Abstract
Objective
To investigate the incidence of infantile esotropia from a defined population in the United States over a 30-year period. Recent reports from the United Kingdom have suggested that strabismus or strabismus surgery is occurring less frequently today than in previous years.
Methods
The medical records of all patients diagnosed with infantile esotropia within Olmsted County, Minnesota, from January 1, 1965, through December 31, 1994, were retrospectively reviewed.
Results
The birth prevalence of infantile esotropia during the 30-year period was 25 (95% confidence interval, 21–29) per 10 000, or 1 in 403 live births. Although there were slightly more cases of infantile esotropia in the earlier years (45 from 1965–1974, 51 from 1975–1984, and 34 from 1985–1994), the change in incidence over time was not statistically significant (P = .32). The mean number of surgeries performed on each patient in this cohort was similar during the 30-year study: 1.8 for those diagnosed from 1965 to 1974, 1.9 for 1975 to 1984, and 1.6 for 1985 to 1994.
Conclusions
The incidence of infantile esotropia in this population has not significantly changed from 1965 through 1994. Moreover, the rate of surgical intervention over these years is similar for this patient population.
Several reports from the United Kingdom have described a decrease in the incidence of strabismus or strabismus surgery in recent years.1–4 Explanations for this decline have included the implementation of childhood vision screening programs and the more frequent correction of the full hyperopic refractive error. These reports generally include all forms of esotropia or strabismus without emphasis on a particular subtype. Of these studies, only one is population based,1 while the other 3 are reviews of clinical, surgical, or hospital records without regard to the patient’s residency status.2–4 The purpose of this study was to ascertain trends in the incidence of infantile esotropia, also known as congenital esotropia, as well as the incidence of surgery for infantile esotropia, over a 30-year period using a population-based medical record retrieval system.
METHODS
The medical records of all patients residing in Olmsted County, Minnesota, and diagnosed with infantile esotropia from January 1,1965, through December 31, 1994, were reviewed retrospectively. Institutional review board approval was obtained for this study. Potential cases of infantile esotropia were identified by using the resources of the Rochester Epidemiology Project, a medical records linkage system designed to capture data on any patient-physician encounter in Olmsted County, Minnesota.5,6 The racial distribution of Olmsted County residents during the years of this study was more than 95% white and less than 3% each for Asian, African, and Native American. The population of this county, which ranged from 81 200 in 1965 to 114 205 in 1994, is relatively isolated from other urban areas, and virtually all medical care is provided to residents by Mayo Clinic or Olmsted Medical Group and their affiliated hospitals.
The medical records of all patients younger than 19 years who were diagnosed with any form of esotropia from the years 1965 through 1994 were reviewed by a pediatric ophthalmologist (B.G.M.). A diagnosis of infantile esotropia was confirmed by the same reviewer and defined as a nonaccommodative esotropia that developed by 6 months of age in a neurologically intact child. The parental recollection of the age at onset and the presence of dissociated vertical deviation or other markers of early-onset strabismus were relied on for late-presenting patients. Trained residency checkers verified each patient’s residency status at the time of birth and at diagnosis using information from city and county directories. Children not residing in Olmsted County at the time of their diagnosis were excluded. The entire medical and surgical record of those diagnosed with infantile esotropia was carefully reviewed through the date of their final examination.
The incidence rate for the cohort was calculated by dividing the number of cases diagnosed at the 2 medical institutions by Olmsted County birth data for 1965 through 1994. The 95% confidence intervals for the prevalence were calculated using the Poisson approximation to the binomial. The relation of incidence rates to age, sex, and decade of diagnosis was assessed by generalized linear models and assuming a Poisson error structure. Continuous data are presented as a mean with a standard deviation, and categorical data are presented as counts and percentages. Comparisons between groups for continuous variables were completed using Wilcoxon rank sum tests and the Fisher exact test was used for comparisons between groups for categorical variables. All statistical tests were 2-sided, and the threshold of significance was set at α=.05.
RESULTS
One hundred thirty new cases of infantile esotropia were diagnosed in Olmsted County, Minnesota, during the 30-year study period. The historical and initial clinical characteristics of the 130 children combined, as well as by decade, are shown in the Table. There were 64 female (49%) and 66 male (51%) incident cases. The birth prevalence of infantile esotropia during the 30-year period was 25 (95% confidence interval, 21–29) per 10,000, or 1 in 403 live births. The mean birth weight of the 130 children was 3316 g (range, 1050–4630 g) and 16 (12.3%) were born prematurely (<37 weeks’ gestation). A family history of strabismus was positive in 36 of the 76 patients (45%) for which these data were documented. The median age at diagnosis was 7.4 months (range, 2–59 months), with 120 of the 130 patients (92.3%) diagnosed by 18 months of age. The principal ocular findings included amblyopia in 48 (38.6%), a median esotropic deviation of 30 prism diopters (range, 10–90 prism diopters), and a mean cycloplegic refraction of +1,84 diopters.
Table.
Historical and Initial Clinical Characteristics of 130 Children With Infantile Esotropia, by Decade, from 1965 through 1994a
| Factor | 1965–1974 | 1975–1984 | 1985–1994 | 1965–1994 | P value |
|---|---|---|---|---|---|
| No. of births in Olmsted Country, MN | 17 655 | 16 492 | 16 425 | 50 572 | |
| No. of cases | 45 | 51 | 34 | 130 | .32 |
| No. (%) of boys/girls | 25 (56)/20 (44) | 28 (55)/23 (45) | 13 (38)/21 (62) | 66 (51)/64 (49) | .24 |
| Premature births, No./total no.(%) | 3/40 (7.5) | 5/45 (11.1) | 8/33 (24.2) | 16/118 (13.6) | .12 |
| Birth weight, g, mean (range) | 3375 (1984 to 4540) | 3337 (1540 to 4261) | 3212 (1050 to 4630) | 3316 (1050 to 4630) | .90 |
| Age at diagnosis, mo, median (range) | 7.7 (3 to 59) | 6.7 (3 to 36) | 7.7 (2 to 39) | 7.4 (2 to 59) | .84 |
| Amblyopia, No./total no.(%) | 24/43 (55.8) | 15/51 (29.4) | 10.33 (30.3) | 49/127 (38.6) | .02 |
| Deviation, PD, median. (range) | 36 (20 to 60) | 38 (10 to 90) | 33 (14 to 60) | 30 (10 to 90) | .48 |
| IO dysfunction, No./total no.(%) | 5/45 (11.1) | 5/49 (10.2) | 2/34 (5.9) | 12/128 (9.4) | .80 |
| DVD, No./total No.(%) | 0/45 (0) | 0/51 (0) | 2/34 (5.9) | 2/130 (1.5) | .07 |
| Cycloplegic refraction (spherecial equivalent), mean (range), D | +1.69 (−0.75 to 4.25) | +1.77 (−1.81 to 5.00) | +2.14 (−1.00 to 3.50) | +1.84 (−1.81 to 5.0) | .08 |
Abbreviations: D, diopter; DVD, dissociated vertical deviation; IO, inferior oblique; PD, prism diopter.
Categorical variables are reported using number (percentage) and P values were obtained using the Fisher exact test. Continuous variables are reported using mean (minimum-maximum) and P values for the effect of decade were obtained using the Kruskal-Wallis test.
Of the 130 study patients, 45 were diagnosed from 1965 to 1974; 51, from 1975 to 1984; and 34, from 1985 to 1994 (P= .32). There was no significant difference in the age at diagnosis between the decade cohorts (P=.84). Comparing the numbers of cases of infantile esotropia with the numbers of live births in Olmsted County during this period showed no significant change over the 30-year study period. From 1965 to 1974, there were 392 live births for every child diagnosed with infantile esotropia; from 1975 to 1984, there were 323 live births for every child diagnosed with infantile esotropia; and from 1985 to 1994, there were 483 live births for every child diagnosed with infantile esotropia (P= .32).
Adjusting for the variable follow-up between the 3 decades, there was no significant difference in the number of surgeries per decade cohort. Overall, the 130 patients underwent a mean of 1.8 surgeries during a mean follow-up period of 13.5 years from their date of diagnosis. By decade, patients diagnosed between 1965 and 1974 underwent 1.8 surgeries per patient during 16.9 years of follow-up from diagnosis, patients diagnosed between 1975 and 1984 underwent 1.9 surgeries per patient during 13.5 years of follow-up, and patients diagnosed between 1985 and 1994 underwent 1.6 surgeries per patient during 9.1 years of follow-up (P=.74).
COMMENT
This study provides population-based data on the incidence of infantile esotropia over a 30-year period from an upper Midwest population of the United States. During the study period, there was no significant change in the numbers of children diagnosed with infantile esotropia, and there was no significant change in the number of surgeries performed on these children.
Infantile esotropia has, for decades, been considered the most common form of strabismus. Prior studies have reported that infantile esotropia occurs in 1% to 2% of all new-born children,7–12 and even recent publications refer to it as the most common form of pediatric strabismus.13–19 However, such statements are in contrast to the findings from this study in which only 1 in 403 newborns were diagnosed with infantile esotropia. Other recent reports from this population have reported similar results, with infantile esotropia making up only 8.1% of all forms of esotropia.20, 21 The previously reported higher incidence of infantile esotropia may have included children with central nervous system disorders9,22–24 or acquired nonaccommodative esotropia, distinct forms of early-onset esotropia that have, in fact, been shown to occur more frequently than infantile esotropia.21 The elevated prevalence of infantile esotropia may also be due, at least in part, to its apparent ubiquity in the outpatient setting; the commonly associated disorders of amblyopia, inferior oblique dysfunction, dissociated vertical deviations, nystagmus, and consecutive deviations invariably lead to more frequent and complicated office consultations, increasing the relative frequency of examinations compared with other forms of childhood esotropia.
This study also showed no significant change in the incidence of infantile esotropia or in the frequency of surgery for infantile esotropia from 1965 through 1994. Previous studies from the United Kingdom have reported a decrease in the diagnosis of strabismus, a decrease in the diagnosis of esotropia, and a decline in the surgical treatment of strabismus.1–4 Ferguson and colleagues1 reported a 5.2% decrease in admissions for strabismus surgery in the Oxford region of England from 1975 through 1985, despite a 16.3% overall increase in ophthalmology admissions. Arora et al2 also reported a decrease in the number of strabismus surgeries by 41.2% in England and Wales from 1989 to 1999 and a decrease of 26.1% in Ontario, Canada, from 1994 to 2000. MacEwen and Chakrabarti3 reported that, between 1986 and 1996, the incidence of esotropia in Scotland and Tayside was stable but that overall numbers of strabismus surgeries fell by 58% to 59%, with esotropia surgery dropping by 63% to 69%. Carney et al4 reported a decrease in the incidence of esotropia in children by 55% and a decrease in the occurrence of strabismus surgery in West Berkshire by 42%. However, they also noted that children younger than 2 years were the only group in which the incidence of esotropia did not decline. This last observation appears to correlate with a consistent incidence of infantile esotropia as was found in this study.
Explanations for the decreasing incidence of strabismus and strabismus surgery observed in the United Kingdom have been postulated. The implementation of child-hood vision screening programs has been suggested as one cause for the decreased frequency of strabismus surgery by Ferguson et al1 and Carney et al.4 They both argued that screening programs improved the early diagnosis of strabismus and, because of this, children were more successfully managed with nonsurgical measures. MacEwen and Chakrabarti3 disagreed, stating that well-established screening programs were in place for their patients and did not appreciably decrease the age at strabismus diagnosis. They postulated that increased spectacle correction of the full hyperopic refractive error was a significant factor for the decrease in the frequency of strabismus surgery. While these factors could potentially influence the frequency of surgery for the acquired forms of esotropia, such as accommodative esotropia or the incidence of strabismus in older children, they are less likely to influence the incidence of infantile esotropia, which is unrelated to significant refractive error or screening programs.
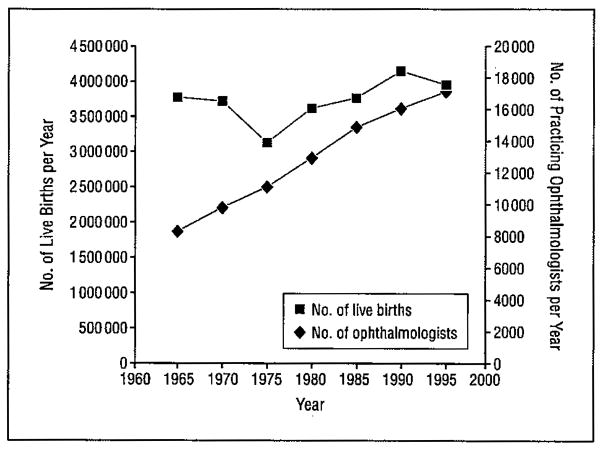
In the United States, there are anecdotal reports among practicing ophthalmologists of a perceived decrease in the incidence of infantile esotropia over the past several decades. While this report found no change in the incidence of infantile esotropia from 1965 to 1994, there may be an explanation for this perception. Although the birth rate in the United States rose by only 3.7% between 1965 and 1994 (from 3 760 000 live births in the United States in 1965 to 3 900 000 live births in the United States in 1994),25 the number of practicing ophthalmologists in the United States rose by 108%, from 8397 physicians to 17 464, during the same period (Figure).26,27 In 1965, there were approximately 448 children born for each practicing ophthalmologist. Assuming a relatively constant incidence of infantile esotropia (at 1 in 403 live births in this study), and assuming that these patients were distributed evenly among practicing ophthalmologists, in 1965 each ophthalmologist would have diagnosed 1.11 new cases of infantile esotropia during the year. However, in 1994, there were approximately 223 children born for each ophthalmologist in practice, allowing each to have diagnosed only 0.55 new case of infantile esotropia. Thus, individual physicians in 1994 were diagnosing half as many patients with infantile esotropia per year as their predecessors were in 1965, which would facilitate the perception that the disorder had become less common over time.
Figure.
Number of live births per year in the United States and number of practicing ophthalmologists per year in the United States, 1965 to 1994.
Regardless of changing demographics, there are several weaknesses to the findings in this study. Its retrospective nature is limited by imprecise inclusion criteria and unequal follow-up. However, the primary purpose of this study was to determine the incidence of infantile esotropia over time, and all children with any form of esotropia diagnosed during the study years were retrospectively reviewed by one of us (B.G.M.) for uniformity of diagnosis. Second, some residents of this population may have sought care outside Olmsted County, artificially decreasing the incidence of infantile esotropia, although the relative isolation of this population from other urban areas makes this occurrence rare. Third, this retrospective cohort may have unknowingly included some children with acquired forms of esotropia, thereby artificially increasing the incidence of infantile esotropia. We sought to overcome this weakness by confirming age at onset or ocular findings of infantile esotropia in the late-presenting infants. Finally, the demographics of Olmsted County limit our ability to extrapolate the findings from this study beyond other semiurban white populations of the United States.
In this population-based cohort of 130 patients from Olmsted County, Minnesota, neither the incidence of infantile esotropia nor the number of surgical procedures significantly changed from 1965 through 1994. A disproportionate increase in the number of practicing ophthalmologists compared with the number of live births in the United States during the same period may have contributed to a perceived decline in the incidence of this disorder. Further population-based studies are warranted to determine if there is a change in the incidence of other forms of strabismus.
Acknowledgments
Funding/Support: This study was funded in part by an unrestricted grant from Research to Prevent Blindness, Inc.
Footnotes
Financial Disclosure: None reported.
References
- 1.Ferguson JA, Goldacre MJ, Henderson J, Bron AJ. Ophthalmology in the Oxford region: analysis of time trends from linked statistics. Eye. 1991;5(pt 3):379–384. doi: 10.1038/eye.1991.61. [DOI] [PubMed] [Google Scholar]
- 2.Arora A, Williams B, Arora AK, McNamara R, Yates J, Fielder A. Decreasing strabismus surgery. Br J Ophthalmol. 2005;89(4):409–412. doi: 10.1136/bjo.2004.053678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacEwen CJ, Chakrabarti HS. Why is squint surgery in children in decline? Br J Ophthalmol. 2004;88(4):509–511. doi: 10.1136/bjo.2002.016618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carney CV, Lysons DA, Tapley JV. Is the incidence of constant esotropia in child-hood reducing? Eye. 1995;9(pt 6)(suppl):40–41. [PubMed] [Google Scholar]
- 5.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245(4):54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 6.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71(3):266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 7.Caputo AR, Gou S, Wagner RS, Picciano MV. Preferred postoperative alignment after congenital esotropia surgery. Ann Ophthalmol. 1990;22(7):269–272. [PubMed] [Google Scholar]
- 8.Helveston EM, Ellis FD, Schott J, et al. Surgical treatment of congenital esotropia. Am J Ophthalmol. 1983;96(2):218–228. doi: 10.1016/s0002-9394(14)77790-6. [DOI] [PubMed] [Google Scholar]
- 9.Nelson LB, Wagner RS, Simon JW, Harley RD. Congenital esotropia. Surv Ophthalmol. 1987;31(6):363–383. doi: 10.1016/0039-6257(87)90030-0. [DOI] [PubMed] [Google Scholar]
- 10.Graham PA. Epidemiology of strabismus. Br J Ophthalmol. 1974;58(3):224–231. doi: 10.1136/bjo.58.3.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duke-Elder S. System of Ophthalmology. Vol. 6. St Louis, MO: Mosby; 1973. pp. 584–585. [Google Scholar]
- 12.Friedman Z, Neumann E, Hyams SW, Peleg B. Ophthalmic screening of 38,000 children, age 1 to 2½ years, in child welfare clinics. J Pediatr Ophthalmol Strabismus. 1980;17(4):261–267. doi: 10.3928/0191-3913-19800701-16. [DOI] [PubMed] [Google Scholar]
- 13.vonNoorden GK, Campos EC. Binocular Vision and Ocular Motility; Theory and Management of Strabismus. St Louis, MO: Mosby; 2002. p. 321. [Google Scholar]
- 14.Optometric Clinical Practice Guideline: Care. of the Patient With Strabismus: Esotropia and Exotropia. St Louis, MO: American Optometric Association; 1999. American Optometric Association Consensus Panel on Care of the Patient With Strabismus; p. 12. [Google Scholar]
- 15.Trigler L, Siatkowski RM. Ophthalmic pearls/pediatrics: managing infantile esotropia. EyeNet. 2001;5:47–48. [Google Scholar]
- 16.Trigler L, Siatkowski RM. Factors associated with horizontal reoperation in congenital esotropia. JAAPOS. 2002;6(1):15–20. doi: 10.1067/mpa.2002.120644. [DOI] [PubMed] [Google Scholar]
- 17.Rowe FJ. Long-term postoperative stability in infantile esotropia. Strabismus. 2000;8(1):3–13. [PubMed] [Google Scholar]
- 18.Gunton KB, Nelson BA. Evidence-based medicine in congenital esotropia. J Pediatr Ophthalmol Strabismus. 2003;40(2):70–73. doi: 10.3928/0191-3913-20030301-04. [DOI] [PubMed] [Google Scholar]
- 19.Major A, Maples WC, Toomey S, DeRosier W, Gahn D. Variables associated with the incidence of infantile esotropia. Optometry. 2007;78(10):534–541. doi: 10.1016/j.optm.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 20.Mohney BG, Erie JC, Hodge DO, Jacobsen SJ. Congenital esotropia in Olmsted County, Minnesota. Ophthalmology. 1998;105(5):846–850. doi: 10.1016/S0161-6420(98)95024-2. [DOI] [PubMed] [Google Scholar]
- 21.Greenberg AE, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood esotropia: a population-based study. Ophthalmology. 2007;114(1):170–174. doi: 10.1016/j.ophtha.2006.05.072. [DOI] [PubMed] [Google Scholar]
- 22.Robb RM, Rodier DW. The broad clinical spectrum of early infantile esotropia. Trans Am Ophthalmol Soc. 1986;84:103–116. [PMC free article] [PubMed] [Google Scholar]
- 23.Wright KW, editor. Pediatric Ophthalmology and Strabismus. St Louis, MO: Mosby; 1995. pp. 179–194. [Google Scholar]
- 24.Archer SM, Helveston EM. Strabismus and eye movement disorders. In: Isen-berg SJ, editor. The Eye in Infancy. 2. St Louis, MO: Mosby; 1994. p. 257. [Google Scholar]
- 25.US Census Bureau. The 2008 Statistical Abstract: Table 77. [Accessed March 12,2008];Live Births, Deaths, Marriages, and Divorces: 1960 to 2006. http://www.census.gov/compendia/statab/tables/08s0077.pdf.
- 26.Roback G, Randolph L, Seidman B. Physician Characteristics and Distribution in the US. Chicago, IL: American Medical Association; 1990. p. 20. [Google Scholar]
- 27.Randolph L, Seidman B, Pasko T. Physician Characteristics and Distribution in the US. Chicago, IL: American Medical Association; 1997. p. 20. [Google Scholar]