Abstract
PURPOSE
To describe the long-term surgical outcomes in a population-based cohort of children with intermittent exotropia.
METHODS
The medical records of all children (<19 years) who were diagnosed with intermittent exotropia as residents of Olmsted County Minnesota, from January 1, 1975, through December 31, 1994, and managed with surgery were retrospectively reviewed.
RESULTS
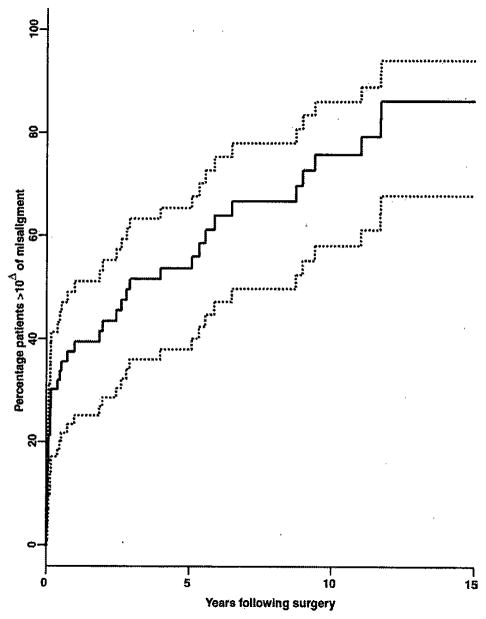
Of 184 patients with intermittent exotropia, 61 (33%) underwent surgery at a mean age of 7.6 years (range, 3.2 to 23 years). Twelve of the 61 children (19.7%) underwent a second surgery (10 for recurrent exotropia and 2 for consecutive esotropia), and no patient received 3 or more surgeries during a mean follow-up of 10 years from the first surgery. The final postoperative measurements were recorded in 56 of 61 patients (92%) at a mean of 7.4 years (range, 0 to 18 years) after the first surgery: 31 of the 56 (55%) were within 9Δ of orthotropia at distance and 25 of 55 (45%) had better than 60 seconds of stereopsis. The Kaplan-Meier rate of developing ≥10Δ of misalignment after the first surgery was 54% by 5 years, 76% by 10 years, and 86% by 15 years.
CONCLUSIONS
In this population-based study of surgery in children with intermittent exotropia, although only 1 in 5 received a second surgery, after a mean follow-up of 8 years, approximately half were successfully aligned and 45% had high-grade stereopsis.
Intermittent exotropia is the most prevalent form of childhood exotropia,1 and is characterized by an acquired, intermittent exodeviation in an otherwise-healthy child. Management for this form of strabismus includes observation, medical therapy (orthoptics, over-minus spectacles, and alternate patching), and surgical intervention.2,3 Although numerous studies on the surgical outcomes of these patients have been published,4–15 none is based on a well-defined population. This study describes the long-term surgical outcomes of children diagnosed with intermittent exotropia during a 20-year period using a population-based medical record retrieval system.
Subjects and Methods
The medical records of all patients younger than 19 years who, while residents of Olmsted County, Minnesota, were diagnosed by an ophthalmologist as having any form of exotropia between January 1, 1975, and December 31, 1994, were retrospectively reviewed. Institutional review board approval was obtained for this study. Intermittent exotropia was distinguished from other forms of exotropia and defined as an intermittent distance exodeviation of at least 10Δ without an underlying or associated neurologic, paralytic, or ocular disorder. Potential cases of intermittent exotropia were identified by the resources of the Rochester Epidemiology Project, a medical record linkage system designed to capture data on any patient-physician encounter in Olmsted County.16 The racial distribution of Olmsted County residents in 1990 was 96% Caucasian, 3.0% Asian American, 0.7% African American, and 0.3% Native American and other. The population of this county (106,470 in 1990) is relatively isolated from other urban areas, and virtually all medical care is provided to residents by the Mayo Clinic or Olmsted Medical Group, and their affiliated hospitals.17 Unaffiliated area optometrists were rarely the sole provider of eye care to children with strabismus during the years of this investigation. Patients not residing in Olmsted County at the time of their diagnosis were excluded.
The angle of deviation was primarily determined by the prism alternate cover technique at both distance and near, although some patients (11%) were measured by the Hirschberg or modified Krimsky techniques at near. The refractive error was measured in the majority of patients after the topical administration of cyclopentolate or atropine in younger patients and by a manifest refraction in older children. Sensory testing, was primarily performed with the Titmus fly and Lang stereotest. There were no specific criteria for enacting medical or surgical therapy: instead, treatment was at the discretion of the provider with parental consent. The follow-up duration was measured for each patient from the initial diagnosis to the final examination in which ocular alignment was measured.
Continuous data are presented as a mean with standard deviation (SD), and categorical data are presented as counts and percentages. Comparisons between groups for continuous variables were completed with the Wilcoxon rank-sum tests, and the Fisher’s exact test was used for comparison between groups for categorical variables. All statistical tests were 2-sided, and the threshold of significance was set at p = 0.05. Successful alignment was defined as less than 10Δ of deviation. The rate of developing ≥10Δ of misalignment after surgery was calculated by the Kaplan-Meier method.18
Results
During the 20-year study period, 184 new cases of intermittent exotropia were diagnosed in Olmsted County, Minnesota. The historical and clinical characteristic of the 61 (33%) who underwent surgery are shown in Table 1. The mean age at diagnosis for the 61 patients was 4.3 years, and two-thirds were female. Mild amblyopia was found in 4, and the mean initial exotropic angle was 20Δ at distance and 14Δ at near. Statistically significant differences between the 61 patients who underwent surgery and the 123 who did not included the mean age at diagnosis of 4.3 years versus 7.4 years (p < 0.0001), and the mean refractive error of + 0.45 versus + 0.2 D (p = 0.035) for the surgical and the observed group, respectively.
Table 1.
Historical clinical characteristics at presentation of 61 children who underwent surgery for intermittent exotropia in Olmsted County, Minnesota
| Number of boys (%)/girls (%) | 19(31)/742 (69) |
| Number born prematurely (%) | 4/52 (7.7) |
| Mean birth weight in grams (range) | 3,288 (953–4330) |
| Mean age in years at diagnosis (range) | 4.3 (1–18.6) |
| Number with amblyopia (%) | 4 (6.6) |
| Mean initial angle of horizontal deviation at distance (range) | 20Δ (10Δ–45Δ) |
| Mean initial angle of horizontal deviation at near (range) | 14Δ (0Δ–45Δ) |
| Number with inferior oblique dysfunction (%) | 9 (14.8) |
| Number with dissociated vertical deviation (%) | 3 (4.9) |
| Mean cycloplegic refraction (spherical equivalent) (range) | +0.5 D (−7.8 D to +3.1 D) |
The surgical features of the 61 patients who underwent surgery are shown in Table 2. The mean exotropic angle at surgery was 28Δ (range, 10Δ–45Δ) at distance and 24Δ (range, 10Δ–45Δ) at near. Twelve (19.7%) of the 61 children under went a second surgery (10 for recurrent exotropia and 2 for consecutive esotropia), and no patient received 3 or more surgeries during the follow-up time. The final postoperative measurements were recorded in 56 (92%) of the 61 children at mean of 10 years (range, 0 to 26 years) after the first surgery: 31 (55%) of the 56 were within 9Δ of orthotropia. Postoperative stereoacuity (≤3,000 arcsec) was documented in 55 (90%) patients, whereas only 25 (45%) had better than 60 arcsec.
Table 2.
Surgical characteristics of 61 children who underwent surgery for intermittent exotropia
| Mean age in years at surgery (range) | 7.6 (3.3 to 22.8) |
| Mean distance deviation at surgery (range) | 27.8Δ (10Δ–45Δ) |
| Mean near deviation at surgery (range) | 23.8Δ (10Δ–45Δ) |
| Number requiring vertical surgery at initial surgery (%) | 2 (3.2) |
| Number undergoing second surgery (%) | 12 (19.7) |
| Number undergoing third surgery (%) | 0 (0) |
| Mean follow-up in years from final surgery (range)1 | 10.2 (0 to 25.8) |
| Number* with 4 weeks or greater postoperative follow-up (%) | 56 (91.8) |
| Number* within 10Δ of orthotropia postoperatively (%) | 31 (56) |
| Number† with 60 arcsec or better postoperatively (%) | 25/55 (45.5) |
Data includes 56 of the 61 patients.
Data includes 55 of the 61 patients.
The Kaplan-Meier rate of developing greater than 10Δ of misalignment at distance after the first surgery was 54% by 5 years, 76% by 10 years, and 86% by 15 years (Figure 1). Successful motor alignment at distance on the final examination was not associated with the amount of time from diagnosis to surgery, age at surgery, preoperative horizontal distance deviation, final stereopsis A- or V-pattern exotropia, nor type of surgery. Alignment within 9Δ of orthotropia, compared with ≥10Δ, was significantly more likely (p = 0.016) only in those patients with a shorter duration of post-operative follow-up.
FIG 1.
Kaplan-Meier estimate of percentage of patients developing ≥10Δ of postoperative deviation from time of first surgery.
Of the 61 children, 27 (44.3%) underwent a bilateral lateral rectus recession (BLRR), 33 (54.1%) underwent a unilateral lateral rectus recession and medial rectus resection (R/R), and 1 patient had a unilateral lateral rectus recession. Fifteen of the 27 (56%) children who underwent a BLRR were <10Δ from orthotropia versus 19 of 33 (58%) children who underwent an R/R procedure (p = 1.00).
Discussion
This study provides population-based data on the surgical outcomes of 61 of 184 children diagnosed with intermittent exotropia during a 20-year period. Successful surgical alignment, defined as <10Δ from orthotropia, was accomplished in 56% of children after a mean follow-up of 10 years. Although only 20% of the study patients underwent a second surgery, just 45% of patients demonstrated 60 arcsec or better of stereopsis. However, the only clinical factor associated with poor postoperative motor alignment was longer follow-up time (p = 0.016).
The long-term postoperative results from this study demonstrating surgical success in 56% of patients is comparable with previous reports (Table 3).4–14,19 Although the success rates reported in published studies range from 50% to 79%, all had shorter mean postoperative follow-up intervals. In general, studies with shorter periods of follow-up reported higher rates of motor success compared with those with longer follow-up intervals.
Table 3.
Published reports of postoperative motor success in patients with intermittent exotropia
| Study | Success (%) | Definition of success | Average follow-up (years) | Year of publication |
|---|---|---|---|---|
| Burian and Spivey7 | 50% | <10Δ of deviation | 2.5 | 1964 |
| Hardesty et al9 | 51% | no tropia; no supplemental treatment; some stereopsis | 6.1 | 1978 |
| Pratt-Johnson et al8 | 68% | <10Δ of deviation | 1 to 8 | 1977 |
| Richard and Parks10 | 56% | <10Δ of deviation | 2 to 8 | 1983 |
| Stoller et al11 | 58% | <10Δ of deviation | 1 | 1994 |
| Maruo et al12 | 50% | orthotropia, mini- microtropia | 4 | 2001 |
| Jeoung et al13 | 67% | <10Δ of deviation | 1.3 | 2006 |
| Chia et al19 | 56% | <10Δ of deviation | 1 | 2006 |
| Wu et al14 | 79% | <8Δ of deviation | 1 | 2006 |
| Current study | 56% | <10Δ of deviation | 10.2 |
Although we found no difference in the motor success rates between BLRR (56%) and unilateral recess resect (58%) procedures (R/R). Maruo et al12 found that 66.7% of BLRR and 32.8% of R/R were orthotropic or mini-microtropic at a mean of 4 years after surgery (Table 4). In a prospective randomized trial Jeoung and co-authors13 reported that alignment of <10Δ of orthotropia was achieved in 48.3% of BLRR versus 83.3% of R/R in 113 patients after a mean follow-up of 15.8 months. Kushner20 in 1998, however, compared BLRR versus R/R for basic type exotropia and found the R/R procedure (82% success compared with 52%, resp.) to be superior, but found similar success with BLRR (81%) for simulated divergence excess after 1 year of follow-up. More recently Chia and colleagues19 demonstrated that although the R/R procedure obtained better alignment after 1 year follow-up, it was more prone to exotropic drift and consecutive esotropia. They also reported worse outcomes in patients with basic-type versus divergence excess-type intermittent exotropia. Because the subtypes of intermittent exotropia are not defined in this study, we are unable to compare our outcomes with those of Kushner20 and Chia et al.19
Table 4.
Comparison of success rates of bilateral lateral rectus recession (BLRR) vs unilateral lateral rectus recession and medial lateral resection (R/R) for surgical correction of intermittent exotropia (IXT)
| Number of patients | Success (%) | Follow-up (years) | Year of publication | |
|---|---|---|---|---|
| Maruo et al12 | ||||
| BLRR | 210 | 66.7 | 4 | 2000 |
| R/R | 180 | 32.8 | ||
| Jeoung et al13 | ||||
| BLRR | 58 | 48.3 | 15.3 | 2006 |
| R/R | 66 | 83.3 | ||
| Kushner20 (basic- type IXT) | ||||
| BLRR | 19 | 52 | 1 | 1998 |
| R/R | 17 | 82 | ||
| Kushner20 (simulated divergence excess type IXT) | ||||
| BLRR | 68 | 81 | 1 | 1998 |
| Our study | ||||
| BLRR | 27 | 56 | 7.8 | |
| R/R | 33 | 58 | ||
Although we found no clinical factors to predict successful postoperative outcomes in children with intermittent exotropia, other investigators have. Pratt-Johnson and coinvestigators8 concluded that surgery before the age of 4 years was the most significant factor in obtaining good alignment. Saunders and Trivedi21 recently reported that even younger children (mean age, 17 months) responded well to surgery. Of their 12 patients, 7 (58%) were aligned within 10Δ of orthotropia after 5 years of follow-up. Richard and Parks10 and Stoller et al11 reported that the patient’s age at exotropia onset and age at surgery did not adversely affect long-term alignment. Stoller and colleagues also found no correlation between a successful motor outcome and preoperative symptoms and signs of amblyopia, anisometropia, and imcomitance. Gezer et al22 reported that a preoperative deviation of <40Δ and a refractive error greater than 2 D of hyperopia, had a greater likelihood of having <10Δ of misalignment. Neither of these factors, however, was statistically significant in our population.
We also report the long-term sensory outcomes in this cohort of children with intermittent exotropia in 55 of the 61 patients. Twenty-five (45%) had 60 seconds or better arc stereopsis after a mean follow-up of 10 years. Wu et al14 reported 74% of their 34 patients with intermittent exotropia as having better than or equal to 60 seconds of arc after one year of follow-up. They reported performing bilateral lateral rectus recession and unilateral recess resect as necessary, based on the distance deviation. Their motor outcomes, at 1 year, were also better than this study (Table 3), which seems to correspond to their superior sensory outcome.
There are several weaknesses to the findings in this study. Its retrospective nature is limited by imprecise inclusion criteria and uneven follow-up. Second, some of the exotropic patients may have sought care outside of the region, thereby potentially introducing selection bias. The findings from this population may also have been biased, however, toward patients with worse outcomes, since such patients are more likely to return for ophthalmic care. However, the majority of our patients continued to be followed at our institution for their contact lens and spectacles needs. Third, the demographics of Olmsted County limit our ability to extrapolate the findings from this study beyond other semiurban white populations of the United States. Also, we were unable to categorize our patients with intermittent exotropia by their specific type (basic, divergence excess, etc) which, in some studies, have been shown to affect motor outcomes. Finally, although the vast majority of surgery was performed by a fellowship-trained pediatric ophthalmologist who aimed for a slight overcorrection in the immediate postoperative period, we are unable to comment on the success or failure of such a strategy.
In this population-based study of surgery for children with intermittent exotropia, while only 1 in 5 received a second surgery, at the final follow-up examination, 56% of patients were successfully aligned and 45% had high-grade stereopsis. The estimated rate of developing ≥10Δ from orthotropia following the initial surgery in this population was 54% by 5 years and 86% by 15 years.
Acknowledgments
Funded in part by an unrestricted grant from Research to Prevent Blindness Inc., New York, New York.
Footnotes
This study was conducted at Mayo Clinic Rochester Minnesota.
Presented in pan at the 34th Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus, Washington, D.C., April 2-6, 2008.
Literature Search
All articles involving surgical outcomes of exotropia were reviewed, including those that specifically discussed intermittent exotropia. PubMed was the primary database used. Search terms used included exotropia, surgical, population-based, children, outcomes, bilateral lateral rectus recession, unilateral medial rectus resection, and lateral rectus recession.
References
- 1.Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: A population-based study. Ophthalmology. 2005;112:104–8. doi: 10.1016/j.ophtha.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 2.Hatt S, Gnanaraj L. Interventions for intermittent exotropia. Cochrane Database Syst Rev. 2006;3:CD003737. doi: 10.1002/14651858.CD003737.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Nusz KJ, Mohney BG, Diehl NN. The course of intermittent exotropia in a population-based cohort. Ophthalmology. 2006;113:1154–58. doi: 10.1016/j.ophtha.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 4.Cooper EL. Muscle surgery and orthoptics in the treatment of comitant nonaccommodative strabismus. Am J Ophthalmol. 1955;40:883–90. [PubMed] [Google Scholar]
- 5.Folk ER. Surgical results in intermittent exotropia. Arch Ophthalmol. 1956;55:484–87. doi: 10.1001/archopht.1956.00930030488004. [DOI] [PubMed] [Google Scholar]
- 6.Dunlap EA. Surgical results in intermittent exotropia. Trans Pa Acad Ophthalmol Otolaryngol. 1963;16:113–15. [PubMed] [Google Scholar]
- 7.Burian HM, Spivey BE. The surgical management of exodeviations. AmJ Ophthalmol. 1965;59:603–20. [PubMed] [Google Scholar]
- 8.Pratt-Johnson JA, Barlow JM, Tillson G. Early surgery in intermittent exotropia. Am J Ophthalmol. 1977;84:689–94. doi: 10.1016/0002-9394(77)90385-3. [DOI] [PubMed] [Google Scholar]
- 9.Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Ophthalmol. 1978;96:268–74. doi: 10.1001/archopht.1978.03910050136006. [DOI] [PubMed] [Google Scholar]
- 10.Richard JM, Parks MM. Intermittent exotropia: Surgical results in different age groups. Ophthalmology. 1983;90:1172–77. [PubMed] [Google Scholar]
- 11.Stoller SH, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia: A survival analysis. J Pediatr Ophthalmol Strabismus. 1994;31:89–92. doi: 10.3928/0191-3913-19940301-06. [DOI] [PubMed] [Google Scholar]
- 12.Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: Long term outcome regarding changes in binocular alignment; A study of 666 cases. Binocul Vis Strabismus Q. 2001;16:265–70. [PubMed] [Google Scholar]
- 13.Jeoung JW, Lee MJ, Hwang JM. Bilateral lateral rectus recession versus unilateral recess-resect procedure for exotropia with a dominant eye. Am J Ophthalmol. 2006;141:683–8. doi: 10.1016/j.ajo.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 14.Wu H, Sun J, Xia X, Xu L, Xu X. Binocular status after surgery for constant and intermittent exotropia. Am J Ophthalmol. 2006;142:822–6. doi: 10.1016/j.ajo.2006.06.045. [DOI] [PubMed] [Google Scholar]
- 15.Chia A, Roy L, Seenyen L. Comitant horizontal strabismus: An Asian perspective. Br J Ophthalmol. 2007;91:1337–40. doi: 10.1136/bjo.2007.116905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 17.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 19.Chia A, Seenyen L, Long QB. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. JAAPOS. 2006;10:206–11. doi: 10.1016/j.jaapos.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 20.Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol. 1998;116:324–8. doi: 10.1001/archopht.116.3.324. [DOI] [PubMed] [Google Scholar]
- 21.Saunders RA, Trivedi RH. Sensory results after lateral rectus muscle recession for intermittent exotropia operated before two years of age. JAAPOS. 2008;12:132–5. doi: 10.1016/j.jaapos.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Gezer A, Sezen F, Nasri N, Gozum N. Factors influencing the outcome of strabismus surgery in patients with exotropia. J AAPOS. 2004;8:56–60. doi: 10.1016/j.jaapos.2003.08.006. [DOI] [PubMed] [Google Scholar]