Abstract
PURPOSE
To report the long-term outcomes of a population-based cohort of children diagnosed with congenital esotropia during a 30-year period.
METHODS
The medical records of all patients diagnosed with congenital esotropia as residents of Olmsted County, MN, from January 1, 1965, through December 31, 1994, were retrospectively reviewed.
RESULTS
A total of 130 children were diagnosed during the 30-year period at a median age of 7.4 months with a mean deviation of 30Δ. During a median follow-up of 11.9 years, 126 patients underwent a mean of 1.8 strabismus surgeries. The risk for undergoing a second surgery was significantly greater in patients with a larger presenting angle (p = 0.017) and a younger age at first surgery (p = 0.006). The Kaplan-Meier rate of having a second surgery was 51% at 10 years and 66% at 20 years. For those with 6 weeks or more of follow-up from the final surgery, last examined at a mean age of 15.1 years, 42 of 94 (45%) were within 8Δ of orthotropia and 30 of 98 had some level of stereopsis (≤3000 arcsec).
CONCLUSIONS
In this population-based study of children with congenital esotropia, a second surgery was necessary in half the patients after 10 years and was more likely in those patients with a larger presenting angle and a younger age at first surgery. Approximately half of the patients were within 8Δ of orthotropia and one-third had measurable stereopsis after a mean of 10.9 years of follow-up.
Congenital or infantile esotropia is a well-recognized disorder of ocular alignment characterized by a non-accommodative, relatively large-angle constant esotropia that develops by 6 months of age in an otherwise-healthy child. Although recently reported to comprise only 8% of all childhood esodeviations,1 congenital esotropia is commonly encountered in ophthalmology clinics as the result, in part, of the associated findings of amblyopia, nystagmus, dissociated vertical deviations, oblique muscle dysfunction, and consecutive deviations. Although a number of previous reports have described the surgical outcomes for these patients,2–8 none were performed in a population-based setting. The purpose of this study is to report the long-term outcomes of children diagnosed with congenital esotropia during a 30-year period using a population-based medical record retrieval system.
Subjects and Methods
The medical records of all patients residing in Olmsted County, MN, and diagnosed with congenital esotropia from January 1, 1965, through December 31, 1994, were reviewed retrospectively through February 28, 2008. This study was approved by the Institutional Review Boards of Mayo Clinic and Olmsted Medical Group and conforms to the requirements of the United States Health Insurance Portability and Accountability Act. Potential cases of congenital esotropia were identified with the use of resources from the Rochester Epidemiology Project, a medical records linkage system designed to capture data on any patient–physician encounter in Olmsted County, MN.9,10 The racial distribution of Olmsted County residents during the years of this study was greater than 95% white and less than 3% each for Asian American, African American, and Native American. The population of this county (92,006 in 1980) is relatively isolated from other urban areas, and virtually all medical care is provided to residents by Mayo Clinic or Olmsted Medical Group and their affiliated hospitals.10 Unaffiliated area optometrists were rarely the sole provider of eye care to children with strabismus during the years of this investigation.11
The medical records of all patients younger than 19 years of age at the time they were diagnosed with any form of esotropia from the years 1965 through 1994 were reviewed by a pediatric ophthalmologist (BGM). A diagnosis of congenital esotropia was confirmed by the same reviewer and defined as a nonaccommodative esotropia that developed by 6 months of age in a neurologically intact child. Children with a paralytic, sensory, or neurologic cause of their deviation, or in the setting of a developmental disorder, were specifically excluded from the study. The parental history of the age at onset and the presence of dissociated vertical deviation or other markers of early-onset strabismus were relied upon for late-presenting patients. Patients who met diagnostic criteria were included in the study regardless of whether or not they underwent surgery. Trained residency checkers verified each patient’s residency status at the time of birth and at diagnosis by using information from city and county directories. Children not residing in Olmsted County at the time of their diagnosis were excluded.
The initial angle of deviation was measured by the Hirschberg estimate or Krimsky test in young infants and by the prism and alternate cover test at both distance (4 m) and near for children old enough to cooperate with testing. A cycloplegic refraction, most often with the administration of atropine or cyclopentolate, was performed in all patients. For the purposes of this study, amblyopia was defined as a difference in best-corrected visual acuity of 2 or more lines between the 2 eyes or as a clear preference for the use of one eye in preverbal children. Stereopsis was evaluated with the Titmus stereotest. The entire medical record of those diagnosed with congenital esotropia was carefully reviewed through the date of their final examination.
Patient characteristics were tabulated with the use of number and percent for categorical variables, and median and range for continuous variables. Comparisons were obtained with the use of the Fisher’s exact test (categorical variables) or the Wilcoxon rank-sum test (continuous variables). All statistical tests were 2-sided, and the threshold of significance was set at α = 0.05. The probability of requiring a second surgery was estimated using the Kaplan-Meier method.12 Potential risk factors for requiring a second surgery were evaluated with the Cox proportional hazards regression model.
Results
In Olmsted County, MN, 130 new cases of congenital esotropia were diagnosed during the 30-year study period. Pertinent historical and clinical characteristics of the 130 study subjects are shown in Table 1. The birth prevalence of congenital esotropia during the 30-year period was 25 (95% confidence interval 21–29) per 10,000, or 1 in 403 live births. Of the 130 patients, 120 (92.3%) were diagnosed by 18 months of age. There was no difference in the mean age at diagnosis throughout the 30-year study. Only 8 patients (6.2%) had + 3.50 D or more of hyperopic refractive error.
Table 1.
Presenting historical characteristics and initial ophthalmologic findings of 130 children with congenital esotropia during a 30-year period from Olmsted County, MN
| Number (%) of boys/girls | 66 (51)/64 (49) |
| Number (%) born premature* | 16/130 (12.3) |
| Number (%) with family history of strabismus | 36/76 (47) |
| Median age at diagnosis in months (range) | 7.4 (2–59) |
| Number (%) with amblyopia | 49/127 (38.6) |
| Median angle of deviation in PD (range) | 30 (10–90) |
| Number (%) with IO overaction at diagnosis | 12/128 (9.4) |
| Number (%) with DVD at diagnosis | 3/130 (2.3) |
| Mean (median) cycloplegic refraction in OD (range)† | 1.85 (2.0) (−1.75 to 5.0) |
| Mean (median) cycloplegic refraction in OS (range)† | 1.83 (2.0) (−1.88 to 5.0) |
| Mean (median) cycloplegic refractions, average of OD and OS (range)† | 1.84 (2.0) (−1.81 to 5.0) |
PD, prism diopters; IO, inferior oblique; DVD, dissociated vertical deviation; OD, right eye; OS, left eye.
Less than 37 weeks’ gestational age;
spherical equivalent refraction.
The clinical characteristics of the 126 (98%) children who underwent surgery are shown in Table 2. These children underwent an average of 1.8 (range, 0–5) surgeries during a median follow-up of 11.9 years (range, 9 days to 40 years) after diagnosis. Sixty-five patients underwent a second surgery during the follow-up period, and only 5 of these procedures were for vertical deviations alone. The risk for undergoing a second surgery was significantly greater in patients with a larger presenting angle (p = 0.017) and a younger age at first surgery (p = 0.006) (Table 3). The Kaplan-Meier rate of undergoing a second strabismus surgery in this population was 45% at 5 years, 51% at 10 years, and 66% at 20 years, as shown in Figure 1.
Table 2.
Surgical characteristics of 126 patients with congenital esotropia who underwent surgery
| Mean age at first surgery in months (range) | 19.0 (5.7–178.1) |
| Median angle of deviation before first surgery in PD (range) | 40 (15–90) |
| Mean number of surgeries (range) | 1.8 (1–5) |
| Mean follow-up time (range) | 11.9 years (9 days to 40 years) |
| Mean age at final follow-up (range)* | 14.9 years (1.2–42 years) |
| Number (%, range) of patients within 8 PD of orthotropia at final examination (range)† | 42 (45, 0–40) |
| Final median stereoacuity (range)‡ | Nil (40 arcsec to nil) |
| No. with amblyopia at final follow-up (%)* | 27 (23) |
PD, prism diopters.
For 119 patients with at least 6 weeks of follow-up from final surgery.
Available for 94 of 119 patients with 6 weeks of follow-up from final surgery.
Available for 98 of 119 patients with 6 weeks of follow-up from final surgery.
Table 3.
Risk factors for requiring a second surgery among 126 patients with congenital esotropia
| Risk factor | Cox proportional hazard ratio (95% confidence interval) | p-value |
|---|---|---|
| Family history of strabismus | 0.76 (0.40–1.44) | 0.40 |
| Prematurity (gestational age <37 weeks) | 1.53 (0.76–3.11) | 0.24 |
| Gestational age at birth (weeks) | 0.93 (0.81–1.06) | 0.28 |
| Birth weight (per 1,000 g) | 0.97 (0.64–1.47) | 0.88 |
| Age at diagnosis (per year of increasing age) | 0.65 (0.37–1.15) | 0.14 |
| Amblyopia at presentation | 1.31 (0.80–2.16) | 0.28 |
| Size of the angle at presentation (per increase of esotropia by 10Δ) | 1.25(1.04–1.51) | 0.017 |
| Age at first surgery (per year of increasing age) | 0.55 (0.36–0.84) | 0.006 |
| Inferior oblique overaction at initial examination | 0.90 (0.36–2.26) | 0.83 |
FIG 1.
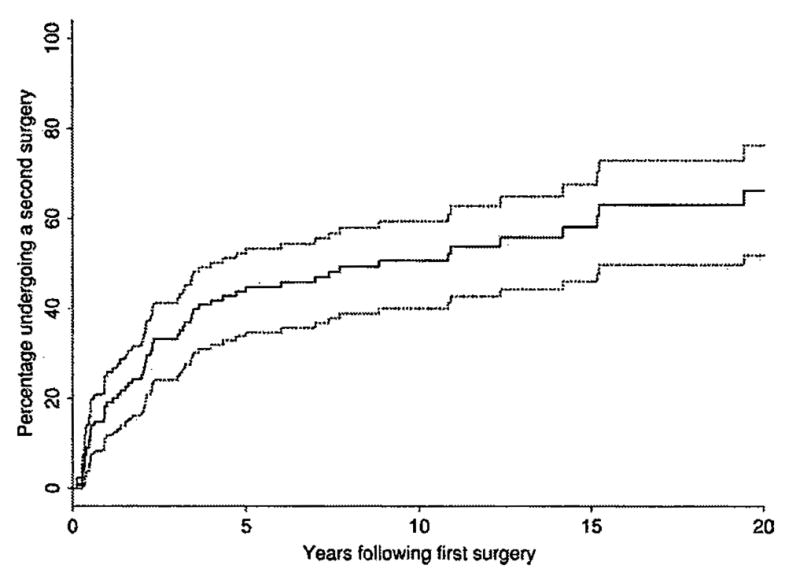
Kaplan-Meier probability of requiring a second surgery in 126 patients with congenital esotropia (95% confidence interval).
Of the 126 surgical patients, 119 (94.4%) had at least 6 weeks or more of follow-up from their final surgery at a mean age of 15.1 years old (range, 14 months to 42 years). Twenty-seven of these 119 (22.7%) children had documentation of decreased vision suggesting amblyopia at their last examination. The angle of deviation was measured at the final examination in 94 patients, of which 42 (45%) were within 8Δ of orthotropia. The final angle of deviation ranged from 25Δ of esotropia to 40Δ of exotropia. The median stereoacuity at the final examination in 98 of these 119 patients was nil, with a range from nil to 40 arcsec. Of the 98 patients with at least 6 weeks of follow-up from the last surgery and a documented evaluation of stereoacuity, 30 (30.6%) had some level of stereopsis (≤3000 arcsec) as measured by the Titmus housefly. Of these 30, 9 had at least 200 arcsec, with a single patient exhibiting 40 arcsec of stereoacuity.
Discussion
This study provides population-based data on a 30-year cohort of 130 children with congenital esotropia. Of these patients, 126 underwent a mean of 1.8 surgeries during a median of 11.9 years from diagnosis, with 2 of 3 patients calculated to undergo a second surgery by 20 years of follow-up. A larger presenting angle of esotropia and a younger age at first surgery were associated with an increased risk for undergoing a second surgery. At final follow-up, less than half of the children were successfully aligned and even fewer had gross stereopsis.
The authors of a number of other studies also have demonstrated the high likelihood of multiple surgeries in children with congenital esotropia.3–5,13 Rowe14 reported an average of 1.35 surgeries per patient after an average of 7 years of follow-up, and Shauly et al8 reported an average of 1.6 surgeries per patient during 8 years of follow-up. There are several potential reasons that patients with congenital esotropia are at risk for undergoing multiple surgeries. When compared with those with acquired esotropia, patients with congenital esotropia generally achieve worse stereopsis, resulting in poorer motor alignment, and are more likely to have vertical deviations such as dissociated vertical deviation or inferior oblique dysfunction, which often require further surgical intervention. A third potential contributor is that preoperative angle measurements are likely to be less accurate in very young children, leading to less successful motor outcomes.
Characteristics that conveyed an increased risk of requiring a second surgery included a larger angle of esotropia at presentation (p = 0.017) and a younger age at first surgery (p = 0.006). These findings are consistent with a report from Trigler and Siatkowski15 showing that children with angles less than 30Δ or older than 15 months of age at first surgery underwent significantly fewer surgeries for horizontal deviations. Kushner et al16 have reported that the response to strabismus surgery correlated significantly with the magnitude of the preoperative deviation. In our study, 33% (16 of 48) of patients who had greater than 40Δ of esotropia prior to their first surgery underwent only one surgery, whereas 58% (45 of 78) of patients with up to 40Δ of esotropia were managed with a single surgery (p = 0.010).
The significantly increased likelihood for a second procedure in children undergoing surgery at a younger age is also consistent with several previous reports. Helveston et al3 reported a high likelihood of requiring a second surgery within 10 years after the first procedure for patients aligned before 6 months of age. Trigler and Siatkowski15 showed that although 47% of patients who were older than 15 months of age at their first surgery underwent one horizontal procedure, only 33% of those who were 15 months of age or younger required only one horizontal procedure. More recently, the authors of the Early versus Late Infantile Strabismus Surgery Study (ELISSS)17 reported that patients in an early treatment cohort (6–24 months of age) had 1.18 surgeries per patient compared with 0.99 surgeries per patient in those randomized to late treatment (32–60 months of age). Some authors advocate early surgery, often before 6 months of age.3,4,18 The findings from this report suggest that such patients are likely to require a second surgery compared with those who are older at the time of their first surgery, and parents of these children should be counseled about the risk of undergoing multiple surgeries. This may be attributable to the difficulty of examining young infants or that surgery in older individuals is more likely to combine horizontal and vertical deviations, thereby decreasing the total number of procedures. Another potential reason for the risk of multiple surgeries in such patients is the instability of the deviating angle. The Pediatric Eye Disease Investigators Group (PEDIG)19 currently is comparing the surgical outcomes of esotropic children with stable angles with those that are unstable. However, Birch and Stager20 reported that, compared with patients who underwent surgery between 7 and 12 months of age, patients who underwent surgery before 6 months of age had no significant differences in the number of second surgeries or in their postoperative alignment.
Forty-five percent of patients in this study who were followed for at least 6 weeks after their final surgery and whose ocular alignment at distance was recorded (mean, 10.9 years after first surgery) were within 8Δ of orthotropia. Previous studies have reported higher rates of postoperative microtropia, but with shorter postoperative durations (Table 4). Reports with longer follow-up periods have fewer microtropic patients at the final follow-up examination. This finding underscores the importance of prolonged follow-up to determine the true evolution of congenital esotropia after surgical intervention.
Table 4.
Published reports on postoperative alignment of patients with congenital esotropia by years of follow-up
| Study | n | % of children with microtropia at follow-up | Mean follow-up time |
|---|---|---|---|
| Teller et al6 | 37 | 80% within 10Δ orthotropia | 4 years after surgery (fixed end point of study) |
| Mauro et al7 | 521 | 72% within 10Δ orthotropia | 4 years after surgery (fixed end point of study) |
| Tolun et al5 | 54 | 66.6% within 10Δ orthotropia | 5 years from diagnosis (2–11 years) |
| Shauly et al8 | 103 | 50.5% within 8Δ orthotropia | 8.7 years after surgery (3–24 years) |
| Current study | 130 | 45% within 8Δ orthotropia | 10.9 years after surgery (9 days–40 years) |
The subjects of this study demonstrated a final median stereoacuity of nil. Of the 30 with measurable stereopsis at their final examination, 9 of the patients had 200 arcsec or better. The development of stereopsis has been an elusive target in the treatment of congenital esotropia and has been the subject of many studies. Rowe14 reported at least gross stereoacuity in 9 of 40 children followed an average of 7 years. Birch et al13 reported postoperative Randot stereoacuity of 200 seconds or better in 41.1% of 73 patients with congenital esotropia, with evidence of macular or foveal stereoacuity in a significantly larger number of patients who were aligned by 12 months of age. Only one well-documented case of normal stereopsis has been reported.21 Several other studies suggest that although it is difficult to obtain excellent stereoacuity, peripheral or gross stereoacuity may be more likely obtained with early surgical alignment.3,4,17–18,20
There are a number of limitations to the findings in this study. For some older presenting patients, the age at onset was less certain and overlap with an acquired esotropia was possible. In such cases, other clinical signs characteristic of congenital esotropia were used to confirm the diagnosis, and the outcomes for these patients were similar to those with congenital esotropia rather than to those with an acquired esodeviation. A second potential weakness is that some residents of this population may have sought care outside Olmsted County, although the relative isolation of this population from other urban areas makes this occurrence rare. Additionally, this study is limited by its retrospective nature and uneven follow-up of the study patients. Furthermore, these patients were managed by a variety of clinicians within the department, including resident and general ophthalmologists, which may have introduced more errors of measurement than studies performed exclusively by strabismus specialists. Finally, this study is limited by the ethnic composition of Olmsted County, which allows extrapolation only to other semiurban white populations of the United States.
This population-based study provides data on the long-term outcomes for patients with congenital esotropia. These children are likely to undergo multiple surgeries, with 2 of 3 expected to require a second surgery by 20 years of follow-up. Factors significantly associated with requiring a second surgery include a larger angle of esotropia at presentation and a younger age at first surgery. Regular follow-up is required for these patients because of the high risk of poor stereopsis and recurrent strabismus requiring additional surgery.
Footnotes
Presented at the 34th Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, Washington, D.C., April 2–6, 2008.
Funded in part by an unrestricted grant from Research to Prevent Blindness Inc., New York, NY.
Study conducted at Mayo Clinic Rochester Minnesota.
References
- 1.Greenberg AE, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood esotropia. A population-based study. Ophthalmology. 2007;113:170–4. doi: 10.1016/j.ophtha.2006.05.072. [DOI] [PubMed] [Google Scholar]
- 2.Infeld D, Prior C, Ryan H, O’Day J. The long-term results of surgical correction of childhood esotropia. Aust N Z J Ophthalmol. 1993;21:23–8. doi: 10.1111/j.1442-9071.1993.tb00125.x. [DOI] [PubMed] [Google Scholar]
- 3.Helveston EM, Neely DF, Stidham DB, Wallace DK, Plager DA, Springer DT. Results of early alignment of congenital esotropia. Ophthalmology. 1999;106:1716–26. doi: 10.1016/S0161-6420(99)90337-8. [DOI] [PubMed] [Google Scholar]
- 4.Ing MR. Outcome study of surgical alignment before six months of age for congenital esotropia. Ophthalmology. 1995;102:2041–5. doi: 10.1016/s0161-6420(95)30756-7. [DOI] [PubMed] [Google Scholar]
- 5.Tolun H, Dikici K, Ozkiris A. Long-term results of bimedial rectus recessions in infantile esotropia. J Pediatr Ophthalmol Strabismus. 1999;36:201–15. doi: 10.3928/0191-3913-19990701-09. [DOI] [PubMed] [Google Scholar]
- 6.Teller J, Savir H, Yelin N, Cohen R, Leviav A, Elstin R. Late results of surgery for congenital esotropia. Metab Pediatr Syst Ophthalmol. 1988;11:115–18. [PubMed] [Google Scholar]
- 7.Maruo T, Kubota N, Sakaue T, Usui C. Esotropia surgery in children: Long term outcome regarding changes in binocular alignment; a study of 956 cases. Binocul Vis Strabismus Q. 2000;15:213–20. [PubMed] [Google Scholar]
- 8.Shauly Y, Prager TC, Mazow ML. Clinical characteristics and long-term postoperative results of infantile esotropia. Am J Ophthalmol. 1994;117:183–9. doi: 10.1016/s0002-9394(14)73075-2. [DOI] [PubMed] [Google Scholar]
- 9.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 10.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 11.Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: A population-based study. Ophthalmology. 2005;112:104–8. doi: 10.1016/j.ophtha.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan EL, Meier P. Nonparametric estimation from incomplete data. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 13.Birch EE, Stager DR, Everett ME. Random dot stereoacuity following surgical correction of infantile esotropia. J Pediatr Ophthalmol Strabismus. 1995;32:231–5. doi: 10.3928/0191-3913-19950701-07. [DOI] [PubMed] [Google Scholar]
- 14.Rowe FJ. Long-term postoperative stability in infantile esotropia. Strabismus. 2000;8:3–13. [PubMed] [Google Scholar]
- 15.Trigler L, Siatkowski RM. Factors associated with horizontal reoperation in infantile esotropia. J AAPOS. 2002;6:15–20. doi: 10.1067/mpa.2002.120644. [DOI] [PubMed] [Google Scholar]
- 16.Kushner BJ, Fisher MR, Lucchese NJ, Morton GV. Factors influencing response to strabismus surgery. Arch Ophthalmol. 1993;111:75–9. doi: 10.1001/archopht.1993.01090010079030. [DOI] [PubMed] [Google Scholar]
- 17.Simonsz HJ, Kolling GH, Unnebrink K for the Early vs. Late Infantile Strabismus Surgery Group. Final report of the early vs. late infantile strabismus surgery study (ELISSS), a controlled, prospective, multicenter study. Strabismus. 2005;13:169–99. doi: 10.1080/09273970500416594. [DOI] [PubMed] [Google Scholar]
- 18.Wright KW, Edelman PM, McVey JH, Terry AP, Lin M. High-grade stereo acuity after early surgery for congenital esotropia. Arch Ophthalmol. 1994;112:913–9. doi: 10.1001/archopht.1994.01090190061022. [DOI] [PubMed] [Google Scholar]
- 19.Christiansen SP Protocol Chair Pediatric Eye Disease Investigator Group. Esotropia Treatment Study 1: An Observational Study of Infantile Acquired Non-accommodative, and Acquired Partially-Accommodative Esotropia. Study Protocol Version 2.0. 2005 August 22; [Google Scholar]
- 20.Birch EE, Stager DR. Long-term motor and sensory outcomes after early surgery for infantile esotropia. J AAPOS. 2006;10:409–13. doi: 10.1016/j.jaapos.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Parks MM. Congenital esotropia with a bifixation result. Report of a case. Doc Ophthalmol. 1984;58:109–14. doi: 10.1007/BF00140907. [DOI] [PubMed] [Google Scholar]


