Abstract
The New York Heart Association (NYHA) functional class is a subjective estimate of a patient's functional ability based on symptoms that does not always correlate with the objective estimate of functional capacity, peak oxygen consumption (peak VO2). Additionally, relationships between these two measurements have not been examined in the current medical era when patients are using beta blockers, aldosterone antagonists, and cardiac resynchronization therapy (CRT). Using baseline data from the HF-ACTION (Heart Failure and A Controlled Trial Investigating Outcomes of Exercise TraiNing) study, we examined this relationship.
Methods
1758 patients underwent a symptom limited metabolic stress test and stopped exercise due to dyspnea or fatigue. The relationship between NYHA functional class and peak VO2 was examined. Additionally, the effects of beta blockers, aldosterone antagonists, and CRT therapy on these relationships were compared.
Results
NYHA II patients have a significantly higher peak VO2 (16.1 ± 4.6 vs. 13.0 ± 4.2 ml/kg/min), a lower Ve/VCO2 slope (32.8 ± 7.7 versus 36.8 ± 10.4), and a longer duration of exercise (11.0 ± 3.9 versus 8.0 ± 3.4 minutes) than NYHA III/IV patients. Within each functional class, there is no difference in any of the exercise parameters between patients on or off of beta blockers, aldosterone antagonists, or CRT therapy. Finally, with increasing age a significant difference in peak VO2, Ve/VCO2 slope, and exercise time was found.
Conclusion
For patients being treated with current medical therapy, there still is a difference in true functional capacity between NYHA functional class II and III/IV patients. However, within each NYHA functional class, the presence or absence or contemporary heart failure therapies does not alter exercise parameters.
The New York Heart Association (NYHA) functional class is a subjective estimate of a patient's true functional ability1. While it may be easy to distinguish between an NYHA functional class I and IV patient, it is much more difficult to distinguish between a class II and III patient. This has implications for patient care as well as enrollment in clinical trials. Clinically, many therapies including aldosterone antagonists, hydralazine/isosorbide dinitrate, and biventricular pacemakers are indicated for patients with NYHA functional class III and IV heart failure symptoms but not NYHA functional class II symptoms2. Similarly, when enrolling patients in a clinical trial by functional class, there may be a tendency for “class creep” by investigators to make patients fit the inclusion criteria of an individual study3. To overcome this subjective assessment of a patient's functional capacity, objective measures such as exercise testing have been advocated4.
The measurement of peak oxygen consumption (VO2) has been shown to correlate with functional capacity and mortality. Mancini et al were the first to demonstrate a relationship between peak oxygen consumption and outcomes5. More recently, other measurements obtained during a metabolic exercise test have been shown to predict mortality in patients with end stage heart failure. These measurements include the slope of the relationship between ventilation and carbon dioxide production (Ve/VCO2 slope), end tidal carbon dioxide (CO2), the oxygen uptake efficiency slope, and the rate of heart rate recovery6. Based on this data, metabolic exercise testing is now routinely performed in the assessment of patients for heart transplantation and is often used in the assessment of new therapies for the treatment of heart failure4, 7.
Over the past 10 years, there have been significant advancements in the therapy of heart failure. The use of beta adrenergic blockers, aldosterone antagonists, implantable cardioverter defibrillators (ICDs), and biventricular pacemakers (CRT devices) have all been shown to improve mortality in patients with advanced heart failure8-12. Despite demonstrated improvement in mortality, only biventricular pacemakers have led to improved exercise capacity13-15. Studies evaluating the prognostic ability of peak VO2 were performed in patients prior to the use of these therapies. Therefore, the relationship between peak VO2 and mortality for patients using these therapies is less clear. Peterson et al examined the predictive benefit of peak VO2 for patients on and off beta blockers and found that the outcome for patients on beta blockers was improved for patients with a similar peak VO2 when compared to those not taking beta blockers16. Similar studies with the other therapies have not been performed.
The purpose of this study is to examine the relationship between the objective measurement peak VO2 and the subjective measurement NYHA functional class in patients being treated with current medical therapy. The HF-ACTION (Heart Failure and A Controlled Trial Investigating Outcomes of Exercise TraiNing) trial was a randomized trial evaluating the effects of exercise training in 2331 patients with NYHA functional class II-IV heart failure symptoms17. Prior to randomization, 2329 patients underwent a maximal exercise test with gas exchange to evaluate exercise capacity. We evaluated the relationship between this baseline exercise test and NYHA functional class to test our hypothesis that a relationship still persists for patients utilizing contemporary medical therapy.
Methods
The design of the HF-ACTION trial has been described previously17. In brief, 2331 subjects were enrolled in a randomized trial of exercise training versus usual care to determine if exercise training improves the primary outcome of all-cause mortality or all-cause hospitalization.
Prior to randomization, patients underwent a symptom limited, graded exercise test with the analysis of expired gases. The majority of patients were tested on a treadmill using a modified-Naughton protocol. However, a 10 watt per minute ramp cycle protocol was used for those unable to walk on a treadmill or for those tested at sites where only cycle ergometry was available. Subjects were instructed to take their medications as usual with specific instructions to take their beta blocker between 3 and 10 hours prior to the test. Sites were instructed to exercise patients until they were limited by either dyspnea or fatigue. Additionally, site personnel were told to push the patients to at least a Borg Rating of Perceived Exertion (RPE) of > 16 and/or a respiratory exchange ratio (RER) > 1.1. Patients underwent testing using a metabolic cart and the endpoints of peak VO2, Ve/VCO2 slope, RER, and ventilatory threshold were determined.
Statistical analysis
Of the 2329 patients with a baseline test, 1758 stopped exercise due to dyspnea or fatigue. Other tests were stopped due to angina/ischemia, arrhythmias, musculoskeletal complaints, or adverse changes in blood pressure and these patients were excluded from further analysis. Baseline characteristics were analyzed using descriptive statistics. Continuous variables were presented as medians and interquartile ranges; categorical variables were presented as frequencies and percentage. Continuous variables were compared using the Wilcoxon rank-sum test.
The primary objective of this paper was to assess the relationship between NYHA functional class and exercise endpoints. The exercise endpoints of interest included peak VO2, Ve/VCO2 slope and exercise duration. To analyze the differences in metabolic parameters between NYHA functional classes, the patients were split into NYHA class II, III, and IV. Because there were only 16 patients that were NYHA functional class IV, these patients were combined with the NYHA III patients. The descriptive statistics for the exercise endpoints were provided within each of the two NYHA functional classes (II versus III and IV combined). The impact of other factors which might be associated with the exercise endpoints including use of beta blockers, aldosterone/antagonists and CRT was then examined. Due to its known impact on functional capacity, we also evaluated the effect of age on the exercise endpoints. The General Linear Model (GLM) was used to compare the differences in exercises endpoints between the two NYHA functional class groupings in a model that included effects for the use of beta blockers, the use of aldosterone/antagonists, the use of CRT, and age (> 50, 50−70 and > 70). The interactions between NYHA functional class and each of the other factors in the model were also examined. Statistical comparisons were performed using 2-sided significance test and were considered significant at p ≤ 0.05. SAS statistical software (version 9.1, Cary, NC) was used for all analyses.
Results
The baseline characteristics of the patients are shown in Table 1. The mean age was 59 years old and 71% of the patients were male. Only 48.5% of the patients had an ischemic etiology. Greater than 95% of the participants were appropriately treated with either an ACE inhibitor or angiotensin receptor blocker (ARB) and almost 95% being treated with a beta blocker. Perhaps reflecting the time when this trial started, only 39.1% of the patients had implantation of an ICD and 16.5% had a biventricular pacemaker.
Table 1.
Baseline demographics
| N | 1758 |
| Age (yrs) | 58.8 (51.0, 67.8) |
| Body mass index () | 30.0 (26.0, 35.5) |
| Male, n (%) | 1245 (70.8) |
| Race – African American, n (%) | 588 (34.0) |
| White, n (%) | 1055 (61.0) |
| Other, n (%) | 86 (5.0) |
| Ejection fraction (%) | 24.6 (20.1, 30.1) |
| Ischemic etiology, n (%) | 853 (48.5) |
| Hypertension, n (%) | 1030 (59.0) |
| Diabetes, n (%) | 556 (31.6) |
| Therapies | |
| ACE inhibitors, n (%) | 1313 (74.7) |
| ARB, n (%) | 413 (23.5) |
| Beta blocker, n (%) | 1668 (94.9) |
| Digoxin, n (%) | 781 (44.4) |
| Aldosterone antagonist, n (%) | 788 (44.8) |
| Biventricular pacemaker, n (%) | 290 (16.5) |
| ICD, n (%) | 687 (39.1) |
| Systolic blood pressure (mmHg) | 110.0 (100.0, 126.0) |
| Heart rate (bpm) | 70.5 (63.0, 79.0) |
Values expressed as medians and interquartile ranges or number and percent. ACE – angiotensin converting enzyme, ARB – angiotensin II receptor blocker, bpm – beats per minute, ICD – implantable cardioverter defibrillator
The exercise endpoints for the entire 1758 patients and those with NYHA functional class II and III/IV symptoms are shown in Table 2. For the entire cohort, the peak VO2 was 15.0 ml/kg/min with a Ve/VCO2 slope of 34.2. The patients exercised to an RER of 1.1 and the duration of exercise time was almost 10 minutes. When evaluating the differences between NYHA functional classes, the NYHA functional class II patients have a significantly greater peak VO2 and a lower Ve/VCO2 slope than classes III and IV. As expected, this was associated with a longer exercise time but no difference in RER or Borg RPE.
Table 2.
Exercise endpoints
| Total | NYHA II | NYHA III/IV | |
|---|---|---|---|
| Peak VO2 (ml/kg/min) | 15.0 ± 4.7 (1717) | 16.1 ± 4.6* (1099) | 13.0 ± 4.2* (618) |
| Ve/VCO2 slope | 34.2 ± 8.9 (1702) | 32.8 ± 7.7* (1091) | 36.8 ± 10.4* (611) |
| Peak RER | 1.1 ± 0.1 (1703) | 1.1 ± 0.1 (1091) | 1.1 ± 0.1 (612) |
| Borg RPE | 16.7 ± 2.3 (1747) | 16.8 ± 2.3 (1116) | 16.7 ± 2.3 (631) |
| Exercise time (min) | 9.9 ± 4.0 (1742) | 11.0 ± 3.9* (1110) | 8.0 ± 3.4* (632) |
Values expressed as mean ± standard deviation (n). NYHA – New York Heart Association, VO2 – oxygen consumption, Ve – Ventilation, VCO2 – Carbon dioxide production, RER – Respiratory exchange ratio, RPE – Rating of Perceived Exertion.
- p value < 0.01
Similar to NYHA functional class, there was a significant relationship between age and exercise capacity. As depicted in Table 3, younger patients had significantly better peak VO2, Ve/VCO2 slope, and exercise time than older patients.
Table 3.
Exercise endpoints by functional class and age.
| NYHA II | |||
|---|---|---|---|
| Age < 50 | 50−70 | >70 | |
| Peak VO2 (ml/kg/min) | 17.7 ± 5.0 (265) | 16.1 ± 4.4* (633) | 14.1 ± 3.8* (201) |
| Ve/VCO2 slope | 30.0 ± 6.3 (263) | 33.0 ± 7.6* (630) | 36.1 ± 8.2* (198) |
| Peak RER | 1.1 ± 0.1 (263) | 1.1 ± 0.1 (630) | 1.1 ± 0.1 (198) |
| Borg RPE | 17.0 ± 2.4 (270) | 16.8 ± 2.3 (642) | 16.4 ± 2.2 (204) |
| Exercise time (min) | 12.5 ± 4.4 (268) | 10.9 ± 3.6* (638) | 9.3 ± 3.4* (204) |
| NYHA III/IV | |||
|---|---|---|---|
| Age < 50 | 50−70 | >70 | |
| Peak VO2 (ml/kg/min) | 14.6 ± 5.2 (119) | 13.0 ± 4.1* (352) | 11.7 ± 3.2* (142) |
| Ve/VCO2 slope | 32.4 ± 9.0 (118) | 36.4 ± 10.1* (346) | 41.4 ± 10.4* (147) |
| Peak RER | 1.1 ± 0.1 (118) | 1.1 ± 0.1 (348) | 1.1 ± 0.1 (146) |
| Borg RPE | 17.1 ± 2.3 (121) | 16.8 ± 2.3 (360) | 16.1 ± 2.3 (150) |
| Exercise time (min) | 9.5 ± 3.7 (120) | 8.1 ± 3.3* (360) | 6.6 ± 2.7* (152) |
Values expressed as mean ± standard deviation (n). Abbreviations as in Table 2.
- p value < 0.01 for within NYHA functional class comparisons.
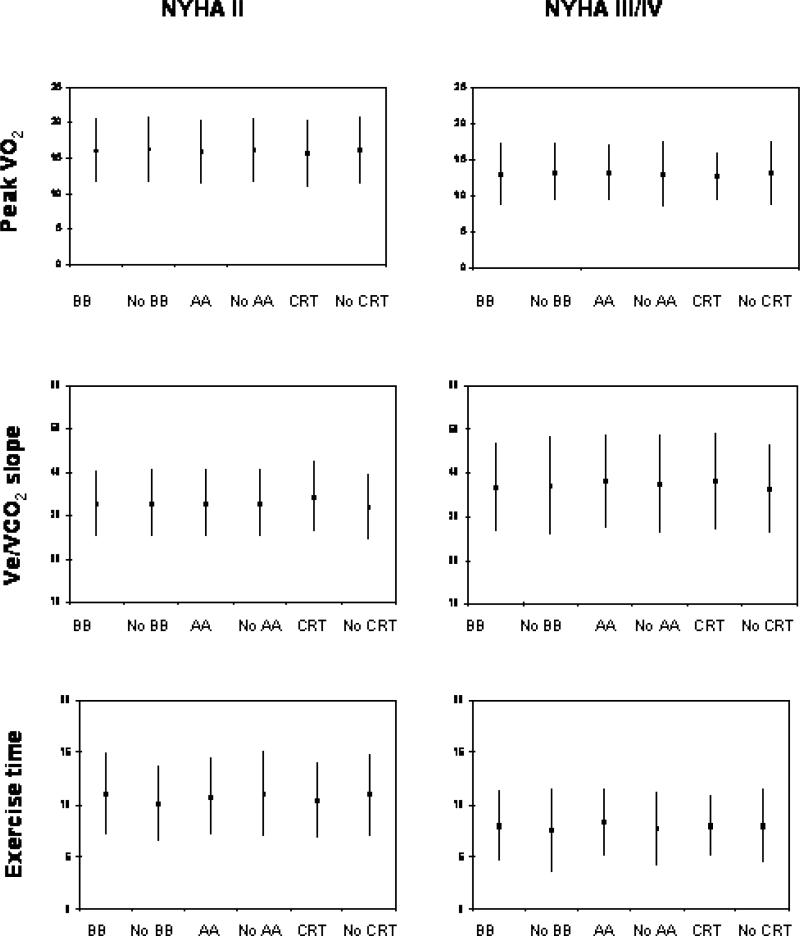
Next, the effects of the use of beta blockers, aldosterone antagonists, CRT therapy, and age on exercise capacity within each functional class were examined. For patients with NYHA functional class II symptoms, as shown in figure 1 there was no difference in peak VO2 (ml/kg/minute) for patients on or off beta blockers (16.1±4.6 versus 16.3±4.6, p=0.64), aldosterone antagonists (16.0±4.5 versus 16.2±4.6, p=0.73), or CRT therapy (15.7±4.1 versus 16.2±4.7, p=0.29). Similarly, for Ve/VCO2 slope, there was no difference in patients on or off beta blockers (32.9±7.7 versus 31.9±7.0, p=0.47), aldosterone antagonists (32.6±7.6 versus 32.9±7.7, p=0.29). However, there was a difference for those on or off CRT therapy (34.4±8.2 versus 32.2±7.6, p=0.005) although this small change is not clinically significant. Finally, for exercise duration, there was no difference in patients on or off beta blockers (11.0±3.9 minutes versus 10.1±3.6, p=0.11), aldosterone antagonists (10.8±3.7 versus 11.1±4.0, p=0.28), or CRT (10.4±3.6 versus 11.0±3.9, p=0.10). For all 3 exercise parameters, there was a significant difference based on age as shown in table 3.
Figure 1.
Mean plus/minus standard deviation of patients peak VO2 measured in ml/kg/minute, Ve/VCO2 slope, and exercise duration in minutes for patients taking or not taking beta blockers (BB – n = 1668, No BB – n = 90), aldosterone antagonists (AA – n = 788, no AA – n = 970), or CRT therapy (CRT – n = 290, No CRT – n = 1468). Patients are split by their NYHA functional class.
The results are quite similar for those with NYHA functional class III/IV symptoms. There was no significant difference in peak VO2 for those on versus off beta blockers (13.0±4.3 versus 13.2±4.0, p=0.64), aldosterone antagonists (13.2±3.9 versus 12.9±4.5, p=0.12), or CRT therapy (12.7±3.3 versus 13.1±4.5, p=0.86). Likewise, for Ve/VCO2 slope, patients on or off beta blockers (36.7±10.3 versus 37.2±11.3, p=0.96), aldosterone antagonists (36.1±9.4 versus 37.4±11.2, p=0.29), or CRT therapy (38.3±11.0 versus 36.3±10.2, p=0.07) had similar values. Finally, the exercise time was not different between those on or off beta blockers (8.0±3.4 minutes versus 7.6±4.0, =0.20) or CRT therapy (8.0±2.9 minutes versus 8.0±3.5, p=0.70), but was mildly prolonged for those on aldosterone antagonists (8.3±3.2 minutes versus 7.7±3.5, p=0.003). Similar to the NYHA II patients, for each age group all 3 of the exercise parameters had a significant difference as shown in table 3.
Discussion
For patients being treated with current medical therapy, there is a significant difference in the exercise endpoints of peak VO2, Ve/VCO2 slope, and exercise time in patients with NYHA functional class II symptoms compared to those with NYHA functional class III/IV symptoms. Within each NYHA functional class, there is no clinically significant difference in peak VO2, Ve/VCO2 slope, or exercise time for patients on or off beta blockers, aldosterone antagonists, or CRT therapy. Similar to NYHA functional class, the peak VO2, Ve/VCO2 slope and exercise time also varies by age.
Metabolic exercise testing is useful for the evaluation of heart failure patients. Depending on the variable used, it has been shown to be useful for determining overall prognosis, survival with heart transplantation, and the etiology of functional limitations to exercise4-7, 16. Peak VO2, the most widely studied gas exchange variable, has been shown to vary based on the type of exercise, gender, age, the baseline level of activity, and natural endowment18. One limitation of peak VO2 is that it is effort dependent. Various methods are used to ensure a maximal test including pushing a patient to an RER > 1.1 and/or a Borg RPE > 16, but there still is some inherent limitation because of the effort requirement. Because of this limitation, investigators have now shown that the effort independent Ve/VCO2 slope has similar if not greater prognostic significance for patients with heart failure19-22. In multiple studies, a Ve/VCO2 slope > 34 has greater prognostic prediction for mortality than the classic peak VO2 of < 14 ml/kg/min23. While some authors have evaluated the differences in peak VO2 based on functional class or medications, the effects of these differences on Ve/VCO2 slope are unclear. For both clinical and research purposes, understanding the effects of both medications and devices on these variables is quite important.
Weber et al were the first to evaluate the relationship between NYHA functional class and maximum oxygen uptake24. Sixty two patients were split into four different classifications based on a VO2 max of > 20 ml/kg/min (A), 16−20 ml/kg/min (B), 10−15 ml/kg/min (C), and < 10 ml/kg/min (D). Although the NYHA functional classes tended to correlate with the Weber classes, the correlation was not perfect, as Weber class B patients included patients with NYHA class I-III symptoms and Weber class C patients included patients ranging from NYHA class I to IV symptoms. Williams et al further studied the relationship of NYHA functional class and oxygen consumption in 96 patients25. Although there was some overlap between peak VO2 values within each NYHA class, they did report a significant correlation between peak VO2 and both N-BNP and NYHA functional class indicating differences between peak VO2 by NYHA class.
Using the baseline metabolic exercise test in the HF-ACTION trial, we have now shown that age and NYHA functional class are associated with peak VO2, Ve/VCO2 slope, and exercise time, but the use of beta blockers, aldosterone antagonists, or CRT therapy are not. This is consistent with the findings of Weber et al and Williams et al who both found that peak VO2 varied by functional capacity24, 25. An additional novel finding in our data is that the Ve/VCO2 slope also varies by NYHA class.
Of interest, three new therapies that improve mortality – beta blockers, aldosterone antagonists, and CRT devices - did not affect exercise endpoints in a clinically significant manner in this study. This finding is not surprising for patients on beta blockade. Despite improving mortality and quality of life, studies have not reliably shown an improvement in exercise capacity with beta blockers26. In contrast, CRT therapy has been shown to improve peak VO2 by 1.1 ml/kg/min in the MIRACLE ICD trial of patients with NYHA functional class III/IV symptoms14. Based on this finding, one would expect that patients with a CRT device would have a higher peak VO2, lower Ve/VCO2 slope, and longer exercise duration. However, a sub study of the COMPANION trial evaluating patients with NYHA class IV symptoms demonstrated no difference in 6 minute walk distance so perhaps the functional benefit is not as pronounced as initially expected27.
Implications
These results have important clinical and research implications. Clinically, metabolic stress testing is often used to determine prognosis and functional capacity in patients with advanced heart failure. For an individual patient, one can use subjective symptoms such as NYHA functional class to estimate exercise capacity based on this data. However, as shown previously, there is a fair amount of overlap between these classes and NYHA functional class should not be solely relied on to determine listing for transplantation. Additionally, for any group of patients grouped by functional class, one should not expect to see differences in any exercise endpoint based on the presence or absence of beta blocker, aldosterone antagonist, or CRT therapy. It is important to distinguish this from the use of either peak VO2 or Ve/VCO2 slope when predicting mortality. This study does not evaluate the outcomes of these patients and it is quite possible that patients being treated with these therapies may have superior outcomes than untreated patients with a similar peak VO2.
From a research perspective, metabolic stress testing is often used as a secondary endpoint when evaluating the use of therapies in patients with heart failure4, 28. Also, many therapies have been tested in patients with NYHA class III/IV symptoms, but have not yet been examined in NYHA class I or II patients. For future trials, the use of metabolic exercise testing variables as a decision point for inclusion criteria would help to understand the group of patients that will or will not benefit from a therapy. There now are approximate definitions based on NYHA function class (Class II: peak VO2 16.1 ml/kg/min, Ve/VCO2 slope 32.8 and class III/IV: peak VO2 13.0 ml/kg/min, Ve/VCO2 slope 36.8).
Limitations
There are several limitations to this analysis. First, almost 95% of the patients were being treated with beta blocker therapy at the start of the trial. Although there were a large number of patients in the trial, the small number not taking a beta blocker may make it difficult to demonstrate a difference between those being treated and not being treated with these agents. There are also a small number of patients with CRT devices. Second, this study only evaluates relationships between exercise parameters and therapies at one point in time. Some patients may have recently had a change in therapies and experience a further effect on these outcomes over time. However, subjects were not to be enrolled unless they were on stable therapy and further improvements in functional capacity or NYHA function class should be minimal. Finally, the relationship between metabolic exercise parameters, therapies, and clinical outcomes is not yet available. Further studies evaluating the effects of these differences on clinical outcomes should be performed.
Conclusion
In conclusion, for patients with heart failure, functional capacity endpoints including peak VO2 and Ve/VCO2 slope vary based on age and NYHA functional class. This relationship is not affected by newer therapies that alter mortality in these patients such as beta blockers, aldosterone antagonists, and CRT devices.
Acknowledgments
A complete list of the HF-ACTION Investigators can be found at JAMA. 2009;301:1449. This research was supported by National Institutes of Health grants: 5U01HL063747, 5U01HL068973, 5U01HL066501, 5U01HL066482, 5U01HL064250, 5U01HL066494,5U01HL064257, 5U01HL066497, 5U01HL068980, 5U01HL064265, 5U01HL066491, 5U01HL064264, R37AG18915, P60AG10484.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ClinicalTrials.gov Identifier: NCT00047437
Funding Source: National Institutes of Health; National Heart, Lung, and Blood Institute
References
- 1.The Criteria Committee of the New York Heart Association . Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels. 9th ed Little, Brown & Co; Boston, Mass: 1994. pp. 253–256. [Google Scholar]
- 2.Adams KF, Lindenfeld J, Arnold JMO, Baker DW, Barnard DH, Baughman KL, Boehmer JP, Deedwania P, Dunbar SB, Elkayam U, Gheorghiade M, Howlett JG, Konstam MA, Kronenberg MW, Massie BM, Mehra MR, Miller AB, Moser DK, Patterson JH, Rodeheffer RJ, Sackner-Bernstein J, Silver MA, Starling RC, Stevenson LW, Wagoner LE. Executive Summary: HFSA 2006 Comprehensive Heart Failure Practice Guideline. J Cardiac Failure. 2006;12:10–38. [Google Scholar]
- 3.Kubo SH, Schulman S, Starling RC, Jessup M, Wentworth D, Burkhoff D. Development and validation of a patient questionnaire to determine New York Heart Association classification. J Cardiac Fail. 2004;10:228–235. doi: 10.1016/j.cardfail.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Fleg JL, Pina IL, Balady GJ, Chaitman BR, Fletcher B, Lavie C, Limacher MC, Stein RA, Williams M, Bazzarre T. Assessment of functional capacity in clinical and research applications. An advisory from the Committee on Exercise, Rehabilitation, and Prevention Council on Clinical Cardiology, American Heart Association. Circulation. 2000;102:1591–1597. doi: 10.1161/01.cir.102.13.1591. [DOI] [PubMed] [Google Scholar]
- 5.Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH, Wilson JR. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation. 1991;83:778–786. doi: 10.1161/01.cir.83.3.778. [DOI] [PubMed] [Google Scholar]
- 6.Myers J, Arena R, Dewey F, Bensimhon D, Abella J, Hsu L, Chase P, Guazzi M, Peberdy MA. A cardiopulmonary exercise testing score for predicting outcomes in patients with heart failure. Am Heart J. 2008;156:1177–83. doi: 10.1016/j.ahj.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, Mohacsi P, Augustine S, Aaronson K, Barr M. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant. 2006;25:1024–42. doi: 10.1016/j.healun.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 8.MERIT-HF Study Group Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353:2001–2007. [PubMed] [Google Scholar]
- 9.Packer M, Coats AJS, Fowler MB, Katus HA, Krum H, Mohacsi P, Rouleau JL, Tendera M, Castaigne A, Roecker EB, Schultz MK, DeMets DL, for the Carvedilol Prospective Randomized Cumulative Survival Study Group Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–1658. doi: 10.1056/NEJM200105313442201. [DOI] [PubMed] [Google Scholar]
- 10.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 11.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, DeMarco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM, for the Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Eng J Med. 2004;350:2140–2150. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 12.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, for the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Eng J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 13.Gullestad L, Manhenke C, Aarsland T, Skardal R, Fagertun H, Wikstrand J, Kjekshus J. Effect of metoprolol CR/XL on exercise tolerance in chronic heart failure – a substudy to the MERIT-HF trial. Eur J Heart Fail. 2001;3:463–468. doi: 10.1016/s1388-9842(01)00146-5. [DOI] [PubMed] [Google Scholar]
- 14.Young JB, Abraham WT, Smith AL, Leon AR, Lieberman R, Wilkoff B, Canby RC, Schroeder JS, Liem LB, Hall S, Wheelan KR, for the Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE ICD) Trial Investigators Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA. 2003;289:2685–2694. doi: 10.1001/jama.289.20.2685. [DOI] [PubMed] [Google Scholar]
- 15.Abraham WT, Young JB, Leon AR, Adler S, Bank AJ, Hall SA, Lieberman R, Liem LB, O'Connell JB, Schroeder JS, Wheelan KR, on behalf of the Multicenter InSync ICD II Study Group Effects of cardiac resynchronization on disease progression in patients with left ventricular systolic dysfunction, an indication for an implantable cardioverter-defibrillator, and mildly symptomatic chronic heart failure. Circulation. 2004;110:2864–2868. doi: 10.1161/01.CIR.0000146336.92331.D1. [DOI] [PubMed] [Google Scholar]
- 16.Peterson LR, Schechtman KB, Ewald GA, Geltman EM, de las Fuentes L, Meyer T, Krekeler P, Moore ML, Rogers JG. Timing of cardiac transplantation in patients with heart failure receiving b-adrenergic blockers. J Heart Lung Transplant. 2003;22:1141–1148. doi: 10.1016/s1053-2498(02)01225-1. [DOI] [PubMed] [Google Scholar]
- 17.Whellan DJ, O'Connor CM, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, Leifer ES, Kraus WE, Kitzman DW, Blumenthal JA, Rendall DS, Houston-Miller N, Fleg JL, Schulman KA, Piña IL, HF-ACTION Trial Investigators Heart failure and a controlled trial investigating outcomes of exercise training (HF-ACTION): design and rationale. Am Heart J. 2007;153:201–11. doi: 10.1016/j.ahj.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Higginbotham MB. Cardiovascular applications for cardiopulmonary exercise testing. Cont Int Med. 1995;12:16–27. [Google Scholar]
- 19.Chua TP, Ponikowski P, Harrington D, Anker SD, Webb-Peploe K, Clark AL, Poole-Wilson PA, Coats AJS. Clinical correlates and prognostic significance of the ventilatory response to exercise in chronic heart failure. J Am Coll Cardiol. 1997;29:1585–1590. doi: 10.1016/s0735-1097(97)00078-8. [DOI] [PubMed] [Google Scholar]
- 20.Robbins M, Francis G, Pashkow RJ, Snader CE, Hoercher K, Young JB, Lauer MS. Ventilatory and heart rate responses to exercise. Better predictors of heart failure mortality than peak oxygen consumption. Circulation. 1999;100:2411–2417. doi: 10.1161/01.cir.100.24.2411. [DOI] [PubMed] [Google Scholar]
- 21.Francis DP, Shamim W, Davies LC, Piepoli MF, Ponikowski P, Anker SD, Coats AJS. Cardiopulmonary exercise testing for prognosis in chronic heart failure: continuous and independent prognostic value from Ve/VCO2 slope and peak VO2. Eur Heart J. 2000;21:154–161. doi: 10.1053/euhj.1999.1863. [DOI] [PubMed] [Google Scholar]
- 22.Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA. Peak VO2 and Ve/VCO2 slope in patients with heart failure: A prognostic comparison. Am Heart J. 2004;147:354–360. doi: 10.1016/j.ahj.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev. 2008;13:245–69. doi: 10.1007/s10741-007-9067-5. [DOI] [PubMed] [Google Scholar]
- 24.Weber KT, Kinasewitz GT, Janicki JS, Fishan AP. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation. 1982;65:1213–1223. doi: 10.1161/01.cir.65.6.1213. [DOI] [PubMed] [Google Scholar]
- 25.Williams SG, Ng LL, O'Brien RJ, Taylor S, Wright DJ, Li YF, Tan LB. Complementary roles of simple variables, NYHA and N-BNP, in indicating aerobic capacity and severity of heart failure. Int J Cardiol. 2005;102:279–286. doi: 10.1016/j.ijcard.2004.05.054. [DOI] [PubMed] [Google Scholar]
- 26.Gullestad L, Manhenke C, Aarsland T, Skardal R, Fagertun H, Wikstrand J, Kjekshus J. Effect of metoprolol CR/XL on exercise tolerance in chronic heart failure – a substudy to the MERIT-HF trial. Eur J Heart Fail. 2001;3:463–468. doi: 10.1016/s1388-9842(01)00146-5. [DOI] [PubMed] [Google Scholar]
- 27.Lindenfeld J, Feldman AM, Saxon L, Boehmer J, Carson P, Ghali JK, Anand I, Singh S, Steinberg JS, Jaski B, DeMarco T, Mann D, Yong P, Galle E, Ecklund F, Bristow M. Effects of cardiac resynchronization therapy with or without a defibrillator on survival and hospitalizations in patients with New York Heart Association class IV heart failure. Circulation. 2007;115:204–212. doi: 10.1161/CIRCULATIONAHA.106.629261. [DOI] [PubMed] [Google Scholar]
- 28.Narang R, Swedberg K, Cleland JG. What is the ideal study design for evaluation of treatment for heart failure? Insights from trials assessing the effect of ACE inhibitors on exercise capacity. Eur Heart J. 1996;17:120–134. doi: 10.1093/oxfordjournals.eurheartj.a014670. [DOI] [PubMed] [Google Scholar]