Abstract
Aims
The aim of the study was to describe Registered Nurses’ reports of unmet nursing care needs and examine the variation of nursing care quality across hospitals.
Background
Large proportions of Registered Nurses have reported leaving necessary care activities undone because they lacked the time to complete the activities. Nursing care left undone can be expected to adversely affect the quality of care. However, little is known about the degree of variation in the quality of nursing care across hospitals.
Methods
In 2008, a secondary analysis of a 1999 survey of Registered Nurses (N=10,184) was conducted using descriptive and comparative statistics. Data were derived from inpatient staff nurses working in acute care hospital settings (N=168). A hospital-level measure (i.e. unmet nursing care needs) of the quality of nursing care was developed from care needs left undone among all nurses.
Results
Across hospitals there was a wide range in the proportion of Registered Nurses who reported leaving each nursing care need undone. They reported leaving 2 out of 7 necessary nursing care activities undone during their last shift. After controlling for nurses’ demographic information, we found statistically significant variations in the quality of nursing care across hospitals.
Conclusion
Differences in nursing care quality across hospitals appear to be closely associated with variations in the quality of care environments. Understanding the determinants of unmet nursing care needs can support policy decisions on systems and human resources management to enhance nurses’ awareness of their care practices and the care environment.
Keywords: Variations, Nursing Care, Quality, Hospitals, secondary analysis
INTRODUCTION
Registered Nurses represent a patient surveillance system and are essential to the prevention and early detection of adverse patient events (Clarke & Aiken, 2003). Adverse events occur in an estimated 2.9 to 3.7 percent of acute care hospitalizations in the United States of America (U.S.A.), and it is estimated that between 44,000 and 98,000 patients die in hospitals each year as a result, with nearly half due to errors in the delivery of care (Institute of Medicine, 2000). A recent systematic review of eight studies conducted in the U.S.A., Australia, United Kingdom (U.K.), and Canada revealed that the median overall incidence of in-hospital adverse events was 9.2% and that 43.5% of the incidents were preventable, with 7.2% leading to death (De Vries Ramrattan et al., 2008). Theoretically, if nurses fail to carry out necessary nursing care, then the effectiveness of patient surveillance may be compromised and lead to a preventable adverse patient event.
Registered Nurses (RNs) may find it increasingly difficult to provide necessary nursing care due to the increasing complexity of healthcare delivery (i.e. new technologies, numerous providers’ treatment recommendations, regulatory constraints, and patients’ illness severity), and continuing efforts to contain costs by reducing hospital length of stay. Hospital in-patient average length of stay continued to decline from 1990 to 2005 among developed countries (e.g., USA from 9.1 to 6.5 days, U.K. from 17.6 to 9.0 days, Japan from 50.5 to 35.7 days, and Spain from 12.2 to 8.5 days) (Organisation for Economic Co-Operation and Development, 2009). The intended consequence of this trend is to reduce overall healthcare expenditures. However, sicker patients who do not receive the benefits of receiving necessary nursing care may have increased length of stays, which could result in financial losses for hospitals.
It has been documented for over 50 years that the time RNs spend on nursing care activities may affect the quality of care. In 1954, a study of nursing in three general hospitals in the USA reported that RNs spent as little as 50 percent of their time on accomplishing required care activities (Abdellah & Levine, 1954). In 2000 and 2004, more than 9 out of 10 RNs in the USA reported that not having enough time to spend with patients was a major problem affecting the quality of their nursing care (Buerhaus et al., 2005). Large proportions reported leaving necessary nursing care activities undone because they lacked the time to complete the activities (Aiken et al., 2001). In the USA, Canada, and Germany, the proportion of RNs reporting necessary care left undone ranged from 13 to 53 percent (Aiken et al., 2001). Meanwhile, little is known about the degree of variation in the quality of nursing care across hospitals. In this paper we address this issue by examining the omission of necessary nursing care needs across hospitals as a quality indicator of nursing care. Documenting variations in nursing care quality in this way may be compelling to policymakers, hospital and nursing managers, and staff nurses as they seek to manage and prioritize nursing care to maximize patient and hospital outcomes.
BACKGROUND
Theoretical Model
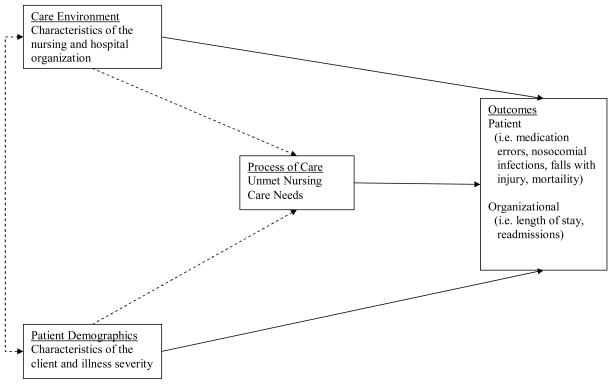
The conceptual framework that guided this study, the Process of Care and Outcomes Model (Figure 1), has origins in Donabedian’s (1966) quality paradigm. While Donabedian emphasizes a linear relationship between doing things right (i.e. processes) and having the right things happen (i.e. outcomes), in this study we explored the quality of nursing care by examining necessary “things” left undone by nurses. The study was informed further by the Quality Health Outcomes Model (QHOM) (Mitchell et al., 1998) developed by the American Academy of Nursing. The QHOM illustrates the relationships of four main constructs, namely interventions, client, system, and outcomes. The effect of interventions on outcomes is thought to be mediated by system and/or client characteristics. The QHOM provides a broader understanding than Donabedian’s structure-process-outcome framework about key variables to consider when examining the process of care (i.e. interventions).
Figure 1.
Process of Care and Outcomes Model
The Process of Care and Outcomes Model (Figure 1) incorporates elements of the structure-process-outcome and quality health outcomes models. The model posits a temporal relationship among the care environment, patient factors, the process of care, and outcomes. The care environment, patient factors, and the process of care have a direct relationship on outcomes. The traditional structural characteristics of the nursing and hospital organization are built in to the care environment. Nursing care can be thought of as a healthcare organization’s surveillance function for the early detection of deterioration in patients’ health status. Since nurses are continually adapting to changes in the care environment and patients’ health status, the association between the process of care and outcomes may be influenced by both the care environment and patient factors. If the care environment is considered an “organized agency, such as a hospital or provider network” (Mitchell et al., 1998, p. 44), then the nurse practice environment, nurse staffing, and hospital size and ownership would be structural characteristics that influence the process of care, patients, and outcomes. Registered Nurses’ reports of “unmet nursing care needs” provide a measure of what nurses were not able to do for patients, and serve as a hospital level indicator of the quality of nursing care. Unmet nursing care needs refer to nursing care activities considered necessary by RNs but left undone during their last shift worked because they lacked the time to complete them.
Process of Care
The process of care has been considered an essential element of quality care for more than four decades (Donabedian, 1966, 1988, 2003; Doran et al., 2006; Hegyvary & Haussman, 1976; Lindeman et al., 1978; Mitchell et al., 1989). The traditional “nursing process,” a clinical problem-solving technique, makes it possible to identify processes of care (Leddy & Pepper, 1993). Processes of care are grouped into assessment (i.e. clinical history and physical examination), planning (i.e. care plan development, and coordination/continuity of care), intervening (i.e. performance of therapeutic interventions including teaching and communicating information to patients), and evaluation (i.e. measure progress towards desired health integrity or quality of life) (Donabedian, 2003; Yura & Walsh, 1973).
An early study of the process of nursing care showed that only a minority of patients received up to 60 percent more direct care during periods of increased nurse staffing (Aydelotte & Tener, 1960). While the characterizations of the process of care in that study may not be completely relevant to today’s nursing, the majority of nursing activities detailed are still provided by RNs. Through direct observation, the processes of nursing care were identified and grouped into seven major categories: 1) Direct Patient Care Activities Controlled by the Nurse (e.g. bathing, comforting/communicating with patients), 2) Direct Patient Care Activities only partially Controlled by the Nurse (e.g. nutrition, treatments, and procedures), 3) Variable Communication (e.g. charting and information exchange), 4) Cleaning and Specimens (e.g. maintenance of the ward and patient intake and output), 5) Non-Variable Communication (e.g. nurse-to-nurse report and clerical duties), 6) Preparations (e.g. gathering equipment and preparing medications), and 7) Personal and Miscellaneous Activities (e.g. student teaching, rest periods, and surveillance of comatose patients). In more recent times, standardized nursing vocabularies such as the Nursing Interventions Classification (McCloskey & Bulechek, 2004) and International Classification for Nursing Practice (International Council of Nurses, 1996) have been developed in an attempt to describe the nursing process, document nursing care, and facilitate the aggregation of data for comparisons at multiple levels.
Nurse reports of tasks left undone may provide a measure that indicates the quality of nursing care. In a study of 8,670 nurses, Sochalski (2004) examined the association between tasks left undone and the quality of care. Forty percent of the nurses reported three or more tasks left undone. Nurses rated the quality of nursing care delivered to their patient on their last shift as poor, fair, good, and excellent. There was a strong relationship (r = .634, P < 0.001) between the number of tasks left undone and the quality of nursing care. The contribution of tasks left undone, workload, and patient safety problems to the quality of nursing care was examined using linear regression. While all three variables were statistically significantly associated with quality, tasks left undone produced the largest share of the explained variance (β = −.21, SE = .004; p < .001).
Quality of the Process of Care
Chang et al (2002) found systematic variations in the quality of nursing care. This study of 291 heart failure and 283 patients who had cerebrovascular accidents in five US states used scales measuring specific aspects of nursing care: assessment, problem identification, and problem management. Expert professional nurses identified specific types of independent nursing activities through medical record reviews. Nursing activities were grouped into scales and combined to rate the overall quality of the process of nursing care. About one third of patients received inadequate care. The investigators found statistically significant variations in the quality of nursing care by hospital size, geographical location, and level of poverty only for patients with heart failure. Hospitals in zip (postal) code areas with greater poverty as well as small hospitals had statistically significantly poorer nursing care quality.
Until recently, a national database on the quality of care provided by hospitals did not exist in the USA (American Hospital Association, 2007). The Hospital Quality Alliance (HQA) is the first initiative that routinely evaluates quality of care data on certain processes of care for patients with acute myocardial infarction, heart failure, and pneumonia. Researchers using HQA data have found that the quality of care in US hospitals varies greatly among processes of care, medical conditions, and outcomes (Jha et al., 2005; Werner & Bradlow, 2006). Werner and Bradlow (2006) determined that these process measures were correlated with and predictive of hospitals’ risk-adjusted mortality rates. According to Werner and Bradlow, if one third of the 750,000 patients hospitalized per year who received care at the lowest-performing hospitals received care at the high-performing hospitals instead, approximately 3,000 more lives could have been saved.
Researchers have further documented variation in care using a combination of HQA data and data reported by hospitals to the Joint Commission on Accreditation of Hospital Organizations (Landon et al., 2006). Only 75.9 percent of patients hospitalized with acute myocardial infarction, heart failure, and pneumonia received recommended care. In the final analysis, hospitals with more technology available and higher RN staffing levels had higher performance on all of the process of care measures.
THE STUDY
Aims
The aims of the study were to: 1) describe Registered Nurses’ reports of unmet nursing care needs, and 2) examine the variation of nursing care quality across hospitals.
Design
A secondary analysis was carried out in 2008 of data collected in 1999 for a study in which RNs in the state of Pennsylvania (USA) were surveyed about their work setting.
Participants
A questionnaire was mailed to the homes of a 50% random sample of RNs who resided in Pennsylvania and were on the rolls of the Pennsylvania State Board of Nursing. Questionnaires were returned by 42,000 RNs, yielding a 52% response rate, an average of 200 RNs for each of the 210 general hospitals operating in Pennsylvania. The study included nurses from all nursing unit types.
Registered Nurses were included in the study if they met the following criteria: 1) worked in one of the 210 acute care hospitals in the state of Pennsylvania, 2) worked as a staff nurse, 3) worked in an acute care environment, and 4) cared for at least one patient but fewer than 20 patients during their last shift worked (Aiken et al., 2002). Hospitals met the inclusion criteria if: 1) there were sufficient nurse respondents to yield a reliable estimate for an aggregate measure of unmet nursing care needs, and 2) the organization reported surgical discharges to the Pennsylvania Healthcare Cost Containment Council in the specific categories studied in the parent study. An average of 60 nurse respondents from each hospital completed the questionnaires; half of the sample hospitals had more than 50 nurse respondents, and more than 80% of the hospitals had more than 25 nurse respondents. The analyses were performed on a sample of 10,184 nurses who worked in 168 acute care hospitals.
Data Collection
In the parent study, RNs were surveyed in 1999 to obtain demographic information and information about their care environment. The original questionnaire has been translated with minor adaptations and used internationally (i.e. Canada, U.K., Germany, Russia, Armenia, and Japan) (Aiken et al., 2001). Other items included patient workload, perceptions about burnout, job satisfaction, and perceptions of nursing quality.
Nurses
Demographic information including gender, age, experience, highest nursing degree, and employment status was collected in the original survey of Pennsylvania Registered Nurses.
Care environment
The Practice Environment Scale of the Nursing Work Index (PES-NWI) (Lake, 2002) was used as a measure of the nursing organization. The PES-NWI was developed from the Nursing Work Index, a questionnaire containing factors thought to contribute to nurse job satisfaction and quality nursing care (NWI) (Kramer & Hafner, 1989). Registered Nurses were asked to indicate the degree of agreement (i.e. strongly agree, somewhat agree, somewhat disagree, and strongly disagree) to each of the 31 PES-NWI items. Data from the 1999 survey of the American Hospital Association, the Pennsylvania Department of Health Hospital Questionnaire, and the Pennsylvania Bureau of Professional and Occupational Affairs public use data file contained measures of the hospital organization (i.e. bed size, technology status, and surgeon board certification).
Unmet nursing care needs
Unmet nursing care needs were measured based on Registered Nurses’ reports of necessary nursing care left undone. This questionnaire item was constructed based on focus groups of acute care staff RNs. The activities comprise nursing interventions related to the overall process of care that if left undone may compromise the quality of nursing care. Respondents were asked to indicate among the list of seven activities which were necessary but left undone because they lacked the time to complete them. The questionnaire item contained the following seven activities: teach patients or family, prepare patients and families for discharge, comfort/talk with patients, adequately document nursing care, back rubs and skin care, oral hygiene, and develop or update nursing care plans.
A hospital-level measure unmet nursing care needs was developed from individual nurses’ reports of necessary nursing activities left undone (Sochalski, 2004). Unmet nursing care needs overall may provide a useful quality indicator of nursing care in a hospital. To construct the hospital-level composite measure of unmet nursing care needs, an individual composite measure was calculated as the average count of unmet nursing care needs for each nurse. Individual nurse composite measures were then aggregated for each hospital, resulting in a mean number of unmet nursing care needs by nursing in a hospital.
Ethical Considerations
The institutional review board of the affiliated university approved the study. Implied consent in the parent study was obtained from nurses upon return receipt of the mailed survey to the investigators. Confidentiality was maintained through the use of a unique identification number on each questionnaire, and findings are reported in the aggregate.
Data Analysis
The initial steps of the analysis examined descriptive statistics of the study participants, the care environment, and unmet nursing care needs overall. Continuous variables were assessed based on the mean, median, standard deviation, and range. The assessment of unmet nursing care needs across hospitals was examined using univariate statistics. Measures of central tendency, variability, and symmetry were used to appraise each care need left undone and the unmet nursing care needs composite measure across hospitals.
Variation in unmet nursing care needs across hospitals was examined in successive analyses. First, the variation in unmet nursing care needs was assessed based on the distribution of the composite measure of unmet nursing care needs across hospitals. Theoretically, the composite measure should be normally distributed with a range of 0 to 7. It is unlikely that the distribution would cover the theoretical range because some care needs may have been met and other care needs may not have been perceived as necessary. A meaningful distribution of the hospital-level measure of unmet nursing care needs was expected to cover at least half of the theoretical range. Next, analysis of variance (ANOVA) was used to examine whether the variation in the mean number of unmet nursing care needs (i.e. composite measure) was greater across hospitals than within hospitals. Finally, analysis of covariance (ANCOVA) was used to take into account the composition of nurses (i.e. age, gender, experience, education) to examine variation in the mean number of unmet nursing care needs across hospitals. Care environment variables were not controlled for because these variables are a part of the context. In other words, the objective was not to explain the differences in unmet nursing care needs, but to explicate patterns of variation in this variable across hospitals.
Stata 9.0 was used to analyze the data. Statistical significance was set at p < .05 for the ANOVA and ANCOVA.
RESULTS
Demographic Characteristics of the Nurses
Nurses in this study were 40 years old on average and 93% were female. The average nurse had nearly 14 years of nursing experience, and 10 years of experience in their current hospital position. Almost 40% of the nurses’ highest nursing degree was the baccalaureate degree or higher, followed by the diploma (35%) and then the associate degree (24%). Ninety-five percent were permanently employed in a hospital.
Characteristics of the Care Environment
Table 1 shows the nursing organization characteristics. On average, nurses in this study cared for six patients during their last shift. Based on the Practice Environment Scale of the Nursing Work Index (Lake, 2002) subscale scores, most nurses reported that Nursing Foundations for Quality of Care and Collegial Relations between Nurses and Physicians were present in their care environment. There was wide variation in the nursing education mix across hospitals. Hospitals on average had slightly more than one-third of their nursing workforce educated at the baccalaureate degree or higher.
Table 1.
Distribution of Nursing Organization Characteristics
| Variable | Mean (SD) | Median | Range |
|---|---|---|---|
| Nurse Staffing† | 6.3 (1.7) | 6.0 | 3.4–17.6 |
| BSN-MIX (%)†† | 35.0 (14.0) | 33.0 | 0–0.78 |
| PES-NWI††† | |||
| Nurse Participation in Hospital Affairs* | 2.3 (0.2) | 2.3 | 1.5–2.8 |
| Nursing Foundations for Quality of Care** | 2.8 (0.2) | 2.8 | 2.1–3.3 |
| Nurse Manager Ability, Leadership, and Support of Nurses | 2.4 (0.3) | 2.3 | 1.3–3.2 |
| Staffing and Resource Adequacy | 2.2 (0.1) | 2.2 | 1.2–3.0 |
| Collegial Relations between Nurses and Physicians | 2.8 (0.2) | 2.8 | 2.1–3.1 |
Note.
Nurse staffing is the average number of patients per nurse across hospitals.
BSN-MIX is the proportion of nurses per hospital with a Baccalaureate, Master’s, or higher nursing degree.
PES-NWI is the Practice Environment Scale of the Nurse Work Index (Lake, 2002).
Nurse Participation in Hospital Affairs is the participatory role and valued status of nurses in a broad hospital context.
Nurse Foundations for Quality of Care is the pervasiveness of nursing philosophy, a nursing rather than a medical model of care, and nurses’ clinical competence.
A majority of the hospitals were medium in size, with 101 to 250 beds (Table 2). Almost two-thirds were non-teaching facilities and 72% were classified as high technology. Admitting surgeons who were board certified (i.e., surgeons who are certified medical specialists) ranged from 0% to 98% across hospitals.
Table 2.
Characteristics of the Hospitals (N=168)
| Variable | Mean (SD) | Range | Hospitals (%) | Nurses (%) |
|---|---|---|---|---|
| Surgeon Board Certified (%)* | 70.0 (22.0) | 0.0–98.0 | ||
| Hospital Size | ||||
| Fewer than 100 beds | 41 (24.0) | 16,123 (7.0) | ||
| 101–250 beds | 95 (57.0) | 110,510 (47.0) | ||
| More than 250 beds | 32 (19.0) | 105,709 (46.0) | ||
| Hospital Teaching Status | ||||
| Non-teaching | 107 (64.0) | 99,907 (43.0) | ||
| Minor-teaching | 44 (26.0) | 78,996 (34.0) | ||
| Major-teaching | 17 (10.0) | 53,439 (23.0) | ||
| Hospital High Technology | ||||
| Yes | 121 (72.0 | 103,824 (45.0) | ||
| No | 47 (28.0) | 128,518 (55.0) | ||
Note.
Surgeon Board Certified is the proportion of surgeons who are certified medical specialists in a hospital.
Nurse Reports of Care Needs Left Undone
Among the seven care needs left undone captured in this study, developing or updating nursing care plans was the activity left undone by most nurses (Table 3). This was followed closely by comforting/talking with patients (40.3%), back rubs and skin care (31.7%), teaching patients and family (28.5%), adequately documenting nursing care (21.4%), oral hygiene (20.8%), and preparing patients and families for discharge (12.9%).
Table 3.
Percent of Nurses Reporting Care Needs Left Undone (N=10,184)
| Variable | Frequency (%) |
|---|---|
| Develop or update nursing care plans | 4,274 (42.0) |
| Comfort/talk with patients | 4,101 (40.3) |
| Back rubs and skin care | 3,232 (31.7) |
| Teach patients or family | 2,902 (28.5) |
| Adequately document nursing care | 2,179 (21.4) |
| Oral hygiene | 2,117 (20.8) |
| Prepare patients and families for discharge | 1,312 (12.9) |
Unmet Nursing Care Needs across Hospitals
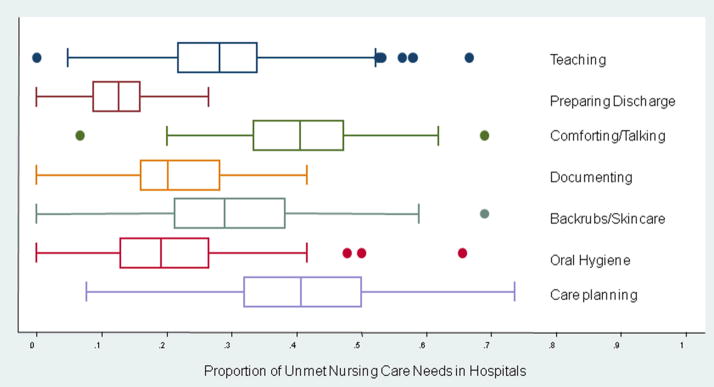
Table 4 gives the hospital distribution of each unmet nursing care need. The proportion of RNs reporting leaving nursing care needs undone across hospitals was nearly identical to the overall individual reports. On average, 41 percent left developing or updating nursing care plans undone and 12 percent left preparing patients and families for discharge undone. The range of unmet nursing care needs varied from as low as 26% for preparing patients and families for discharge to as high as 74% for developing or updating nursing care plans in some hospitals. The variation of nurses reporting leaving developing or updating nursing care plans undone was slightly right-skewed across the 168 hospitals. Examining this variation using a series of box-and-whisker plots (Figure 2) reveals that the broad dispersion in four of the seven unmet nursing care needs was due to a few outlying hospitals.
Table 4.
Proportion of Nurses Reporting Unmet Nursing Care Needs (N=168)
| Variable | Mean | SD | Median | Range | α |
|---|---|---|---|---|---|
| Unmet Nursing Care Needs | |||||
| Develop or update nursing care plans | 41.0 | 13.0 | 32.0 | 8.0–74.0 | |
| Comfort/talk with patients | 40.0 | 10.0 | 41.0 | 7.0–69.0 | |
| Back rubs and skin care | 30.0 | 13.0 | 30.0 | 0–69.0 | |
| Teach patients or family | 29.0 | 11.0 | 28.0 | 0–67.0 | |
| Adequately document nursing care | 22.0 | 9.0 | 20.0 | 0–42.0 | |
| Oral hygiene | 20.0 | 10.0 | 19.0 | 0–66.0 | |
| Prepare patients and families for discharge | 12.0 | 6.0 | 13.0 | 0–26.0 | |
| Unmet nursing care needs composite | 1.9 | 0.5 | 1.9 | 0.2–3.5 | 0.73 |
Note. The distribution of each unmet care needs is based on the proportion of nurses reporting leaving the care need(s) undone. The Unmet Nursing Care Needs Composite was derived from the aggregate average sum of unmet nursing care needs.
Figure 2.
Box and Whisker Plots of Unmet Nursing Care Needs (N=168)
A composite measure of unmet nursing care needs was constructed to evaluate the variation of the quality of nursing care across hospitals. The internal consistency of this composite measure was confirmed with a Cronbach’s alpha coefficient of 0.73. Across hospitals, RNs reported leaving an average of 2 out of 7 nursing care activities undone, with a range of 0.2 to 3.5 (Table 4). This variation was statistically significantly greater for unmet nursing care needs across hospitals than within hospitals (df = 167, F = 3.49). Table 5 presents the degree of variation across hospitals for unmet nursing care needs after taking into account nurse’s demographic information. The composition of the nurses in hospitals did not affect the statistical significance of the variation across hospitals. The F value for unmet nursing care needs (df = 167, F = 3.17) exceeded the critical value at the .001 level of probability across hospitals.
Table 5.
Analysis of Covariance for Unmet Nursing Care Needs Composite Measure (N=10,184)
| Source | df† | Partial SS†† | MS††† | F†††† |
|---|---|---|---|---|
| Model± | 172 | 2739.17 | 15.93 | 4.72** |
| Hospital | 167 | 1784.42 | 10.69 | 3.17** |
| Sex | 1 | 21.75 | 21.75 | 6.45* |
| Age | 1 | 7.74 | 7.74 | 2.29 |
| Years in nursing | 1 | 225.06 | 225.06 | 66.73** |
| Years in hospital | 1 | 6.35 | 6.35 | 1.88 |
| Baccalaureate degree or higher | 1 | 0.01 | 0.01 | 0.00 |
| Residual | 8625 | 29090.71 | 3.37 | |
| Total | 8797 | 31829.88 | 3.62 |
Note.
p < .05.
p < .001.
Model refers to the effects of both the predictor (i.e. hospital) and the covariates.
df (degrees of freedom) is the number of values in the final statistical calculation that were free to vary.
Partial SS (sums of square) is the variation contributed uniquely by each independent variable.
MS (mean square) is the estimate of the population variance based on the variability among the independent variables (MS = SS / df).
F (F-test) is a test of differences between groups (F=between-group variability / within-group variability).
DISCUSSION
This study is the first known to examine closely the variation in unmet nursing care needs in a large set of hospitals. However, research has continued to document nurses’ reports of nursing care left undone. Canadian nurses (n=4,799) in 49 acute care hospitals and hemodialysis nurses (n=422) in the USA have reported leaving 30% and 18% of necessary nursing care undone, respectively (Estabrooks et al., 2005; Thomas-Hawkins et al., 2008). In the current investigation we found extensive and statistically significant variation in unmet nursing care needs. These differences in unmet nursing care needs across hospitals may explain in part the variation in hospital quality overall (Donabedian, 1966).
Study Limitations
A common limitation in secondary analysis is the reliance on data collected for unrelated research purposes. While the data used were not initially intended for the purpose of this study, thoughtful deliberation was given to the theoretical and conceptual congruence for data use. Ideally, data at the nursing unit level would provide a more desirable measure of unmet nursing care needs. This study extends previously published research (Aiken et al., 2001; Aiken et al., 2002; Aiken et al., 2003) by characterizing the quality of nursing care across hospitals based on unmet nursing care needs.
While the care activities were internally consistent as a whole, the question remains whether the unmet nursing care needs composite is a valid measure of the quality of nursing care. Future researchers should give consideration to a process of care measure that captures more than what nurse “do or don’t do” for their patients. The conceptual basis may be the capacity of nurses intellectually and physically to organize and deliver necessary nursing care. Researchers (Schubert et al., 2008) asked Swiss nurses to assess how often nursing activities were performed during the previous seven working days using a Likert type scale (i.e. never = 0, rarely = 1, sometimes = 2, often = 3, very often = 4). The nursing care activities were grouped into five categories (i.e. activities of daily living, caring-support, rehabilitation-instruction-education, monitoring-safety, and documentation) (Schubert et al., 2007). These five categories included direct (i.e. bathing/skin care and monitoring vital signs) and indirect (i.e. coping with the delayed response of a physician and formulate/update patient care plans) nursing care activities. A measure of this type would yield information with greater meaning because the quality of nursing care in hospitals could be ranked in the aggregate.
There may be concerns about the time between when the original data were collected in the parent study and its current use. However, there are few studies addressing the process of nursing care, because nursing care activities are often difficult to measure and data are typically not collected by healthcare organizations. The process of care has demonstrated enduring relevance over time (Donabedian, 1966, 1988, 2003) and the conceptualization of the nursing process of care has remained practically constant (Aydelotte & Tener, 1960; Chang et al., 2002; Doran et al., 2006; Hageman & Ventura, 1981; Hegyvary & Haussman, 1976; Lindeman et al., 1978; Mitchell et al., 1989). The data used in this study provided an opportunity to contribute to our understanding of a limited topic of research.
Discussion of results
The large number of respondents as well as the exclusive information about hospital settings allowed for the characterization of the quality of nursing care for a group of RNs who worked in a large number of acute care settings. The demographic characteristics of the nurses in this study were similar to the U.S. National Sample Survey of Registered Nurses conducted in 2000 (Spratley et al., 2002). The number of RNs who responded to the survey was directly proportional to the number of RN positions in each hospital. This suggests response rates were similar across hospitals, which should theoretically mitigate any hospital response bias (Aiken et al., 2003).
We documented considerable variation in the proportion of nurses who reported leaving necessary nursing care undone and found statistically significant variations in nursing care quality across hospitals in Pennsylvania. There were instances in which 60% or more of the nurses in a hospital left a necessary care need undone on their last shift. The distribution of unmet nursing care needs overall revealed a meaningful representation of the quality of nursing care. It may be common that 28% or more care overall is left undone by RNs in hospitals. These findings are disturbing because unmet nursing care needs were identified by nurses, given that the care activities were both necessary and left undone during their last shift. The proportion of care left undone by this large number of nurses across 168 hospitals confirms in part RNs’ continued concern about the quality of care.
While the effect of nurse staffing on outcomes (e.g. mortality, hospital length of stay, and adverse events) has been consistently documented by research internationally (Aiken et al., 2002; Estabrooks et al., 2005; Rafferty et al., 2007; Van den Heede et al., in press), the causal pathway linking nurse staffing to outcomes is not well understood. Chang and colleagues (2002) found that variation in the care of patients with heart failure (n=291) was associated with hospital type in a study of the quality of nursing care based on five process of nursing care scales. The statistically significant variation in nursing care quality across hospitals in our study suggests that real differences in nursing care quality may be more closely associated with the variation in hospital care environments, including nurse staffing.
Nurses have the greatest amount of direct contact with patients and are the largest segment of healthcare providers in developed nations (Organisation for Economic Co-Operation and Development, 2008). Learning the consequences of unmet nursing care needs may influence nursing managers to develop evidence-based resource allocation and strategies and interventions (e.g. staffing improvements or better workforce management policies) with the goal of improving patient outcomes (Aiken et al., 2001). A set of nursing care quality measures and methods could serve as a gold standard for nursing care, such as the National Database of Nursing Quality Indicators (American Nurses Association, 2005). Linking unmet nursing care needs to outcomes may give further support for policy related to pay-for-performance reimbursement programmes (Trude et al., 2006).
Hospital organizations must develop care environments that integrate individual and organizational behaviors which seek to continuously reduce harm to patients that may result from poor nursing care quality or unmet nursing care needs. Nurses must rely on behavioral (e.g. back rubs and skin care) and cognitive (e.g. teach patients or family, comfort/talk with patients, and develop or update nursing care plans) skills to prevent and detect potential patient adverse events (Institute of Medicine, 2004). For example, when nurses are bathing patients they are actually performing a number of cognitive skills, such as assessing skin color for evidence of poor oxygenation, evaluating skin integrity for signs of skin breakdown, engaging patients in conversation to assess mental status, or educating them about their disease and its management. This study points to the need for nursing research on the relationship between the process of care and adverse events to improve healthcare quality.
Given the assumption that outcomes are not only the result of healthcare structures but also of the process of care (Donabedian, 1966, 1988), the statistically significant variation in the quality of nursing care in this study was expected. Numerous international studies have documented variations in a number of outcomes that may be influenced by the quality of nursing care, including mortality (Aiken et al., 2002; Estabrooks et al.,, 2005; Heijink et al., 2008; Jarman et al., 1999; Price et al., 2006; Wolfe et al., 2004), activities of daily living (Wolfe et al., 2004), length of stay (Ashton et al., 1999; Brooks, 2001; Paul-Shaheen et al., 1987; Price et al., 2006; Wennberg, 1999), and use of services (Wolfe et al., 2004). The variation in nursing care quality found in this large scale analysis of 10,184 nurses across 168 hospitals supports both theoretical and empirical assertions about the associations between variations in the care environment (i.e. nursing staffing), the process of nursing care (i.e. interventions), and outcomes (Hammermeister et al., 1995).
CONCLUSION
Our study was an innovative approach to evaluate the quality of nursing care across hospitals. Unlike nursing care quality based on Donabedian’s conceptualization, unmet nursing care needs has rarely been used to measure nursing care quality. While there is a clear distinction between nursing care done for patients versus nursing care left undone, the empirical evidence from this study supports the theoretical underpinnings of Donabedian’s quality paradigm which have been recognized internationally. Evaluating nursing care quality based on nursing care deficiencies may be more congruent conceptually in a care environment characterized by poor nurse staffing and higher than average adverse event rates. Research on the determinants of unmet nursing care needs can support policy decisions on systems and human resources management to enhance nurses’ awareness of their care practices and the care environment. These policies could support nurses’ capacity to identify unsafe situations and minimize or eliminate potential harm to patients. This is especially important not only because evidence from this study supports the hypothesis that variations in nursing care quality reflect differences in hospital care environments, but also due to nurses’ ongoing concern about spending insufficient time with patients.
SUMMARY STATEMENT
What is already known about this topic
Nurses have the greatest amount of direct contact with patients and are the largest segment of healthcare providers in developed nations.
Large proportions of Registered Nurses have reported leaving necessary nursing care activities undone because they lacked the time to complete the activities.
for more than five decades, Registered Nurses have voiced their concerns about spending insufficient time with patients to deliver quality care.
What this paper adds
Data on unmet nursing care needs provides researchers with a measure to comprehensively evaluate the quality of care across hospitals.
Large proportions of care left undone by Registered Nurses Across a large number of hospitals confirm in part nurses’ ongoing concern about the quality of nursing care.
Verifying the existence of variation in nursing care quality across hospitals supports assertions about the associations between variations in the care environment, the process of care, and outcomes.
Implications for practice and/or policy
Real differences in nursing care quality may be more closely associated with the variation in the care environments of hospitals.
Learning the consequences of unmet nursing care needs may influence nursing managers to develop evidence-based resource allocation and strategies and interventions, with the goal of improving patient outcomes.
Hospital and nursing managers must promote care environments which continuously reduce harm to patients that may result from poor nursing care quality by endorsing a culture of safety.
Acknowledgments
We thank Sean P. Clark, RN, PhD and Suzanne Bakken DNSc, RN for their review and suggestions for improving the manuscript.
Funding
Preparation of the manuscript was supported by the Reducing Health Disparities through Informatics Training Program (NIH T32-NR007969, Suzanne Bakken, PI) and Advanced Training in Nursing Outcomes Research (NIH T32- 007104, Linda Aiken, PI). Data were collected under NIH R01-NR-005043, Linda Aiken, PI.
Footnotes
Conflicts of Interest
No conflict of interest has been declared by the author(s).
Author Contributions:
RJL & ETL were responsible for the study conception and design
LHA performed the data collection
RJL performed the data analysis.
RJL were responsible for the drafting of the manuscript.
RJL, ETL & LHA made critical revisions to the paper for important intellectual content.
RJL & ETL provided statistical expertise.
LHA obtained funding
LHA provided administrative, technical or material support.
RJL, ETL & LHA supervised the study
Contributor Information
Robert J. Lucero, Postdoctoral Research Fellow, Center for Evidence-Based Practice in the Underserved, Columbia University, New York, USA, 212-342-6886, rl2451@columbia.edu.
Eileen T. Lake, Associate Professor, School of Nursing, Secondary Faculty, Department of Sociology, Associate Director, Center for Health Outcomes and Policy Research, University of Pennsylvania, USA.
Linda H. Aiken, The Claire M. Fagin Leadership Professor of Nursing, Professor of Sociology, Director, Center for Health Outcomes and Policy Research, University of Pennsylvania, USA
References
- Abdellah F, Levine E. Work-sampling applied to the study of nursing personnel. Nursing Research. 1954;3(1):11–16. [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA-Journal of the American Medical Association. 2003;290(12):1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA-Journal of the American Medical Association. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty AM, Shamian J. Nurses’ reports on hospital care in five countries. Health Affairs. 2001;20(3):43–53. doi: 10.1377/hlthaff.20.3.43. [DOI] [PubMed] [Google Scholar]
- American Hospital Association. Hospital quality alliance. 2007 Retrieved April 1, 2007, from http://www.aha.org/aha/key_issues/qualityalliance/
- American Nurses Association. National database of nursing quality indicators: Guidelines for data collection and submission on quarterly indicators. Kansas City, KS: 2005. [Google Scholar]
- Ashton CM, Petersen M, Souchek J, Menke TJ, Yu HJ, Pietz K, Eigenbrodt ML, Barbour G, Kizer KW, Wray NP. Geographic variations in utilization rates in veterans affairs hospitals and clinics. New England Journal of Medicine. 1999;340(1):32–39. doi: 10.1056/NEJM199901073400106. [DOI] [PubMed] [Google Scholar]
- Aydelotte ME, Tener M. An investigation of the relationship between nursing activity and patient welfare. Iowa City, Iowa: The University of Iowa; 1960. [Google Scholar]
- Buerhaus PI, Donelan K, Ulrich BT, Norman L, Williams M, Dittus R. Hospital RNs’ and CNOs’ perceptions of the impact of the nursing shortage on the quality of care. Nursing Economics. 2005;23(5):214–221. [PubMed] [Google Scholar]
- Brooks N. Length of stay in community hospitals. Nursing Standard. 2001;15:33–8. doi: 10.7748/ns2001.03.15.27.33.c2998. [DOI] [PubMed] [Google Scholar]
- Chang BL, Lee JL, Pearson ML, Kahn KL, Elliott MN, Rubenstein LL. Evaluating quality of nursing care: The gap between theory and practice. Journal of Nursing Administration. 2002;32(7/8):405–418. doi: 10.1097/00005110-200207000-00009. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Aiken LH. Failure to rescue. American Journal of Nursing. 2003;103(1):42–47. doi: 10.1097/00000446-200301000-00020. [DOI] [PubMed] [Google Scholar]
- De Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Quality and Safety in Health Care. 2008;17:216–223. doi: 10.1136/qshc.2007.023622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. Evaluating quality of medical care. Milbank Memorial Fund Quarterly-Health and Society. 1966;44(3):166–206. [PubMed] [Google Scholar]
- Donabedian A. The quality of care: How can it be assessed. JAMA-Journal of the American Medical Association. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Donabedian A. An Introduction to Qaulity Assurance in Health Care. Oxford: University Press; 2003. [Google Scholar]
- Doran D, Harrison MB, Laschinger H, Hirdes J, Rukholm E, Sidani S, Hall ML, Tourangeau AE, Cranley L. Relationship between nursing interventions and outcome achievement in acute care settings. Research in Nursing and Health. 2006;29(1):61–70. doi: 10.1002/nur.20110. [DOI] [PubMed] [Google Scholar]
- Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The impact of hospital nursing characteristics on 30-day mortality. Nursing Research. 2005;54(2):74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Hageman PT, Ventura MR. Utilizing Patient Outcome Criteria to Measure the Effects of a Medication Teaching Regimen. Western Journal of Nursing Research. 1981;3(1):25–33. [Google Scholar]
- Hammermeister KE, Shroyer AL, Sethi GK, Grover FL. Why it is important to demonstrate linkages between outcomes of care and processes and structures of care. Medical Care. 1995;33(10):OS5–OS16. doi: 10.1097/00005650-199510001-00002. [DOI] [PubMed] [Google Scholar]
- Hegyvary ST, Haussman RK. Correlates of the quality of nursing care. Journal of Nursing Administration. 1976;6(9):22–27. [PubMed] [Google Scholar]
- Heijink R, Koolman X, Pieter D, Van Der Veen A, Jarman B, Westert G. Measuring and explaining mortality in Dutch hospitals; The hospital standardized mortality rate between 2003 and 2005. BMC Health Services Research. 2008;8:73. doi: 10.1186/1472-6963-8-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. To err is human: Building a safer health system. Washington, District of Columbia: National Academy Press; 2000. [Google Scholar]
- Institute of Medicine. Keeping patients safe: Transforming the work environment of nurses. Washington, District of Columbia: National Academy Press; 2004. [Google Scholar]
- International Council of Nurses. The International Classification for Nursing Practice: a unifying framework. Geneva, Switzerland: International Council of Nurses; 1996. [Google Scholar]
- Jarman B, Gault S, Alves B, Hider A, Dolan S, Cook A, Hurwitz B, Iezzoni LI. Explaining differences in English hospital death rates using routinely collected data. British Medical Journal. 1999;318:1515–1520. doi: 10.1136/bmj.318.7197.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Li ZH, Orav EJ, Epstein AM. Care in U.S. hospitals: The hospital quality alliance program. New England Journal of Medicine. 2005;353(3):265–274. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- Kramer M, Hafner LP. Shared values: Impact on staff nurse job-satisfaction and perceived productivity. Nursing Research. 1989;38(3):172–177. [PubMed] [Google Scholar]
- Lake ET. Development of the practice environment scale of the nursing work index. Research in Nursing & Health. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Landon BE, Normand SLT, Lessler A, O’Malley AJ, Schmaltz S, Loeb JM, Mcneil BJ. Quality of care for the treatment of acute medical conditions in U.S. hospitals. Archives of Internal Medicine. 2006;166(22):2511–2517. doi: 10.1001/archinte.166.22.2511. [DOI] [PubMed] [Google Scholar]
- Leddy S, Pepper J. Conceptual basis for professional nursing. 3. Philadelphia, Pennsylvania: Lippincott Company; 1993. [Google Scholar]
- Lindeman CA, Enloe CH, Funderburk L, Gruendemann B, Harmon M, Kneedler J, Nolan M, Van Poole M. AORN-WICHE report. Relationship between OR nursing activities and patient outcomes. AORN- Journal of the Association of Operating Room Nurse’s. 1978;27(2):203–219. [PubMed] [Google Scholar]
- McCloskey JC, Bulecheck GM, editors. Nursing Interventions Classification (NIC) St. Louis: Missouri, Mosby; 2004. [PubMed] [Google Scholar]
- Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. Image - The Journal of Nursing Scholarship. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. [DOI] [PubMed] [Google Scholar]
- Mitchell PH, Armstrong S, Simpson TF, Lentz M. American association of critical-care nurses demonstration project: Profile of excellence in critical care nursing. Heart and Lung. 1989;18(3):219–237. [PubMed] [Google Scholar]
- National Center for Health Statistics. Healthy, United States, 2006. Washington, District of Columbia: U.S. Department of Health and Human Services; 2006. [Google Scholar]
- Organisation for Economic Co-Operation and Development. SourceOECD: Statistics. 2008 Retrieved September 10, 2008, from http://miranda.sourceoecd.org/vl=1234089/cl=12/nw=1/rpsv/cgi-bin/jsearch_oecd_stats.
- Organisation for Economic Co-Operation and Development. SourceOECD: Statistics. 2009 Retrieved January 30, 2009, from http://miranda.sourceoecd.org/vl=1234089/cl=12/nw=1/rpsv/cgi-bin/jsearch_oecd_stats.
- Paul-Shaheen P, Clark JD, Williams D. Small area analysis: A review and analysis of the North-American literature. Journal of Health Politics Policy and Law. 1987;12(4):741–809. doi: 10.1215/03616878-12-4-741. [DOI] [PubMed] [Google Scholar]
- Price LC, Lowe D, Hosker HSR, Anstey K, Pearson MG, Roberts CM. UK National COPD Audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax. 2006;61:837–842. doi: 10.1136/thx.2005.049940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, Aiken LH. Outcomes of variation in hospital nurse staffing in English hospitals: Cross-sectional analysis of survey data and discharge records. International Journal of Nursing Studies. 2007;44(2):175–182. doi: 10.1016/j.ijnurstu.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, de Geest S. Rationing of nursing care and its relationship to patient outcomes: The Swiss extension of the international hospital outcomes study. International Journal for Quality in Health Care. 2008;20(4):227–237. doi: 10.1093/intqhc/mzn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Schaffert-Witvliet B, de Geest S. Validation of the basal extent of rationing of nursing care instrument. Nursing Research. 2007;56(6):416–424. doi: 10.1097/01.NNR.0000299853.52429.62. [DOI] [PubMed] [Google Scholar]
- Sochalski J. Is more better? The relationship between nurse staffing and the quality of nursing care in hospitals. Medical Care. 2004;42(2):67–73. doi: 10.1097/01.mlr.0000109127.76128.aa. [DOI] [PubMed] [Google Scholar]
- Spratley E, Johnson A, Sochalski J, Fritz M, Spencer W. The registered nurse population, March 2002. Washington, District of Columbia: U.S. Department of Health and Human Services; 2002. [Google Scholar]
- Thomas-Hawkins C, Flynn L, Clarke SP. Relationships between registered nurse staffing, processes of nursing care, and nurse-reported patient outcomes in chronic hemodialysis units. Nephrology Nursing Journal: Journal of the American Nephrology Nurses’ Association. 2008;35:123–30. [PMC free article] [PubMed] [Google Scholar]
- Trude S, Au M, Christianson JB. Health plan pay-for-performance strategies. American Journal of Managed Care. 2006;12(9):537–542. [PubMed] [Google Scholar]
- Van den Heede K, Sermeus W, Diya L, Clarke SP, Lesaffre E, Vleugels A, Aiken LH. Nurse staffing and patient outcomes in Belgian acute hospitals: Cross-sectional analysis of administrative data. International Journal of Nursing Studies. doi: 10.1016/j.ijnurstu.2008.05.007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg JE. Understanding geographic variations in health care delivery. New England Journal of Medicine. 1999;340(1):52–53. doi: 10.1056/NEJM199901073400111. [DOI] [PubMed] [Google Scholar]
- Werner RM, Bradlow ET. Relationship between Medicare’s hospital compare performance measures and mortality rates. JAMA-Journal of the American Medical Association. 2006;296(22):2694–2702. doi: 10.1001/jama.296.22.2694. [DOI] [PubMed] [Google Scholar]
- Wolfe CDA, Tilling K, Rudd A, Giroud M, Inzitari D. Variations in care and outcome in the first year after stroke: a Western and Central European perspective. Journal of Neurology Neurosurgery and Psychiatry. 2004;75:1702–1706. doi: 10.1136/jnnp.2004.039438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yura H, Walsh MB. The Nursing Process: Assessing, Planning, Implementing, and Evaluating. New York, New York: Appleton Century Crofts; 1973. [Google Scholar]