Abstract
It has been demonstrated that patients receiving mobilization techniques do not exhibit tolerance to repeated applications. However, this phenomenon has not been investigated for thoracic manipulation. Our aim was to determine if patients receiving thoracic thrust manipulation exhibit tolerance to repeated applications in acute mechanical neck pain. Forty-five patients were randomly assigned to two groups. The control group received electro- and thermotherapy for 5 sessions, and the experimental group received the same program and also received a thoracic thrust manipulation once a week for 3 consecutive weeks. Outcome measures included neck pain and cervical mobility. Within-session change scores for pain and mobility during treatment sessions #1, 3, and 5 were examined with a one-way repeated measured ANOVA. A 2-way ANOVA with session as within-subject variable and group as between-subject variable was used to compare change scores for each visit between groups to ascertain if there were significant between-group differences in within-session changes for the experimental versus the control group. The ANOVA showed that for either group the 3 within-session change scores were not significantly different (P > 0.1). The 2-way ANOVA revealed significant differences between groups for both pain and neck mobility in within-session change scores (all, P < 0.001). Change scores in each session were superior in the experimental group as compared to those in the control group. The results suggest that patients receiving thoracic manipulation do not exhibit tolerance to repeated applications with regard to pain and mobility measures in acute mechanical neck pain. Further studies should investigate the dose-response relationship of thoracic thrust manipulation in this population.
KEYWORDS: Neck Pain, Thoracic Thrust Manipulation, Tolerance
Neck pain is a significant problem in society. The incidence rate for self-reported neck pain in the general population has been reported to be between 146 and 213 per 1,000 patient years1. The reported point prevalence of neck pain varies between 9.5–35%2,3. The 12-month prevalence for neck pain ranges from 30–50%, and the 12-month prevalence of activity-limiting pain is reported to be between 1.7% and 11.5%1. Nearly half of patients with neck pain will go on to develop chronic symptoms4, and many will continue to exhibit moderate disability at long-term follow-up5. In the United States, neck pain accounts for almost 1% of all visits to primary care physicians6. After lumbar spine-related diagnoses at 19%, cervical spine diagnoses were the second most common reason for referral at 16% in a US study on outpatient physical therapy7. Similarly, the economic burden associated with the management of neck pain patients is second only to low back pain in annual workers' compensation costs in the United States8.
In the majority of patients with neck pain, no patho-anatomic diagnosis can be provided resulting in a diagnostic label of non-specific or mechanical neck pain for many patients. Childs et al9 have proposed a treatment-based classification system to further differentiate among this likely heterogeneous group of patients. In this classification, manual therapy to the cervical and thoracic spine, particularly thrust and non-thrust manipulation, is the main treatment intervention proposed for management of the mobility subgroup. There is growing evidence supporting the use of thoracic thrust manipulation in the management of this subgroup of patients with mechanical neck pain with multiple studies showing noted improvements in pain, range of motion, and function10–13.
However, the design of previous studies10–13 has varied in that the researchers have used different numbers of manipulations. This makes it difficult for clinicians to determine how many applications of thrust manipulation are likely to maximize patient outcomes. In this context, one issue we need to consider is whether repeated application of thoracic manipulation leads to tolerance. Tolerance is defined here as a decrease in the effect size or magnitude of the intervention over time, as measured within sessions. Tolerance should affect the number of interventions provided. In the context of thoracic manipulation for patients with mechanical neck pain, tolerance to thoracic manipulation would logically decrease the number of manipulations that are applied and that are required for the demonstrated positive study outcomes.
Paungmali et al14 studied tolerance to repeated applications of a manual non-thrust technique directed at the elbow region. They showed that the technique had a hypoalgesic effect measured as an increase in pressure pain threshold levels at each session that was of similar magnitude to the first time the technique was administered, suggesting that non-thrust techniques do not cause tolerance to repeated applications. It should be noted that this study did not include a control group so the possibility of consistent improvements in their cohort could have potentially been related to a placebo effect. Irrespective, this phenomenon of cumulative tolerance has yet to be investigated with regards to thrust techniques. Studying thrust in addition to non-thrust techniques is relevant, since non-thrust and thrust interventions stimulate different axial sensory beds15. Also, thoracic spine manipulation was shown to result in significantly greater short-term reductions in pain and disability than thoracic non-thrust manipulation in neck pain patients16. From a clinical perspective, one could argue that it is necessary to investigate the tolerance aspect not only with regard to neurophysiological measures, such as pressure pain thresholds, but also with regard to clinically relevant outcomes, such as pain and mobility.
We recently conducted a randomized clinical controlled trial comparing the effectiveness of an electro- and thermotherapy program alone or in combination with thoracic spine thrust manipulation in patients with acute neck pain17. This paper presents a secondary analysis of data related to the tolerance aspect of the thoracic spine thrust manipulation. The purpose of this paper is to analyze whether repeated application of thoracic manipulation causes tolerance with regard to pain and mobility outcomes in patients with acute neck pain. We hypothesized that repeated application of thoracic spine manipulation would not lead to tolerance to repeated applications both with regard to pain and neck mobility outcomes.
Methods
Participants
Consecutive patients referred by their primary care physician for physical therapy with complaints of mechanical neck pain of less than 1-month duration were screened for eligibility in the original study17. Mechanical neck pain was defined as generalized neck and/or shoulder pain provoked by neck postures, neck movement, or palpation of the cervical musculature. Exclusion criteria were contraindication to thrust manipulation; history of cervical surgery or whiplash trauma; diagnosis of cervical radiculopathy or myelopathy; diagnosis of fibromyalgia syndrome18; treatment with spinal manipulative therapy in the previous two months; or less than 18 or greater than 45 years old. The Human Research Committee of the Escuela de Osteopatia de Madrid approved this study. All subjects signed an informed consent prior to participation in the study.
Group Assignment
Of 60 patients presenting upon referral by their primary care physician, 45 (mean age 34±5 years) were randomized into an electro- and thermotherapy program alone or in combination with thoracic spine thrust manipulation. A researcher not further involved in the study prepared sequentially numbered index cards placed in sealed and opaque envelopes with a random assignment based on a computer-generated random table of numbers. The treating therapist, blinded to baseline examination findings, opened the envelopes and proceeded with treatment according to the random group assignment.
Interventions
Both groups received 5 sessions of an electro- and thermotherapy program over a 3-week period. We applied superficial thermotherapy by way of an infrared lamp (250 watts), located 50 cm from the patient's neck for 15 minutes. Electrotherapy was provided in the form of transcutaneous electrical nerve stimulation (Phyaction 782; Uniphy BV, Son, the Netherlands) with a frequency of 100 Hz and 250 microsecond pulses for 20 minutes using two 4×6 cm electrodes placed bilaterally at the spinous process of C7 vertebra.
In addition, the experimental group received a thoracic thrust manipulation intervention. Patients were seated with the arms crossed over the chest and hands passed over the shoulders (one hand on the opposite shoulder and the other hand along the ribcage). The therapist placed his chest at the level of the patient's mid-thoracic spine and grasped the patient's elbows. Gentle flexion of the thoracic spine was introduced until a slight tension was felt in the tissues at the contact point between the therapist's chest and patient's back. Then, a “seated” distraction manipulation in an upward direction was applied19 (Figure 1). During the manipulation, the therapist listened for a popping sound. If no popping was heard on the first attempt, the therapist repositioned the patient and performed a second thrust manipulation. A maximum of two attempts were performed on each patient.
FIGURE 1.
Thoracic thrust manipulation.
Outcome Measures
A Visual Analog Scale (VAS) was used to record the patient's level of pain (0 = no pain; 10 = the worst pain imaginable). Patients placed a mark along the 10-cm line corresponding to the intensity of their symptoms, which was scored to the nearest millimeter. The VAS has been demonstrated to be a reliable and valid instrument for measuring pain intensity20. The VAS was selected as an outcome measure based on its ability to detect immediate changes in pain and because its minimal clinically important difference (MCID) has been established as 9–11 mm21,22.
Cervical range of motion (CROM) was assessed with the patient in a relaxed sitting position. All subjects were asked to sit on a chair with both feet flat on the floor, hips and knees positioned at 90° angles, and buttocks positioned against the back of the chair. The goniometer was placed on the top of the head. Once the goniometer was set in the neutral position, the patient was asked to move the head as far as possible in a standard sequence: Flexion, extension, right lateral flexion, left lateral flexion, right rotation, and left rotation. Three trials were recorded for each direction of movement, and the mean was employed in the analysis. This method of assessment has been described previously23. Reliability testing of these specific methods of measuring CROM have yielded an ICC2,1 ranging between 0.66– 0.7824.
Study Protocol
A baseline examination consisting of a standardized history and physical examination by an experienced physical therapist assessed patients for study eligibility. Demographic data recorded included age, gender, past medical history, and location, nature, and onset of symptoms. After eligibility was established and the patent consented to participate, random group assignment occurred as described above. All patients received the first treatment session on the day of the initial examination by the treating therapist, who was unaware of findings on the baseline examination. All patients attended the first visit on a Monday with the second visit on Thursday, the third visit on the following Monday, and so on. Patients in the experimental group received thoracic thrust manipulation once per week for the three consecutive weeks (1st visit, 3rd visit, and 5th visit). Patients were blinded to the treatment allocation group by not revealing that the inclusion of a specific intervention (thoracic spine thrust manipulation) was in fact being evaluated.
All patients completed pain (VAS) and mobility (CROM) outcome measures at baseline (prior to the 1st session) and immediately following the 1st treatment (allowing for calculation of within-session change for visit 1), prior to and immediately following the 3rd treatment (representing within-session change for visit 3), and prior to and immediately following the 5th treatment (allowing for calculation of within-session change for visit 5). CROM was assessed by an assessor blinded to the treatment allocation of the patient.
Statistical Analysis
Data were analyzed with SPSS version 14.0. Key baseline demographic variables were compared between groups using independent t-tests for continuous data and [.chi]2 tests of independence for categorical data. Within-session change scores for pain and mobility (flexion, extension, rotation, and lateral flexion) that occurred during treatment sessions #1, 3, and 5 were examined with a oneway repeated-measure ANOVA for each group to determine it thoracic thrust manipulation led to tolerance with repeated applications. Additionally, a 2-way ANOVA with session (#1, #3, #5) as the within-subject variable and group (experimental, control) as the between-subject variable was used to compare within-session change scores for each visit between both groups to ascertain if there were significant between-group differences in same-session within-session changes for the experimental versus the control group. Separate ANOVAs were conducted with pain and mobility (flexion, extension, rotation, or lateral flexion) as the dependent variable. Posthoc comparisons were done with the Tukey test (SNK). The statistical analysis was conducted at a 95% confidence level with a P value < 0.05 considered statistically significant.
Results
Baseline Data
Twenty-two patients (45% female; mean age 35±6 years) were allocated to the control (electro- and thermotherapy program) group, whereas 23 patients (48% female; mean age 34±4 years old) were allocated to the experimental (electro- and thermotherapy program plus thoracic manipulation) group. Baseline characteristics between the groups were similar for all variables (P>0.05) (Table 1).
TABLE 1.
Baseline demographics for both groups∗.
| Control Group | Experimental Group | |
|---|---|---|
| Gender (Male/Female) | 12/10 | 12/11 |
| Age (years) | 35 ± 6 | 34 ± 4 |
| Duration of symptoms (days) | 18.7 ± 3.9 | 19.5 ± 4.5 |
| Neck pain∗∗ | 52.7 ± 5.5 | 54.7 ± 8.2 |
| Northwick∗∗∗ | 27.0 ± 3.1 | 27.9 ± 3.0 |
| Cervical range of motion (degrees) | ||
| Flexion | 44.4 ± 5.1 | 45.2 ± 4.6 |
| Extension | 58.8 ± 5.8 | 59.4 ± 8.2 |
| Right lateral-fexion | 39.4 ± 4.7 | 38.2 ± 5.2 |
| Lef lateral-fexion | 40.2 ± 4.8 | 39.2 ± 4.6 |
| Right rotation | 56.1 ± 6.6 | 55.4 ± 7.3 |
| Lef rotation | 57.6 ± 5.4 | 58.2 ± 6.4 |
Data are mean ± SD except for gender. No diference between groups, P>0.30.
Measured with a 0-100 mm visual analogue scale (0, no pain; 100, worst pain imaginable).
Range of score is 0-36 with higher scores meaning greater disability.
Participant Flow
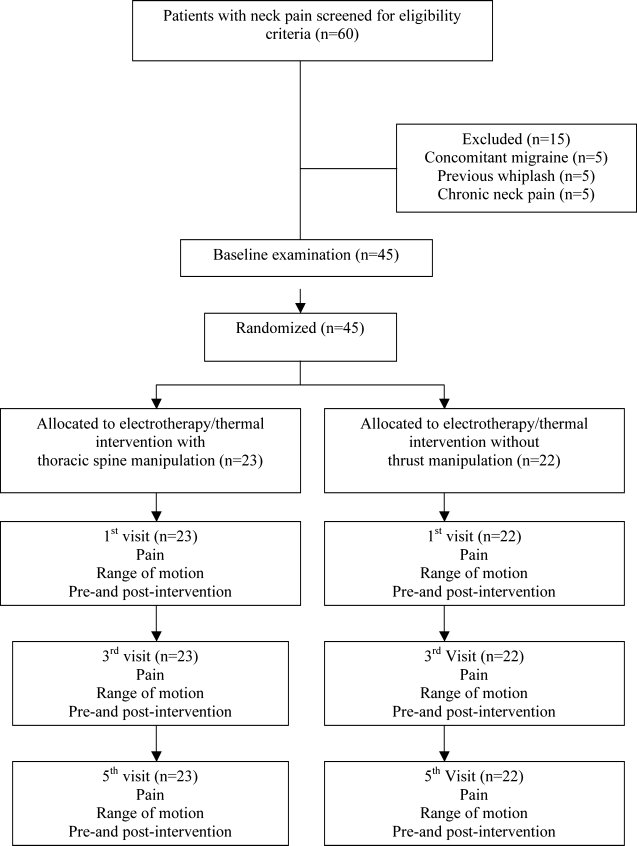
All subjects in both groups completed the study, and a complete set of data was collected for pre- and post-intervention scores on both outcome measures for both groups at visits # 1, 3, and 5 (Figure 2).
FIGURE 2.
Flow diagram of subjects throughout the course of the study.
Outcomes
The repeated-measures ANOVA showed significant differences for pain (F = 181.4; P < 0.001), flexion (F = 113.2; P < 0.001), extension (F = 68.5; P < 0.001), right (F = 60.5; P < 0.001) and left (F = 84.3; P < 0.001) rotations, and right (F = 52.8; P < 0.001) and left (F = 64.1; P < 0.001) lateral-flexions for the experimental group. However, for the control group, the ANOVA revealed significant differences only for pain (F = 16.6; P < 0.001) and not for any cervical motion: flexion (F = 0.6; P = 0.6), extension (F = 0.4; 0.5), right and (F = 0.9; P = 0.3) left rotation (F = 0.8; P = 0.5), and right and left lateral flexion (F = 0.6; P = 0.4). Interpreting these statistical data, we noted that the experimental group showed significant improvements in both pain and cervical mobility, whereas the control group only got improvement for the pain outcome measure throughout the course of the study (Tables 2–4).
TABLE 2.
Mean pre-/post-intervention and change scores (95% Ci) for pain and mobility for session #1.
| Outcome Group | Pre-Intervention | Post-Intervention | Within-Group Change Scores | Between-Group Difference in Change Scores |
|---|---|---|---|---|
| Pain (0–100 mm) | ||||
| Electro/thermal program | 52.7 (50.2, 55.2) | 48.8 (46.6, 52.9) | −3.8 (−2.9, −4.8) | 9.4 (8.9, 11.7) |
| Trust manipulation | 54.7 (51.1, 58.3) | 41.4 (37.2, 45.4) | −13.3 (−12.3, −14.1) | |
| Cervical Flexion (deg) | ||||
| Rlectro/thermal program | 44.4 (42.2, 46.6) | 44.8 (42.4, 47.2) | 0.4 (−0.2, 1.1) | 4.8 (3.9, 5.7) |
| Trust manipulation | 45.2 (43.2, 47.2) | 50.4 (48.4, 52.5) | 5.2 (4.6, 5.9) | |
| Cervical Extension (deg) | ||||
| Electro/thermal program | 58.8 (56.3, 61.3) | 59.8 (57.4, 62.3) | 1.0 (0.1, 1.8) | 4.4 (3.4, 5.7) |
| Trust manipulation | 59.2 (55.6, 62.7) | 64.6 (61.2, 68.3) | 5.4 (4.7, 6.4) | |
| Cervical Right Cervical Rotation (deg) | ||||
| Electro/thermal program | 56.1 (53.2, 59.0) | 56.6 (53.8, 59.4) | 0.5 (−0.2, 1.3) | 4.0 (2.8, 5.1) |
| Trust manipulation | 55.4 (52.7, 58.9) | 59.9 (56.5, 58.9) | 4.5 (3.4, 5.8) | |
| Cervical Lef Cervical Rotation (deg) | ||||
| Electro/thermal program | 57.8 (55.4, 60.2) | 58.2 (55.7, 60.6) | 0.4 (−0.4, 1.1) | 3.9 (2.9, 4.8) |
| Trust manipulation | 58.2 (56.5, 60.9) | 62.5 (59.5, 65.5) | 4.3 (3.6, 5.1) | |
| Cervical Right Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 39.4 (37.3, 41.6) | 40.3 (38.1, 42.4) | 0.4 (0.2, 1.5) | 3.7 (2.5, 4.2) |
| Trust manipulation | 36.2 (35.9, 40.4) | 40.3 (37.9, 42.6) | 4.1 (3.4, 4.8) | |
| Cervical Lef Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 40.2 (38.2, 42.2) | 40.7 (38.8, 42.6) | 0.5 (0.0, 1.1) | 2.9 (2.3, 3.8) |
| Trust manipulation | 39.2 (37.0, 41.0) | 42.6 (40.5, 44.7) | 3.4 (3.0, 4.1) | |
TABLE 4.
Mean pre-/post-intervention and change scores (95% Ci) for pain and mobility for session #5.
| Outcome Group | Pre-Intervention | Post-Intervention | Within-Group Change Scores | Between-Group Difference in Change Scores |
|---|---|---|---|---|
| Pain (0–100 mm) | ||||
| Electro/thermal program | 48.7 (45.2, 52.4) | 44.7 (42.3, 47.2) | −4.0 (−3.4, −5.4) | 11.2 (9.9, 12.9) |
| Trust manipulation | 35.4 (30.7, 40.2) | 20.2 (16.8, 23.6) | −15.2 (−13.7, −16.8) | |
| Cervical Flexion (deg) | ||||
| Electro/thermal program | 44.9 (42.4, 47.4) | 44.8 (43.0, 46.7) | 0.1 (0.0, 0.7) | 5.7 (4.8, 6.4) |
| Trust manipulation | 51.8 (49.3, 54.3) | 57.6 (55.4, 59.8) | 5.8 (4.8, 6.2) | |
| Cervical Extension (deg) | ||||
| Electro/thermal program | 59.2 (57.0, 61.5) | 59.0 (57.0, 61.0) | −0.2 (−0.5, 1.0) | 6.6 (5.8, 7.7) |
| Trust manipulation | 64.7 (60.9, 68.5) | 71.1 (67.9, 74.3) | 6.4 (5.3, 6.9) | |
| Cervical Right Cervical Rotation (deg) | ||||
| Electro/thermal program | 55.7 (53.3, 58.1) | 54.7 (52.2, 57.3) | −1.0 (−2.1, 1.3) | 6.5 (5.1, 7.2) |
| Trust manipulation | 61.0 (57.6, 64.4) | 66.5 (63.5, 69.6) | 5.5 (5.0, 6.3) | |
| Cervical Lef Cervical Rotation (deg) | ||||
| Electro/thermal program | 57.3 (54.8, 59.7) | 57.2 (55.3, 59.1) | −0.1 (−1.1, 1.0) | 5.6 (4.9, 7.2) |
| Trust manipulation | 63.6 (61.1, 66.0) | 69.1 (66.8, 71.3) | 5.5 (4.3, 6.0) | |
| Cervical Right Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 40.5 (38.7, 42.4) | 39.9 (38.3, 41.4) | −0.6 (−1.2, 1.1) | 5.9 (4.2, 6.9) |
| Trust manipulation | 42.7 (40.5, 44.9) | 48.0 (46.0, 50.0) | 5.3 (3.9, 6.1) | |
| Cervical Lef Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 40.6 (38.4, 42.9) | 39.4 (38.0, 40.7) | −1.2 (−1.4, 1.8) | 6.9 (5.1, 8.2) |
| Trust manipulation | 43.4 (41.2, 45.6) | 49.1 (47.0, 51.1) | 5.7 (4.4, 6.4) | |
Further, the ANOVA revealed that within-session change scores of each session were not significantly different when comparing the three sessions for the experimental group (pain: F = 2.1, P = 0.2; flexion: F = 0.3, P = 0.7; extension: F = 0.4, P = 0.6; right rotation: F = 1.0, P = 0.4; left rotation: F = 2.2, P = 0.2; right lateral-flexion: F = 0.4, P = 0.6; or left lateral-flexion: F = 1.6, P = 0.3). The within-session changes for the three sessions where outcomes were collected in the control group were also not significantly different (pain: F = 1.4, P = 0.3; flexion: F = 0.7, P = 0.4; extension: F = 1.1, P= 0.4; right rotation: F = 0.1, P = 0.9; left rotation: F = 1.7, P = 0.3; right lateral-flexion: F = 0.9, P = 0.4; or left lateral-flexion: F = 0.8, P = 0.5) groups (Tables 2–4).
Finally, the 2-way ANOVA showed significant between-group differences for within-session changes with regard to pain (F = 38.9, P< 0.001), flexion (F = 33.5, P < 0.001), extension (F = 18.5, P< 0.001), right (F = 17.7, P < 0.001) and left rotations (F = 14.4, P < 0.001), and right (F = 18.5, P < 0.001) and left lateral flexions (F = 15.6, P < 0.001). Again to interpret these statistical data, within-session change scores in each session were significantly higher in the experimental group as compared to the control group (Tables 2–4).
Discussion
The results of this secondary analysis of data collected during our original study on the effects of thoracic manipulation in patients with acute mechanical neck pain17 demonstrated that thoracic thrust manipulation did not lead to tolerance (or diminishing therapeutic return) with 3 repeated applications. In the experimental group, within-session improvements in both neck pain and mobility were similar and consistent after each time that the technique was applied. Also, adding thrust manipulation was clearly superior to the electro- and thermotherapy program alone. Between-group comparisons of within-session changes for the same sessions showed significantly higher improvements for pain and mobility in the experimental group on all three sessions. In addition, it should be noted that on each session, within-session change scores for neck pain achieved by the thoracic manipulation group exceeded the MCID for the VAS, which has been established as 9–11 mm21,22. In fact, even the lower bound estimate exceeded the MCID for within-session for visits 1, 3, and 5. Further improvements were maintained between visits, and between visits 1 and 3 exceeded the MCID (11.3mm) and were approaching the MCID between visits 3 and 5 (8mm). However, we would expect that it might take multiple manipulation sessions to assure that the lower bound estimate in change in pain exceeds the MCID and is maintained at follow-up. Therefore, 1 session of thoracic manipulation may not be sufficient to achieve a change in pain that exceeds the MCID that is maintained at follow-up. However, the results of this study demonstrate that with repeated applications (up to 3 sessions) may result in continued within-session improvements in pain levels and significantly better outcomes than the comparison group. We only performed thoracic spine thrust manipulation once per week, which may be a limitation to the current study. It is possible that changes in tolerance might occur if manipulation was repeated more than once per week. However, future studies are necessary to investigate this. Nevertheless, we should consider that the MCID for changes in the VAS was investigated in patients with a menagerie of disorders but not neck pain. Only one recent study determined the MCID for a numerical pain rate scale, but not VAS, in patients with neck pain25. Finally, no MCID has been reported for neck mobility as measured in this study, and future studies are needed to determine this psychometric property. The most relevant question is how to interpret these findings. Evidence for the treatment of neck pain with electrotherapy is lacking or, at best, conflicting26,27. This limits the validity of our control intervention as a realistic comparison and weakens confidence in the comparative effectiveness for our experimental intervention of thoracic spine thrust manipulation. However, previous research has shown superior results for thrust compared to the arguably more realistic comparison treatment of non-thrust thoracic spine manipulation16. Therefore, in our opinion, the results of the current study further add to the growing body of evidence supporting the effectiveness of thoracic spine manipulation in the management of patients with mechanical neck pain10-13,17.
More relevant is the fact that the absence of tolerance to repeated applications of thoracic thrust manipulation provides preliminary evidence and support for the common clinical practice within physical therapy of including thrust manipulations to the same region in consecutive sessions.
Indirectly, the findings of this study also may shed some light on the mechanism of action of thrust manipulation. A number of theoretical constructs surround the biological plausibility of why thoracic spine thrust manipulation may be beneficial in patients with neck pain. Both biomechanical and neurophysiological (either segmental or central) mechanisms have been proposed. Mobility restrictions in the thoracic spine have been associated with neck pain28–30, and it is certainly possible that spinal manipulative therapy has a mechanical effect on the treated segments and thereby indirectly on the painful neck region. However, a solely biomechanical explanation would have us likely find tolerance to repeated applications of thrust manipulation, reflecting the fact that increasingly lasting mobility changes to the targeted segments are achieved. In contrast, the lack of tolerance to repeated applications in the current study might be related to a mechanism of action for thrust manipulation involving the stimulation of descending inhibitory endogenous systems. Previous studies showing that sympatho-excitation accompanying manipulative procedures is directly correlated with the hypoalgesic effect31, indicating the presence of bilateral mechanical hypoalgesia with unilateral interventions32 and showing hypoalgesic effects not reversible by the application of naloxone33. These suggest that non-opioid descending inhibitory systems are at least partly responsible for the hypoalgesic effect of manipulative interventions. Although we are limited in our extrapolations due to the limited number of manipulative interventions provided in this current study, Wright34 has associated the absence of tolerance with repeated manual interventions to the role of descending mechanisms in manipulation-induced hypoalgesia. We acknowledge that this hypoalgesic effect is but one explanation for the observed positive outcomes on pain and mobility in the present study and that a similar study looking at specific indicators of hypoalgesia is required before strong statements in this regard are warranted.
In our discussion of the equivocal research base for the control intervention and the unwarranted extrapolation of pain and mobility outcome measures to hypoalgesia, we have already discussed some of the limitations of this study. We are also aware that the fact that one clinician performed all manipulations somewhat limits the generalizability of the results. In addition, there exist many different thoracic spine thrust techniques and we cannot make any conclusions about the clinical benefits of other thoracic spine thrust techniques. On the other hand, the particular technique selected might not be as critical as identifying the proper patient on whom to use the technique35–37. We also realize that this hypothesis requires further investigation. Additionally, since thoracic thrust manipulation does not exhibit tolerance to repeated applications, future studies should investigate in detail the dose-response relationship for thrust manipulation; i.e., how many sessions of thoracic thrust manipulations will optimize patient outcome? This also needs to occur in populations of patients with chronic mechanical neck pain.
Conclusion
The results of the current analysis suggest that repeated applications of thoracic spine thrust manipulation did not lead to tolerance with regard to magnitude of within-session changes in pain and cervical range of motion in patients with acute mechanical neck pain. Future studies should investigate the dose-response relationship of thoracic spine thrust manipulation in varied populations of patients with mechanical neck pain.
TABLE 3.
Mean pre-/post-intervention and change scores (95% Ci) for pain and mobility for session #3.
| Outcome Group | Pre-Intervention | Post-Intervention | Within-Group Change Scores | Between-Group Difference in Change Scores |
|---|---|---|---|---|
| Pain (0–100 mm) | ||||
| Electro/thermal program | 52.0 (49.0, 54.9) | 47.4 (44.4, 50.2) | −4.6 (−3.3, −6.1) | 8.6 (7.0, 10.8) |
| Trust manipulation | 43.4 (38.9, 47.9) | 29.8 (25.3, 34.4) | −13.6 (−12.2, −15.0) | |
| Cervical Flexion (deg) | ||||
| Electro/thermal program | 44.4 (42.2, 46.6) | 45.0 (42.6, 47.4) | 0.6 (0.0, 1.3) | 4.4 (3.5, 5.3) |
| Trust manipulation | 48.9 (46.6, 51.3) | 54.0 (51.6, 56.4) | 5.1 (4.4, 5.6) | |
| Cervical Extension (deg) | ||||
| Electro/thermal program | 59.2 (56.5, 61.8) | 57.6 (51.8, 63.3) | −1.6 (−5.0, 1.8) | 7.6 (2.9, 12.4) |
| Trust manipulation | 61.9 (58.2, 65.7) | 67.9 (64.1, 71.7) | 6.0 (2.7, 9.3) | |
| Cervical Right Cervical Rotation (deg) | ||||
| Electro/thermal program | 55.4 (52.8, 57.9) | 55.9 (53.4, 58.5) | 0.5 (0.0, 1.2) | 3.5 (2.6, 4.3) |
| Trust manipulation | 59.2 (55.9, 62.5) | 63.1 (59.8, 66.5) | 3.9 (3.3, 4.5) | |
| Cervical Lef Cervical Rotation (deg) | ||||
| Electro/thermal program | 57.8 (55.5, 60.1) | 56.2 (49.9, 63.7) | −1.6 (−2.1, 1.2) | 6.3 (5.2, 7.8) |
| Trust manipulation | 60.9 (58.2, 63.6) | 65.6 (62.8, 68.3) | 4.7 (4.1, 5.3) | |
| Cervical Right Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 40.3 (38.3, 42.2) | 40.7 (38.7, 42.8) | 0.4 (0.3, 1.2) | 3.9 (2.7, 4.8) |
| Trust manipulation | 40.4 (38.2, 42.7) | 44.7 (42.1, 47.3) | 4.3 (3.5, 5.0) | |
| Cervical Lef Cervical Lateral Flexion (deg) | ||||
| Electro/thermal program | 40.8 (38.8, 42.8) | 41.8 (39.9, 43.7) | 1.0 (0.3, 1.7) | 3.3 (2.2, 4.3) |
| Trust manipulation | 41.1 (39.1, 43.2) | 45.4 (43.2, 47.6) | 4.3 (3.5, 5.0) | |
REFERENCES
- 1.Hogg-Johnson S, Van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population. Spine. 2008;33:S39–S51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 2.Côté P, Cassidy J, Carroll L. The factors associated with neck pain and its related disability in the Saskatchewan population. Spine. 2000;25:1109–1117. doi: 10.1097/00007632-200005010-00012. [DOI] [PubMed] [Google Scholar]
- 3.Nygren A, Berglund A, von Koch M. Neckand-shoulder pain, an increasing problem: Strategies for using insurance material to follow trends. [PubMed] [Google Scholar]
- 4.Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: A systematic review. Pain. 1998;77:1–13. doi: 10.1016/S0304-3959(98)00058-X. [DOI] [PubMed] [Google Scholar]
- 5.Gore DR, Sepic SB, Gardner GM, et al. Neck pain: A long-term follow-up of 205 patients. Spine. 1987;12:1–5. doi: 10.1097/00007632-198701000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Douglass AB, Bope ET. Evaluation and treatment of posterior neck pain in family practice. J Am Board Fam Pract. 2004;17:S13–S22. doi: 10.3122/jabfm.17.suppl_1.s13. [DOI] [PubMed] [Google Scholar]
- 7.Boissonnault WG. Prevalence of comorbid conditions, surgeries, and medication use in a physical therapy outpatient population: A multi-centered study. J Orthop Sports Phys Ther. 1999;29:506–519. doi: 10.2519/jospt.1999.29.9.506. discussion 520-525. [DOI] [PubMed] [Google Scholar]
- 8.Wright A, Mayer TG, Gatchel RJ. Outcomes of disabling cervical spine disorders in compensation injuries: A prospective comparison to tertiary rehabilitation response to chronic lumbar spine disorders. Spine. 1999;24:178–183. doi: 10.1097/00007632-199901150-00020. [DOI] [PubMed] [Google Scholar]
- 9.Childs JD, Fritz JM, Piva SR, Whitman JM. Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther. 2004;34:686–700. doi: 10.2519/jospt.2004.34.11.686. [DOI] [PubMed] [Google Scholar]
- 10.Cleland JA, Childs JD, Fritz JM, et al. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: Use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 11.Cleland JA, Childs JD, McRae M, et al. Immediate effects of thoracic manipulation in patients with neck pain: A randomized clinical trial. Man Ther. 2005;10:127–135. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Fernández-de-las-Peñas C, Palomeque-delCerro L, Rodriguez-Blanco C, Gomezconesa A, Miangolarra-Page JC. Changes in neck pain and active range of motion after a single thoracic spine manipulation in subjects presenting with mechanical neck pain: A case series. J Manipulative Physiol Ther. 2007;30:312–320. doi: 10.1016/j.jmpt.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 13.González-Iglesias J, Fernández-de-las-Pe-ñas C, Cleland JA, Albuquerque-Sendín F, Palomeque-del-Cerro L, Méndez-Sánchez R. Inclusion of thoracic spine thrust manipulation into an electrotherapy program for the management of patients with acute mechanical neck pain: A randomized clinical trial. Man Ther. 2008 doi: 10.1016/j.math.2008.04.006. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 14.Paungmali A, Vicenzino B, Smith M. Hypoalgesia induced by elbow manipulation in lateral epicondylalgia does not exhibit tolerance. J Pain. 2003;4:448–454. doi: 10.1067/s1526-5900(03)00731-4. [DOI] [PubMed] [Google Scholar]
- 15.Bolton P, Budgell B. Spinal manipulation and spinal mobilization influence different axial sensory beds. Med Hypotheses. 2006;66:258–262. doi: 10.1016/j.mehy.2005.08.054. [DOI] [PubMed] [Google Scholar]
- 16.Cleland JA, Glynn P, Whitman J, Eberhart SL, MacDonald C, Childs JD. Short-term response of thoracic spine thrust versus non-thrust manipulation in patients with mechanical neck pain: A randomized clinical trial. Phys Ther. 2007;87:431–440. doi: 10.2522/ptj.20060217. [DOI] [PubMed] [Google Scholar]
- 17.González-Iglesias J, Fernández-de-las-Pe-ñas C, Cleland J, Gutiérrez-Vega MR. Thoracic spine manipulation for the management of patients with neck pain: A randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:20–27. doi: 10.2519/jospt.2009.2914. [DOI] [PubMed] [Google Scholar]
- 18.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for classification of fibromyalgia: Report of the multi-center criteria committee. Arthritis Rheum. 1990;33:160–170. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 19.Gibbons P, Tehan P. Manipulation of the Spine, Thorax and Pelvis. Edinburgh, UK: Churchill Livingstone; 2000. [Google Scholar]
- 20.Bijur P, Silveer W, Gallagher JE. Reliability of the visual analogue scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 21.Bird SB, Dickson EW. Clinically significant changes in pain along the visual analogue scale. Ann Emerg Med. 2001;36:639–643. doi: 10.1067/mem.2001.118012. [DOI] [PubMed] [Google Scholar]
- 22.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analogue scale. Ann Emerg Med. 2001;38:633–638. doi: 10.1067/mem.2001.118863. [DOI] [PubMed] [Google Scholar]
- 23.Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Forward head posture and neck mobility in chronic tension-type headache: A blinded, controlled study. Cephalalgia. 2006;26:314–319. doi: 10.1111/j.1468-2982.2005.01042.x. [DOI] [PubMed] [Google Scholar]
- 24.Cleland JA, Childs JD, Fritz JM, Whitman M. Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil. 2006;87:1388–1395. doi: 10.1016/j.apmr.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. doi: 10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 26.Brosseau L, Tugwell P, Wells GA. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain. Phys Ther. 2001;81:1701–1717. [PubMed] [Google Scholar]
- 27.Kroeling P, Gross A, Houghton PE, Cervical Overview Group Electrotherapy for neck disorders. Cochrane Database Syst Rev. 2005;2 doi: 10.1002/14651858.CD004251.pub3. CD004251. [DOI] [PubMed] [Google Scholar]
- 28.Norlander S, Gustavsson BA, Lindell J, et al. Reduced mobility in the cervico-thoracic motion segment. A risk factor for musculoskeletal neck-shoulder pain: A two-year prospective follow-up study. Scand J Rehabil Med. 1997;29:167–174. [PubMed] [Google Scholar]
- 29.Norlander S, Nordgren B. Clinical symptoms related to musculoskeletal neck-shoulder pain and mobility in the cervico-thoracic spine. Scand J Rehabil Med. 1998;30:243–251. doi: 10.1080/003655098443995. [DOI] [PubMed] [Google Scholar]
- 30.Norlander S, ste-Norlander U, Nordgren B, et al. Mobility in the cervico-thoracic motion segment: An indicative factor of musculoskeletal neck-shoulder pain. Scand J Rehabil Med. 1996;28:183–192. [PubMed] [Google Scholar]
- 31.Vicenzino B, Collins D, Benson H, et al. An investigation of the interrelationship between manipulative therapy-induced hypoalgesia and sympatho-excitation. J Manipulative Physiol Ther. 1998;21:448–453. [PubMed] [Google Scholar]
- 32.Fernández-de-las-Peñas C, Pérez-de-Heredia M, Brea-Rivero M, Miangolarra-Page JC. Immediate effects on pressure pain threshold following a single cervical spine manipulation in healthy subjects. J Orthop Sports Phys Ther. 2007;37:325–329. doi: 10.2519/jospt.2007.2542. [DOI] [PubMed] [Google Scholar]
- 33.Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Naloxone fails to antagonize initial hypoalgesic effect of a manual therapy treatment for lateral epicondylalgia. J Manipulative Physiol Ther. 2004;27:180–185. doi: 10.1016/j.jmpt.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 34.Wright A. Pain-relieving effects of cervical manual therapy. In: Grant R, editor. Physical Therapy of the Cervical and Thoracic Spine. Edinburgh, UK: Churchill Livingstone; 2002. [Google Scholar]
- 35.Chiradejnant A, Latimer J, Maher CG, et al. Does the choice of spinal level treated during postero-anterior mobilisation affect treatment outcomes? Phys Theor Pract. 2002;18:165–174. [Google Scholar]
- 36.Chiradejnant A, Maher CG, Latimer J, et al. Efficacy of «therapist-selected» versus «randomly selected» mobilisation techniques for the treatment of low back pain: A randomised controlled trial. Aust J Physiother. 2003;49:233–241. doi: 10.1016/s0004-9514(14)60139-2. [DOI] [PubMed] [Google Scholar]
- 37.Flynn TW. There's more than one way to manipulate a spine. J Orthop Sports Phys Ther. 2006;36:198–199. doi: 10.2519/jospt.2006.0105. [DOI] [PubMed] [Google Scholar]