Abstract
Introduction:
Much of the existing research on smoking outcome expectancies has been guided by the Smoking Consequences Questionnaire (SCQ ). Although the original version of the SCQ has been modified over time for use in different populations, none of the existing versions have been evaluated for use among Spanish-speaking Latino smokers in the United States.
Methods:
The present study evaluated the factor structure and predictive validity of the 3 previously validated versions of the SCQ—the original, the SCQ-Adult, and the SCQ-Spanish, which was developed with Spanish-speaking smokers in Spain—among Spanish-speaking Latino smokers in Texas.
Results:
The SCQ-Spanish represented the least complex solution. Each of the SCQ-Spanish scales had good internal consistency, and the predictive validity of the SCQ-Spanish was partially supported. Nearly all the SCQ-Spanish scales predicted withdrawal severity even after controlling for demographics and dependence. Boredom Reduction predicted smoking relapse across the 5- and 12-week follow-up assessments in a multivariate model that also controlled for demographics and dependence.
Discussion:
Our results support use of the SCQ-Spanish with Spanish-speaking Latino smokers in the United States.
Introduction
Outcome expectancies for drug use have been conceptualized as beliefs about the positive and negative consequences of use and are included within influential theoretical models of addiction as critical determinants of drug use motivation (Baker, Morse, & Sherman, 1986; Goldman, Brown, & Christensen, 1987; Marlatt & Gordon, 1985; Niaura, Goldstein, & Abrams, 1991; Witkiewitz & Marlatt, 2004). Most research on smoking outcome expectancies has been conducted with predominantly White heavily dependent smokers (Copeland, Brandon, & Quinn, 1995; Wetter et al., 1994) or college students (Brandon & Baker, 1991; Cepeda-Benito & Ferrer, 2000; Reig-Ferrer & Cepeda-Benito, 2007). However, important racial/ethnic differences in smoking prevalence, patterns, cessation, and health consequences between Whites and racial/ethnic minorities have been well documented (Centers for Disease Control and Prevention [CDC], 2008; U.S. Department of Health and Human Services [USDHHS], 1998), and research addressing the uptake, maintenance, and cessation of tobacco use among minority populations in the United States has been identified as an important priority for future research (Fiore et al., 2000; USDHHS, 2001).
Latinos are the largest and fastest growing minority population in the United States (Bernstein, 2006), and Latino smokers merit special attention because they diverge from other racial/ethnic minority groups in important ways. Despite having a lower prevalence of smoking (13.3%; CDC, 2008) and a lower smoking rate than non-Latino Whites (Fagan, Moolchan, Lawrence, Fernander, & Ponder, 2007; USDHHS, 1998; Zhu, Pulvers, Zhuang, & Baezconde-Garbanati, 2007), Latinos suffer severe adverse health consequences from tobacco use (CDC, 2007). Five of the 10 leading causes of mortality among Latinos are smoking related (i.e., heart disease, cancer, stroke, birth defects, and chronic respiratory diseases; CDC, 2004). These data underscore the importance of understanding the mechanisms driving tobacco dependence and cessation among Latino smokers in the United States.
The Smoking Consequences Questionnaire
Much of the research on smoking outcome expectancies has been conducted with the Smoking Consequences Questionnaire (SCQ; Brandon & Baker, 1991). Since the SCQ was introduced, several versions have been developed and validated for use with specific populations (Cepeda-Benito & Ferrer, 2000; Copeland et al., 1995; Lewis-Esquerre, Rodrigue, & Kahler, 2005; Myers, McCarthy, MacPherson, & Brown, 2003). The original SCQ was developed with college students (Brandon & Baker) and comprises four factors: Negative Consequences, Positive Reinforcement–Sensory Satisfaction, Negative Reinforcement–Negative Affect Reduction, and Appetite–Weight Control. The factor structure and predictive validity were subsequently cross–validated using a large sample of older, more heavily addicted treatment seeking smokers (Wetter et al., 1994).
Copeland and colleagues (1995) subsequently developed the SCQ-Adult to assess expectancies in older, more nicotine-dependent smokers. It comprises 10 factors: Negative Affect Reduction, Stimulation/State Enhancement, Health Risk, Taste/Sensorimotor Manipulation, Social Facilitation, Weight Control, Craving/Addiction, Negative Physical Feelings, Boredom Reduction, and Negative Social Impression.
A third version, the SCQ-Spanish, was developed with Spanish-speaking college smokers in Spain (Cepeda-Benito & Ferrer, 2000) and subsequently cross-validated in a sample of older, heavier smokers in Spain (Reig-Ferrer & Cepeda-Benito, 2007). The SCQ-Spanish comprises eight factors: Negative Affect Reduction, Stimulation/State Enhancement, Health Risk, Taste/Sensorimotor Manipulation, Social Facilitation, Weight Control, Craving/Addiction, and Boredom Reduction. However, because the SCQ-Spanish has not been evaluated for use with Spanish-speaking Latino smokers in the United States, its appropriateness for use with this population is unclear. It is notable that smokers in Spain differ in important ways from Latino smokers in the United States. Smoking prevalence is much higher in Spain (36.4% among men and 27.1% among women; World Health Organization, 2005) than among Latinos in the United States (18.0% among men and 8.3% among women; CDC, 2008). In addition, smoking among Latinos in the United States also tends to increase as individuals become more acculturated (Abraido-Lanza, Chao, & Gates, 2005; Marin, Marin, Perez-Stable, Sabogal, & Otero-Sabogal, 1989; Perez-Stable et al., 2001). Therefore, despite a shared language, important social, cultural, and contextual factors may differentially influence smoking outcome expectancies across the two populations of Spanish-speaking smokers.
Expectancies, withdrawal, and relapse
It is hypothesized that strong expectancies for the positive consequences of smoking (particularly negative affect reduction expectancies) will be positively associated with withdrawal severity and relapse over time because these expectancies are likely to be associated with a greater loss of reinforcement after quitting. Wetter and colleagues (1994) found that all the positive expectancy scales from the original SCQ predicted withdrawal severity after controlling for treatment condition, demographics, and dependence. Similarly, Copeland and colleagues (1995) found that relapsers held significantly stronger positive expectancies posttreatment compared with abstainers. The rationale for this hypothesis is also supported by theory. Baker, Piper, McCarthy, Majeskie, and Fiore's (2004) reformulation of the negative reinforcement model of drug addiction proposes that negative affect is the single most important motivational factor driving addictive substance use, and negative affect is conceptualized as a hallmark of withdrawal. Furthermore, empirical data indicate that negative affect (Brandon, 1994; Kenford et al., 2002; Piasecki et al., 2000; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996) and affective vulnerability (Borrelli, Bock, King, Pinto, & Marcus, 1996; Glassman et al., 1990; Niaura et al., 1999; Wetter et al., 1999) enhance the risk of relapse. Wetter and colleagues (1994) found that strong expectancies for the negative affect reduction properties of smoking predicted both withdrawal severity and relapse.
On the other hand, expectancies for the negative consequences of smoking (e.g., health risks) are hypothesized to be negatively associated with withdrawal severity and relapse over time because individuals may be less likely to return to smoking if they expect to suffer serious health consequences resulting from continued smoking. This is consistent with empirical data indicating that expectancies concerning the negative consequences of smoking predict cessation success (Wetter et al., 1994). Specifically, strong beliefs concerning the negative consequences of smoking are negatively associated with relapse (Gibbons, Eggleston, & Benthin, 1997; Gibbons, McGovern, & Lando, 1991; Wetter et al., 1994). We do not have a priori hypotheses concerning the potential association of expectancies for the negative consequences of smoking with withdrawal. However, no studies have examined associations of expectancies with withdrawal or cessation outcomes among Latino smokers.
Study purpose
This study sought to address the question of which of three previously validated versions of the SCQ—the original, the SCQ-Adult, or the SCQ-Spanish—is most appropriate for use with Spanish-speaking Latino smokers in the United States. This goal was accomplished by testing which version best fit the data obtained from a community-based sample of Spanish-speaking Latino smokers residing in Texas. Confirmatory factor analysis (CFA) was used to evaluate which version best fit the data. The predictive validity of the best fitting SCQ version was also evaluated by examining the utility of the measure in predicting withdrawal and relapse over time. Specifically, the SCQ scales supported by the CFA were used in univariate and multivariate models to predict withdrawal severity across baseline, 5-week, and 12-week follow-ups and smoking relapse across 5- and 12-week follow-ups.
Methods
Study design and participants
Participants were Spanish-speaking Latino smokers in Texas who participated in “Adiós al Fumar,” a two-group randomized clinical trial that evaluated the efficacy of a culturally tailored telephone delivered smoking cessation intervention targeted to Spanish-speaking smokers. Participants were recruited through calling the Spanish-language smoking cessation quitline provided by the National Cancer Institute's Cancer Information Service (CIS). Inclusion criteria were that participants call the CIS to request smoking cessation assistance in Spanish, live in Texas, be ≥18, and self-identify as a current smoker. The sample comprised 297 individuals (84% participation rate). Follow-up assessments were conducted via telephone 5 and 12 weeks following study enrollment. For a detailed description of recruitment, treatments, and cessation outcomes, see Wetter and colleagues (2007).
Measures
Demographics included age, gender, education, marital status, employment, household income, ethnicity, immigrant status, and language spoken at home. All variables except age and education were dichotomized.
Nicotine dependence was assessed using the Heaviness of Smoking Index (HSI; Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989). The HSI comprises two items from the Fagerström Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991), cigarettes per day (CPD) and time to the first cigarette after waking (TTFC). The HSI has fair internal consistency (α = .63; Etter, 2005) and the TTFC item predicts relapse (Baker et al., 2007).
Smoking Consequences Questionnaire items.
Items comprising the original SCQ (50 items), the SCQ-Adult (55 items), and the SCQ-Spanish (40 items) were administered as a single measure. Because many of the items are identical across the three versions, the total item pool comprised 66 items.
Withdrawal.
The Wisconsin Smoking Withdrawal Scale (WSWS; Welsch et al., 1999) includes subscales for anger, anxiety, sadness, concentration difficulty, craving, hunger, and sleep. All have excellent internal consistency and demonstrate clear increases as a function of withdrawal (Welsch et al., 1999; Wetter et al., 2000).
Smoking relapse was defined as any self-report of smoking during the 7 days prior to the 5- and 12-week assessments. Self-reported abstinence was not biochemically verified because all assessments and treatment were conducted by telephone. Relapse analyses were based on participants who provided data at follow-up. Follow-up rates at 5 and 12 weeks were 91% and 83%, respectively.
Translation of measures into Spanish
Translation of all study measures and materials into Spanish followed recommended procedures (Brislin, Lonner, & Thorndike, 1973; Swaine-Verdier, Doward, Hagell, Thorsen, & McKenna, 2004). The two English versions of the SCQ (i.e., the original and the SCQ-Adult) were translated into Spanish by members of the research team who were native Spanish speakers. Bilingual native English speakers translated the items back to English. In addition, the first drafts of the Spanish items were revised by laypersons who were monolingual Spanish speakers. Next, the measure was evaluated and revised by bilingual licensed translators to ensure that items were linguistically and culturally appropriate. Finally, items were reviewed and revised by all individuals who participated in the translation process, and these individuals determined the final version by consensus.
Data analysis
Confirmatory factor analysis with maximum likelihood estimation was used to assess the three SCQ versions. In an attempt to assess various aspects of model fit, a battery of overall fit indices was considered, including: (a) the chi-square statistic, (b) root mean square error of approximation (RMSEA), (c) non-normed fit index (NNFI), (d) comparative fit index (CFI), and (e) standardized root mean square residual (SRMR). Selection of the best fitting model was based on the overall fit indices indicating good fit and model complexity (Kline, 1998). LISREL, version 8.54, was used to perform the CFA (Joreskog & Sorbom, 1996). Internal consistency reliability of the scales was evaluated by calculating Cronbach's alphas. Next, point biserial correlations were used to examine associations of SCQ scales at baseline with the HSI.
A series of generalized linear mixed model (GLMM) regressions examined how well the SCQ scales predicted smoking withdrawal and relapse over time. GLMM is a flexible analytic approach commonly used in social science research. GLMM is well suited to handling missing data (Brown & Prescott, 1999) and designed to handle repeated measures that are correlated within subjects. It is common in smoking cessation studies to code all missing outcome data as smoking. However, this approach is conservative and may create bias and error, particularly when a fair proportion of the data is missing (Hughes et al., 2003). Because GLMM is very adept at handling missing data, we chose not to impute values for missing abstinence data. The first GLMM models controlled only for time and treatment condition. The second set of models controlled for time, treatment condition, and demographics (i.e., age, gender, marital status, education, employment status, household income, ethnicity, immigrant status, and language spoken at home). The third set of models controlled for time, treatment condition, demographics, and dependence (i.e., CPD and TTFC, in minutes).
Results
Participant characteristics
Participants (N = 297) were in their early 40s on average, and slightly more than half were male (54.9%). The majority were married (66.2%), immigrants (93.4%), of Mexican ethnicity/origin (66.0%), spoke only Spanish in the home (61.3%), and had an annual household income <$20,000 (56.3%). On average, participants had less than a high school degree (mean years of education = 10.86; SD = 4.05). Just under half smoked <10 cigarettes/day (46.5%) and just over half smoked within an hour of waking (51.6%).
Confirmatory factor analysis was used to test which version of the SCQ best fit the data. A summary of the overall fit indices for each version is provided in Table 1. Results indicated that both the SCQ-Adult and the SCQ-Spanish provided a better overall fit than the original SCQ. The factor structures of both the SCQ-Adult and the SCQ-Spanish represented well-fitted solutions, with each fulfilling the criteria of good fit for four of the five indices (i.e., RMSEA, NNFI, CFI, and SRMR). However, the SCQ-Spanish represents the least complex solution because it has the fewest items and fewest subscales. As such, it was used for all further analyses.
Table 1.
Confirmatory factor analysis results for the SCQ: Three hypothesized factor structures
| Goodness of fit indices | College (original SCQ) | Adult (SCQ-Adult) | Spanish (SCQ-Spanish) | Criteria for good fita |
| χ2 (df), p value | 4262 (1121), <0.001 | 3043 (138), <0.001 | 1479 (637), <0.001 | p > .05 |
| Root mean squared error of approximation (90% CI) | 0.098 (0.095; 0.10) | 0.064 (0.061; 0.067) | 0.067 (0.063; 0.072) | p < .06 (UL < .08) |
| Non-normed fit index | 0.95 | 0.97 | 0.98 | p > .95 |
| Comparative fit index | 0.94 | 0.98 | 0.98 | p > .95 |
| Standardized root mean square residual | 0.11 | 0.061 | 0.051 | p < .08 |
Notes. SCQ = Smoking Consequences Questionnaire; UL = upper acceptance limit.
Internal consistency reliability
The eight SCQ-Spanish scales had good internal consistency reliability with Cronbach's alphas ranging from .74 to .96 (Negative Affect Reduction α = .96, Stimulation/State Enhancement α = .84, Weight Control α = .92, Taste/Sensorimotor Manipulation α = .92, Social Facilitation α = .85, Craving/Addiction α = .76, Boredom Reduction α = .88, and Health Risk α = .74).
Associations of SCQ scales at baseline with dependence
Point-biserial correlation coefficients revealed significant positive associations between dependence and all expectancies except Health Risk. Smoking rate was positively correlated with Negative Affect Reduction (r = .18, p < .01), Stimulation/State Enhancement (r = .24, p < .01), Weight Control (r = .20, p < .01), Taste/Sensorimotor Manipulation (r = .26, p < .01), Social Facilitation (r = .19, p < .01), Craving/Addiction (r = .34, p < .01), and Boredom Reduction (r = .32, p < .01). Minutes to first cigarette was positively correlated with Negative Affect Reduction (r = .18, p < .01), Stimulation/State Enhancement (r = .20, p < .01), Weight Control (r = .25, p < .01), Taste/Sensorimotor Manipulation (r = .16, p < .01), Social Facilitation (r = .15, p < .01), Craving/Addiction (r = .25, p < .01), and Boredom Reduction (r = .21, p < .01).
SCQ-Spanish predicting withdrawal severity across baseline, 5-week, and 12-week follow-ups
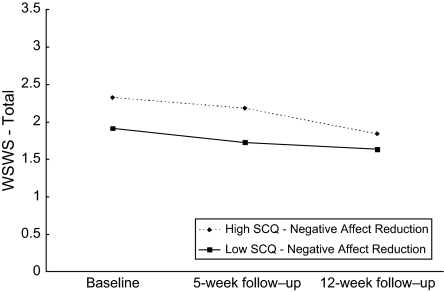
As described above, three separate sets of GLMM regression analyses evaluated the predictive validity of the SCQ-Spanish with respect to craving and total withdrawal severity from baseline through the 12-week follow-up. Smoking status at the 5- and 12-week follow-ups was included in the models because smoking after achieving an initial period of abstinence could influence withdrawal scores. Because results were essentially identical across the three models, only results of the third model (controlling for time, treatment, demographics, and dependence) are reported. In addition to examining main effects of SCQ scores on withdrawal severity over time, we examined whether expectancies interacted with time to influence withdrawal. Because consistent patterns of significant longitudinal associations of expectancies predicting withdrawal severity were observed for only two of the eight withdrawal subscales, WSWS-Craving and WSWS-Total, associations between expectancies and the other WSWS subscales are not reported (see Table 2). A graph depicting the significant Negative Affect Reduction × Time interaction predicting the WSWS-Total score is presented in Figure 1. SCQ Negative Affect Reduction was graphed at ±1 SD from the M.
Table 2.
SCQ-Spanish scales predicting WSWS-Craving and WSWS-Total scores
| SCQ-Spanish scales | WSWS-Craving |
WSWS-Total |
||||
| β | SE | p | β | SE | p | |
| Negative Affect Reduction | .17 | .03 | <.0001 | .09 | .02 | <.0001 |
| Negative Affect Reduction × Time interaction | −.04 | .01 | .0035 | −.02 | .01 | .0038 |
| Stimulation/State Enhancement | .13 | .03 | <.0001 | .04 | .02 | .0292 |
| Stimulation/State Enhancement × Time interaction | −.04 | .01 | .0072 | −.005 | .01 | .5491 |
| Weight Control | .13 | .03 | <.0001 | .07 | .02 | .0001 |
| Weight Control × Time interaction | −.05 | .01 | .0002 | −.02 | .01 | .0062 |
| Taste/Sensorimotor Manipulation | .14 | .03 | <.0001 | .04 | .02 | .0446 |
| Taste/Sensorimotor Manipulation × Time interaction | −.03 | .01 | .0254 | −.01 | .01 | .2129 |
| Social Facilitation | .16 | .03 | <.0001 | .06 | .02 | .0028 |
| Social Facilitation × Time interaction | −.03 | .01 | .0201 | −.002 | .01 | .8344 |
| Craving/Addiction | .23 | .03 | <.0001 | .11 | .02 | <.0001 |
| Craving/Addiction × Time interaction | −.03 | .02 | .1014 | −.02 | .01 | .0718 |
| Boredom Reduction | .15 | .03 | <.0001 | .07 | .02 | .0002 |
| Boredom Reduction × Time interaction | −.02 | .01 | .1295 | −.01 | .01 | .2873 |
| Health Risk | .18 | .07 | .0078 | .06 | .04 | .1585 |
| Health Risk × Time interaction | −.08 | .03 | .0106 | −.01 | .02 | .5767 |
Note. SCQ = Smoking Consequences Questionnaire; WSWS = Wisconsin Smoking Withdrawal Scale. All models controlled for time, treatment condition, demographics (i.e., age, gender, marital status [married vs. not married], education [years], employment status [employed vs. not employed], household income [<$20,000 vs. ≥$20,000], ethnicity [% Mexican origin vs. not Mexican origin], immigrant status [immigrant vs. not immigrant], and language spoken at home [Spanish only vs. not Spanish only]), dependence, and smoking status at 5- and 12-week follow-ups.
Figure 1.
Interaction of SCQ-Spanish Negative Affect Reduction score with time predicting WSWS-Total score. SCQ Negative Affect Reduction was graphed at ±1 SD from the M.
WSWS-Craving
All eight of the SCQ-Spanish scales were positively associated with WSWS-Craving over time. Six of the scales—Negative Affect Reduction, Stimulation/State Enhancement, Weight Control, Taste/Sensorimotor Manipulation, Social Facilitation, and Health Risk—interacted with time to predict craving over time. The pattern of significant interactions was similar for all the scales. In general, individuals with stronger positive expectancies reported greater baseline craving. They also reported a steeper decline in craving between baseline and 12-week follow-up. In contrast, those with weaker positive expectancies reported a lower and relatively stable level of craving from baseline through 12-week follow-up. In addition, a significant crossover interaction emerged between the Health Risk scale and time. Individuals with stronger baseline Health Risk expectancies reported greater craving at baseline. However, craving declined more over time among these individuals and dropped below the level of craving reported by those with weaker baseline expectancies for the health risks of smoking.
WSWS-Total
Seven of the eight expectancy scales (all but Health Risk) significantly predicted total withdrawal severity over time. Two scales—Negative Affect Reduction and Weight Control—interacted significantly with time to predict total withdrawal severity over time (Table 2 and Figure 1). The interaction pattern was nearly identical for both expectancies. Those with higher baseline positive expectancies reported greater total withdrawal severity throughout the study but experienced a greater decline in total withdrawal severity over time. Total withdrawal between the two groups was nearly identical at the 12-week follow-up.
SCQ-Spanish predicting relapse across 5-week and 12-week follow-ups
The first set of GLMM models, controlling for time and treatment, revealed that three of the scales—Social Facilitation, Craving/Addiction, and Boredom Reduction—were positively associated with relapse across 5- and 12-week follow-ups. The association of two additional scales with relapse—Stimulation/State Enhancement and Taste/Sensorimotor Manipulation—approached significance (Table 3). In the second (controlling for time, treatment, and demographics) and third (controlling for time, treatment, demographics, and dependence) models, Boredom Reduction was the only scale that continued to predict relapse at follow-up. Again, stronger expectancies at baseline predicted an increased likelihood of relapse at follow-up.
Table 3.
SCQ-Spanish scales predicting smoking relapse
| SCQ-Spanish scales | Controlling for time and treatment condition |
Controlling for time, treatment condition, and demographics |
Controlling for time, treatment condition, demographics, and dependence |
||||||
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| Negative Affect Reduction | 1.08 | .163 | 0.97–1.21 | 1.06 | .337 | 0.94–1.20 | 0.99 | .886 | 0.86–1.13 |
| Stimulation/State Enhancement | 1.12 | .054 | 0.99–1.26 | 1.10 | .152 | 0.97–1.24 | 1.04 | .505 | 0.91–1.20 |
| Weight Control | 1.04 | .428 | 0.94–1.16 | 1.05 | .445 | 0.93–1.17 | 0.99 | .959 | 0.88–1.13 |
| Taste/Sensorimotor Manipulation | 1.12 | .051 | 1.00–1.25 | 1.09 | .168 | 0.96–1.23 | 1.04 | .528 | 0.91–1.19 |
| Social Facilitation | 1.15 | .024 | 1.02–1.29 | 1.13 | .059 | 0.99–1.29 | 1.08 | .306 | 0.94–1.24 |
| Craving/Addiction | 1.15 | .021 | 1.02–1.30 | 1.15 | .110 | 0.98–1.28 | 1.05 | .499 | 0.91–1.23 |
| Boredom Reduction | 1.23 | .001 | 1.10–1.36 | 1.20 | .003 | 1.07–1.35 | 1.14 | .046 | 1.00–1.30 |
| Health Risk | 1.07 | .513 | 0.95–3.12 | 0.98 | .871 | 0.75–1.28 | 0.98 | .881 | 0.75–1.29 |
Note. SCQ = Smoking Consequences Questionnaire. Demographic variables included age, gender, marital status (married vs. not married), education (years), employment status (employed vs. not employed), household income (<$20,000 vs. ≥$20,000), ethnicity (% Mexican origin vs. not Mexican origin), immigrant status (immigrant vs. not immigrant), and language spoken at home (Spanish only vs. not Spanish only). Dependence variables included cigarettes per day (≤10 cigarettes/day vs. >10 cigarettes/day) and minutes to first cigarette after waking (≤60 min vs. >60 min). OR = odds ratio (0 = abstinent; 1 = relapse).
*p < .05; **p < .01.
Discussion
The SCQ-Spanish demonstrated good psychometric properties and predictive validity among a sample of Spanish-speaking Latino smokers in Texas. Specifically, CFAs revealed that the SCQ-Spanish represented a good fit to the data and was less complex compared with Spanish language versions of both the original SCQ and the SCQ-Adult. In addition, each of the eight scales demonstrated good internal consistency.
The predictive validity of the SCQ-Spanish was generally supported in that virtually all the scales prospectively predicted postcessation withdrawal severity over time even after controlling for demographics and dependence. In addition, expectancies interacted with time to predict withdrawal severity, indicating that expectancies assessed at baseline had differential effects on withdrawal at different time points. In general and as hypothesized, smokers with stronger expectancies for the positive consequences of smoking reported more severe craving and greater total withdrawal severity over time. By the 12-week follow-up, however, levels of craving and total withdrawal severity had dropped to levels nearly identical to those with weaker positive expectancies. This finding is consistent with previous research with non-Latino smokers (Copeland et al., 1995; Wetter et al., 1994). Given that withdrawal severity predicts smoking relapse (Hendricks, Ditre, Drobes, & Brandon, 2006), the current findings suggest that Spanish-speaking Latino smokers with stronger positive expectancies may have greater difficulty handling withdrawal and ultimately be at elevated risk for relapse during the early stages of quitting. Thus, these smokers may benefit from interventions designed to provide relatively intensive support early following cessation.
Only one of the SCQ-Spanish scales—Boredom Reduction—predicted relapse after controlling for demographics and dependence. Thus, the expectancy that cigarettes can help pass the time when individuals are bored, tired, or have nothing to do may be an important predictor of relapse among Spanish-speaking Latino smokers. This finding may be useful in guiding the development and delivery of interventions within this population. For example, emphasizing boredom as a high-risk situation and providing training in relevant coping skills may ultimately enhance cessation outcomes. It is also notable that four additional expectancies were marginally (Stimulation/State Enhancement and Taste/Sensorimotor Manipulation) or significantly (Social Facilitation and Craving/Addiction) associated with relapse over time in models that did not control for demographics or dependence. Thus, expectancies may ultimately have relevance for understanding relapse in this population and should be explored in future research.
It was surprising that only one of the eight expectancies examined predicted relapse after controlling for other key predictors. In contrast, Wetter and colleagues (1994) found that strong positive expectancies for the negative reinforcement properties and the negative consequences of smoking predicted relapse after controlling for demographics and dependence. A notable difference between the two studies is that abstinence in our study was assessed later (i.e., 5 weeks and 12 weeks following the baseline assessment) than in the study by Wetter and colleagues (1994; i.e., 1 week and 6 to 8 weeks postcessation). Thus, it may be that expectancies most strongly influence cessation soon after quitting and that the follow-up assessments in the current study were conducted too late to capture this effect. This interpretation is consistent with the findings of the current study indicating that the effect of expectancies on withdrawal severity declined over time.
The results further indicated that positive—but not negative—expectancies consistently predicted total withdrawal severity. That is, stronger positive expectancies, such as alleviating negative affect, facilitating social interactions, and controlling one's weight, predicted greater total withdrawal severity, whereas negative expectancies were unrelated. Furthermore, results indicated that smokers who were more dependent held stronger positive expectancies. These findings are generally consistent with previous research with non-Latino smokers (Copeland et al., 1995) and smokers in Spain (Reig-Ferrer & Cepeda-Benito, 2007). Despite overlap among positive expectancies and dependence, it is important that positive expectancies continued to predict total withdrawal severity after controlling for dependence. Thus, it appears that positive expectancies have unique utility in predicting withdrawal severity in this population. Taken together, the results indicate that the SCQ-Spanish is valid for use with Spanish-speaking Latino smokers in the United States and that it has utility in predicting both withdrawal severity and potential relapse over time, even after controlling for the effects of demographics and dependence.
This study has several limitations. First, expectancies were assessed only at baseline. Therefore, participants may have experienced changes in expectancies during the course of the study that were not captured, and such changes may have influenced postcessation withdrawal severity and relapse. For example, expectancies for the health risks of smoking may have increased during the course of the study as participants learned new information about the negative effects of smoking on health. Of note, however, Gwaltney and colleagues (2005) found that the strength of positive outcome expectancies assessed at baseline was a better predictor of relapse than daily measures of expectancies collected via ecological momentary assessment. Further research on expectancy effects over time is clearly needed.
It is also notable that the findings are based on a low socioeconomic-status sample comprising primarily immigrant smokers of largely Mexican ethnicity/origin who resided in Texas. Therefore, findings may not generalize to other Spanish-speaking Latino populations in the United States. Also, the results do not address whether or not the SCQ-Spanish is suitable for use among English-speaking Latino smokers in the United States. In addition, the data may be limited in terms of providing unique information regarding the SCQ and cessation processes among Spanish-speaking Latinos given that Latinos were not directly compared with English-speaking Latinos or other racial/ethnic groups. Another limitation is that the results were not corrected for multiple comparisons. However, because this study is the first to compare different versions of the SCQ among Spanish-speaking Latino smokers in the United States, we felt that a less conservative approach was appropriate. A final limitation is that cessation outcomes were not biochemically verified. However, fairly compelling evidence suggests that biochemical verification of smoking status is not necessary in population-based studies such as this one (Velicer, Prochaska, Rossi, & Snow, 1992).
The current results add to the existing literature in several key ways. This study is the first to evaluate the utility of any existing versions of the SCQ for use with Spanish-speaking Latino smokers in the United States. Nearly all the SCQ-Spanish scales prospectively predicted both craving and total withdrawal severity after controlling for demographics and dependence, suggesting that expectancies have incremental utility in predicting which Spanish-speaking Latino smokers are at elevated risk for severe withdrawal symptoms. The finding that Boredom Reduction emerged as a key and unique predictor of relapse may also have important implications. For example, interventions that specifically target Boredom Reduction as an important high-risk situation may ultimately reduce relapse in this population. In addition, the four other expectancies that were marginally (Stimulation/State Enhancement and Taste/Sensorimotor Manipulation) or significantly (Social Facilitation and Craving/Addiction) associated with relapse in models that did not control for demographics or dependence may also be useful in better understanding smoking relapse in this population. In summary, reducing smoking among Latinos in the United States is a critical public health priority (Fiore et al., 2000; USDHHS, 2001), and more widespread use of the SCQ-Spanish in studies with Spanish-speaking Latino smokers will be useful in elucidating how expectancies influence smoking initiation, maintenance, and cessation.
Funding
This research was supported by grants from the Minority Health Research and Education Program of the Texas Higher Education Coordinating Board, the National Cancer Institute (R01CA125413, R01CA94826, R01CA89350, R01CA097893, R01CA132636, K07CA121037), and the Centers for Disease Control and Prevention (K01DP000086).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
We acknowledge the National Cancer Institute's Cancer Information Service for their contributions to the original research project, Adiós al Fumar, from which our data were derived.
References
- Abraido-Lanza AF, Chao MT, Gates CY. Acculturation and cancer screening among Latinas: Results from the National Health Interview Survey. Annals of Behavioral Medicine. 2005;29:22–28. doi: 10.1207/s15324796abm2901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Morse E, Sherman JE. The motivation to use drugs: A psychobiological analysis of urges. Nebraska Symposium on Motivation. 1986;34:257–323. [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, Kim SY, et al. Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine and Tobacco Research. 2007;9(Suppl. 4):S555–S570. doi: 10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bernstein R. Nation's population one-third minority. 2006. Retrieved December 31, 2007, from http://www.census.gov/Press-Release/www/releases/archives/population/006808.html. [Google Scholar]
- Borrelli B, Bock B, King T, Pinto B, Marcus BH. The impact of depression on smoking cessation in women. American Journal of Preventive Medicine. 1996;12:378–387. [PubMed] [Google Scholar]
- Brandon TH. Negative affect as motivation to smoke. Current Directions in Psychological Science. 1994;3:33–37. [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:484–491. [Google Scholar]
- Brislin R, Lonner W, Thorndike E. Cross-cultural research methods. New York: Wiley; 1973. [Google Scholar]
- Brown H, Prescott R. Applied mixed models in medicine. West Sussex, England: John Wiley and Sons, Ltd; 1999. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Health disparities experienced by Hispanics—United States. Morbidity and Mortality Weekly Report. 2004;53:535–537. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults—United States, 2006. Morbidity and Mortality Weekly Report. 2007;55:1157–1161. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults—United States, 2007. Morbidity and Mortality Weekly Report. 2008;57:1221–1226. [PubMed] [Google Scholar]
- Cepeda-Benito A, Ferrer AR. Smoking Consequences Questionnaire–Spanish. Psychology of Addictive Behaviors. 2000;14:219–230. doi: 10.1037//0893-164x.14.3.219. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire–Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7:484–494. [Google Scholar]
- Etter JF. A comparison of the content-, construct- and predictive validity of the cigarette dependence scale and the Fagerstrom test for nicotine dependence. Drug and Alcohol Dependence. 2005;77:259–268. doi: 10.1016/j.drugalcdep.2004.08.015. [DOI] [PubMed] [Google Scholar]
- Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007;102(Suppl. 2):5–29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Treating tobacco use and dependence: Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2000. (No. 1-58763-007-9) [Google Scholar]
- Gibbons FX, Eggleston TJ, Benthin AC. Cognitive reactions to smoking relapse: The reciprocal relation between dissonance and self-esteem. Journal of Personality and Social Psychology. 1997;72:184–195. doi: 10.1037//0022-3514.72.1.184. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, McGovern PG, Lando HA. Relapse and risk perception among members of a smoking cessation clinic. Health Psychology. 1991;10:42–45. doi: 10.1037//0278-6133.10.1.42. [DOI] [PubMed] [Google Scholar]
- Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, et al. Smoking, smoking cessation, and major depression. Journal of the American Medical Association. 1990;264:1546–1549. [PubMed] [Google Scholar]
- Goldman MS, Brown SA, Christensen BA. Expectancy theory: Thinking about drinking. In: Blane HT, Leonard KE, editors. Psychological theories of drinking and alcoholism. New York: Guilford Press; 1987. pp. 181–226. [Google Scholar]
- Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114:661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Ditre JW, Drobes DJ, Brandon TH. The early time course of smoking withdrawal effects. Psychopharmacology (Berl) 2006;187:385–396. doi: 10.1007/s00213-006-0429-9. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine and Tobacco Research. 2003;5:13–25. [PubMed] [Google Scholar]
- Joreskog KG, Sorbom D. LISREL 8: User's reference guide. Chicago: Scientific Software International; 1996. [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: Contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology. 2002;70:216–227. [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Lewis-Esquerre JM, Rodrigue JR, Kahler CW. Development and validation of an adolescent smoking consequences questionnaire. Nicotine and Tobacco Research. 2005;7:81–90. doi: 10.1080/14622200412331328475. [DOI] [PubMed] [Google Scholar]
- Marin G, Marin BV, Perez-Stable EJ, Sabogal F, Otero-Sabogal R. The role of acculturation in the attitudes, norms, and expectancies of Hispanic smokers. Journal of Cross-Cultural Psychology. 1989;20:399–415. [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- Myers MG, McCarthy DM, MacPherson L, Brown SA. Constructing a short form of the Smoking Consequences Questionnaire with adolescents and young adults. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 2003;15:163–172. doi: 10.1037/1040-3590.15.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niaura R, Britt DM, Borrelli B, Shadel WG, Abrams DB, Goldstein MG. History and symptoms of depression among smokers during a self-initiated quit attempt. Nicotine and Tobacco Research. 1999;1:251–257. doi: 10.1080/14622299050011371. [DOI] [PubMed] [Google Scholar]
- Niaura R, Goldstein M, Abrams D. A bioinformational systems perspective on tobacco dependence. British Journal of Addiction. 1991;86:593–597. doi: 10.1111/j.1360-0443.1991.tb01814.x. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, et al. Cigarette smoking behavior among US Latino men and women from different countries of origin. American Journal of Public Health. 2001;91:1424–1430. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, et al. Smoking withdrawal dynamics in unaided quitters. Journal of Abnormal Psychology. 2000;109:74–86. doi: 10.1037//0021-843x.109.1.74. [DOI] [PubMed] [Google Scholar]
- Reig-Ferrer A, Cepeda-Benito A. Smoking expectancies in smokers and never smokers: An examination of the smoking Consequences Questionnaire-Spanish. Addictive Behaviors. 2007;32:1405–1415. doi: 10.1016/j.addbeh.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Swaine-Verdier A, Doward LC, Hagell P, Thorsen H, McKenna SP. Adapting quality of life instruments. Value in Health: The journal of the International Society for Pharmacoeconomics and Outcomes Research. 2004;7(Suppl. 1):S27–S30. doi: 10.1111/j.1524-4733.2004.7s107.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Tobacco use among U.S. racial/ethnic minority groups. Atlanta, GA: Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Healthy people 2010. Washington, DC: Author; 2001. [Google Scholar]
- Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychological Bulletin. 1992;111:23–41. doi: 10.1037/0033-2909.111.1.23. [DOI] [PubMed] [Google Scholar]
- Welsch SK, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Development and validation of the Wisconsin Smoking Withdrawal Scale. Experimental and Clinical Psychopharmacology. 1999;7:354–361. doi: 10.1037//1064-1297.7.4.354. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Carmack CL, Anderson CB, Moore CA, De Moor CA, Cinciripini PM, et al. Tobacco withdrawal signs and symptoms among women with and without a history of depression. Experimental and Clinical Psychopharmacology. 2000;8:88–96. doi: 10.1037//1064-1297.8.1.88. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Fiore MC, Young TB, McClure JB, de Moor CA, Baker TB. Gender differences in response to nicotine replacement therapy: Objective and subjective indexes of tobacco withdrawal. Experimental and Clinical Psychopharmacology. 1999;7:135–144. doi: 10.1037//1064-1297.7.2.135. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Mazas C, Daza P, Nguyen L, Fouladi RT, Li Y, et al. Reaching and treating Spanish-speaking smokers through the National Cancer Institute's Cancer Information Service: A randomized controlled trial. Cancer. 2007;109(Suppl. 2):406–413. doi: 10.1002/cncr.22360. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Smith SS, Kenford SL, Jorenby DE, Fiore MC, Hurt RD, et al. Smoking outcome expectancies: Factor structure, predictive validity, and discriminant validity. Journal of Abnormal Psychology. 1994;103:801–811. doi: 10.1037//0021-843x.103.4.801. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Prevalence of current tobacco smoking among adults, 15 years and older—2005. 2005. Retrieved February 12, 2009, from http://www.who.int/whosis/database/core/ [Google Scholar]
- Zhu SH, Pulvers K, Zhuang Y, Baezconde-Garbanati L. Most Latino smokers in California are low-frequency smokers. Addiction. 2007;102(Suppl. 2):104–111. doi: 10.1111/j.1360-0443.2007.01961.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.