Abstract
Objective
To evaluate the cost-effectiveness of non face-to-face interventions for increasing physical activity in sedentary adults. The study took place in Providence, Rhode Island between the years 2000 and 2004.
Methods
239 participants were randomized to: Phone, Print, or a contact control. Phone and Print groups were mailed regular surveys regarding their level of physical activity, motivational readiness and self-efficacy. Surveys were scanned by a computer expert system to generate feedback reports. Phone group participants received feedback by telephone. Print group participants received feedback by mail. The contact control group received mailings unrelated to physical activity. Intervention costs were assessed prospectively, from a payer perspective. Physical activity was measured using the Physical Activity Recall. Ambulatory health service use was assessed via monthly surveys.
Results
The Print intervention was more economically efficient than the Phone intervention in engaging participants in a more active lifestyle.
Conclusion
The Print intervention provides an efficient approach to increasing physical activity. Research is needed to determine the cost-effectiveness of the intervention in a more diverse population, within the context of the health service delivery system, and over a longer period of time.
Keywords: Medical subject headings: economics, exercise, health promotion, physical fitness, primary prevention, randomized controlled trials
Introduction
Over a decade ago the Centers for Disease Control and Prevention (CDC) and the American College of Sports Medicine (ACSM) published a joint summary statement on the health benefits of physical activity and recommended an accumulation of at least 30 minutes of moderate intensity physical activity on most days of the week (Pate et al. 1995). Consistent with this recommendation, Healthy People 2010 identified the need to increase the proportion of adults who meet this physical activity goal (U.S. Department of Health and Human Services 2000). Unfortunately, many adults in the US engage in little or no physical activity. Only about 25% of Americans meet the recommended levels of physical activity (Center for Disease Control 2001), and about 25% of the population engages in no leisure-time physical activity (Center for Disease Control 2004).
Physical inactivity contributes to many disease states including diabetes, cardiovascular disease, hypertension, colon cancer, osteoarthritis and osteoporosis (Ewing et al. 2003). The burden of chronic disease due to sedentary lifestyles can be measured in both physical and economic costs. The financial burden of physical inactivity to the US health care system from cardiovascular disease alone was estimated to be over $23 billion in 2001 (Wang et al. 2004). Thus, there is substantial motivation to identify effective interventions that can be used to increase physical activity in the general public.
Recent meta-analyses have shown home-based physical activity interventions to be more effective than center-based interventions (Hillsdon and Thorogood 1996) and that interventions not involving face-to-face contact to have larger effect sizes (Dishman and Buckworth 1996). Such approaches are also likely to be more economical than center-based interventions. However, few cost analyses of physical activity interventions appear in the literature. These include primary care-based counseling (Stevens et al. 1998; Elley et al. 2004), worksite counseling (Proper et al. 2004), and center-based physical activity interventions (Sevick et al. 2000; see summaries in Table 1). No studies were found comparing the cost-effectiveness of alternative intervention approaches that do not involve face-to-face contact. With this report we evaluate the cost-effectiveness of two intervention approaches that do not require face-to-face contact, and that may have broad reach within the population of sedentary adults: 1) a telephone-based, individualized motivationally tailored feedback intervention and 2) a print-based, individualized motivationally-tailored feedback.
Table 1.
Summary of the literature on cost-effectiveness analyses of interventions to increase physical activity in healthy but sedentary populations. (All costs converted to US$)
| Author (country) | Intervention/Outcomes | Cost |
|---|---|---|
| Stevens, Hillsdon, Thorogood, McArdle (United Kingdom)4 | Primary care-based intervention. Participants referred by general practitioner to exercise development officer for counseling session. Participants Provided information on recommendations for physical activity and health. Participants invited for second counseling session. Movement of participant from “sedentary” to “active” assessed at 8 months. |
Total cost: $117 per intervention group participant Incremental cost-effectiveness: $1,153 to move one participant out of the “sedentary” group (i.e., success in achieving more than four 20-minute episodes of vigorous or moderate-intensity physical activity in a 1-month period). Incremental cost-effectiveness: $4,434 to move one participant to “recommended” levels of physical activity participation (i.e., success in achieving vigorous activity for 20 minutes for 3 days each week, or moderate-intensity physical activity for 30 minutes 5 days a week). |
| Elley, Kerse, Arroll, Swinburn, Ashton, Robinson (New Zealand)5 | Participants were given advice from a general practitioner or nurse regarding physical activity. A “prescription” was FAXed to an exercise specialist who provided telephone counseling on 3 separate occasions over the following 3 months. Physical activity assessed at 12 months. |
Total cost: $120 per intervention group participant. Incremental cost-effectiveness: $1,240 to move one participant out of the “sedentary” group (i.e., success in achieving 2.5 hours or more of moderate-intensity physical activity per week). Incremental cost-effectiveness: $8 per additional kcal/kg/day of energy expenditure per day. |
| Proper, de Bruyne, Hildebrandt, van der Beek, Meerding, van Mechelen (Scandinavia)6 | Worksite physical activity counseling. Over 9 months, participants were offered seven 20-minute consultations to promote physical activity and healthy dietary habits using the individual’s stage of change as a guide. Energy expenditure and submaximal heart rate assessed at 9 months. |
Total cost: $520 per intervention participant. Incremental cost-effectiveness: $3 per additional kcal of energy expenditure per day. Incremental cost-effectiveness: $55 per beat reduction/minute in submaximal heart rate. |
| Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN (USA)7 | Compared two 24-month center-based physical activity interventions. The lifestyle intervention was delivered 31 group sessions over decreasing frequency over the course of the study. Sessions integrated behavior modification and cognitive-behavior modification techniques for behavior change, tailored to the participant’s level of motivational readiness for change The structured intervention participants received an exercise prescription, and 6 months of access to a state-of-the-art fitness facility, under the supervision of a health educator. At the end of the active phase of the intervention, participants met with a staff person to review plans for continued exercise and were provided a referral list of local fitness facilities. |
Total cost:
|
Methods
Design
STRIDE was a randomized, controlled trial to evaluate the effectiveness of interventions delivering theory-based, motivationally-tailored individualized feedback to sedentary adults, with the goal of increasing physical activity. Participants were randomized to one of three groups: 1) telephone-based intervention [Phone]; 2) print-based intervention [Print]; or 3) contact control (Marcus et al. 2007; Marcus et al. In Press) Block randomization was performed, with blocks defined as stage of motivational readiness and gender.
A prospective cost-effectiveness analysis was performed from a payer perspective, including those costs that would borne by and outcomes that would be relevant to a health plan or insurer offering the intervention as part of their covered services. Costs were calculated at 6 and 12 months, and a physical activity recall was obtained at 6 and 12 months. The cost of ambulatory health services used during the study was estimated from monthly reports of health service utilization obtained from study participants.
Sample
Healthy but sedentary (< 90 minutes per week of at least moderate or vigorous physical activity) adults ages 18 to 65 were recruited. Participants were recruited from the community using newspaper advertisements, as well as from a local hospital work site using a variety of communication strategies (e.g., intranet postings, email, and announcements attached to pay stubs). Participants were screened for eligibility by a research assistant via telephone.. Exclusion criteria included: BMI > 35 (which could hamper physical activity uptake and may require a more targeted behavioral weight control approach); a schedule that would make adherence unlikely; plans to move from the area within the year; pregnancy or plans to become pregnant; self-report of more than 3 alcoholic drinks/day on 5 or more days/week; recent psychiatric disorder; current prescription medication that might impair exercise performance or tolerance; or one or more of the following co-morbid conditions: hypertension, heart disease of any kind, an abnormal electrocardiogram, stroke, chronic infectious disease, musculoskeletal problems that would impair ability to exercise, asthma, emphysema, chronic bronchitis, or any other serious medical condition that would make exercise unwise or unsafe.
1700 individuals were screened. The final sample was 239 men and women, who were predominately Caucasian (90.3%), female (82.0%) middle-aged (M = 44.5 years), college-educated (70.6%), and earning > $50,000/year (60.8%). The study arms were comparable on key variables including: age, BMI, baseline physical activity, blood pressure, heart rate, % body fat, and exercise stress testing results. Sample characteristics are summarized in Table 2 (Marcus et al. 2007; Marcus et al. In Press).
Table 2.
Descriptive Statistics by Group, 2000–2004 in Providence, Rhode Island, United States.
| Variable | Phone (n=80) | Print (n=81) | Contact Control (n=78) |
|---|---|---|---|
| Age (years) | 45.16 (8.30*) | 43.44 (10.42) | 44.79 (10.08) |
| Gender (% Female) | 85.00 | 75.31 | 85.90 |
| Race (% Caucasian) | 95.00 | 86.42 | 87.18 |
| Marital Status (% Married) | 68.75 | 62.96 | 58.97 |
| Employed (% Employed) | 91.25 | 90.12 | 89.74 |
| College Graduate (%) | 78.75 | 65.43 | 65.38 |
| Income (% total household income >$50,000) | 62.50 | 55.56 | 47.44 |
| Cigarette Use (% Smokers) | 13.75 | 14.81 | 8.97 |
| Body Mass Index | 27.92 (4.65) | 28.24 (5.16) | 29.49 (6.78) |
| Physical Activity (minutes per week) | 19.75 (26.56) | 20.19 (24.15) | 19.36 (24.51) |
standard deviations in parentheses
Signed informed consent was obtained from all participants. The protocol was approved by the Institutional Review Board at The Miriam Hospital.
Intervention
The theories underlying the proposed intervention were the Stages of Motivational Readiness for Change Model; and Social Cognitive Theory (SCT). The Stages of Change model posits that individuals who are contemplating behavior change move through a series of motivational stages and that counseling message to change behavior should be tailored accordingly (Prochaska and DiClemente 1983). SCT posits that outcome expectations and self-efficacy strongly influence behavior change and maintenance (Bandura 1997).
Phone and Print participants received baseline materials describing the study goal (accumulating 5 days, 30 minutes per day of at least moderate intensity physical activity), and tip sheets for reaching that goal. Both groups mailed-in physical activity logs and brief surveys each month for the 12-month study period. Surveys queried intervention participants about their level of physical activity, current stage of motivational readiness, self-efficacy to engage in physical activity, strategies and techniques for increasing physical activity, and decisional balance. The return of each monthly survey was reinforced with a $10 incentive. Surveys were scanned by a computer expert system, and feedback forms were generated containing theory-based counseling messages individualized to the participants’ situation, based on their survey responses, and aimed to enhance the participant’s perceived capability to engage in and sustain physical activity, and were tailored to the participant’s motivational stage (Marcus, Napolitano et al. 2007). Feedback was communicated to participants via mail or telephone with contacts occurring 14 times over 12 months. Contacts were weekly for the first 4 weeks, biweekly for 8 weeks, monthly for 3 months, and bi-monthly for 6 months.
Phone participants were contacted directly by a health educator. Print participants were mailed the feedback report generated by the computer expert system. The contact control group received mailings unrelated to physical activity on the same schedule as Phone and Print participants, as well as a packet of health information at the beginning of the study. The interventions are described in more detail elsewhere.(Marcus et al. 2007; Marcus et al. 1998a , b).
Measures
Outcomes
The primary outcome was the 7-day Physical Activity Recall Interview (PAR) (Sallis et al. 1985) obtained at 6 and 12 months. The PAR is a widely used, interviewer-administered, self-report measure that assesses physical activity across a range of activity types and intensity levels (Sallis 1997). The PAR has been found to be a valid and reliable measure of physical activity across a broad range of ages (Sallis 1997; Hayden-Wade et al. 2003; Dubbert, Vander Weg et al. 2004). Using PAR data, we determined if the participant achieved 150 minutes or more of physical activity per week.
Health service utilization was assessed via monthly questionnaires of the frequency and reason for physician office visits. Health service encounters were matched to an appropriate CMS (Centers for Medicare and Medicaid Services) code and assigned a reimbursable dollar amount based on the National Physician Fee Schedule Relative Value File, adjusted to 2004 dollars, (Department of Health and Human 2005) not adjusting for geographic location, considering type of provider (e.g., generalist vs. gynecologist) in cost approximation, assuming a visit of intermediate complexity with an established provider.
Costs
Table 3 provides the value of each cost component at 6 and 12 months. Costs include personnel time for delivering the intervention, value of the expert system, curriculum materials, printing, postage, and facility costs. A tracking system was developed that prospectively captured the date of each reports, mailing, survey incentive payments, and telephone contact, as well as the duration of each successful telephone contact. On an approximately biannual basis, study staff completed activity logs recording time devoted to activities not captured on the tracking system, including time required to generate expert system reports, and generate mailings. Research costs (e.g. for measurement visits and to obtain consent) were not included in the analysis. Recruitment costs were included in the analysis as replication of the intervention in real-world settings would require effort to enroll participants in the program, and also evaluate whether they could safely engage in physical activity. (Additional details regarding cost calculations are available upon request).
Table 3.
Cost by intervention arm at 6 and 12 months for Project STRIDE, 2000–2004 in Providence, Rhode Island, United States.
| 6-month costs | 12-month costs | |||||
|---|---|---|---|---|---|---|
| Phone (n=80) | Print (n=81) | Contact Control (n=78) | Phone (n=80) | Print (n=81) | Contact Control (n=78) | |
| Phone interventionist | ||||||
| Counseling | 5,728 | 0 | 0 | 7,098 | 0 | 0 |
| General office activities | 6,880 | 0 | 0 | 13,760 | 0 | 0 |
| Expert system coordinator | ||||||
| Generation of expert system reports | 1,431 | 3,102 | 0 | 2,263 | 4,529 | 0 |
| General office activities | 0 | 4,189 | 0 | 0 | 8,378 | 0 |
| Wellness group | ||||||
| Generation of wellness mailings | 0 | 0 | 1,005 | 0 | 0 | 1,259 |
| Supervision of Phone Interventionist Recruitment | 570 | 0 | 0 | 1,140 | 0 | 0 |
| Personnel costs | 2,106 | 2,106 | 2,106 | 2,106 | 2,106 | 2,106 |
| Advertisement costs | 4,759 | 4,759 | 4,759 | 4,759 | 4,759 | 4,759 |
| Expert System | ||||||
| software | 702 | 702 | 0 | 1,404 | 1,404 | 0 |
| hardware | 1,360 | 1,360 | 0 | 2,720 | 2,720 | 0 |
| system maintenance and supplies | 466 | 466 | 0 | 932 | 932 | 0 |
| Printing and postage | 561 | 1,170 | 503 | 848 | 1,662 | 623 |
| Telephone costs | 295 | 0 | 0 | 354 | 0 | 0 |
| Facilities | 18,997 | 6,333 | 1,267 | 37,994 | 12,665 | 2,533 |
| Total intervention cost | 43,855 | 24,187 | 9,640 | 75,378 | 39,155 | 11,280 |
| Average monthly cost per participant (rounded to nearest dollar) | $91 | $50 | $21 | $79 | $40 | $12 |
| Average incremental cost relative to contact control | $70 | $29 | -- | $67 | $28 | -- |
1. Personnel costs
Personnel costs were estimated by multiplying the amount of time devoted to intervention activities by an hourly wage and fringe rate for each staff person involved in the study. As noted above, staff time requirements were obtained from the tracking system, as well as biannual staff activity logs.
2. Expert System
The value of the expert system was estimated as a capital expenditure and valued at the beginning of the study as follows: an optical scanner with automatic feed at $3,340, scanner software at $1,450, a computer at $2,500, and printer at $700. These costs were annuitized over the 5-year period of the study using the approach described by Shaffer and Haddix, (1996) assuming a discount rate of 5%, a useful life of 5 years, and a value at the end of the study equal to 10% of the original purchase value. Hardware costs are allocated equally between the Phone and Print groups.
The expert system software was developed by the investigators in 1992, by two psychologists and a programmer at a cost of $10,742. In annualizing the value of the software, we assume a discount rate of 5%, a useful life of 20 years, and a $0 “scrap” value at the end of the study (i.e., it is licensed and cannot be resold). Under these assumptions the annual cost of the software is $2,808, with these costs allocated equally between the Phone and Print group.
Ongoing costs for the expert system include replacement of the optical scanner read head at $20 per year, and printer cartridges at $250 per year (in 2004 dollars), again equally allocated between the Phone and Print groups.
3. Printing and postage
Printing and postage costs for each mailing, for each participant, in each group were recorded in the tracking system as described above.
4. Materials
Self-help manuals matched to Stage of Motivational Readiness were sent to participants in the Print group, the cost of which were recorded in the tracking system.
5. Telephone costs
The date and duration of each successful telephone call made to the Phone group was recorded in the tracking system as well as the rate, based upon the call zone in which the participant resided. Unsuccessful calls were also dated and assigned a value of one minute.
6. Facilities
The value of space is estimated at $25.37/square foot in years 2004 dollars, or $1,548/month. The space is considered shared, with the value estimated at the staff’s percent effort devoted to intervention-related activities, with the Phone interventionist’s space estimated at 75% of total, the research assistant’s space estimated at 25% of total, and the research assistant estimated at 5% of total.
Analysis
Regression analysis was used to compare the three groups in terms of change in physical activity at 6 and 12 months, controlling for baseline PAR, season (i.e. spring, summer, fall, winter), and gender. Missing data were addressed by carrying baseline values forward. Real wage and fringe rates were used in calculating personnel costs. Other costs were adjusted for inflation (either inflated or deflated, depending upon the base year of the cost estimate) using the Medical Care Price Deflators of the Consumer Price Index to reflect year 2004 dollars. To adjust for the time preference for money, all costs were discounted 5% annually (Shaffer and Haddix 1996) (Note: Outcomes were not discounted). The ratio of additional dollars spent per average gain in PAR was computed for each intervention arm, relative to the contact control at 6 and 12 months. Health utilization cost estimates were summed for each participant, and intergroup differences in ranks were explored using the Kruskal-Wallis statistic.
Results
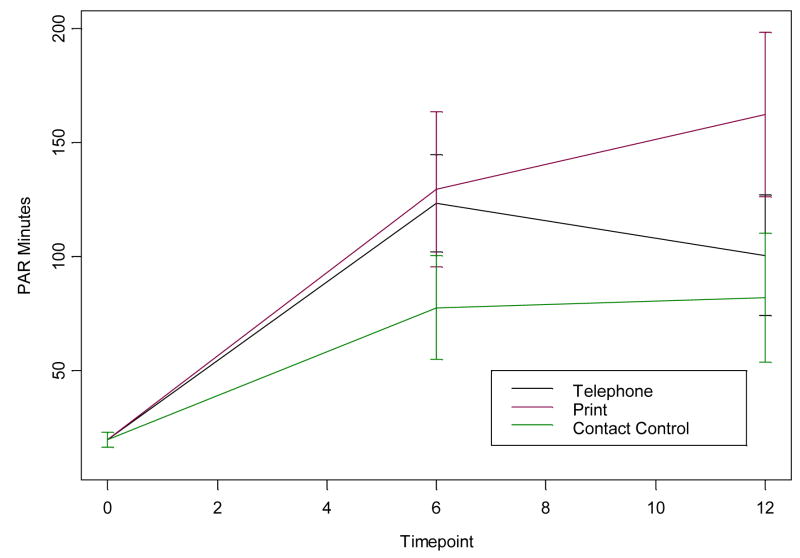
Figure 1 shows that the Phone and Print groups had an equivalent improvement in physical activity at 6 months, compared to the contact control.(Marcus et al. In Press) At 12 months, physical activity declined for the Phone group while the Print group continued to experience increases in time devoted to physical activity. Table 4 outlines the 6 and 12-month PAR results, including incremental cost (i.e., difference in cost between the contact control and intervention arms) and incremental improvement (i.e., difference between contact control and intervention arms in minutes of physical activity) for the Phone and Print interventions relative to the contact control group. At each time point it is clear that the Print group was more effective in improving physical activity and also more cost-effective.
Figure 1. Minutes devoted to physical activity from Physical Activity Recall (PAR) at baseline, 6 and 12 months of participants randomized to Project STRIDE, in Providence, Rhode Island, United States.
Note: Common means was assumed at baseline (N=239)
LCL = 95% Lower Confidence Limit
UCL = 95% Upper Confidence Limit
At 6 months, Telephone>Control, p<.01, Print>Control, p<.01 and Telephone = Print. At 12 months, Telephone=Control, Print>Control, p<.001, and Print>Telephone, p<.05.
Table 4.
Cost effectiveness at 6 months and 12 months for Project STRIDE, 2000–2004 in Providence, Rhode Island, United States.
| Phone | Contact control | ||
|---|---|---|---|
| Cost-effectiveness at 6 months | 123 minutes | 129 minutes | 78 minutes |
| Average incremental unit of improvement in Physical Activity Recall relative to the contact control at 6 months | 45 minutes | 51 minutes | -- |
| Cost-effectiveness w/r to physical activity | $1.56/mo./minute of improvement in Physical Activity Recall | $0.57/mo./minute of improvement in Physical Activity Recall | -- |
| Cost effectiveness under the assumption of reduced time requirements for generating expert system reports | $1.53/mo./minute of improvement in Physical Activity Recall | $0.53/mo./minute of improvement in Physical Activity Recall | -- |
| Cost effectiveness when varying the cost of telephone counseling downward by 1 standard deviation | $1.49/mo./minute of improvement in Physical Activity Recall | $0.57/mo./minute of improvement in Physical Activity Recall | -- |
| Cost-effectiveness at 12 months | 101 minutes | 162 minutes | 82 minutes |
| Average incremental unit of improvement in Physical Activity Recall relative to the contact control at 12 months | 19 minutes | 80 minutes | -- |
| Cost-effectiveness w/r to physical activity | $3.53/mo./minute of improvement in Physical Activity Recall | $0.35/mo./minute of improvement in Physical Activity Recall | -- |
| Cost effectiveness under the assumption of reduced time requirements for generating expert system reports | $3.42/mo./minute of improvement in Physical Activity Recall | $0.35/mo./minute of improvement in Physical Activity Recall | -- |
| Cost effectiveness when varying the cost of telephone counseling downward by 1 standard deviation | $3.37/mo./minute of improvement in Physical Activity Recall | $0.36/mo./minute of improvement in Physical Activity Recall | -- |
Post hoc sensitivity analyses were conducted around the time required to generate expert system reports, and the amount of time required for counseling of the Phone group. In reviewing the data, STRIDE study staff indicated that, as the protocol became established, the expert system reports for the Phone and Print groups required less time than estimated from biannual staff time logs. Therefore sensitivity analyses were conducted under the assumption that Phone expert system reports required 6 minutes/report to generate, and that Print expert system reports required 10 minutes/report to generate and process for mailing. As shown in Table 4, under these new assumptions, the relative cost-effectiveness remained essentially unchanged. Also, there was significant variation in the amount of counseling time costs for the Phone participants ($71.61 ± $20.12 at 6 months and, $88.73 ± $25.79 at 12 months). Thus, we varied the average value of the Phone interventionists’ time downward time by one standard deviation to determine if this altered the relative cost-effectiveness of the 2 interventions. Again, as shown in Table 4, the results remain unchanged.
We examined the total investment required by each intervention approach to successfully engage one participant in a more active lifestyle (150 minutes or more of physical activity per week). At 6 months the cost of moving one person out of sedentary status was $1,290 for the Phone group and $756 for the Print Group. At 12 months these costs were $3,967 and $955 respectively.
While not statistically significant (p=.055), the median cost of health care services used by the contact control group ($41 range $0–719, IQR 102) was twice that of either intervention group ($21 for Phone, range $0–444, IQR 62; and $20 for Print, range $0–496, IQR 82).
Discussion
It is clear from the results that the Print intervention was not only more effective than Phone for improving physical activity, it was also the more cost-effective. While the per participant cost of the Project STRIDE Print intervention ($480 at 12 months) was somewhat greater than the primary care-based interventions by Stevens et al., ($117) (1998) and Elley et al., ($120) (2004) that were described earlier in this report, the cost of successfully engaging one participant in a more active lifestyle was less expensive for the STRIDE Print group ($955) than in Stevens et al., ($1,153) (1998) or Elley et al. ($1,240) (2004). It is important to note that the Elley study had the same duration of follow-up as STRIDE (12 months). The Stevens study followed participants for only 8 months. In the absence of continued contact, some of the gains in physical activity experienced by participants in the Stevens intervention are likely to be lost by 12 months, making the of cost engaging one person in regular physical activity for a full year even higher than the $1,153 figure. The primary care-based interventions described by Stevens et al., (1998) and Elley et al.,(2004) involved only 2–3 contacts and, apparently did not produce effects that were either as large or as sustained as those experienced with the STRIDE Print intervention. While the theory-driven STRIDE intervention may appear to be more costly than similar interventions reported in the literature, STRIDE was more efficient in increasing physical activity.
With that being said, Project STRIDE was designed with primary prevention in mind, and a significant proportion of those screened for the study were ineligible due to obesity, co-existing disease, and/or conditions limiting their ability to exercise (n=865). Consequently, comparisons to similar interventions with clinical populations must be made with caution. It is possible that obesity and conditions commonly seen in primary care settings may serve as barriers to physical activity uptake, although development of disease may also serve as a motivator for lifestyle change. Additional research is needed to examine the cost-effectiveness of the intervention in a more diverse population.
Another limitation of the study is the fact that subjects were voluntary participants in a clinical trial to increase physical activity. Consequently all are likely to be in, at least, the contemplation stage of motivational readiness to engage in exercise. Additional effort, beyond those described in the protocol, may be required to engage those who are not yet considering a more active lifestyle.
Staffing requirements might be different if the interventions were to be replicated within the context of a large primary care population, reducing the cost of both Phone and Print intervention arms. For quality control and consistency of intervention delivery, one primary health educator was involved in delivering the telephone intervention. However, during a medical leave, another person assumed the delivery of the program for 3 months. Therefore, if this program were to be delivered to a larger number of individuals, it is possible to implement training protocols that enable multiple health educators to deliver the information. Also, Phone and Print intervention activities could be performed by those who have other responsibilities.
Recruitment within a clinical population may be less costly than recruitment from the community, and expansion to a larger group of patients may result in greater efficiencies due to economies of scale. However, relying on busy health primary care staff to deliver the intervention could result in inconsistencies and a weakening of effect. In fact, systematic reviews of physical activity interventions delivered within the context of primary care have been very disappointing, resulting in the US Preventive Services Task Force conclusion that there is insufficient evidence to support behavioral interventions to increase physical activity in primary care.(US Preventive Service Task Force 2002; Lawlor and Hanratty 2001; Eaton and Menard 1998; Eden et al. 2002) A weakening of effect would likely be more of a problem with Phone than Print – in that activities associated with Print are mostly clerical in nature. Given that Print is clearly superior to Phone in engaging healthy but sedentary participants in a more active lifestyle and also likely to be less costly than Phone under any scenario, additional research is needed to examine the cost-effectiveness of the Print intervention when delivered within the primary care population. Two of the co-authors (Marcus, Napolitano) are currently involved in testing internet delivery of the Print intervention which, if equally effective to feedback messages delivered via postal mail, would further enhance cost-effectiveness of the intervention.(Marcus et al. 2006)
Of the 239 participants randomized, 91% completed the 6 month assessment, and 86% completed the 12 month assessment. Drop-out rates did not differ significantly by intervention arm. Only those costs realized (i.e, for intervention activities recorded in the tracking system) were included in the analysis. However, outcomes were estimated using an intent-to-treat analysis with baseline values (conservatively) carried forward. Thus, our analysis provides a realistic estimate of resources required to deliver the intervention, with a worst case estimate of physical activity improvements resulting from the intervention.
Finally, there are no data available regarding the long-term effectiveness of this intervention, or the extent of contact required to sustain intervention effects. Additional research is needed to examine differing levels of Print intervention contacts beyond 12 months. Longer term studies will be helpful for identifying the most effective and efficient approach for achieving sustained increases in physical activity, and would allow estimation of downstream cost savings from reduced utilization of health care services.
Conclusion
The Print intervention is an efficient approach to increasing activity in healthy but sedentary adults, and requires a modest investment (about $40 per participant per month for a 12-month program) on the part of the payer. While, these costs may appear large in comparison to the brief, primary care based programs evaluated by Stevens et al.(1998) and Elley et al. (2004), STRIDE appears to be more efficient in successfully engaging people in a more active lifestyle. Additional research is needed to determine the cost-effectiveness of the intervention when delivered to a more diverse population, within the context of the health service delivery system, and over a longer period of time.
Acknowledgments
This research was supported in part through a grant from the National Heart, Lung, and Blood Institute by (#HL64342). The authors would like to acknowledge the individual contributions of: Linda Christian, RN, Robin Cram, M.F.A., Lisa Cronkite, B.S., Santina Ficara, B.S., Maureen Hamel, B.S., Beth Lewis, PhD., Jaime Longval, M.S., Kenny McParlin, Hazel Ouellette, Susan Pinheiro, B.A., Regina Traficante, Ph.D., Jessica Whiteley, PhD., Kate Williams, B.S.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bandura A. Self-Efficacy: The Exercise of Control. New York: Freeman and Co; 1997. [Google Scholar]
- Centers for Disease Control. Physical activity trends--United States, 1990–1998. MMWR. 2001;50:166–168. [Google Scholar]
- Centers for Disease Control. Prevalence of No Leisure-Time Physical Activity – 35 States and the District of Columbia, 1988–2002. MMWR. 2004;53:82–86. [PubMed] [Google Scholar]
- Dishman RK, Buckworth J. Increasing physical activity: A quantitative synthesis. Med Sci Sports Exerc. 1996;28:706–719. doi: 10.1097/00005768-199606000-00010. [DOI] [PubMed] [Google Scholar]
- Dubbert PM, Vander Weg MW, Kirchner KA, Shaw B. Evaluation of the 7-day physical activity recall in urban and rural men. Med Sci Sport Exerc. 2004;36:1646–54. doi: 10.1249/01.mss.0000139893.65189.f2. [DOI] [PubMed] [Google Scholar]
- Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2002;137:208–15. doi: 10.7326/0003-4819-137-3-200208060-00015. [DOI] [PubMed] [Google Scholar]
- Elley R, Kerse N, Arroll B, Swinburn B, Ashton T, Robinson E. Cost-effectiveness of physical activity counseling in general practice. N Z Med J. 2004;117:U1216. [PubMed] [Google Scholar]
- Eaton CB, Menard LM. A systematic review of physical activity promotion in primary care office settings. Br J Sports Med. 1998;32:11–16. doi: 10.1136/bjsm.32.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18:47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-Day PAR. Med Sci Sports Exerc. 2003;35:801–809. doi: 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- Hillsdon M, Thorogood M. A systematic review of physical activity promotion strategies. British Journal of Sports Medicine. 1996;30:84–9. doi: 10.1136/bjsm.30.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawlor DA, Hanratty B. The effect of physical activity advice given in routine primary care consultations: a systematic review. Journal of Public Health Medicine. 2001;23:219–26. doi: 10.1093/pubmed/23.3.219. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally tailored physical activity intervention. Ann Beh Med. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Emmons KM, Simkin-Silverman LR, Linnan LA, Taylor ER, Bock BC, Roberts MB, Rossi JS, Abrams DB. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. Am J Health Promot. 1998;12:246–253. doi: 10.4278/0890-1171-12.4.246. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Lewis B, Williams D, Napolitano M, Whiteley J, Albrecht A, Bock B, Hogan J, Jakicic J, Neighbors C, Sciamanna C, Parisi A, Tate D. Relative Efficacy of Tailored Internet and Tailored Print-Based Physical Activity Interventions: Six-Month Findings Society for Behavioral Medicine. San Francisco, CA: Mar 22–25, 2006. [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, Parisi A, Bock B, Pinto B, Sciamanna C, Jakicic J, Papandonatos GD. Examination of Print and Telephone Channels for Physical Activity Promotion: Rationale, Design, and Baseline Data from Project STRIDE. Contemp Clin Trials. 2007;28:90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Napolitano M, King AC, Lewis BS, Whiteley JA, Albrecht A, Parisi A, Bock B, Pinto B, Sciamanna C, Jakicic J, Papandonatos GD. Telephone versus print delivery of an individualized motivationally-tailored physical activity intervention: Project STRIDE. Health Psychol. doi: 10.1037/0278-6133.26.4.401. In Press. [DOI] [PubMed] [Google Scholar]
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C. Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. The stages and processes of self-change in smoking: Towards an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Proper KI, de Bruyne MC, Hildebrandt VH, van der Beek AJ, Meerding WJ, van Mechelen W. Costs, benefits and effectiveness of worksite physical activity counseling from the employer’s perspective. Scand J Work Environ Health. 2004;30:36–46. doi: 10.5271/sjweh.763. [DOI] [PubMed] [Google Scholar]
- Sallis JF. Seven-day physical activity recall. Med Sci Sport Exerc. 1997;29:S89–S103. doi: 10.1080/02701367.1990.10607494. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- Shaffer PA, Haddix AC. Time Preference. Chapter 6. In: Haddix AC, Teutsch SM, Shaffer PA, editors. Chapter 6: Time Preference. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. Oxford University Press; New York: 1996. [Google Scholar]
- Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45–74 year old men and women: a randomized controlled trial. Br J Sprts Med. 1998;32:236–241. doi: 10.1136/bjsm.32.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN. Cost-Effectiveness of Lifestyle and Structured Exercise Interventions in Sedentary Adults: Results of Project ACTIVE. Am J Prev Med. 2000;19:1–8. doi: 10.1016/s0749-3797(00)00154-9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. Vol. 2. Washington, DC: US Dept of Health and Human Services; 2000. Conference ed. [Google Scholar]
- U.S. Department of Health and Human Services. Centers for Medicare and Medicaid Services. 2005 National Physician Fee Schedule Relative Value File. 2005 http://www.cms.hhs.gov. (June 22, 2006)
- U.S. Preventive Services Task Force. Behavioral counseling in primary care to promote physical activity: recommendation and rationale. Annals of Internal Medicine. 2002;137:205–7. doi: 10.7326/0003-4819-137-3-200208060-00014. [DOI] [PubMed] [Google Scholar]
- Wanf G, Pratt M, Macera CA, Zheng ZJ, Heath G. Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med. 2004;28:88–94. doi: 10.1207/s15324796abm2802_3. [DOI] [PubMed] [Google Scholar]