.
References
- 1.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten MD, Sinal MD. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290:621–626. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 2.Perez-Arjona E, Dujovny M, Viñas F, Park HK, Lizarraga S, Park T, Diaz FG. CNS child abuse: epidemiology and prevention. Neurol Res. 2002;24:29–40. doi: 10.1179/016164102101199512. [DOI] [PubMed] [Google Scholar]
- 3.Caffey J. The whiplash shaken infant syndrome: manual shaking by the extremity with whiplash-induced intracranial and intraocular bleeding, linked with residual permanent brain damage and mental retardation. Pediatrics. 1974;54:396–403. [PubMed] [Google Scholar]
- 4.David TJ. Shaken baby (shaken impact) syndrome: non-accidental head injury in infancy. J R Soc Med. 1999;92(11):556–61. doi: 10.1177/014107689909201105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dias MS. Traumatic brain and spinal cord injury. Pediatric Clinics of North America. 2004;51(2):271–303. doi: 10.1016/S0031-3955(03)00211-6. [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal I. Shaken baby syndrome. Postgrad Med J. 2002;78:732–735. doi: 10.1136/pmj.78.926.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haviland J, Russell RI. Outcome after severe non-accidental head injury. Arch Dis Childhood. 1997;77:504–507. doi: 10.1136/adc.77.6.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King WJ, MacKay M, Sirnick A. Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. CMAJ. 2003;168:155–159. [PMC free article] [PubMed] [Google Scholar]
- 9.Gerber P, Coffman K. Nonaccidental head trauma in infants. Childs Nerv Syst. 2007;23:499–507. doi: 10.1007/s00381-006-0267-4. [DOI] [PubMed] [Google Scholar]
- 10.Rubin DM, Christian CW, Bilaniuk LT, Zazyczny A, Durbin DR. Occult head injury in high-risk abused children. Pediatrics. 2003;111:1382–1386. doi: 10.1542/peds.111.6.1382. [DOI] [PubMed] [Google Scholar]
- 11.Kleinman PK. Diagnostic Imaging of Child Abuse. 2. Mosby; 1998. pp. 290–298. [Google Scholar]
- 12.Morad Y, Kim YM, Armstrong DC, Huyer D, Mian M, Levin AV. Correlation between retinal abnormalities and intracranial abnormalities in the shaken baby syndrome. American Journal of Opthalmology. 2002;134:354–359. doi: 10.1016/s0002-9394(02)01628-8. [DOI] [PubMed] [Google Scholar]
- 13.Datta S, Stoodley N, Jayawant S, Renowden S, Kemp A. Neuroradiological aspects of subdural haemorrhages. Arch Dis Child. 2005;90:947–951. doi: 10.1136/adc.2002.021154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laskey AL, Holsti M, Runyan DK, Socolar RS. Occult head trauma in young suspected victims of physical abuse. J Pediatr. 2004;144:719–722. doi: 10.1016/j.jpeds.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 15.Jaspan T, Griffiths PD, McConachie NS, Pung JAG. Neuroimaging for non-accidental head injury in childhood: a proposed protocol. Clinical Radiology. 2003;58:44–53. doi: 10.1053/crad.2002.1094. [DOI] [PubMed] [Google Scholar]
- 16.Liu AY, Maldjian JA, Bagley LJ, Sinson GP, Grossman RI. Traumatic brain injury: diffusion weighted MR imaging findings. AJNR. 1999;20:1636–1641. [PMC free article] [PubMed] [Google Scholar]
- 17.Biousse V, Suh DY, Newman NJ, Davis PC, Mapstone T, Lambert SR. Diffusion-weighted magnetic resonance imaging in shaken baby syndrome. Am J of Ophthalmol. 2002;133:249–255. doi: 10.1016/s0002-9394(01)01366-6. [DOI] [PubMed] [Google Scholar]
- 18.Green MA, Lieberman G, Milroy CM, Parsons MA. Ocular and cerebral trauma in non-accidental injury in infancy: underlying mechanisms and implications for paediatric practice. Br J Opthalmol. 1996;80:282–287. doi: 10.1136/bjo.80.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilkinson WS, Han DP, Rappley MD, Owings CL. Retinal hemorrhages predicts neurologic injury in the shaken baby. Arch Opthamol. 1989;107:1472–1474. doi: 10.1001/archopht.1989.01070020546037. [DOI] [PubMed] [Google Scholar]
- 20.Aryan HE, Ghosheh FR, Jandial R, Levy ML. Retinal hemorrhage and pediatric brain injury: etiology and review of the literature. J Clin Neurosci. 2005;12:624–631. doi: 10.1016/j.jocn.2005.05.005. [DOI] [PubMed] [Google Scholar]