A 59-year-old man presented with the concern that his wife had witnessed him stopping breathing while asleep. Review of his sleep history also revealed agitated behaviors occurring during sleep. He reported almost nightly episodes of flailing his arms and legs about, often accompanied by angry yelling. When awoken from these episodes by his wife, he had clear dream recall, usually involving being in an argument or a fight with someone. His wife had resorted to sleeping in another bed so as not to be harmed. He had to date not suffered serious injury from one of these episodes.
These behaviors were first noticed at 30 years of age. His past medical history included depression, hypertension, coronary artery disease and hypercholesterolemia, for which he took fluoxetine, clopidogrel, atenolol, ezetimibe/simvastatin, lisinopril, aspirin, and a multivitamin. Neurologic and systemic examinations were normal. There was no family history of neurodegenerative disease.
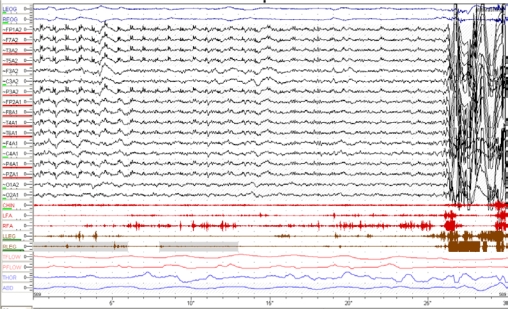
Polysomnography with time-synchronized audiovisual monitoring and an expanded EEG montage showed mild OSA, with an AHI of 5. REM sleep was notable for persistent muscle tone recorded using 3 chin EMG leads. Overt yelling (“you want trouble, then keep it shut”) and swinging of the arms in a punching motion were recorded on video during REM sleep as well. An example of his REM sleep is shown in Figure 1.
Figure 1.
30-second epoch tracing of polysomnography recorded during REM sleep reveals persistent chin EMG tone during REM sleep, with overt whole-body movements at the end of the epoch. LEOG = Left electrooculogram, REOG = Right electrooculogram, FP1A2 – O2A2 = Electroencephalogram leads, Chin, LFA, RFA = Facial electromyelograms, LLEG = Left leg electromyelogram, RLEG = Right leg electromyelogram, Tflow = thermistor flow monitor, Pflow = pressure flow monitor, THOR = Thoracic piezoelectric band, ABD = Abdominal piezoelectric band.
How would you treat this patient?
Withdrawal of fluoxetine with careful psychiatric monitoring.
REM sleep behavior disorder (RBD) is a REM-sleep parasomnia characterized by a lack of generalized atonia during REM sleep. Clinically, this usually presents as pronounced activity during sleep accompanied by vivid dream recall when awoken. Most often, the dream content is violent or anxious in nature.1 RBD may be idiopathic or secondary, being associated with neurodegenerative diseases, narcolepsy, cerebrovascular disease, intracranial tumors, central nervous system infection, and medication use. In particular, selective serotonin reuptake inhibitors, including fluoxetine, have been shown to cause secondary RBD.2
After a careful review of the patient's medication history, it was found that the RBD symptoms began around the time he had started taking fluoxetine 40 mg daily for severe depression symptoms. Therefore, secondary RBD (to fluoxetine) was suspected due to the start of symptoms with the start of fluoxetine therapy. Fluoxetine had fully controlled his depression symptoms during 19 years of continuous therapy. Two options were considered to treat the patient's RBD: addition of clonazepam, or withdrawal of fluoxetine with careful monitoring. The patient chose the latter option, and weaning was performed with close outpatient monitoring of his depressive symptoms.
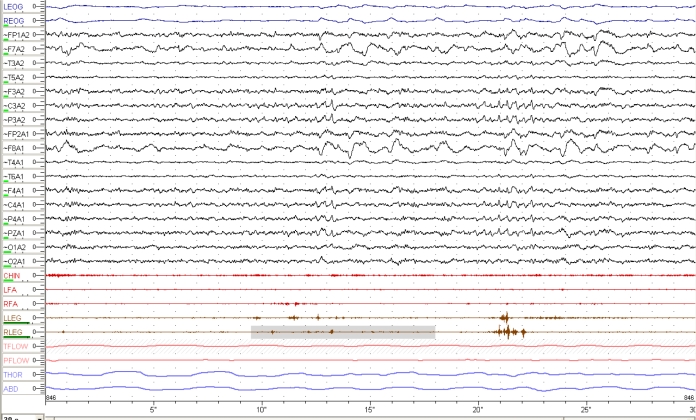
His RBD symptoms resolved around 6 weeks after discontinuation of fluoxetine, and a repeat polysomnogram was performed 3 months later. A representative REM sleep epoch is shown in Figure 2, showing a restoration of appropriate atonia in REM. The patient's clinical course demonstrates a more rapid response to withdrawal of fluoxetine compared to the original case report of this association, a major difference between the cases being patient age.2 There was a recurrence of depressive symptoms four months after discontinuing fluoxetine, and the patient was treated with bupropion, a dopaminergic/noradrenergic antidepressant without any reported tendency to induce or aggravate RBD.3 Bupropion therapy did not result in recurrence of RBD symptoms.
Figure 2.
0-second epoch tracing of polysomnography recorded during REM sleep shows normal reduction of EMG tone during REM sleep 3 months after fluoxetine discontinuation. LEOG = Left electrooculogram, REOG = Right electrooculogram, FP1A2 – O2A2 = Electroencephalogram leads, Chin, LFA, RFA = Facial electromyelograms, LLEG = Left leg electromyelogram, RLEG = Right leg electromyelogram, Tflow = thermistor flow monitor, Pflow = pressure flow monitor, THOR = Thoracic piezoelectric bands, ABD = Abdominal piezoelectric bands.
The possibility of obstructive sleep apnea (OSA) triggering the RBD symptoms was entertained.4 Given the mild nature of the OSA, the polysomnographic findings, and the clinical response to fluoxetine withdrawal, this was not considered a major factor in this case. The patient's OSA was treated with positional therapy, and he and his wife were able to return to sleeping in the same bed with improvement in both his OSA and RBD symptoms.
PEARLS
RBD may be idiopathic or secondary. Careful review for secondary causes of RBD can broaden treatment options.
Medications contributing to secondary RBD include selective serotonin reuptake inhibitors, venlafaxine, mirtazapine, tricyclic antidepressants, anticholinergics, and with alcohol abuse and abstinence states.
If RBD is thought to be secondary to a medication, weaning or changing the medication with careful follow-up should be considered. Withdrawal of an antidepressant should be slow and include close follow-up and psychiatric consultation as needed.
A history of snoring and/or observed apneas during sleep with agitated dream-enacting behaviors, as reported for this patient, may be consistent with “OSA pseudo RBD” in which the parasomnia behaviors emerge from OSA-induced arousals without the presence of increased muscle tone in REM sleep during polysomnography.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Mahowald MW, Schenck CH, Bornemann MA. Pathophysiologic mechanisms in REM sleep behavior disorder. Curr Neurol Neurosci Rep. 2007;7:167–72. doi: 10.1007/s11910-007-0013-7. [DOI] [PubMed] [Google Scholar]
- 2.Schenck CH, Mahowald MW, Kim SW, et al. Prominent eye movements during NREM sleep and REM sleep behavior disorder associated with fluoxetine treatment of depression and obsessive-compulsive disorder. Sleep. 1992;15:226–35. doi: 10.1093/sleep/15.3.226. [DOI] [PubMed] [Google Scholar]
- 3.Gugger JJ, Wagner MC. Rapid eye movement sleep behavior disorder. Ann Pharmacother. 2007;41:1833–41. doi: 10.1345/aph.1H587. [DOI] [PubMed] [Google Scholar]
- 4.Iranzo A, Santamaria J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005;28:203–6. doi: 10.1093/sleep/28.2.203. [DOI] [PubMed] [Google Scholar]