Abstract
Cyriax and Cyriax advocated the use of deep transverse friction massage in combination with Mill's manipulation in treating lateral epicondylalgia. Evidence comparing this approach with other physical therapies is lacking. The purpose of this randomized clinical trial was to compare the effectiveness of deep transverse friction massage with Mill's manipulation versus phonophoresis with supervised exercise in managing lateral epicondylalgia. Sixty patients age 30-60, presenting with the teno-periosteal variety of lateral epicondylalgia with symptom duration greater than one month, were randomized into two groups. The control group received phonophoresis with diclofenac gel over the area of the lateral epicondyle for 5 minutes combined with supervised exercise. The experimental group received 10 minutes of deep transverse friction massage followed by a single application of Mill's manipulation. Both groups received treatment 3 times per week for 4 weeks. Outcomes of interest included pain via visual analog scale (VAS), pain-free grip strength, and functional status measured with the Tennis Elbow Function Scale. Data were analyzed using a one-way ANOVA. Whereas both groups improved significantly from the initiation of treatment, a between-group comparison revealed significantly greater (p<0.05) improvements regarding pain, pain-free grip, and functional status for the experimental group compared to the control group. The results of this study demonstrate that Cyriax physiotherapy is a superior treatment approach compared to phonophoresis and exercise in managing lateral epicondylalgia.
KEYWORDS: Cyriax's Physiotherapy, Lateral Epicondylalgia, Mill's Manipulation, Phonophoresis, Tennis Elbow
Lateral epicondylalgia is a painful and debilitating musculoskeletal condition that poses significant challenges to the healthcare industry1. This condition is reported to be one of the most common upper extremity disorders with a well-defined clinical presentation and functional limitations that include impaired job performance, activities of daily living, and leisure pursuits2. Symptoms are often provoked with activities that involve gripping actions of the hand including holding tools, shaking hands, and lifting a kettle3. Lateral epicondylalgia appears to be a chronic overuse injury with degenerative changes to the common extensor tendon with the extensor carpi radialis brevis (ECRB) cited as the most commonly involved structure4. Histological studies suggest that lateral epicondylalgia involves a degenerative process, citing the presence of disorganized collagen as opposed to inflammatory cells. Consequently, the term epicondylitis is an inaccurate descriptor of the disorder, prompting the use of a more generalized term such as epicondylalgia5.
Despite the fact that lateral epicondylalgia has a well-defined clinical presentation, no ideal treatment strategy has emerged. Although conservative treatment of this condition has been the subject of numerous studies, there is no agreement as to the most effective management strategy6. Many clinicians advocate a conservative approach; however, a plethora of interventions both medical and physiotherapeutic have been reported7. Regardless of the variety of treatment options, all have the same goal: to reduce pain and improve function8.
Cyriax and Cyriax advocated the use of deep transverse friction massage in combination with Mill's manipulation in treating lateral epicondylalgia9. However, few studies examining the effectiveness of this approach are available, and most of those that are lack randomization, blinded outcome assessors, and valid functional outcome questionnaires10–12. For these reasons, additional research is indicated to examine the effectiveness of this approach.
Phonophoresis, a commonly used treatment method for lateral epicondyalgia, has been advocated to accelerate functional recovery by decreasing pain and promoting tissue healing13. Baskurt et al14 found both phonophoresis and iontophoresis to be effective strategies in managing lateral epicondylalgia. In addition to modalities such as phonophoresis, exercise therapy has also been recommended. For example, Stasinopoulos et al15 advocated the use of static stretching of the extensor carpi radialis brevis and eccentric strengthening exercises for the wrist extensors in treating lateral epicondylalgia.
Given that such a variety of treatment options exist with no agreement as to the optimal strategy, additional research is indicated to establish the effectiveness of current treatment regimens. The purpose of the present study was to compare the effectiveness of 1) Cyriax physiotherapy to the effectiveness of 2) phonophoresis coupled with supervised exercise and static stretching in regards to pain, grip strength, and function in patients with lateral epicondylalgia.
Methods
A randomized clinical trial was conducted between June 2005 and December 2007 in an outpatient clinic in Wardha, Maharashtra, India. Subjects were referred by their healthcare providers as well as recruited via advertisements in local newspapers and health magazines. Individuals were included if they were between 30-60 years of age and had been diagnosed with the tenoperiosteal variety of lateral epicondylalgia with symptoms of one month or more. Patients with tenoperiosteal lateral epicondylalgia were clinically identified with the following criteria: 1) tenderness to palpation over the lateral humeral epicondyle, 2) pain with gripping, 3) pain with passive wrist flexion with the elbow extension, and 4) pain with resisted wrist extension. Exclusion criteria included bilateral elbow pain, previous surgery or trauma to the region, medial epicondylgia, supracondylar variety of lateral epicondylalgia defined by the presence of tenderness 3–5mm above the lateral epicondyle, cervical radiculopathy, corticosteroid injection within six months, and peripheral nerve entrapment.
Following screening for inclusion, all eligible patients completed a standardized questionnaire, which included information pertaining to patient demographics, symptom presentation including duration and mechanism, history of previous episodes, treatment, and employment status. In addition, all patients underwent a standardized physical examination that included palpation of the lateral epicondyle, resisted wrist and middle finger extension, and passive stretching of the wrist extensor mass. Patients were randomly allocated into two groups. Patients in group A received the control treatment of phonophoresis with supervised exercise while patients in group B received the experimental treatment of Cyriax physiotherapy. All participants were seen 3 times a week for 4 weeks for a total of 12 treatment sessions.
Outcome Measures
Outcome measures of pain intensity, pain-free grip strength, and functional status were captured at baseline, immediately following the first treatment session (0 weeks), then at 2 weeks and 4 weeks. In addition, follow-up data was collected again at 8 weeks to examine the lasting effects of treatment. All outcome measures were assessed by an independent observer who was blinded to the patient's group assignment.
Pain severity was measured with the visual analogue scale (VAS). The VAS consists of a 10 cm line with 0 cm representing the “least pain imaginable” and 10 cm the “worst pain imaginable.” Patients were instructed to intersect the scale with a vertical line based on their current level of pain. The visual analogue scale has been found to be a valid and reliable method of measuring perceived pain16,17. VAS is a general measure that may be used for multiple conditions and is not specific to the elbow.
Pain-free grip strength was measured in pounds with a hand-held dynamometer (Fabrication Enterprises, USA). Patients were positioned as described previously by Abbott et al18 and instructed to squeeze the dynamometer to the point where they first experienced pain and then release. Patients were blinded to the reading. A total of three measures were recorded with 30-sec rest intervals between each. The mean value of the repetitions was calculated and represented the patient's pain-free grip strength. The reading was also kept blinded to the treating therapist as readings were taken by an evaluator who was not involved in the treatment. Pain-free grip strength has been found to be a valid measure for assessing clinical change over time in patients with lateral epicondylalgia19.
Functional status was evaluated by completion of the Tennis Elbow Function Scale (TEFS)20. The TEFS is a 10-item questionnaire on which the patient rates selected functional activities based on the level of discomfort. Each activity is rated 0 through 4 with a total possible score of 40. Higher scores are indicative of greater levels of disability. The TEFS has been found to have high test-retest reliability (ICC 0.92) and moderate construct validity (Pearson's correlation coefficient 0.47)20.
Treatment
Subjects in the experimental group received Cyriax physiotherapy consisting of 10 minutes of deep transverse friction massage immediately followed by a single application of Mill's manipulation. For the delivery of friction massage, patients were seated and positioned in 90 degrees of elbow flexion with forearm supination. The treating clinician stabilized the patient's wrist and forearm with one hand while applying the massage with the other. The thumb of the treating hand was used to apply the friction and was positioned with the distal interphalangeal joint in 90 degrees of flexion with the tip of the thumb resting against the lateral epicondyle. The thumb was then drawn across the epicondyle by flexion of the fingers. Friction was applied for a total of 10 minutes; hand placement is detailed in Figure 1. For the delivery of Mill's manipulation, patients were positioned seated with the affected upper extremity in 90 degrees of abduction with internal rotation enough so that the olecranon faced up. The clinician stabilized the patient's wrist in full flexion and pronation with one hand while the other was placed over the olecranon. The maintenance of full wrist flexion is important as failure to maintain this position could lead to a majority of the thrusting force being borne by the humeroulnar joint. While maintaining full wrist flexion and pronation, the clinician delivered a high-velocity lowamplitude (HVLA) thrust at the end range of elbow extension (Figure 2).
FIGURE 1.
Deep transverse friction massage.
FIGURE 2.
Near end range of Mill's manipulation.
Patients assigned to the control group received phonophoresis followed with supervised therapeutic exercise. The medication applied with phonophoresis was Voveran Emulgel, Novartis (diclofenac sodium 1%), which is a topical non-steroidal anti-inflammatory agent. Ultrasound parameters were based on previously published guidelines21 and consisted of 100% duty cycle, at a frequency of 1 MHz, delivered at an intensity of 0.8 W/cm2 over the area of the lateral epicondyle for 5 minutes. The supervised exercise program included static stretching of the extensor carpi radialis brevis followed by eccentric strengthening of the wrist extensors. Static stretching was performed seated with elbow extension, forearm pronation, and wrist flexion with ulnar deviation. Stretch was applied according to patient tolerance. This position was held for 30-45 seconds and was performed three times before and three times after the eccentric exercise portion of the treatment for a total of 6 repetitions. There was a 30-second rest interval between each bout of stretching.
Eccentric strengthening was performed seated with full elbow extension, forearm pronation, and maximum wrist extension. From this position, the patient slowly lowered the wrist into flexion for a count of 30, using the contralateral hand to return the wrist to maximum extension. Patients were instructed to continue the exercise in the presence of mild discomfort and to cease exercise if the pain became disabling. When eccentric exercises could be performed without minor pain or discomfort, the load was increased using free weights based on the patient's 10 repetition maximum. Three sets of 10 repetitions were performed during each treatment with a one-minute rest interval between each set. In addition to treatment, all participants were provided with education regarding ergonomics and activity modification to avoid provocation of symptoms while attempting to remain as active as possible.
Data Analysis
Statistical analysis including mean, standard deviation, and standard error were calculated for all measurements. Data analysis was performed with SPSS version 14.0. The mean differences with SD for outcome measures of pain, pain-free grip, and function were calculated for time periods of baseline – 2 weeks, baseline – 4 weeks, and baseline – 8 weeks. A one-way ANOVA was used to determine if significant differences (p<0.05) existed within and between groups for each outcome measure at each followup period. Intra-rater reliability for hand grip dynamometry for each group was calculated and presented as intra-class correlation coefficients (ICC 1,1) with associated standard error of measurement and 95% confidence intervals. Effect sizes were calculated at 8 weeks for each outcome measure with the following formula for Cohen's D: (mean of experimental group) – (mean of control group) / (SD). Effect sizes of .2–.5 were regarded as small, .5–.8 as medium, and greater than .8 as large22.
Results
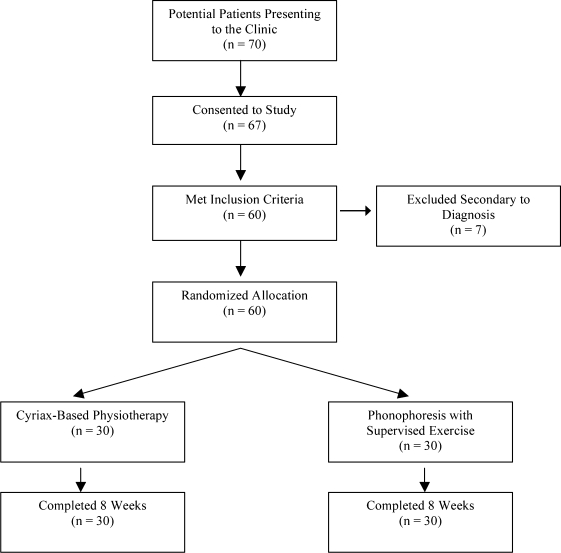
Seventy patients were screened for inclusion with a total of 60 subjects enrolling in the study. Of those excluded, 7 subjects didn't meet the inclusion criteria and 3 were unwilling to participate in the study. Participant flow through the trial is illustrated in Figure 3.
FIGURE 3.
Flow of subject inclusion and participation.
The mean age of the patient sample was 38.6 years with 76.7% of subjects aged 30–40. The sample was made up of a greater number of females. Regarding employment status, 23.33% of patients were domestic workers (i.e., homemakers) while the remainder were exposed to repetitive motions such as keyboarding or manual tool use. Baseline characteristics for both treatment groups are displayed in Table 1. Groups were found to be similar at baseline with the exception of age where a significant difference existed (p=0.002). Outcome measure scores were found to be similar between groups at baseline.
TABLE 1.
Baseline characteristics.
| Variable | Cyriax (n=30) | Phono & Exercise (n=30) | P |
|---|---|---|---|
| Gender (% of female) | 78% | 65% | |
| Age | 38(6.24) | 32 (5.25) | 0.002 |
| Symptom duration (weeks) | 14.5(4.5) | 12.5 (4.3) | 0.83 |
| Tennis Elbow Function Scale | 33.66(1.66) | 33.10(2.09) | 0.255 |
| VAS | 8.20(0.76) | 8.10(0.75) | 0.60 |
| Pain-free grip (pounds) | 16.53(3.23) | 17.33(3.12) | 0.33 |
All values represent the mean with (SD) with the exception of gender.
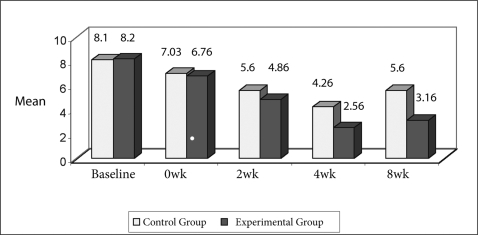
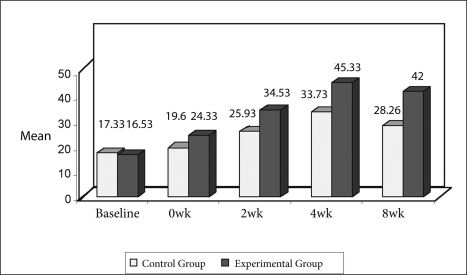
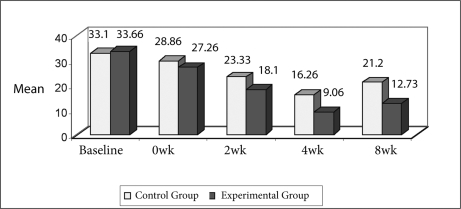
Outcome measures for both groups displayed steady improvement from onset of treatment to 4 weeks. Mean scores for each outcome of interest at each follow-up period are displayed in Figures 4–6. Both treatment groups experienced significant improvements in all outcome measures from baseline to discharge at 4 weeks (p<0.05 for all measures). Improvements at the 4-week mark were not maintained, however, with both groups experiencing a significant decline in outcome at the 8-week follow-up. However, all outcome measures for both groups remained significantly improved compared to baseline at 8 weeks. Between-group analysis indicated that the Cyriax physiotherapy group had significantly better outcome scores at all follow-up periods compared to those receiving phonophoresis, supervised exercise, and static stretching (p<0.05 for all measures), with the exception of VAS collected immediately following the first treatment (0 week) where no significant difference between groups was found. Within-group changes are displayed in Table 2. Calculated effect sizes at 8 weeks revealed a medium-size treatment effect favoring the Cyriax group for pain-free grip and TEFS, both with an effect size of 0.74. A large-size treatment effect favoring the Cyriax group was found for pain via VAS at 8 weeks with a calculated effect size of 0.81. Actual effect sizes for VAS and TEFS scores were negative due to the nature of the outcome measure; however, they are presented as positive values for the purpose of this article.
TABLE 2.
Within-group change scores from baseline to 4 and 8 weeks.
| Time Period |
||||
|---|---|---|---|---|
| Measure | Baseline – 4 weeks | P | Baseline – 8 weeks | P |
| Vas | ||||
| Cyriax | 5.63 (5.31, 5.95) | 0.000 | 5.03 (4.62, 5.44) | 0.000 |
| Phono & Exercise | 3.83 (3.52, 4.14) | 0.000 | 2.50 (2.12, 2.87) | 0.000 |
| Pain-Free Grip | ||||
| Cyriax | 28.80 (27.21, 30.38) | 0.000 | 25.46 (23.13, 27.80) | 0.000 |
| Phono & Exercise | 16.40 (15.07, 17.72) | 0.000 | 10.93 (9.38, 12.48) | 0.000 |
| Function∗ | ||||
| Cyriax | 24.60 (23.41, 25.78) | 0.000 | 20.93 (19.30, 22.56) | 0.000 |
| Phono & Exercise | 16.83 (15.70, 17.96) | 0.000 | 11.90 (10.64, 13.15) | 0.000 |
All values expressed as mean with (95% CI).
Phono = phonophoresis
Function measured with the Tennis Elbow Function Scale (score range 0-40 with higher score indicating greater disability).
The ICC (1,1) for the hand-held dynamometer test-retest reliability was found to be 0.95 (95% CI 0.85–0.95) in the control group with a standard error of (SEM) ± 6.98. For the experimental group, the ICC was 0.93 (95% CI 0.84–0.95) with a SEM of ± 12.4 Overall, these values reflect high test-retest reliability of pain-free grip measured via hand-grip dynamometry.
Discussion
The results of this clinical trial are novel as no other studies comparing Cyriax physiotherapy to a treatment regimen consisting of phonophoresis with supervised exercise and static stretching were identified. The results of this study demonstrate that both the Cyriax and phonophoresis with supervised exercise and static stretching groups experienced significant improvements in pain, pain-free grip strength, and function following 12 treatment sessions. The Cyriax physiotherapy group experienced greater outcomes for all variables in comparison to those receiving phonophoresis with supervised exercise and static stretching.
The reported success of Cyriax physiotherapy in the present study conflicts with previously published trials11,12. Stasinopoulos et al11 compared the effectiveness of Cyriax physiotherapy, supervised exercise, and treatment with polychromatic non-coherent light in managing lateral epicondylalgia. They concluded that supervised exercise consisting of static stretching and eccentric strengthening produced the largest effect in reducing pain and improving function. However, their study lacked randomization, which can result in unbalanced groups regarding prognosis23. Verhaar et al12 compared local corticosteroid injection with Cyriax physiotherapy and concluded that steroid injection provided greater benefit at 6 weeks regarding grip strength and patient satisfaction although no significant differences were found between groups at one year. The authors did not offer any description or reference regarding technique; therefore, it is not clear if their application of Cyriax physiotherapy differed from that of the present study. In addition, studies of this type do little to aid physical therapists in making clinical decisions as injections are not delivered as part of physical therapy treatment.
The improvements experienced by the phonophoresis with supervised exercise and static stretching group are consistent with previous trials addressing these interventions11,14,24. As mentioned above, Stasinopoulos et al11 found greater success with supervised exercise than with Cyriax physiotherapy and polychromatic non-coherent light. The supervised exercise program used in their trial was similar in design to that used in the present study. Previous trials examining phonophoresis have also reported benefits for patients diagnosed with LE14,24. Baskurt et al14 found equal success regarding pain and grip strength following treatment with phonophoresis or iontophoresis both with naproxen. Cabak and colleagues24 shared similar results concluding that phonophoresis with ketoprofen was superior to ultrasound alone. In comparing the results of these trials to those experienced by the phonophoresis treatment group in the present study, two points must be considered. First, none of the above mentioned trials used a true control group, thereby not controlling for the natural course of the disorder or spontaneous recovery. Second, the present study did not assign patients to receive supervised exercise or phonophoresis as an isolated treatment. Therefore, comparisons between our results and those of previous trials should be made with caution as it is not possible to determine which intervention made the greatest contribution to the treatment effect.
Patients included in this study were those clinically identified as having the tenoperiosteal variety of lateral epicondylalgia as it is hypothesized that this form is best managed with Mill's manipulation25. The proposed mechanism of Mill's manipulation is the lengthening of scar tissue following the rupture of adhesions due to the manipulation9. This increased length decreases tension on the scar leading to less pain, effectively converting a tear shaped like a “V” into one resembling a “U”26. The resulting gap is filled with fibrous tissue, resulting in permanent lengthening and abolition of pain25,27. The application of friction massage is said to provide the patient with analgesia prior to the manipulation as well as softening the scar27. It has been hypothesized that the mechanism of pain relief secondary to friction massage may be due to modulation of nociceptive impulses at the spinal cord level, also known as the gate control theory28. Currently, no published evidence exists to prove the proposed mechanism as to what actually occurs during and following manual treatment with Cyriax physiotherapy9. What's more, despite the considerable evidence supporting the use of manual therapy techniques in treating musculoskeletal pain, there still exists no consensus as to the exact mechanisms of action there either29.
Recent evidence has indicated that the central nervous system may play a role in pain inhibition following joint manipulation30,31. Vicenzino et al32 investigated the effects of a non-thrust cervical lateral glide in patients with chronic lateral epicondylalgia. This technique was shown to result in increased pain-free grip, pressure pain threshold, as well as a sympathetic nervous system response as indicated with measures of skin conductance and blood flux. More recently, Paungmali et al33 found similar results with improved pain-free grip, pressure pain threshold, and sympatho-excitation following mobilization with movement directed at the elbow. It should be noted that the above studies captured outcomes only immediately following treatment; therefore, no generalization can be made regarding long-term effects. Given the results of these trials, the potential exists for a similar SNS response following the application of Cyriax physiotherapy, which may explain the technique's superiority in decreasing pain and improving pain-free grip strength.
Despite the fact that LE is commonly encountered, there exists no consensus as to the exact cause and pathological process of the disorder3. It has been stated that LE stems from overuse of the ECRB with degenerative changes present as opposed to inflammation5. The lack of an active inflammatory process may explain the decreased treatment effect experienced by the phonophoresis with supervised exercise and static stretching group in the present study. Aside from local degenerative changes in the ECRB, it has been hypothesized that other sources exist such as local articular and nerve lesions as well as involvement of the cervicothoracic spine5. A higher incidence of cervical and thoracic pain and dysfunction has been found in patients with LE, and recent evidence supports the inclusion of interventions directed at the cerviothoracic spine34–36.
Impairment-based multi-modal treatment including therapeutic exercise and manipulative therapy has been previously recommended37, and based on the above evidence, it appears that this approach would be ideal in managing patients with LE. The experimental group in the present study did not receive a multi-modal treatment approach. Results based on the application of a single treatment technique may raise questions of generalizability as it appears that multi-modal approaches are more typically used in physical therapy practice. The favorable results in the current study indicate the need for future research examining the incorporation of Cyriax techniques into multimodal treatment regimens.
Limitations
The present study is not without limitations. First, the absence of a true notreatment control group makes it diflcult to differentiate between treatment effect and the natural course of the disorder, thus threatening the internal validity of the study. Each group received multiple interventions; therefore, it is not possible to discern which component of the treatment had the greatest impact on outcome. It may be advantageous for future studies to include groups receiving friction massage and Mill's manipulation in isolation, thus allowing for conclusions to be made regarding individual effects. Another potential limitation of this study was the use of area-specific palpation for inclusion/exclusion. The reliability and validity of the differentiation between tenoperiosteal and supracondylar LE is unknown and may have led to error during the inclusion/exclusion process. The TEFS, while found to have high reliability and adequate validity, lacks a defined minimally clinically important difference (MCID). Although the changes in patient scores were found to be statistically significant, the absence of the MCID makes it difficult to identify if these changes were perceived as important by the patient and thus represented a functional benefit. Finally, no longterm follow-up data was collected past 8 weeks; therefore, the long-term effects of the interventions in the present study remain unknown.
Conclusion
The results of this randomized clinical trial demonstrate that Cyriax physiotherapy was found to provide a superior benefit in terms of pain, pain-free grip, and functional status when compared to a treatment regimen consisting of phonophoresis with supervised exercise and static stretching. The long-term effects of treatment remain unknown past 8 weeks. However, the decline in status for both groups at 8 weeks compared to discharge at 4 weeks may suggest a gradual return to baseline following the cessation of treatment. The results of this clinical trial contribute to the growing body of evidence supporting the use of manual therapy in treating lateral epicondylitis. Further research is warranted with longer follow-up periods as well as the inclusion of Cyriax physiotherapy as a component of a multi-modal approach thus increasing the generalizability of the findings.
FIGURE 4.
Comparison of VAS (in cms) at baseline and follow-up periods.
FIGURE 5.
Comparison of pain-free grip strength (in lbs) at baseline and follow-up periods.
FIGURE 6.
Comparison of Tennis Elbow Function Scale score at baseline and followup periods.
REFERENCES
- 1.Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411–422. doi: 10.1136/bjsm.2004.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waugh EJ, Jaglal SB, Davis AM, Tomlinson G, Verrer MC. Factors associated with prognosis of lateral epicondylitis after 8 weeks of physical therapy. Arch Phys Med Rehabil. 2004;85:308–318. doi: 10.1016/s0003-9993(03)00480-5. [DOI] [PubMed] [Google Scholar]
- 3.Vicenzino B, Wright A. Lateral epicondylalgia I: A review of epidemiology, pathophysiology, aetiology, and natural history. Phys Ther Rev. 1996;1:23–34. [Google Scholar]
- 4.Kraushaar B, Nirschl R. Current concepts review tendinosis of the elbow (tennis elbow): Clinical features and findings of histological immunohistochemical and electron microscopy studies . J Bone Joint Surg Am. 1999;81:259–285. [PubMed] [Google Scholar]
- 5.Waugh EJ. Lateral epicondylalgia or epicondylitis: What's in a name? J Orthop Sports Phys Ther. 2005;35:200–202. doi: 10.2519/jospt.2005.0104. [DOI] [PubMed] [Google Scholar]
- 6.Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard C-H. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: An attempted metaanalysis. J Bone Joint Surgery (Br) 1992;74–B:646–651. doi: 10.1302/0301-620X.74B5.1388172. [DOI] [PubMed] [Google Scholar]
- 7.Trudel D, Duley J, Zastrow I, Kerr E, Davidson R, MacDermid J. Rehabilitation for patients with lateral epicondylitis: Systematic review. J Hand Ther. 2004;17:243–266. doi: 10.1197/j.jht.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Wright A, Vicenzino B. Lateral epicondylagia II: Therapeutic management. Phys Ther Rev. 1997;2:39–48. [Google Scholar]
- 9.Stasinopoulos D, Johnson MI. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med. 2004;38:675–677. doi: 10.1136/bjsm.2004.013573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baltaci G, Ergun N, Tunay VB. Effectiveness of Cyriax manipulative therapy and elbow band in the treatment of lateral epicondylitis. Eur J Sport Traumatol Rel Res. 2001;23:113–118. [Google Scholar]
- 11.Stasinopoulos D, Stasinopoulos I. Comparison of effects of Cyriax physiotherapy, a supervised exercise programme, and polarized polychromatic non-coherent light (Bioptron light) for the treatment of lateral epicondylitis. Clin Rehab. 2006;20:12–23. doi: 10.1191/0269215506cr921oa. [DOI] [PubMed] [Google Scholar]
- 12.Verhaar JAN, Walenkamp GHIM, Van Mameren HV, Kester ADM, Vander Linden AJ. Local corticosteroid injection vs. Cyriaxtype physiotherapy for tennis elbow. J Bone Joint Surg (Br) 1995;77–B:128–132. [PubMed] [Google Scholar]
- 13.Oziomek R, Perrin D, Herold D, Denegar C. Effect of phonophoresis on serum salicylate levels. Med Sci Sports Exerc. 1990;23:397–401. [PubMed] [Google Scholar]
- 14.Baskurt F, Ozcan A, Algun C. Comparison of effects of phonophoresis and iontophoresis of naproxen in the treatment of lateral epicondylitis. Clin Rehabil. 2003;17:96–100. doi: 10.1191/0269215503cr588oa. [DOI] [PubMed] [Google Scholar]
- 15.Stasinopoulos D, Stasinopoulos K, Johnson MI. An exercise programme for management of lateral elbow tendinopathy. Br J Sports Med. 2005;39:944–947. doi: 10.1136/bjsm.2005.019836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 17.Price DD, Bush FM, Long S, Harkins SW. A comparison of pain characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217–226. doi: 10.1016/0304-3959(94)90097-3. [DOI] [PubMed] [Google Scholar]
- 18.Abbott JH, Patla CE, Jensen RH. The initial effects of an elbow mobilization with movement technique of grip strength in subjects with lateral epicondylalgia. Man Ther. 2001;6:163–169. doi: 10.1054/math.2001.0408. [DOI] [PubMed] [Google Scholar]
- 19.Stratford PW, Levy DR. Assessing valid change over time in patients with lateral epicondylitis at the elbow. Clin J Sports Med. 1994;4:88–91. [Google Scholar]
- 20.Lowe KA. A thesis submitted to the Faculty of Graduate Studies and Research in partial fullfillment of the requirements for the degree of Master of Science. Edmonton, Alberta: Department of Physical Therapy; Fall 1999. Test/retest reliability, construct validity, and responsiveness of the tennis elbow function scale. [Google Scholar]
- 21.Watson T. Ultrasound dose calculations. In Touch. 2002;101:14–17. [Google Scholar]
- 22.Cook C. Clinimetrics Corner: Use of effect sizes in describing data. J Man Manip Ther. 2008;16:E54–E57. doi: 10.1179/jmt.2008.16.4.82E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyatt G, Rennie D. User's Guide to the Medical Literature: A Manual for Evidencebased Clinical Practice. Chicago, IL: AMA Press; 2002. [Google Scholar]
- 24.Cabak A, Maczewska M, Lyp M, Dobosz J, Gasiorowska U. The effectiveness of phonophoresis with ketoprofen in the treatment of epicondylopathy. Orthop Traumatol Rehabil. 2005;7:660–665. [PubMed] [Google Scholar]
- 25.Cyriax J. Textbook of Orthopaedic Medicine: Volume 1. New Delhi, India: AITBS; 1936. [Google Scholar]
- 26.Mills GP. The treatment of tennis elbow. Br Med J. 1928;1:12–13. doi: 10.1136/bmj.1.3496.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kushner S, Reid D. Manipulation in the treatment of tennis elbow. J Orthop Sports Phys Ther. 1986;7:264–272. doi: 10.2519/jospt.1986.7.5.264. [DOI] [PubMed] [Google Scholar]
- 28.De Bruijn R. Deep transverse friction: Its analgesic effect. Int J Sports Med. 1984;5:35–36. [Google Scholar]
- 29.Bialosky J, Bishop M, Price D, Robinson M, George S. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Man Ther. 2008 doi: 10.1016/j.math.2008.09.001. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sterling M, Jull G, Wright A. Cervical mobilisation: Concurrent effects on pain, sympathetic nervous system activity and motor activity. Man Ther. 2001;6:72–81. doi: 10.1054/math.2000.0378. [DOI] [PubMed] [Google Scholar]
- 31.Schmid A, Brunner F, Wright A, Bachmann LM. Paradigm shift in manual therapy? Evidence for a central nervous system component in the response to passive cervical joint mobilisation. Man Ther. 2008;13:387–396. doi: 10.1016/j.math.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Vicenzino B, Collins D, Benson H, Wright A. An investigation of the inter-relationship between manipulative therapy-induced hypoalgesia and sympathoexcitation. J Manipulative Physiol Ther. 1998;21:448–453. [PubMed] [Google Scholar]
- 33.Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Hypoalgesic and sympathoexcitatory effects of mobilization with movement for lateral epicondylalgia. Phys Ther. 2003;83:374–383. [PubMed] [Google Scholar]
- 34.Cleland J, Whitman J, Fritz J. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epicondylalgia: A retrospective analysis. J Orthop Sports Ther. 2004;34:713–724. doi: 10.2519/jospt.2004.34.11.713. [DOI] [PubMed] [Google Scholar]
- 35.Cleland J, Flynn T, Palmer J. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: A pilot clinical trial. J Man Manip Ther. 2005;13:143–151. [Google Scholar]
- 36.Berglund KM, Persson BH, Denison E. Prevalence of pain and dysfunction in the cervical and thoracic spine in persons with and without lateral elbow pain. Man Ther. 2008;13:295–299. doi: 10.1016/j.math.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 37.Vicenzino B. Lateral epicondylalgia: A musculoskeletal physiotherapy perspective. Man Ther. 2003;8:66–79. doi: 10.1016/s1356-689x(02)00157-1. [DOI] [PubMed] [Google Scholar]