Abstract
Lung cancer is the major cancer killer worldwide, and 5-yr survival is extremely poor (≤15%), accentuating the need for more effective therapeutic strategies.
Significant advances in lung cancer biology may lead to customised therapy based on targeting specific genes and pathways. The main signalling pathways that could provide roadmaps for therapy include the following: growth promoting pathways (Epidermal Growth Factor Receptor/Ras/PhosphatidylInositol 3-Kinase), growth inhibitory pathways (p53/Rb/P14ARF, STK11), apoptotic pathways (Bcl-2/Bax/Fas/FasL), DNA repair and immortalisation genes.
Epigenetic changes in lung cancer contribute strongly to cell transformation by modifying chromatin structures and the specific expression of genes; these include DNA methylation, histone and chromatin protein modification, and micro-RNA, all of which are responsible for the silencing of tumour suppressor genes while enhancing expression of oncogenes.
The genetic and epigenetic pathways involved in lung tumorigenesis differ between smokers and nonsmokers, and are tools for cancer diagnosis, prognosis, clinical follow-up and targeted therapies.
Keywords: Lung cancer pathology, molecular biology, molecular genetics, molecular pathology, molecular therapy, signal pathways
Nonsmall cell lung cancer (NSCLC) is the major cancer killer worldwide in both sexes, accounting for > 1.2 million deaths each year [1]. Current standard therapies rarely cure the disease and the overall 5-yr survival rate is only 15% because NSCLC is usually a systemic disease at the time of presentation. Of lung cancers, 85% are caused by tobacco smoke, which induces a stepwise accumulation of genetic and epigenetic abnormalities leading to pre-invasive lesion and invasive lesion, as well as the metastatic process. However, another category of lung cancer, accounting for 20% of adenocarcinomas (ADCs), occurs in never-smoking patients and uses different signalling pathways for tumour development [2]. A recent advance in spiral computed tomography gives some hope of improving early detection, at least for peripheral lung cancer [3, 4]. However, significant advances are being made in NSCLC tumour biology that may ultimately lead to customisation of therapy based on the molecular characteristics of the tumour, as well as on the patient’s clinicopathological condition.
Extensive molecular genetic studies of lung cancer targeted at specific genes and pathways [5] or by genome-wide approaches [6, 7] have shown that clinically overt lung cancers have multiple genetic and epigenetic alterations (>20 per tumour) [8].
Histologically normal cells in smokers, as well as pre-neoplastic cells, already display a number of genetic and epigenetic abnormalities, suggesting a sequential development from normal epithelial cells through a multistep process in multiple areas of the respiratory field, usually coincident with cigarette smoking [9]. This field of cancerisation phenomena, which is both multistep and multicentric, is considered to be universal in smoking patients, and explains the rate of second primaries (3% per year) in patients treated for a first primary tumour. The aims of the present review article are: 1) to provide a comprehensive summary of the signalling pathways involved in the pathogenesis of lung cancer, and 2) to discuss how these are the subject of ongoing translational efforts to offer tools for early detection and diagnosis and to bring effective drugs to clinics.
CAUSES (AETIOLOGY) OF LUNG CANCER
Major histological types of lung cancer (small cell lung cancer (SCLC), squamous cell carcinoma (SCC) and ADC) derive from different compartments in the lung: SCLC and SCC and some (20%) ADC arise in the central compartment of conducting bronchial airways from a putative stem cell, the basal bronchial cell. This candidate stem cell is capable of differentiation towards either ciliated or mucous cells, which can give rise to central ADC and possibly neuroendocrine cells of terminal bronchioles [2, 10–12]. The terminal respiratory unit, consisting of the peripheral compartment respiratory bronchioles and alveoli, gives rise to peripheral ADC from a putative stem cell candidate for self-renewal and proliferation, the bronchioloalveolar stem cell, which is better recognised by pathologists as Clara cells (expressing CC10) and type-II pneumonocytes (expressing surfactants and their transcription factor, TTF1). Lung cancer in non- or never-smokers arises in the peripheral compartment, driven by as yet poorly identified exogeneous carcinogens, among which passive smoking should be considered.
The majority of lung cancers, 85% of NSCLC and 98% of SCLC, arise in smokers. Carcinogens from tobacco smoke target both the central and peripheral compartments. Among the 20 carcinogens that are present in tobacco smoke and strongly associated with lung cancer development, the best known are polycyclic aromatic hydrocarbons and nicotine-derived nitroso-aminoketone, which lead to genetic mutations through DNA adduct formation [13]. Adduct formation is caused by metabolic activation of these carcinogens by P450 cytochromes, enzymes encoded by the CYP family of genes, and glutathione S-transferases (GSTs). Repair of these adducts is linked to adduct excision, which is mainly led by the nucleotide excision repair family, including ERCC1 and XRCC. Critical mutations may occur due to the persistence of DNA adduct formation, such as p53, and Ras gene mutation of the transversion type (i.e. substituting a pyrimidine for a purine and vice versa) rather than the transition type, as is seen in nonsmokers (i.e. substituting purine for purine and pyrimidine for pyrimidine). Oxidative lesion also occurs under the influence of tobacco carcinogens; the major oxidative lesion is 8-oxoguanine, which can be repaired by 8-oxoguanine DNA N-glycosylase 1 (OGG1). Candidate susceptibility genes in lung cancer are those involved in carcinogen metabolism and DNA repair. However, epidemiological studies have shown that <10–20% of smokers develop cancer, suggesting genetic determinants of susceptibility. A number of polymorphisms at cytochrome P450 1A1 gene and GSTM1 homozygous deletion have been associated with increased lung cancer risk [14, 15]. In addition, susceptibility to lung cancer may rely on different capacities of DNA repair. Polymorphisms in the DNA repair gene, which include base excision repair (XRCC1 and OGG1), nucleotide excision repair (ERCC1-2 and XPA), double-strand DNA break repair (XRCC3) and mismatch repair genes (MLH1 and MSH2), have been linked to lung cancer risk [16]. However, it is striking that they have not been identified as risk factors in the recent, broad genomic investigation of polymorphisms predisposing to lung cancer risk [17, 18].
Recently, three parallel genetic-wide analyses linking susceptibility loci to lung cancer have shown a nicotinic receptor polymorphism at chromosomal locus 15q25, linking gene variants of acetylcholine receptors 3 and 5 to a higher risk of lung cancer [17] and/or nicotine addiction [18]. While these genes are described as susceptibility genes, activated cholinergic signalling has been shown both to provide an autocrine growth loop in SCC where cholinergic signalling is upregulated, and to exert pro-inflammatory functions in chronic obstructive pulmonary disease (COPD). This introduces a confounding factor in the lung cancer risk prediction, as inferred from the close link between COPD and lung cancer in smokers [19]. Blocking cholinergic signalling could limit the nicotine-stimulated growth, which shows that these nicotinic receptors are also involved in lung tumorigenesis [11].
Although most cases of lung cancer are due to tobacco smoke, 25% of lung cancer cases worldwide are not attributable to smoking. Striking differences in the epidemiological, clinical and molecular characteristics in lung cancer arising in nonsmokers and smokers as compared with smokers have been recognised [2].
Despite the fact that the first cause of lung cancer risk is, indeed, tobacco consumption, epidemiological studies have shown a 2.5-fold increased risk attributable to family history of lung cancer [20], implying a major susceptibility locus at 6q23–25 [21].
ABNORMALITIES IN GROWTH-STIMULATORY SIGNALLING PATHWAYS
The genetic abnormalities linked to risk of lung cancer should be regarded in the context of signalling pathways having their main functions altered, rather than focusing on individual factors. Several pathways with major components have their functions altered in lung cancer, and these pathways are emerging as having considerable importance with regard to targeted therapy. Most stimulatory signalling pathways are led by oncogenes, which drive cells towards a malignant phenotype, proliferation and escape from apoptosis. Mutated oncogenic proteins cause an addiction of tumour cells to their abnormal functions, a concept referred to as “oncogene addiction” [12]. When this abnormal function is inhibited or removed by a target drug, cells die, and this provides a tremendous opportunity for pharmacogenic susceptibility: As the genetically normal cells are not addicted to the mutant protein, they will be resistant to the targeted drug. In contrast to normal cells, the “addicted” tumour cell is fully dependent for survival of these abnormal or overexpressed oncogenic functions [12].
Epidermal growth factor receptor signalling pathway
Epidermal growth factor receptor deregulation
Of the ~90 known tyrosine kinases (TKs), the receptor TKs (RTKs) form a group of 58 cell-surface growth factor receptors with ligand-mediated TK activity [22]. Whereas RTK activity in normal resting cells is tightly regulated, mutations or deregulated expression might cause them to function as potent oncogenes. Epidermal growth factor receptor is the prototypical member of a family of four RTKs, EGFR (ERBB1, HER1), ERBB2 (HER2, Neu), ERBB3 (HER3) and ERBB4 (HER4) [23]. ERBB receptors are composed of an extracellular ligand-binding domain, a transmembrane segment and an intracellular TK domain followed by a regulatory C-terminal segment. The greatest sequence homologies among the four genes are in the TK domain (59–81% identity). Multiple ligands activate the different family members; those for EGFR include epidermal growth factor, transforming growth factor-α and amphiregulin. Ligand binding enables the formation of homo-or heterodimer complexes and results in TK activation and receptor transphosphorylation. This in turn creates docking sites for a diverse set of cytoplasmic signalling molecules and results in the activation of pathways including Ras, phosphatidylinositol-3-kinase (PI3K). EGFR deregulation has been observed in multiple tumour types, including NSCLCs [24]. Hirsch et al. [25] identified frequent EGFR protein overexpression (62%) in NSCLCs of squamous cell and ADC subtypes. EGFR overexpression is often associated with adverse prognosis [26]. The RTK superfamily of cell surface receptors serve as mediators of cell signalling via extracellular growth factors. Members of the ERBB family of RTKs have received much attention due to their strong association with malignant proliferation.
The Ras/mitogen-activated protein kinase and PI3K/Akt pathways are major signalling networks linking EGFR activation to cell proliferation and survival (fig. 1) [23]. EGFR signalling pathway genes have been found to be mutated in NSCLC (and very rarely in other tumours). Depending on the geographical location, EGFR and KRAS mutations have been identified in ~10–30% of NSCLCs [27, 28]. EGFR mutations are independently associated with ADC histology, East Asian ethnicity, never-smoking status and female sex. Mutations of KRAS also target ADC histology, but otherwise differ from EGFR mutations because they are relatively rare in East Asians and occur more frequently in males and smokers [29]. Less commonly, somatic mutations have also been found in other EGFR pathway genes, including HER2 (~2%) [30], HER4 (~2%) [31], BRAF (~2%) [32] and PIK3CA (~4%) [33, 34]. The mutations target critical regions of the TK domain associated with downstream signalling (exons 18–21) and are of several types, including deletions, insertions and activating point mutations. However, two major types account for ~85% of mutations: deletions in exon 19 and point mutation L858R in exon 21.
FIGURE 1.
Epidermal growth factor receptor (EGFR) pathway. Ligands, such as epidermal growth factor (EGF), transforming growth factor (TGF)-α, or others, bind to the homo- and heterodimer kinase domain (TK), resulting in activation and receptor transphosphorylation. This creates docking sites for the adaptor proteins, Grb2 and Sos, which recruit Ras and phosphatidylinositol 3-kinase (PI3K), leading to the formation of two major signalling pathway branches, Ras/MAPK and PI3K/Akt. These networks result in, amongst others, proliferation, evasion of apoptosis and angiogenesis. MAPK: mitogen-activated kinase-like protein.
As a consequence of the frequent deregulation of EGFR pathway genes in NSCLC, EGFR became one of the first rationally selected molecules for targeted therapy. While initial targeted approaches utilised monoclonal antibodies, which block the ligand–receptor interaction, newer approaches have utilised small molecule reversible TK inhibitors (TKIs). The TK activity of EGFR is required for the biochemical responses induced by this receptor [23, 35, 36]. Two TKIs, gefitinib (Iressa®; AstraZeneca, London, UK) and erlotinib (Tarceva®; Roche, Basel, Switzerland) have been widely used in the treatment of advanced or recurrent NSCLC. Responses were noted in subsets, notably East Asian ethnicity, female sex, never-smoking status and ADC histology [37–39]. Subsequently, EGFR mutations in the TK domain were found to predict response to TKI in the same subset of patients [40–42]. According to a meta-analysis of 1,170 patients, >70% of NSCLCs with EGFR mutations responded to TKIs, whereas 10% of tumours without EGFR mutation responded [43]. However, not all activating mutations are associated with response to TKIs, and a point mutation T790M is associated with secondary resistance [44]. In addition, insertion mutations in exon 20 are also associated with primary resistance [45, 46]. Further studies indicated that factors other than EGFR mutations may play a role in determining response and survival after TKI therapy. EGFR gene copy number gain was associated with significantly improved TKI sensitivity and survival in a large unselected study with appropriate controls [47, 48]. In addition, other members of the EGFR family, i.e. HER2 [49] and EGFR3 [50] may be important factors involved in TKI sensitivity. A further complexity is the clinical observation that somatic mutations of KRAS confer intrinsic resistance to TKIs [51].
While mutations target ADC histology, upregulation of protein is often present in squamous carcinomas. Other mechanisms of upregulation include autocrine loops resulting from ligand production by tumour cells [52, 53], and of sheddase proteins involved in ligand release from the cell surface [54]. Several different approaches have demonstrated that mutations are an early feature during multistage pathogenesis, exhibiting a limited field effect surrounding mutation positive tumours, while increased copy number is a relatively late event associated with the tumour phenotype or with metastases [55].
Mutations in other EGFR signalling pathway genes
The complex EGFR signalling pathway consists of a large number of interacting genes and subpathways (fig. 1). The downstream KRAS gene, encoding a small guanosine-5′-triphosphate-binding protein, is one of the well-documented oncogenes, and is frequently activated by missense mutations in many human cancers, making it the most frequent oncogene known to be activated in human cancers. KRAS mutations are detected in ~20% of NSCLCs, especially in ADC and in smokers. Several studies that analysed both KRAS and EGFR mutation status in the same tumours indicate that EGFR and KRAS mutations are mutually exclusive [27]. KRAS binds to BRAF, and thus both genes are part of the EGFR family signalling cascade. However, BRAF mutations are rarely detected (0–3%) in lung cancer in comparison with KRAS mutations [56, 57]. BRAF is a nonreceptor serine/threonine kinase, but its kinase domain has a structure similar to other protein kinases, including EGFR members. BRAF mutations are also located in the P-loop or A-loop, as are some of the EGFR mutations. The V600 mutation in the A-loop is the most frequent type of BRAF mutation in human cancers. It is of interest that mutations of RET, Ras and BRAF are mutually exclusive in thyroid papillary cancer and lung cancer, as are KRAS and BRAF in colorectal cancers. These results indicate that simultaneous mutations of multiple genes in the same signalling pathways are not required for lung cancer pathogenesis, as well as for other types of cancer, and a single mutation in any of the four genes may suffice. HER2 (ERBB2) is one of the EGFR family gene members and, while it is occasionally amplified in NSCLC, mutations occur in a small proportion of cases [30]. The finding that EGFR and HER2 gene mutations target never-smokers, while KRAS mutations favour smokers, is further evidence that ADCs in smokers and never-smokers arise via different pathogenic pathways.
PI3K
PI3Ks are heterodimeric lipid kinases composed of catalytic and regulatory subunits. The regulatory subunit p85a is the only PI3K molecule found to have somatic mutations in human cancers; these occur predominantly in helical or kinase domains of its catalytic subunit encoded by the phosphoinositide-3-kinase, catalytic, alpha polypeptide (PIK3CA) gene. Mutations of PIK3CA occur in many human epithelial cancers, resulting in PIK3CA being one of the two most commonly mutated oncogenes (along with KRAS) identified in human cancers [58]. However, individual types of epithelial cancers show great variability in their mutational rates, with high rates present in glioblastomas, and gastric, hepatocellular and breast cancers, whereas the rates described in NSCLC are relatively low. In addition to mutations, increased chromosomal copy number (by amplification or polysomy) is another method of oncogene activation. A region of chromosome 3q (3q25–27), where PIK3CA (3q26) is located, is frequently amplified in lung cancers, especially SCCs [59]. However, the relationship between mutations and amplification of PIK3CA has not been studied comprehensively. Also, the functional effects of mutant or amplified PIK3CA in lung cancers are still unclear. The present authors analysed the mutational status of exons 9 and 20 and gene copy number of PIK3CA using 86 NSCLC cell lines, 43 SCLC cell lines, three extrapulmonary small cell cancer cell lines and 691 resected NSCLC tumours, and studied the relationship between PIK3CA alterations and mutational status of EGFR signalling pathway genes (EGFR, KRAS, HER2 and BRAF). PIK3CA expression and activity was also determined, and the findings correlated with effects on cell growth. Mutations were identified in 4.7% of NSCLC cell lines and 1.6% of tumours of all major histological types. PIK3CA copy number gains were more frequent in SCC (33.1%) than in adenocarcinoma (6.2%) or SCLC lines (4.7%). Thus, deregulation of the PI3K pathway is one of the few known molecular changes recognised to be more frequent in SCCs than in adenocarcinomas. PIK3CA mutations or gains are present in a subset of lung cancers and are of functional importance.
Anaplastic lymphoma kinase fusion proteins
A recurrent gene fusion between echinoderm microtubule-associated protein-like 4 (EML4; and, occasionally, of other fusion partners) and the anaplastic lymphoma kinase (ALK) gene occurs in ~7% of NSCLCs [60–62], resulting in activation of a potent ALK fusion protein. ALK fusion protein is usually found in never-smoker subjects. Although relatively rare, the relative paucity of fusion proteins known to contribute to lung cancer pathogenesis makes this a finding of biological interest. Although present understanding of the ALK fusion protein is limited, it may play a role in activating RAS [61]. Thus it is negatively associated with the presence of KRAS or EGFR mutations, and may favour ADC histology and never-smoker status.
Thyroid transcription factor 1 (TITF1)
Thyroid transcription factor 1 (TITF1; also known as NKX2-1) is a master transcription factor essential for the development of the peripheral airways [63], and is a lineage-specific marker for tumours developing from the terminal respiratory unit, i.e. peripheral ADCs [64]. It is frequently overexpressed and occasionally amplified in these tumours [6, 65]. Inhibition of TITF1 by RNA interference induced growth inhibition and apoptosis in a subset of lung ADC cell lines expressing TTF1 (the protein product of TITF1); sustaining TTF1 expression is crucial for TTF1-expressing ADC [64]. As most EGFR mutant ADCs arise from the terminal respiratory unit, they strongly express TITF1 [10]. In adult tissues, TITF1 has a very limited distribution, in only peripheral airway and thyroid epithelial cells. However, it is also expressed in the fetal forebrain, and perhaps that is the reason why it is also expressed in SCLCs.
MYC family
The MYC gene family encodes nuclear phospho-proteins (C-MYC, N-MYC, L-MYC) that control cellular growth and apoptosis. MYC genes are amplified in 15–30% of SCLC and less frequently in NSCLC. L- and N-MYC amplification is specific for neuroendocrine lung tumours, including SCLC and large cell neuroendocrine carcinoma (LCNEC). More frequently than amplification, a high level of transcription leads to overexpression of MYC proteins [66, 67].
ABNORMALITIES IN TUMOUR SUPPRESSOR GENE PATHWAYS
The p53 pathway
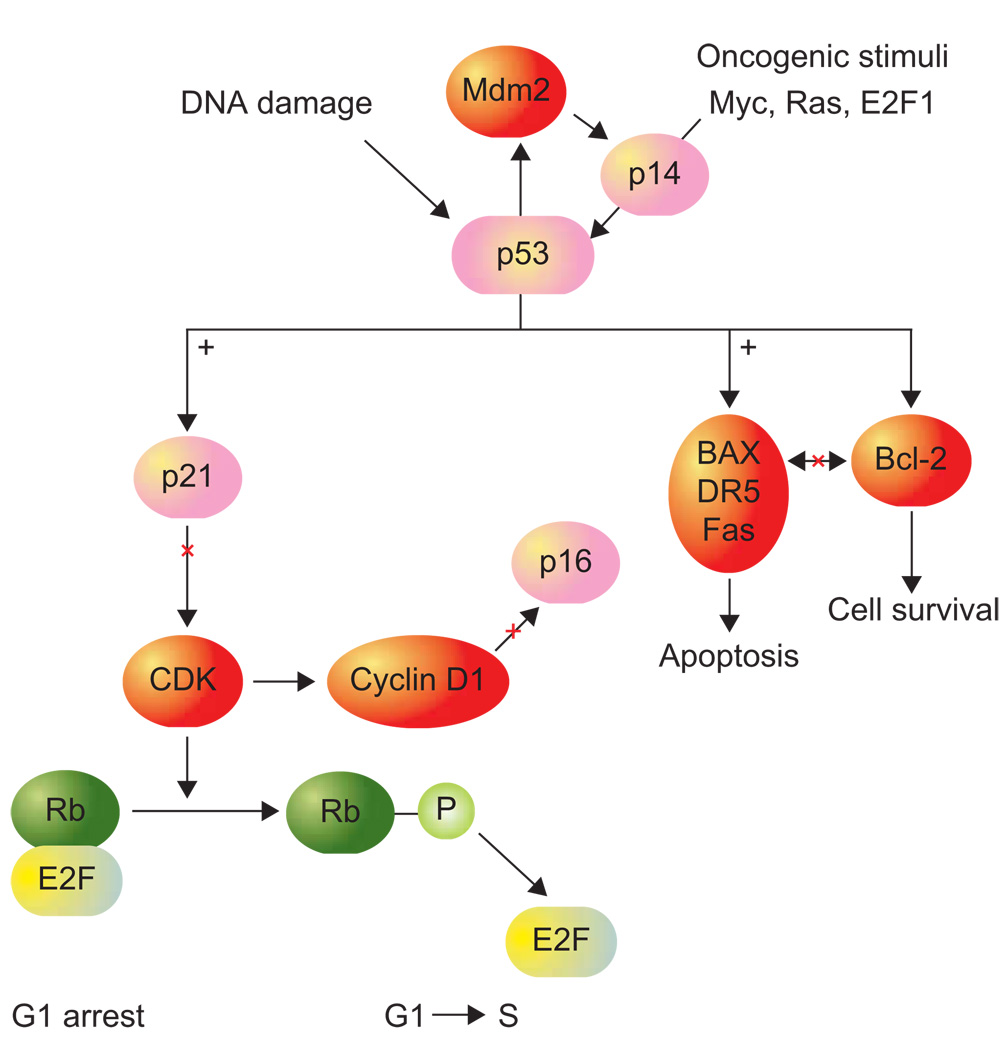
The p53 pathway includes several genes that belong to multiple upstream and downstream subpathways (fig. 2).
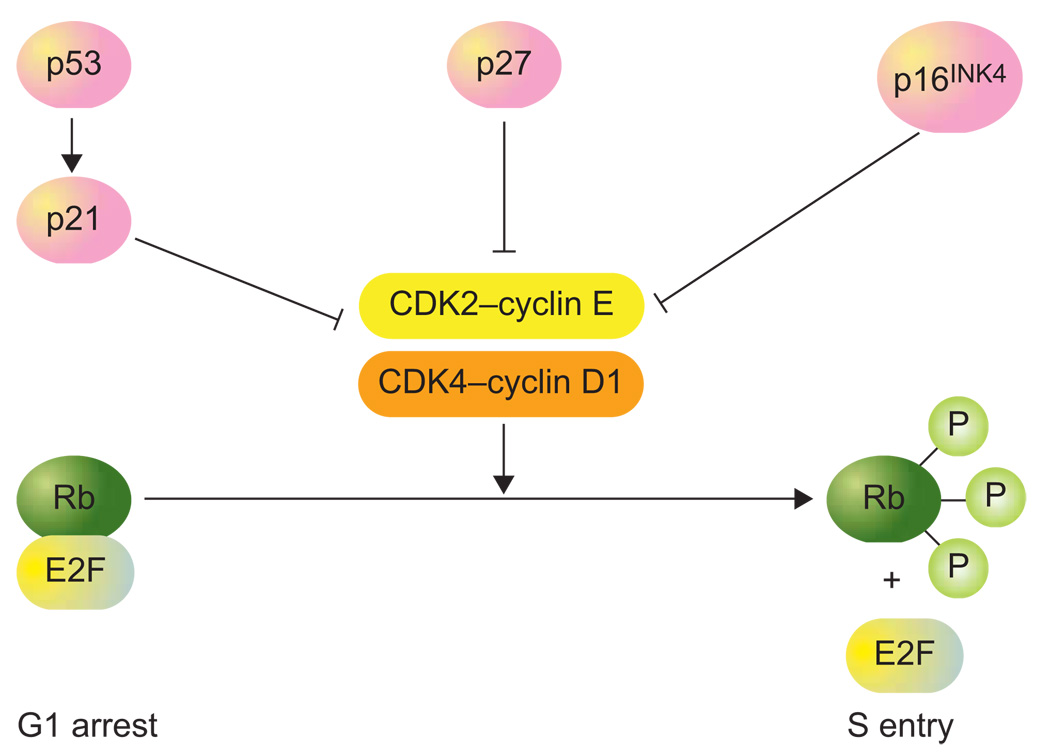
FIGURE 2.
The retinoblastoma gene product (Rb) pathway. Rb is the main downstream effector of p53 in the control of G1 arrest. This Rb function depends on the level of phosphorylation of Rb, which is achieved by cyclin-dependent kinases (CDK) 2 and 4 in complex with either cyclin E or cyclin D1. These kinases complexes are retro-controlled by the following CDK inhibitors: p21 (the transcriptional target of p53), p16 (INK4β) and p27 (kip1). Phosphorylated Rb releases E2F1 from binding to Rb, which allows E2F1 transcriptional activities on S-phases genes target and disrupt the G1 checkpoint. Loss of functional CDK inhibitors p53, activation/gain of cyclin D1 or cyclin E, and Rb loss all result in E2F1 activation and disruption of the G1 checkpoint.
p53 is the cellular gatekeeper, guarding against genetic instability and abnormality. It functions as a sensor of multiple stress signals, including DNA damage, oncogene activation and hypoxia. This transcription factor has downstream target genes involving cell cycle arrests (G1 and G2), DNA repair or apoptosis, and upstream regulatory genes, including p14 and Mdm2. p53 is the most frequently mutated gene in lung cancer [68]. Inactivating mutations in the DNA binding domain are displayed in 90% of SCLC and LCNEC and 50% of NSCLC, of which gain-of-function mutations prevent the p53 protein binding to Mdm2 and subsequent p53 ubiquitin-dependent proteolysis. The most frequent mutations are responsible for p53 protein stabilisation and are recognised by a simple immunohistochemical test; wild-type protein is not detectable by immunohistochemistry because of its very short half-life of 7 min. The mutation spectrum of p53 is tightly linked to carcinogen exposure, particularly smoking, which is related to GC to TA (G–T) transversions at CpG sites. Benzo[a]pyrene adducts preferentially induce mutation at guanine in codons 157, 248, 273 and 157; these are the fingerprints of tobacco carcinogenesis. In contrast, GC to TA (G–A) transition at non-CpG sites are associated with lung cancer in never-smokers. p53 alterations and stabilisation by mutation are frequent in proximal pre-invasive lesions of squamous dysplasia type and carcinoma in situ [69, 70].
There are two important upstream regulators of p53, Mdm2 and p14ARF, which belong to the upstream p53 regulator subpathway, and which suffer abnormal functions alternative to p53. p14ARF is now considered to be a master tumour suppressor gene responding to both oncogenic stimuli (Ras, MYC, E2F1) and DNA damage. p14ARF is encoded at the 9p21 locus of p16INK4 from an alternative exon 1β. p14ARF activation induces G1 arrest and apoptosis, either dependently or independently of p53 [71, 72]. p14ARF loss of protein expression, through as yet unknown mechanisms, occurs frequently in SCLC, LCNEC and some ADC [73]. As p14ARF acts in sequestrating Mdm2 in the nucleoli, thus allowing p53 to generate its transcriptional functions, the overexpression of Mdm2 is a second phenomenon upstream to p53, which is responsible for functional p53 inactivation in triggering the cytoplasmic shuttling of p53 and subsequent ubiquitin-dependent proteasomic degradation of wild-type p53. Mdm2 amplification is rare (~6% of NSCLC), although overexpression at the level of mRNA and protein is frequent, occurring in 30% of both SCLC and NSCLC [71].
Ataxia telangiectasia mutated (ATM), another gene upstream of the p53/p14ARF pathway, mediates the response to DNA damage. It is known to be mutant in ataxia telangectasia disease, characterised by a lack of DNA repair, but is not known as a mutant in lung cancer. A recent DNA sequencing of 623 genes in 188 ADCs [5] showed ATM to be mutant in 14 (7.4%), thus complementing the strong targeting of p53 pathway functions in lung cancer.
The downstream p53 pathway (fig. 2) includes target genes of p53 transcription, which play key roles in the mitochondrial apoptotic pathway, as well as in the death receptor pathway: Bcl-2 (anti-apoptotic) and Bax (pro-apoptotic) are up- and downregulated by p53, respectively; Fas and the tumour necrosis factor receptor-like apoptosis inducing ligand (TRAIL) receptor DR5 (TRAIL-death receptor 5) belong to the tumour necrosis factor receptor family. These four factors are strongly deregulated in lung cancer, which results in strong resistance to both mitochondrial and death receptor-induced apoptosis.
The p16INK4/cyclin D1/Rb pathway
The Rb gene was the first tumour suppressor gene to be recognised (fig. 2) [74], and is the downstream effector of p53-mediated G1 arrest through activation of the cyclin-dependent kinase (CDK) inhibitor p21. Rb function on the G1 check-point is tightly linked to Rb phosphorylation status, whereas hypophosphorylated Rb binds E2F1 transcription factor to maintain a cell cycle arrest in G0–G1. Rb inactivation also occurs via Rb phosphorylation. Phosphorylation of Rb achieved by CDK4–6, cyclin D and CDK2-cyclin E allows the release of the transcription factor E2F1, leading to G1–S transition. Thus, both the lack of Rb protein, the most frequent mechanism of escape from G1 check-point in SCLC, or the hyperphosphorylation of Rb frequent in NSCLC, disrupt the G1 checkpoint control. Loss of Rb protein occurs in >70% and >90% of high-grade neuroendocrine LCNEC and SCLC tumours, respectively, and in only 15% of NSCLC. A wide analysis of DNA sequences in ADC also identified RB1 mutation in some cases [5], pointing to the persistent negative selection for Rb functions in lung cancer (loss, phosphorylation and mutation) in addition to loss of heterozygosity (LOH) at 13q14 (allelic loss) [6, 75].
Inactivation of Rb functions by phosphorylation in NSCLC is mainly achieved by the loss of p16 CDK expression and/or overexpression of cyclins D1 and E (fig. 3). CDK4 is rarely overexpressed and is amplified in a small subset of NSCLC. In contrast, cyclin D1 overexpression and p16 loss occur in 40–50% of NSCLC, as assessed by immunohistochemistry. p16 loss of expression is the consequence of p16 methylation in 40%, p16 homozygous deletion in 30% and mutation in 10% of losses of expression [76]. Cyclin D1 is rarely amplified in lung cancer; however, a small percentage of amplification of CCD1 (cyclin D1 gene) was recently found in a wide genomic characterisation of the lung ADC [6]. Overexpression of CCD1 is observed in 35–50% of NSCLC and both CCD1 overexpression and p16 loss are early phenomena, and occur as soon as pre-invasive lesion appears, with an increasing level of grade of squamous dysplasia [70, 77]. p16INK4 is never lost in the absence of Rb, which suggests that retinoblastoma gene product (RB) and p16 are assuming the same function devoted to Rb phosphorylation in a unique pathway. Cyclin D1 (CCND1) and cyclin E (CCNE2) genes were found among the top focal regions of amplification in lung ADC [6]. p16 loss of allele (LOH) at 9p21 locus (CDKN2A/CDKN2B) is very frequent [6], weakening the p16 functions in addition to methylation. An inverse relationship between cyclin D1 overexpression and Rb loss also shows that cyclin D1 and p16INK4 are the only actors of RB phosphorylation and have no role when RB is lost. This is the case in SCLC, where RB is mostly lost, but p16INK4 or cyclin D1 alterations are rare. In contrast, cyclin E may be overexpressed (30% of NSCLC specially SCC) in the absence of Rb, because of the cyclin E response to DNA damage and genetic instability. Cyclin E overexpression is an early phenomenon in lung cancer bronchial pre-neoplasia [70].
FIGURE 3.
The p53 pathway. p53 is a sensor of cell stress, such as DNA damage and oncogenic stimuli, and functions as a transcription factor. Its target genes play roles in the control of the G1 arrest pathway (retinoblastoma gene product (Rb)/cyclin-dependent kinase (CDK) inhibitor/E2F1), susceptibility to apoptosis (Bax/Bcl-2), and control of the tumour necrosis factor receptor-like apoptosis inducing ligand (TRAIL) receptor 5 (DR5), Fas. It also enters into a DNA repair protein complex with proliferation cell nuclear antigen (PCNA). Mdm2 is an upstream regulator of p53, which governs its cytoplasmic shuttling protein, ubiquitin, ligation and degradation, and p14ARF, which sequesters Mdm2 in the nucleoli, thus allowing p53 transcriptional activity.
The serine/threonine kinase 11 gene
Germline mutations in serine/threonine kinase 11 (STK11), also called LKB1, located on the short arm of chromosome 19, are associated with the Peutz–Jeghers syndrome, which is characterised by intestinal hamartomas and an increased incidence of epithelial cancers. Although uncommon in most sporadic cancers, inactivating somatic mutations of STK11 occur in primary human lung ADCs and a smaller percentage of SCC. STK11 is a critical barrier to pulmonary tumorigenesis, controlling initiation, differentiation of cell polarity and metastasis [78]. Mutations are more frequent in ADCs arising in smokers and non-Asian populations, and are usually found in association with KRAS mutations [79, 80].
EVASION OF APOPTOSIS
Mitochondrial apoptosis (Bax/Bcl-2)
Evading apoptosis (programmed cell death) constitutes a major mechanism of tumour growth in addition to intrinsic proliferation. Bcl-2 (anti-apoptotic) and Bax (pro-apoptotic) are key factors of mitochondrial apoptosis in controlling the mitochondrial outer membrane permeabilisation, which leads to release of cytochrome C, the point of no return in the cell’s commitment to apoptosis. Anti-apoptotic Bcl-2 blocks channel formation by BAX [81]. The survival function of Bcl-2 is linked to its selective binding of the BH3 domain from pro-apoptotic proteins, particularly to its ability to form dimers with BAX, which depends on the relative amounts of the two proteins in tumour cell cytoplasm.
Bcl-2 is overexpressed in most SCLC and LCNEC and in a minority of NSCLC [69, 82]. In contrast to Bcl-2, Bax, which heterodimerises with Bcl-2 to control the level of apoptotic susceptibility, is downregulated in SCLC and upregulated in NSCLC, resulting in a ratio of Bcl-2:Bax of >1 in 95% of SCLC and 25% of NSCLC prone to resistance to apoptosis [82]. This ratio is reversed in favour of Bcl-2 early on in tumour progression, as soon as minor dysplasia occurs [69], suggesting an early escape of apoptosis during the pre-neoplastic process and its requirement to clonal selection against apoptosis.
Observation of a high level of the anti-apoptotic Bcl-2 in SCLC is striking in consideration of their exquisite chemosensitivity. Conversion of Bcl-2 to its inactive phosphorylated form or to Bax-like forms have been advocated [83], as well as alternative functions of Bcl-2 in cell cycle checkpoints downstream of DNA damage.
These apoptotic factors can be targeted by inhibitors of Bcl-2/Bcl-XL, such as ABT-737 and Bcl-2 antisense oligonucleotides [84, 85]. These compounds have shown efficacy in xenograft models of SCLC, as well as in NSCLC cell lines.
Death receptor deregulation
On binding to its ligand, FasL, the death receptor Fas activates a signalling pathway leading to apoptosis via caspase-8 activation, bridging the mitochondrial apoptotic pathway at the level of caspase-8. The Fas receptor (CD95) is down-regulated in the majority (70%) of NSCLC, as is its ligand FasL. In contrast, SCLC disclose a particular phenotype with low or null expression of Fas and a high expression of FasL (in 50%), suggesting a resistance to apoptosis by disruption of the Fas receptor pathway, but also to escape immune surveillance. Indeed, tumour FasL may engage Fas on T cytotoxic CD8 lymphocyte to induce a tumour-driven apoptosis [86].
E2F1 plays a critical role in cell cycle progression at G1–S transition, and belongs to the p53-Rb pathway. A differential expression has been shown between high-grade neuroendocrine tumours (SCLC and LCNEC) expressing very high levels and NSCLC with a low-to-undetectable level [87]. However, it is also recognised as an apoptotic factor. Its role in apoptosis was demonstrated to be Myc-induced, and either p53-dependent or -independent. E2F1 leads to apoptosis by affecting the alternative splicing of Flip (an inhibitor of the death receptor pathway Fas) towards downregulation of Flip-s (Flip short) [88]. Moreover E2F1 is now considered as a splicing organiser for several genes of the apoptotic pathway, such as BclX (L versus S), and caspases 8 and 9 [89]. The low level of E2F1 in NSCLC may increase cell survival, whereas its extremely high level of expression in SCLC is expected to enhance proliferation [87].
Cell immortalisation and telomerase activation
Telomeres are repetitive sequences located at the end of eukaryotic chromosomes composed of TTAGGG repeats that represent critical structures for chromosome length stabilisation, preventing them from end-to-end fusion and exonuclease excision. Telomeres shorten after each cell division, limiting the life span of cells [90]. Critical shortening of telomeres limits cell proliferation and induces apoptosis or cellular senescence, since short telomeres are perceived as damaged DNA leading to p53/ATM pathway activation. In tumour cells, this so-called mortality stage I (M1) crisis of cellular senescence is generally rescued by p53/Rb pathway inactivation, such as P16INK4 inactivation and p14ARF inactivation. DNA damage responses, which include p14ARF activation, ATM, p53, H2AX and CHK2 phosphorylation, as well as p53 stabilisation, are frequently impaired at an early stage of carcinogenesis in pre-neoplastic lesions, which escape from DNA damage by telomere shortening [91–93]. Telomerase is then re-expressed in tumour cells lacking p53- and Rb-mediated checkpoints, which have escaped M1 and have proliferated to mortality stage II (M2), a mortality crisis that selects tumour cells with huge genetic instability and telomerase reactivation. Telomerase is an RNA protein complex responsible for telomere repeat synthesis. It is composed of telomerase (hTERT), a protein catalytic subunit of telomerase hTERT, which represents the limiting factor for telomerase activity, and the RNA template of telomere repeat sequence. Upregulation of telomerase is thought to contribute to the early immortalisation steps of tumorigenesis. In pulmonary ADC precursor, hTERT overexpression is observed mainly in high-grade atypical alveolar hyperplasia (77%) and nonmucinous bronchioloalveolar carcinoma (97%) [94]. In preinvasive bronchial lesions, hTERT/mRNA and/or protein expression significantly increase along with the severity of their grade [95]. At least 80% of NSCLCs and nearly 100% of SCLCs have detectable or high levels of telomerase [96, 97]. Novel antagonist telomerase compounds targeting the RNA template region of hTR (human telomerase RNA) inhibit independent growth and in vivo xenograft tumour growth in lung cancer cells [98], providing the basis for lung cancer treatment.
EPIGENETIC CHANGES IN LUNG CANCER
Epigenetic modifications refer to a number of molecular mechanisms that regulate gene expression without changing the DNA sequence. These include the following: 1) alteration of the methylation status of DNA within CpG islands, with hypermethylation of CpG island promoters of tumour suppressor genes leading to their silencing; 2) covalent modification of histone tails; and 3) gene regulation by micro-RNA (miRNA).
DNA methylation and lung cancer
An excellent recent review article has summarised the role of DNA methylation in cancer [99]. Epigenetics may be defined as heritable changes in gene expression that are not due to any alteration in the DNA sequence. The best-known epigenetic marker is DNA methylation, perhaps because of the ease with which it can be studied. DNA methylation occurs as one part of a complex chromatin network that is influenced by modifications in histone structure. Methylation is a normal physiological function. While early embryonic cells lack methylation (as it is not transmitted via the germline), methylation is essential for the development and regulation of gene expression. In postnatal life, it controls expression of oncofetal genes, imprinted genes and tissue-specific gene expression. Three forms of abnormal methylation may play roles in tumour pathogenesis, including global hypomethylation, hypermethylation of tumour-suppressor genes and the recent finding that methylation may regulate expression of some miRNAs. DNA methylation is restricted to cytosines that are upstream of guanines (CpG sites). In the human genome, the promoter (and sometimes the 5′ end) of ~50% of genes are rich in CpG sites (CpG islands). In expressed genes, CpG islands are usually unmethylated, while in other regions of the genome, most of the CpG sites are methylated. Loss of methylation at the latter sites (usually in noncoding regions of the genome) is common in tumours and leads to genomic instability. In contrast, methylation occurs at multiple CpG islands in tumours, resulting in loss of expression of tumour suppressor genes.
In lung cancer, many genes (perhaps hundreds) have been found to be silenced by promoter methylation [100], and include genes in almost all of the Hallmarks of Cancer categories [101]. The most well-studied genes include RARB, CDKN2A, TIMP3, MGMT, DAPK, CDH1, CDH13 and RASSF1A [102]. Methylation begins early during lung cancer pathogenesis [103], and its detection in the sputum of smokers with dysplasia may identify individuals who are at increased risk [104]. DNA methylation may predict for early recurrence in stage I NSCLC [105]. Restoration of expression of epigenetically silenced genes is a new targeted therapeutic approach, and histone deacetylase inhibitors are being investigated for the treatment of lung cancer.
Epigenetic modifications of histones: the histone code of lung cancer
Human cancers undergo a massive overall loss of DNA methylation, although they acquire specific patterns of hypermethylation of certain promoters. DNA methylation occurs in the context of other epigenetic modifications. Methyl-CpG binding proteins and DNA methyltransferase are associated with histone deacetylases and histone methyltransferases. The status of acetylation and methylation of specific lysine residues within the tail of nucleosomal core histones play a crucial role in regulating chromatin packaging, nuclear architecture, gene expression and genomic stability [106–111]. In cancer cells, including lung cancer, hypermethylation of promoter CpG islands of transcriptionally repressed tumour suppressor genes are associated with a particular combination of histone markers, such as deacetylation of histones H3 and H4, loss of histone H3 lysine 4 trimethylation, and gain of H3K9 and H3K27 trimethylation. The impact of histone code changes in lung cancer progression in tumorigenesis and prognosis has been shown by an epigenetic landscape of cancer cells that are profoundly distorted in appearance compared with normal candidate stem cells. Excessive acetylation of H4K5/H4K8 and loss of trimethylation of H4K20 was shown in NSCLC and pre-invasive bronchial dysplastic lesions. H4K20 loss of trimethylation was shown to identify a subpopulation of early stage (I) ADC with shorter survival [112]. In addition, histone H2 and H3 modifications in acetylation and trimethylation status were also detected in NSCLC and SCLC, allowing detection of subpopulations with differential prognosis, and suggesting that histone code epigenetic changes play an important role in lung cancer tumorigenesis [113]. Recent technologies using genome-wide, cancer epigenetics approaches showed that global alterations of histone modifications patterns are linked to DNA methylation and are causal in lung cancer [107].
miRNA in lung cancer
miRNAs are a class of small (~22 nucleotides) nonprotein-encoding RNA molecules that regulate gene expression by modulating the activity of specific messenger RNA targets via direct base-pairing interactions [114–116]. Many miRNAs have tissue-specific expression patterns (miRNA fingerprints), and miRNA expression is commonly dysregulated in a variety of cancers, including lung cancer [117–119]. miRNAs have been shown to be an important class of tissue-based biomarkers, and recent work shows that they are released into the bloodstream by tumour cells, giving them potential as blood-based markers. Nearly 500 human miRNAs have been described, and many more may remain to be discovered. It is of interest that miRNAs may function both as oncogenes and as tumour suppressor genes, and thus may be either up- or down-regulated in cancers. The gene target of only a minority of miRNAs is known with certainty, while several others have putative targets. However, miRNA genes are frequently located at fragile sites, as well as in minimal regions of loss of heterozygosity, minimal regions of amplification, or common breakpoint regions, indicating that they may play important roles in cancer pathogenesis [120]. Several programs exist for the alignment of miRNA expression and gene expression profiling. A unique miRNA molecular profile is characteristic of lung cancer and the miRNA signature of lung cancer differs from normal lung epithelial cells and in different tumour histology [118]. As an example, six miRNA are expressed differently in ADC versus epidermoid carcinoma. Using real-time analysis for precursor miRNA, miRNA expression profiles were correlated with survival of lung ADCs, including those classified as disease stage I, indicating that miRNA expression profiles are diagnostic and prognostic markers of lung cancer [118]. The let-7 family of miRNAs inhibit Ras protein expression [121], which is mutated and overactive in many smoker-related ADCs. Let-7 shows a decreased expression in lung cancer as compared with surrounding normal lung tissue. Two species of Let-7 (Let-7a-1 and Let-7f-1) define two clusters of expression with low levels of expression correlating with shorter survival [117]. Microarray expression has shown that in regulating proliferation, Let-7 expression regulates cell cycle gene expression, such as cyclin E, E2F1, SKP2 and MCM, and cellular division, by regulating aurora A and B, and also regulates response-DNA damage response genes (BRCA1-2, RRM1-2, CHK1, HMGA2). As RAS mutations are rarely found in never-smoker tumours, expression of the let-7 family is predicted to show differences between smoker and never-smoker tumours. miRNAs are connected to the oncogenic pathway of Myc and E2F1 [122]: the cluster miR-17-92, contained in an amplicon at 13q31, is overexpressed in lung cancer and, typically, in SCLC. Finally, miR-34 reproduces almost all functions of p53 [123], thereby completing the puzzle of the p53 network. Indeed, miR-34 recapitulates the main p53 activities towards cell cycle arrest and promotion of apoptosis. Deletions of miR-34 family miRNAs are reported in human cancer, as miR-34a is located within chromosome 1p36, a frequent region of heterozygous deletion. Minimal deletions and reduced expressions containing miR-34 are found in lung cancer and in lung cancer cell lines [120, 124]. The placement of several miRNA into nononcogenic and tumour suppressor networks begins to solve the long-standing mysteries of how the circuitries of these pathways are wired.
Maturation enzymes of miRNA, such as DICER, are necessary for the bronchial branching in lung development [125]. DICER expression decreases in a pre-invasive lesion from atypical alveolar hyperplasia to ADC via bronchioloalveolar carcinoma [126]. Interestingly, the level of DICER is predictive of survival, with a low DICER level in ADC leading to shorter survival time.
Mitochondrial mutations
Somatic mitochondrial DNA (mtDNA) mutations have been increasingly observed in primary human cancers [127, 128]. As each cell contains many mitochondria with multiple copies of mtDNA, it is possible that wild-type and mutant mtDNA can co-exist in a state called heteroplasmy. During cell division, mitochondria are randomly distributed to daughter cells. Over time, the proportion of the mutant mtDNA within the cell can vary and may drift toward predominantly mutant or wild-type, in order to achieve homoplasmy. Thus, the biological impact of a given mutation may vary, depending on the proportion of mutant mtDNAs carried by the cell. Most mutations occur in the coding sequences, but few result in substantial amino acid changes, raising questions as to their biological consequence. Studies reveal that mtDNA plays a crucial role in the development of cancer, and recent work has established the functional significance of specific mitochondrial mutations in cancer and disease progression [129]. mtDNA mutations occur early during pre-neoplasia [130], and have great potential as cancer biomarkers. D-loop alterations are frequent in lung cancers and their cell lines, and these changes are weakly associated with certain clinical parameters [131].
Lung cancer in never-smokers: a different disease
While smoking is the major environmental and lifestyle cause of most lung cancers, ~25% of lung cancer cases worldwide are not attributable to tobacco smoking [2], resulting in lung cancer in never-smokers being the seventh leading cause of cancer deaths in the world. Lung cancer in never-smokers demonstrates a marked sex bias worldwide, occurring more frequently among females, and especially in Asiatic countries. Although smoking-related carcinogens act on both proximal and distal airways, inducing all the major forms of lung cancer, cancers arising in never-smokers target the distal airways and favour ADC histology. While the conventional thought is that lung cancer in never-smokers is due to environmental tobacco smoke, this is a relatively weak carcinogen and can only account for a minority of lung cancers arising in never-smokers. The cause of lung cancer in never-smokers remains controversial, but no conclusive cause for most cases has been identified. Molecular epidemiology studies, in particular of the TP53, KRAS and EGFR genes, demonstrate strikingly different mutation patterns and frequencies between lung cancers in never-smokers and smokers. In addition, there are major clinical differences between lung cancers arising in never-smokers and smokers, and their response to targeted therapies. These facts strongly suggest that lung cancer arising in never-smokers is a disease distinct from the more common tobacco-related forms of lung cancer. Clearly, further efforts are needed to identify the major causes of lung cancers arising in never-smokers and the reasons for its marked pathological, geographical and sex differences.
Global approaches to the molecular study of lung cancer
The availability of the human genome sequence in 2001 has led to multiple approaches to the identification of recurrent changes in tumours. These global approaches include mutational changes, gene expression profiling, copy number changes (by comparative genomic hybridisation or single nucleotide polymorphism analyses), hypermethylation of CpG islands, miRNA profiling and mitochondrial mutations. Over 20 gene expression profiling studies in lung cancer have been reported, and, due to its pathological and molecular heterogeneity, most have focused on ADCs. Several studies have identified prognostic subsets of ADC [132]. In addition, although the total number of never-smoker cancers analysed to date is modest, subsets also relate to the degree of smoke exposure [133–135]. Initial studies identified four subsets. However, on identification and exclusion of LCNECs (which are often misclassified as ADCs), three major subtypes are identified by expression profiling [134, 135]. In addition, the major driving mutations, EGFR and KRAS, are associated with specific expression profiles and histolological subtypes. Global gene mutational profiles (achieved by sequencing the whole or part of the genome) have identified recurrent nonsystemic mutations in many putative oncogenes and tumour suppressor genes [5]. Similarly, comparative genomic hybridisation and single nucleotide polymorphism studies have led to the identification of several sites of recurrent amplicons in human tumours, including lung cancers, and have resulted in the identification of putative oncogenes, such as the lineage-specific TITF1 gene [6, 65, 136]. Integrated approaches to whole genome analyses are likely to be of greater benefit than individual platforms, and have already led to the identification of cancer-related abnormalities in signalling pathways [5].
Another genome-wide approach is proteomics. Proteomics represents the final stage of genomics, and thus may be more directly relevant than analyses of DNA or RNA. The difficulties of finding and identifying rare proteins in body fluids, which demonstrate a concentration gradient of several logs and consist of several thousand proteins, have hampered progress in the past. However, recent advances in technology, especially the application of mass spectrometry, have resulted in applications towards biomarkers for detection and prognosis [137–139].
Application of molecular biology to individualised therapy
The finding, >25 yrs ago, that the EGFR gene was overexpressed in many solid tumours ushered in the era of targeted therapy that focused on molecular changes either in specific tumour types or in subsets of tumours. Individualised therapy received an enormous boost with the success of EGFR TKIs in selective subsets of NSCLC. Recent insights into the molecular pathogenesis and biological behaviour of lung cancer have led to the development of rationally designed methods of early detection, prevention, and treatment of this disease [2, 140, 141]. While targeting signalling pathways and angiogenesis have received most of the attention, all of the hallmarks of cancer have been investigated. In fact, the plethora of possible new drugs makes recruitment to some large clinical trials difficult. While several agents have shown promise and are undergoing phase III clinical trials, issues regarding dosage, duration of therapy, combination with conventional therapy, and combinations with other targeted therapies offer many challenges that will take many years to solve. Clinical trials that use molecular profiling to determine individualised therapy have been initiated [80].
Acknowledgments
SUPPORT STATEMENT
This work and authors were supported by INSERM (Paris, France), INCa, PNES-INCa (Programme National d’Excellence Cancers du Poumon 2006–2009; both Paris, France) (E. Brambilla) and a National Cancer Institute (Bethesda, MD, USA) Lung Cancer Specialized Program of Research Excellence grant P50CA70907 (A. Gazdar).
Footnotes
STATEMENT OF INTEREST
A statement of interest for A. Gazdar can be found at www.erj.ersjournals.com/misc/statements.dtl
REFERENCES
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers–a different disease. Nat Rev Cancer. 2007;7:778–790. doi: 10.1038/nrc2190. [DOI] [PubMed] [Google Scholar]
- 3.Bach PB, Kelley MJ, Tate RC, et al. Screening for lung cancer: a review of the current literature. Chest. 2003;123 Suppl. 1:72S–82S. doi: 10.1378/chest.123.1_suppl.72s. [DOI] [PubMed] [Google Scholar]
- 4.Henschke CI, Yankelevitz DF, Libby DM, et al. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med. 2006;355:1763–1771. doi: 10.1056/NEJMoa060476. [DOI] [PubMed] [Google Scholar]
- 5.Ding L, Getz G, Wheeler DA, et al. Somatic mutations affect key pathways in lung adenocarcinoma. Nature. 2008;455:1069–1075. doi: 10.1038/nature07423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weir BA, Woo MS, Getz G, et al. Characterizing the cancer genome in lung adenocarcinoma. Nature. 2007;450:893–898. doi: 10.1038/nature06358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas RK, Baker AC, Debiasi RM, et al. High-throughput oncogene mutation profiling in human cancer. Nat Genet. 2007;39:347–351. doi: 10.1038/ng1975. [DOI] [PubMed] [Google Scholar]
- 8.Sekido Y, Fong KM, Minna JD. Molecular genetics of lung cancer. Annu Rev Med. 2003;54:73–87. doi: 10.1146/annurev.med.54.101601.152202. [DOI] [PubMed] [Google Scholar]
- 9.Wistuba II, Behrens C, Virmani AK, et al. High resolution chromosome 3p allelotyping of human lung cancer and preneoplastic/preinvasive bronchial epithelium reveals multiple, discontinuous sites of 3p allele loss and three regions of frequent breakpoints. Cancer Res. 2000;60:1949–1960. [PubMed] [Google Scholar]
- 10.Yatabe Y, Kosaka T, Takahashi T, et al. EGFR mutation is specific for terminal respiratory unit type adenocarcinoma. Am J Surg Pathol. 2005;29:633–639. doi: 10.1097/01.pas.0000157935.28066.35. [DOI] [PubMed] [Google Scholar]
- 11.Song P, Sekhon HS, Fu XW, et al. Activated cholinergic signaling provides a target in squamous cell lung carcinoma. Cancer Res. 2008;68:4693–4700. doi: 10.1158/0008-5472.CAN-08-0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein IB, Joe A. Oncogene addiction. Cancer Res. 2008;68:3077–3080. doi: 10.1158/0008-5472.CAN-07-3293. [DOI] [PubMed] [Google Scholar]
- 13.Hecht SS. Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst. 1999;91:1194–1210. doi: 10.1093/jnci/91.14.1194. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz AG, Prysak GM, Bock CH, et al. The molecular epidemiology of lung cancer. Carcinogenesis. 2007;28:507–518. doi: 10.1093/carcin/bgl253. [DOI] [PubMed] [Google Scholar]
- 15.Paz-Elizur T, Sevilya Z, Leitner-Dagan Y, et al. DNA repair of oxidative DNA damage in human carcinogenesis: potential application for cancer risk assessment and prevention. Cancer Lett. 2008;266:60–72. doi: 10.1016/j.canlet.2008.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou W, Liu G, Miller DP, et al. Polymorphisms in the DNA repair genes XRCC1 and ERCC2, smoking, and lung cancer risk. Cancer Epidemiol Biomarkers Prev. 2003;12:359–365. [PubMed] [Google Scholar]
- 17.Thorgeirsson TE, Geller F, Sulem P, et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452:638–642. doi: 10.1038/nature06846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hung RJ, McKay JD, Gaborieau V, et al. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature. 2008;452:633–637. doi: 10.1038/nature06885. [DOI] [PubMed] [Google Scholar]
- 19.Young RP, Hopkins RJ, Hay BA, et al. Lung cancer gene associated with COPD: triple whammy or possible confounding effect? Eur Respir J. 2008;32:1158–1164. doi: 10.1183/09031936.00093908. [DOI] [PubMed] [Google Scholar]
- 20.Amos CI, Xu W, Spitz MR. Is there a genetic basis for lung cancer susceptibility? Recent Results Cancer Res. 1999;151:3–12. doi: 10.1007/978-3-642-59945-3_1. [DOI] [PubMed] [Google Scholar]
- 21.Bailey-Wilson JE, Amos CI, Pinney SM, et al. A major lung cancer susceptibility locus maps to chromosome 6q23–25. Am J Hum Genet. 2004;75:460–474. doi: 10.1086/423857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson DR, Wu YM, Lin SF. The protein tyrosine kinase family of the human genome. Oncogene. 2000;19:5548–5557. doi: 10.1038/sj.onc.1203957. [DOI] [PubMed] [Google Scholar]
- 23.Sharma SV, Bell DW, Settleman J, et al. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer. 2007;7:169–181. doi: 10.1038/nrc2088. [DOI] [PubMed] [Google Scholar]
- 24.Rowinsky EK. The erbB family: targets for therapeutic development against cancer and therapeutic strategies using monoclonal antibodies and tyrosine kinase inhibitors. Annu Rev Med. 2004;55:433–457. doi: 10.1146/annurev.med.55.091902.104433. [DOI] [PubMed] [Google Scholar]
- 25.Hirsch FR, Varella-Garcia M, Bunn PA, Jr, et al. Epidermal growth factor receptor in non-small-cell lung carcinomas: correlation between gene copy number and protein expression and impact on prognosis. J Clin Oncol. 2003;21:3798–3807. doi: 10.1200/JCO.2003.11.069. [DOI] [PubMed] [Google Scholar]
- 26.Nicholson RI, Gee JM, Harper ME. EGFR and cancer prognosis. Eur J Cancer. 2001;37 Suppl. 4:S9–S15. doi: 10.1016/s0959-8049(01)00231-3. [DOI] [PubMed] [Google Scholar]
- 27.Shigematsu H, Gazdar AF. Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer. 2006;118:257–262. doi: 10.1002/ijc.21496. [DOI] [PubMed] [Google Scholar]
- 28.Eberhard DA, Johnson BE, Amler LC, et al. Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J Clin Oncol. 2005;23:5900–5909. doi: 10.1200/JCO.2005.02.857. [DOI] [PubMed] [Google Scholar]
- 29.Gazdar AF, Shigematsu H, Herz J, et al. Mutations and addiction to EGFR: the Achilles “heal” of lung cancers? Trends Mol Med. 2004;10:481–486. doi: 10.1016/j.molmed.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Shigematsu H, Takahashi T, Nomura M, et al. Somatic mutations of the HER2 kinase domain in lung adenocarcinomas. Cancer Res. 2005;65:1642–1646. doi: 10.1158/0008-5472.CAN-04-4235. [DOI] [PubMed] [Google Scholar]
- 31.Soung YH, Lee JW, Kim SY, et al. Somatic mutations of the ERBB4 kinase domain in human cancers. Int J Cancer. 2006;118:1426–1429. doi: 10.1002/ijc.21507. [DOI] [PubMed] [Google Scholar]
- 32.Naoki K, Chen TH, Richards WG, et al. Missense mutations of the BRAF gene in human lung adenocarcinoma. Cancer Res. 2002;62:7001–7003. [PubMed] [Google Scholar]
- 33.Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304:554. doi: 10.1126/science.1096502. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto H, Shigematsu H, Nomura M, et al. PIK3CA mutations and copy number gains in human lung cancers. Cancer Res. 2008;68:6913–6921. doi: 10.1158/0008-5472.CAN-07-5084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moon A. Differential functions of Ras for malignant phenotypic conversion. Arch Pharm Res. 2006;29:113–122. doi: 10.1007/BF02974271. [DOI] [PubMed] [Google Scholar]
- 36.Molina JR, Adjei AA. The Ras/Raf/MAPK pathway. J Thorac Oncol. 2006;1:7–9. [PubMed] [Google Scholar]
- 37.Fukuoka M, Yano S, Giaccone G, et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial) [corrected] J Clin Oncol. 2003;21:2237–2246. doi: 10.1200/JCO.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 38.Kris MG, Natale RB, Herbst RS, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA. 2003;290:2149–2158. doi: 10.1001/jama.290.16.2149. [DOI] [PubMed] [Google Scholar]
- 39.Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353:123–132. doi: 10.1056/NEJMoa050753. [DOI] [PubMed] [Google Scholar]
- 40.Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 41.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 42.Pao W, Miller V, Zakowski M, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci USA. 2004;101:13306–13311. doi: 10.1073/pnas.0405220101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Uramoto H, Mitsudomi T. Which biomarker predicts benefit from EGFR-TKI treatment for patients with lung cancer? Br J Cancer. 2007;96:857–863. doi: 10.1038/sj.bjc.6603665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- 45.Wu JY, Wu SG, Yang CH, et al. Lung cancer with epidermal growth factor receptor exon 20 mutations is associated with poor gefitinib treatment response. Clin Cancer Res. 2008;14:4877–4882. doi: 10.1158/1078-0432.CCR-07-5123. [DOI] [PubMed] [Google Scholar]
- 46.Shigematsu H, Lin L, Takahashi T, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;97:339–346. doi: 10.1093/jnci/dji055. [DOI] [PubMed] [Google Scholar]
- 47.Shepherd FA, Rosell R. Weighing tumor biology in treatment decisions for patients with non-small cell lung cancer. J Thorac Oncol. 2007;2 Suppl. 2:S68–S76. doi: 10.1097/01.JTO.0000269737.05962.a0. [DOI] [PubMed] [Google Scholar]
- 48.Zhu CQ, da Cunha Santos G, Ding K, et al. Role of KRAS and EGFR as biomarkers of response to erlotinib in National Cancer Institute of Canada Clinical Trials Group Study BR.21. J Clin Oncol. 2008;26:4268–4275. doi: 10.1200/JCO.2007.14.8924. [DOI] [PubMed] [Google Scholar]
- 49.Cappuzzo F, Varella-Garcia M, Shigematsu H, et al. Increased HER2 gene copy number is associated with response to gefitinib therapy in epidermal growth factor receptor-positive non-small-cell lung cancer patients. J Clin Oncol. 2005;23:5007–5018. doi: 10.1200/JCO.2005.09.111. [DOI] [PubMed] [Google Scholar]
- 50.Cappuzzo F, Toschi L, Domenichini I, et al. HER3 genomic gain and sensitivity to gefitinib in advanced non-small-cell lung cancer patients. Br J Cancer. 2005;93:1334–1340. doi: 10.1038/sj.bjc.6602865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pao W, Wang TY, Riely GJ, et al. KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med. 2005;2:e17. doi: 10.1371/journal.pmed.0020017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang J, Iwanaga K, Choi KC, et al. Intratumoral epiregulin is a marker of advanced disease in non-small cell lung cancer patients and confers invasive properties on EGFR-mutant cells. Cancer Prev Res. 2008;1:201–207. doi: 10.1158/1940-6207.CAPR-08-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yonesaka K, Zejnullahu K, Lindeman N, et al. Autocrine production of amphiregulin predicts sensitivity to both gefitinib and cetuximab in EGFR wild-type cancers. Clin Cancer Res. 2008;14:6963–6973. doi: 10.1158/1078-0432.CCR-08-0957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou BB, Peyton M, He B, et al. Targeting ADAM-mediated ligand cleavage to inhibit HER3 and EGFR pathways in non-small cell lung cancer. Cancer Cell. 2006;10:39–50. doi: 10.1016/j.ccr.2006.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gazdar AF, Minna JD. Deregulated EGFR signaling during lung cancer progression : mutations, amplicons, and autocrine loops. Cancer Prev Res. 2008;1:156–160. doi: 10.1158/1940-6207.CAPR-08-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ji H, Wang Z, Perera SA, et al. Mutations in BRAF and KRAS converge on activation of the mitogen-activated protein kinase pathway in lung cancer mouse models. Cancer Res. 2007;67:4933–4939. doi: 10.1158/0008-5472.CAN-06-4592. [DOI] [PubMed] [Google Scholar]
- 57.Dhomen N, Marais R. New insight into BRAF mutations in cancer. Curr Opin Genet Dev. 2007;17:31–39. doi: 10.1016/j.gde.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 58.Samuels Y, Diaz LA, Jr, Schmidt-Kittler O, et al. Mutant PIK3CA promotes cell growth and invasion of human cancer cells. Cancer Cell. 2005;7:561–573. doi: 10.1016/j.ccr.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 59.Garnis C, Lockwood WW, Vucic E, et al. High resolution analysis of non-small cell lung cancer cell lines by whole genome tiling path array CGH. Int J Cancer. 2006;118:1556–1564. doi: 10.1002/ijc.21491. [DOI] [PubMed] [Google Scholar]
- 60.Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J Thorac Oncol. 2008;3:13–17. doi: 10.1097/JTO.0b013e31815e8b60. [DOI] [PubMed] [Google Scholar]
- 61.Meyerson M. Cancer: broken genes in solid tumours. Nature. 2007;448:545–546. doi: 10.1038/448545a. [DOI] [PubMed] [Google Scholar]
- 62.Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–566. doi: 10.1038/nature05945. [DOI] [PubMed] [Google Scholar]
- 63.Maeda Y, Dave V, Whitsett JA. Transcriptional control of lung morphogenesis. Physiol Rev. 2007;87:219–244. doi: 10.1152/physrev.00028.2006. [DOI] [PubMed] [Google Scholar]
- 64.Tanaka H, Yanagisawa K, Shinjo K, et al. Lineage-specific dependency of lung adenocarcinomas on the lung development regulator TTF-1. Cancer Res. 2007;67:6007–6011. doi: 10.1158/0008-5472.CAN-06-4774. [DOI] [PubMed] [Google Scholar]
- 65.Lockwood WW, Chari R, Coe BP, et al. DNA amplification is a ubiquitous mechanism of oncogene activation in lung and other cancers. Oncogene. 2008;27:4615–4624. doi: 10.1038/onc.2008.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gazzeri S, Brambilla E, Caron de Fromentel C, et al. p53 genetic abnormalities and myc activation in human lung carcinoma. Int J Cancer. 1994;58:24–32. doi: 10.1002/ijc.2910580106. [DOI] [PubMed] [Google Scholar]
- 67.Gazzeri S, Brambilla E, Chauvin C, et al. Analysis of the activation of the myc family oncogene and of its stability over time in xenografted human lung carcinomas. Cancer Res. 1990;50:1566–1570. [PubMed] [Google Scholar]
- 68.Olivier M, Petitjean A, Marcel V, et al. Recent advances in p53 research: an interdisciplinary perspective. Cancer Gene Ther. 2009;16:1–12. doi: 10.1038/cgt.2008.69. [DOI] [PubMed] [Google Scholar]
- 69.Brambilla E, Gazzeri S, Lantuejoul S, et al. p53 mutant immunophenotype and deregulation of p53 transcription pathway (Bcl2, Bax, and Waf1) in precursor bronchial lesions of lung cancer. Clin Cancer Res. 1998;4:1609–1618. [PubMed] [Google Scholar]
- 70.Jeanmart M, Lantuejoul S, Fievet F, et al. Value of immunohistochemical markers in preinvasive bronchial lesions in risk assessment of lung cancer. Clin Cancer Res. 2003;9:2195–2203. [PubMed] [Google Scholar]
- 71.Eymin B, Gazzeri S, Brambilla C, et al. Mdm2 over-expression and p14ARF inactivation are two mutually exclusive events in primary human lung tumors. Oncogene. 2002;21:2750–2761. doi: 10.1038/sj.onc.1205359. [DOI] [PubMed] [Google Scholar]
- 72.Eymin B, Claverie P, Salon C, et al. p14ARF activates a Tip60-dependent and p53-independent ATM/ATR/CHK pathway in response to genotoxic stress. Mol Cell Biol. 2006;26:4339–4350. doi: 10.1128/MCB.02240-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gazzeri S, Della Valle V, Chaussade L, et al. The human p19ARF protein encoded by the beta transcript of the p16INK4a gene is frequently lost in small cell lung cancer. Cancer Res. 1998;58:3926–3931. [PubMed] [Google Scholar]
- 74.Knudson AG, Jr, Hethcote HW, Brown BW. Mutation and childhood cancer: a probabilistic model for the incidence of retinoblastoma. Proc Natl Acad Sci USA. 1975;72:5116–5120. doi: 10.1073/pnas.72.12.5116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gouyer V, Gazzeri S, Bolon I, et al. Mechanism of retinoblastoma gene inactivation in the spectrum of neuroendocrine lung tumors. Am J Respir Cell Mol Biol. 1998;18:188–196. doi: 10.1165/ajrcmb.18.2.3008. [DOI] [PubMed] [Google Scholar]
- 76.Brambilla E, Moro D, Gazzeri S, et al. Alterations of expression of Rb, p16(INK4A) and cyclin D1 in non-small cell lung carcinoma and their clinical significance. J Pathol. 1999;188:351–360. doi: 10.1002/(SICI)1096-9896(199908)188:4<351::AID-PATH385>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 77.Brambilla E, Gazzeri S, Moro D, et al. Alterations of Rb pathway (Rb-p16INK4-cyclin D1) in preinvasive bronchial lesions. Clin Cancer Res. 1999;5:243–250. [PubMed] [Google Scholar]
- 78.Ji H, Ramsey MR, Hayes DN, et al. LKB1 modulates lung cancer differentiation and metastasis. Nature. 2007;448:807–810. doi: 10.1038/nature06030. [DOI] [PubMed] [Google Scholar]
- 79.Matsumoto S, Iwakawa R, Takahashi K, et al. Prevalence and specificity of LKB1 genetic alterations in lung cancers. Oncogene. 2007;26:5911–5918. doi: 10.1038/sj.onc.1210418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Herbst RS, Heymach JV, Lippman SM. Molecular origins of lung cancer. N Engl J Med. 2008;359:1367–1380. doi: 10.1056/NEJMra0802714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Danial NN. BCL-2 family proteins: critical checkpoints of apoptotic cell death. Clin Cancer Res. 2007;13:7254–7263. doi: 10.1158/1078-0432.CCR-07-1598. [DOI] [PubMed] [Google Scholar]
- 82.Brambilla E, Negoescu A, Gazzeri S, et al. Apoptosis-related factors p53, Bcl2, and Bax in neuroendocrine lung tumors. Am J Pathol. 1996;149:1941–1952. [PMC free article] [PubMed] [Google Scholar]
- 83.Cheng EH, Kirsch DG, Clem RJ, et al. Conversion of Bcl-2 to a Bax-like death effector by caspases. Science. 1997;278:1966–1968. doi: 10.1126/science.278.5345.1966. [DOI] [PubMed] [Google Scholar]
- 84.Herbst RS, Frankel SR. Oblimersen sodium (Genasense bcl-2 antisense oligonucleotide): a rational therapeutic to enhance apoptosis in therapy of lung cancer. Clin Cancer Res. 2004;10:4245s–4248s. doi: 10.1158/1078-0432.CCR-040018. [DOI] [PubMed] [Google Scholar]
- 85.Oltersdorf T, Elmore SW, Shoemaker AR, et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature. 2005;435:677–681. doi: 10.1038/nature03579. [DOI] [PubMed] [Google Scholar]
- 86.Viard-Leveugle I, Veyrenc S, French LE, et al. Frequent loss of Fas expression and function in human lung tumours with overexpression of FasL in small cell lung carcinoma. J Pathol. 2003;201:268–277. doi: 10.1002/path.1428. [DOI] [PubMed] [Google Scholar]
- 87.Eymin B, Gazzeri S, Brambilla C, et al. Distinct pattern of E2F1 expression in human lung tumours: E2F1 is upregulated in small cell lung carcinoma. Oncogene. 2001;20:1678–1687. doi: 10.1038/sj.onc.1204242. [DOI] [PubMed] [Google Scholar]
- 88.Salon C, Eymin B, Micheau O, et al. E2F1 induces apoptosis and sensitizes human lung adenocarcinoma cells to death-receptor-mediated apoptosis through specific downregulation of c-FLIP(short) Cell Death Differ. 2006;13:260–272. doi: 10.1038/sj.cdd.4401739. [DOI] [PubMed] [Google Scholar]
- 89.Merdzhanova G, Edmond V, De Seranno S, et al. E2F1 controls alternative splicing pattern of genes involved in apoptosis through upregulation of the splicing factor SC35. Cell Death Differ. 2008;15:1815–1823. doi: 10.1038/cdd.2008.135. [DOI] [PubMed] [Google Scholar]
- 90.Meyerson M. Role of telomerase in normal and cancer cells. J Clin Oncol. 2000;18:2626–2634. doi: 10.1200/JCO.2000.18.13.2626. [DOI] [PubMed] [Google Scholar]
- 91.Bartkova J, Horejsi Z, Koed K, et al. DNA damage response as a candidate anti-cancer barrier in early human tumorigenesis. Nature. 2005;434:864–870. doi: 10.1038/nature03482. [DOI] [PubMed] [Google Scholar]
- 92.Gorgoulis VG, Vassiliou LV, Karakaidos P, et al. Activation of the DNA damage checkpoint and genomic instability in human precancerous lesions. Nature. 2005;434:907–913. doi: 10.1038/nature03485. [DOI] [PubMed] [Google Scholar]
- 93.Nuciforo PG, Luise C, Capra M, et al. Complex engagement of DNA damage response pathways in human cancer and in lung tumor progression. Carcinogenesis. 2007;28:2082–2088. doi: 10.1093/carcin/bgm108. [DOI] [PubMed] [Google Scholar]
- 94.Nakanishi K, Kawai T, Kumaki F, et al. Expression of human telomerase RNA component and telomerase reverse transcriptase mRNA in atypical adenomatous hyperplasia of the lung. Hum Pathol. 2002;33:697–702. doi: 10.1053/hupa.2002.125775. [DOI] [PubMed] [Google Scholar]
- 95.Lantuejoul S, Soria JC, Morat L. Telomere shortening and telomerase reverse transcriptase expression in preinvasive bronchial lesions. Clin Cancer Res. 2005;11:2074–2082. doi: 10.1158/1078-0432.CCR-04-1376. [DOI] [PubMed] [Google Scholar]
- 96.Hiyama K, Hiyama E, Ishioka S, et al. Telomerase activity in small-cell and non-small-cell lung cancers. J Natl Cancer Inst. 1995;87:895–902. doi: 10.1093/jnci/87.12.895. [DOI] [PubMed] [Google Scholar]
- 97.Lantuejoul S, Soria JC, Moro-Sibilot D, et al. Differential expression of telomerase reverse transcriptase (hTERT) in lung tumours. Br J Cancer. 2004;90:1222–1229. doi: 10.1038/sj.bjc.6601643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dikmen ZG, Gellert GC, Jackson S, et al. In vivo inhibition of lung cancer by GRN163L: a novel human telomerase inhibitor. Cancer Res. 2005;65:7866–7873. doi: 10.1158/0008-5472.CAN-05-1215. [DOI] [PubMed] [Google Scholar]
- 99.Esteller M. Epigenetics in cancer. N Engl J Med. 2008;358:1148–1159. doi: 10.1056/NEJMra072067. [DOI] [PubMed] [Google Scholar]
- 100.Shames DS, Girard L, Gao B, et al. A genome-wide screen for promoter methylation in lung cancer identifies novel methylation markers for multiple malignancies. PLoS Med. 2006;3:e486. doi: 10.1371/journal.pmed.0030486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 102.Zochbauer-Muller S, Fong KM, Virmani AK, et al. Aberrant promoter methylation of multiple genes in non-small cell lung cancers. Cancer Res. 2001;61:249–255. [PubMed] [Google Scholar]
- 103.Zochbauer-Muller S, Lam S, Toyooka S, et al. Aberrant methylation of multiple genes in the upper aerodigestive tract epithelium of heavy smokers. Int J Cancer. 2003;107:612–616. doi: 10.1002/ijc.11458. [DOI] [PubMed] [Google Scholar]
- 104.de Fraipont F, Moro-Sibilot D, Michelland S, et al. Promoter methylation of genes in bronchial lavages: a marker for early diagnosis of primary and relapsing non-small cell lung cancer? Lung Cancer. 2005;50:199–209. doi: 10.1016/j.lungcan.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 105.Brock MV, Hooker CM, Ota-Machida E, et al. DNA methylation markers and early recurrence in stage I lung cancer. N Engl J Med. 2008;358:1118–1128. doi: 10.1056/NEJMoa0706550. [DOI] [PubMed] [Google Scholar]
- 106.Gibbons RJ. Histone modifying and chromatin remodeling enzymes in cancer and dysplastic syndromes. Hum Mol Genet. 2005;14:R85–R92. doi: 10.1093/hmg/ddi106. [DOI] [PubMed] [Google Scholar]
- 107.Esteller M. Cancer epigenomics: DNA methylomes and histone-modification maps. Nat Rev Genet. 2007;8:286–298. doi: 10.1038/nrg2005. [DOI] [PubMed] [Google Scholar]
- 108.Jenuwein T, Allis CD. Translating the histone code. Science. 2001;293:1074–1080. doi: 10.1126/science.1063127. [DOI] [PubMed] [Google Scholar]
- 109.Groth A, Rocha W, Verreault A, et al. Chromatin challenges during DNA replication and repair. Cell. 2007;128:721–733. doi: 10.1016/j.cell.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 110.Kouzarides T. Chromatin modifications and their function. Cell. 2007;128:693–705. doi: 10.1016/j.cell.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 111.Fraga MF, Ballestar E, Villar-Garea A, et al. Loss of acetylation at Lys16 and trimethylation at Lys20 of histone H4 is a common hallmark of human cancer. Nat Genet. 2005;37:391–400. doi: 10.1038/ng1531. [DOI] [PubMed] [Google Scholar]
- 112.Van Den Broeck A, Brambilla E, Moro-Sibilot D, et al. Loss of histone H4K20 trimethylation occurs in preneoplasia and influences prognosis of non-small cell lung cancer. Clin Cancer Res. 2008;14:7237–7245. doi: 10.1158/1078-0432.CCR-08-0869. [DOI] [PubMed] [Google Scholar]
- 113.Barlesi F, Giaccone G, Gallegos-Ruiz MI, et al. Global histone modifications predict prognosis of resected non small-cell lung cancer. J Clin Oncol. 2007;25:4358–4364. doi: 10.1200/JCO.2007.11.2599. [DOI] [PubMed] [Google Scholar]
- 114.Cowland JB, Hother C, Gronbaek K. MicroRNAs and cancer. APMIS. 2007;115:1090–1106. doi: 10.1111/j.1600-0463.2007.apm_775.xml.x. [DOI] [PubMed] [Google Scholar]
- 115.Barbarotto E, Schmittgen TD, Calin GA. MicroRNAs and cancer: profile, profile, profile. Int J Cancer. 2008;122:969–977. doi: 10.1002/ijc.23343. [DOI] [PubMed] [Google Scholar]
- 116.Boyd SD. Everything you wanted to know about small RNA but were afraid to ask. Lab Invest. 2008;88:569–578. doi: 10.1038/labinvest.2008.32. [DOI] [PubMed] [Google Scholar]
- 117.Takamizawa J, Konishi H, Yanagisawa K, et al. Reduced expression of the let-7 microRNAs in human lung cancers in association with shortened postoperative survival. Cancer Res. 2004;64:3753–3756. doi: 10.1158/0008-5472.CAN-04-0637. [DOI] [PubMed] [Google Scholar]
- 118.Yanaihara N, Caplen N, Bowman E, et al. Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell. 2006;9:189–198. doi: 10.1016/j.ccr.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 119.Nana-Sinkam SP, Geraci MW. MicroRNA in lung cancer. J Thorac Oncol. 2006;1:929–931. [PubMed] [Google Scholar]
- 120.Calin GA, Sevignani C, Dumitru CD, et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc Natl Acad Sci USA. 2004;101:2999–3004. doi: 10.1073/pnas.0307323101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Eder M, Scherr M. MicroRNA and lung cancer. N Engl J Med. 2005;352:2446–2448. doi: 10.1056/NEJMcibr051201. [DOI] [PubMed] [Google Scholar]
- 122.Hayashita Y, Osada H, Tatematsu Y, et al. A polycistronic microRNA cluster, miR-17–92, is overexpressed in human lung cancers and enhances cell proliferation. Cancer Res. 2005;65:9628–9632. doi: 10.1158/0008-5472.CAN-05-2352. [DOI] [PubMed] [Google Scholar]
- 123.He L, He X, Lowe SW, et al. microRNAs join the p53 network-another piece in the tumour-suppression puzzle. Nat Rev Cancer. 2007;7:819–822. doi: 10.1038/nrc2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bommer GT, Gerin I, Feng Y, et al. p53-mediated activation of miRNA34 candidate tumor-suppressor genes. Curr Biol. 2007;17:1298–1307. doi: 10.1016/j.cub.2007.06.068. [DOI] [PubMed] [Google Scholar]
- 125.Harris KS, Zhang Z, McManus MT, et al. Dicer function is essential for lung epithelium morphogenesis. Proc Natl Acad Sci USA. 2006;103:2208–2213. doi: 10.1073/pnas.0510839103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chiosea S, Jelezcova E, Chandran U, et al. Overexpression of Dicer in precursor lesions of lung adenocarcinoma. Cancer Res. 2007;67:2345–2350. doi: 10.1158/0008-5472.CAN-06-3533. [DOI] [PubMed] [Google Scholar]
- 127.Chatterjee A, Mambo E, Sidransky D. Mitochondrial DNA mutations in human cancer. Oncogene. 2006;25:4663–4674. doi: 10.1038/sj.onc.1209604. [DOI] [PubMed] [Google Scholar]
- 128.Kagan J, Srivastava S, et al. Mitochondria as a target for early detection and diagnosis of cancer. Crit Rev Clin Lab Sci. 2005;42:453–472. doi: 10.1080/10408360500295477. [DOI] [PubMed] [Google Scholar]
- 129.Zhou S, Kachhap S, Sun W, et al. Frequency and phenotypic implications of mitochondrial DNA mutations in human squamous cell cancers of the head and neck. Proc Natl Acad Sci USA. 2007;104:7540–7545. doi: 10.1073/pnas.0610818104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sui G, Zhou S, Wang J, et al. Mitochondrial DNA mutations in preneoplastic lesions of the gastrointestinal tract: a biomarker for the early detection of cancer. Mol Cancer. 2006;5:73. doi: 10.1186/1476-4598-5-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Suzuki M, Toyooka S, Miyajima K, et al. Alterations in the mitochondrial displacement loop in lung cancers. Clin Cancer Res. 2003;9:5636–5641. [PubMed] [Google Scholar]
- 132.Shedden K, Taylor JM, Enkemann SA, et al. Gene expression-based survival prediction in lung adenocarcinoma: a multi-site, blinded validation study. Nat Med. 2008;14:822–827. doi: 10.1038/nm.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Motoi N, Szoke J, Riely GJ, et al. Lung adenocarcinoma: modification of the 2004 WHO mixed subtype to include the major histologic subtype suggests correlations between papillary and micropapillary adenocarcinoma subtypes, EGFR mutations and gene expression analysis. Am J Surg Pathol. 2008;32:810–827. doi: 10.1097/PAS.0b013e31815cb162. [DOI] [PubMed] [Google Scholar]
- 134.Miura K, Bowman ED, Simon R, et al. Laser capture microdissection and microarray expression analysis of lung adenocarcinoma reveals tobacco smoking- and prognosis-related molecular profiles. Cancer Res. 2002;62:3244–3250. [PubMed] [Google Scholar]
- 135.Takeuchi T, Tomida S, Yatabe Y, et al. Expression profile-defined classification of lung adenocarcinoma shows close relationship with underlying major genetic changes and clinicopathologic behaviors. J Clin Oncol. 2006;24:1679–1688. doi: 10.1200/JCO.2005.03.8224. [DOI] [PubMed] [Google Scholar]
- 136.Kwei KA, Kim YH, Girard L, et al. Genomic profiling identifies TITF1 as a lineage-specific oncogene amplified in lung cancer. Oncogene. 2008;27:3635–3640. doi: 10.1038/sj.onc.1211012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wisniewski JR. Mass spectrometry-based proteomics: principles, perspectives, and challenges. Arch Pathol Lab Med. 2008;132:1566–1569. doi: 10.5858/2008-132-1566-MSPPPA. [DOI] [PubMed] [Google Scholar]
- 138.Hanash SM, Pitteri SJ, Faca VM. Mining the plasma proteome for cancer biomarkers. Nature. 2008;452:571–579. doi: 10.1038/nature06916. [DOI] [PubMed] [Google Scholar]
- 139.Conrad DH, Goyette J, Thomas PS. Proteomics as a method for early detection of cancer: a review of proteomics, exhaled breath condensate, and lung cancer screening. J Gen Intern Med. 2008;23 Suppl. 1:78–84. doi: 10.1007/s11606-007-0411-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Saijo N. Advances in the treatment of non-small cell lung cancer. Cancer Treat Rev. 2008;34:521–526. doi: 10.1016/j.ctrv.2008.03.124. [DOI] [PubMed] [Google Scholar]
- 141.Gridelli C. Targeted therapy developments in the treatment of non-small cell lung cancer: a promising but long and winding road. Curr Opin Oncol. 2008;20:145–147. doi: 10.1097/CCO.0b013e3282f43c6e. [DOI] [PubMed] [Google Scholar]