Abstract
Background
The Institute of Medicine has identified patients as a key source of information for assessing the quality of care.
Objective
To evaluate the association of physician specialty with the content and quality of follow-up cancer care.
Design and Participants
Three hundred three colorectal cancer (CRC) survivors in Northern California were surveyed 2–5 years post-diagnosis.
Measurements
Specialty of physician seen most often [primary care physician (PCP), oncologist, surgeon, or gastroenterologist]; other physician specialties seen; patient characteristics; content of visits; patient-centered quality of follow-up care (communication, coordination, nursing, and staff interactions).
Main Results
A minority (16%) of CRC survivors reported that the doctor they most often saw for follow-up cancer care was a PCP, while 60% saw an oncologist. Many CRC survivors (40%) saw >1 physician for follow-up cancer care. Survivors most often seen by PCPs were more likely to have three or more medical comorbidities (70% vs. 51%, p = 0.012) than survivors seen by subspecialty physicians. Survivors seen by PCPs were less likely to report seeing a doctor for medical tests and more likely to report discussing disease prevention (82% vs. 64%, p = 0.012) or diet (70% vs. 48%, p = 0.005) with their doctor. There were no significant specialty differences in patient-centered quality of follow-up cancer care.
Conclusions
Cancer survivors’ assessment of the quality of care was similar across specialties, while the content of follow-up cancer care varied by physician specialty. These findings provide important information about the potential value of primary care and the need for coordination when delivering care to CRC survivors.
KEY WORDS: cancer survivorship, colorectal cancer, primary care, health services research, quality assessment, patient-centered care
INTRODUCTION
Cancer survivors in general have multiple care needs after primary treatment of their cancer, including (1) management of symptoms resulting from disease or treatment, (2) monitoring for late effects of treatment, (3) follow-up tests to monitor for recurrence, and (4) health promotion1. Symptoms occur often among about one-third of colorectal cancer (CRC) survivors2. Late or long-term side effects of CRC treatment may include fecal leakage, diarrhea3, pain4, intestinal obstruction, and stricture. Follow-up surveillance tests and recommendations for CRC survivors during the first 3 years after surgery include regular history and physicals, serum carcinoembryonic antigen tests, computed tomography, and colonoscopy5. Health promotion behaviors have also become increasingly important for survivors as evidence about the benefits of appropriate diet6 and exercise7 accumulates. Our study responds to the need for better understanding of how often the multiple needs of CRC survivors are met during the course of follow-up cancer care.
It has been asserted that adult cancer survivors predominantly receive follow-up cancer care from oncologists with a focus on surveillance for recurrence8. According to a SEER-Medicare study among CRC survivors using Medicare claims data, 7.5% reported seeing an oncologist only, 35% seeing both a primary care physician (PCP) and oncologist, and 45.7% seeing a PCP only9. However, little is known about what types of physicians are seen most often for the specific purpose of follow-up cancer care, as well as the degree to which physicians address the multiple needs of CRC survivors.
Multiple types of physicians may provide follow-up cancer care for a CRC survivor after primary treatment, including PCPs, oncologists, surgeons, and gastroenterologists. As recommended by the Institute of Medicine (IOM)1, the physician who most often provides follow-up cancer care may address the prevention and health promotion needs of the patient, as well as cancer-directed follow-up tests. Previous randomized controlled trials outside the US have compared primary care and specialty-led follow-up care in breast10,11 and colorectal cancer12 and found equivalent outcomes, including quality of life, time to diagnosis of recurrence, and patient satisfaction.
Based on these previous findings, we set out to determine what types of physicians were seen most often by CRC survivors for cancer-related follow-up care and to examine the association between physician specialty and the content of CRC follow-up visits. We hypothesized that there would be no difference across physician specialties in (1) the content or (2) the quality of follow-up cancer care. While patients have been identified as a key source of information for assessing the quality of care13,14, such assessments within the context of cancer survivorship are rare. To better understand cancer survivors’ perspectives, we tested our hypotheses using survey data from the Assessment of Patients’ Experience of Cancer Care (APECC) study.
METHODS
Sample and Data Collection: The APECC study was a population-based Surveillance Epidemiology and End Results (SEER) study conducted in collaboration with researchers at the National Cancer Institute and Northern California Cancer Center (NCCC). The Greater Bay Area Cancer Registry provided the sampling frame, which gathers information on all cancers diagnosed in a nine-county area. Data were collected between April 2003 and November 2004 through a cross-sectional survey mailed to a representative sample of colorectal, leukemia, and bladder cancer survivors who were diagnosed 2–5 years before being surveyed (diagnosis dates ranged from June 1, 1999 to May 31, 2001). Study procedures were approved by NCCC’s Institutional Review Board. In this study, we focused on the subsample of CRC survivors only.
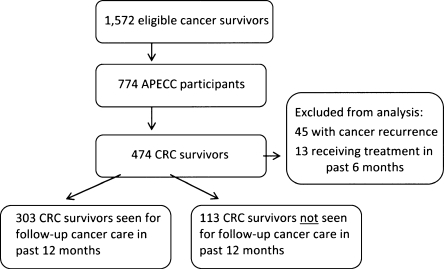
The population recruited into APECC and included in our study is described in Figure 1. The patient survey assessed whether the survivors had received any cancer-related follow-up care in the past year. Among CRC survivors who had not, we reported patient characteristics alone (n = 113); among CRC survivors who had received cancer care follow-up (n = 303), we also reported physician specialty, the content, and patient-centered quality of follow-up care as described below.
Figure 1.
Population recruited into the Assessment of Patients’ Experience of Cancer Care (APECC) study.
Measures Patient characteristics included sociodemographics: age, race/ethnicity, gender, education, family income, and insurance (no insurance or public insurance vs. private insurance or private and public insurance). Clinical characteristics included American Joint Commission on Cancer (AJCC) stage, time since diagnosis, and number of medical comorbidities. The following self-reported comorbidities were measured (yes/no) and combined into an index (0–18): myocardial infarction, angina, heart failure, stroke, hypertension, chronic lung disease, diabetes, kidney disease, liver disease, osteoporosis, depression or anxiety, arthritis, inflammatory bowel disease, HIV, dementia, peptic ulcer disease, thyroid disease, and deep venous thrombosis.
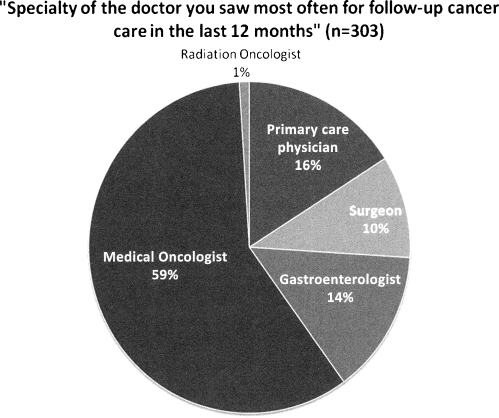
Physician Specialty Survivors were asked the following question: “What is the specialty of the doctor you saw most often for follow-up cancer care in the last 12 months?” Response options included primary care physician (internal medicine or family practice), medical oncologist/hematologist, radiation oncologist, surgeon, or gastroenterologist (GI). Because only 1% of the sample saw a radiation oncologist, we combined them with the medical oncologist/hematologist group into an overall category of oncologists. Survivors were later asked, “In the last 12 months, in addition to your follow-up care doctor, did you see any other doctor for cancer-related issues or problems?” The number of other doctors seen and their specialty were also measured.
Content of Follow-up Care Survivors were asked about the length of the relationship with the doctor they saw most often for follow-up cancer care and the number of visits to this doctor in the last year. We also assessed the reasons for follow-up cancer care with a doctor in the past year including: (1) discuss and/or treat symptoms and side effects, (2) receive follow-up medical tests to check for signs of cancer or other medical problems, and (3) receive a physical examination. For health promotion activities, survivors were asked, using a three-point response scale (yes definitely, yes somewhat, no), whether their cancer follow-up doctor, or someone from that doctor’s office, engaged in the following activities in the last year: (1) talk with you about specific things you could do to improve your health or prevent illness, (2) give you the help you wanted to make changes in your habits or lifestyle that would improve your health or prevent illness, (3) talk with you about how much or what kind of foods you eat, or (4) talk with you about how much or what kind of exercise you get. Dichotomous (yes/no) indicators were created for each of these questions.
Patient-centered Quality of Follow-up Care We assessed cancer survivors’ perceptions of the quality of their follow-up cancer care in several domains by asking them to report the frequency (never, sometimes, usually, always) of certain key behaviors within the context of their follow-up cancer care in the past year. These domains (Appendix 1) included the following: (1) physician communication (ten items, Cronbach’s alpha = 0.93); (2) care coordination (two items, Cronbach’s alpha = 0.65); (3) nursing care (two items, Cronbach’s alpha = 0.82); (4) interactions with office staff (two items, Cronbach’s alpha = 0.90). Overall scores were created for each of the above domains by taking a mean of the score from all items in that domain. We also assessed survivors’ overall ratings of the quality of their follow-up care using two items: (1) “Overall, how would you rate your follow-up care doctor?” on a response scale of 0–10; (2) “Based on your interactions with your doctor, the nurses, and other staff, how would you rate the quality of care you received from your follow-up care doctor’s office or clinic in the last 12 months?” on a response scale of poor, fair, good, very good, and excellent. Scores for all quality measures were linearly transformed to a 0–100 format where 100 reflected optimal quality of care.
The majority of items were adopted from existing instruments assessing patient experiences with care13–16; a few items were newly created for the APECC study. All items underwent cognitive and pilot testing prior to final data collection. Details on the exact wording, source, and score distribution of each item are available at http://outcomes.cancer.gov/surveys/apecc/apecc_codebook.pdf.
Analyses Bivariate associations of being seen for any cancer care follow-up (yes/no) with patient characteristics were evaluated with chi-squared tests. Among survivors being seen for cancer care follow-up, bivariate associations of physician specialty with (1) patient characteristics, (2) reasons for follow-up care visits, and (3) health promotion activities were evaluated with chi-squared and t-tests. Bivariate associations first modeled specialty as a four-category variable; if these overall tests were significant, then subset analyses were performed (not shown in tables) modeling specialty as a two-category variable: primary care vs. subspecialty (oncology, surgery, or gastroenterology). Multivariable logistic regression models tested the associations of specialty with (1) reasons for follow-up care visits and (2) health promotion activities, while adjusting for patient characteristics. Multivariable linear regression models tested associations of specialty with communication, care coordination, nursing care, staff at the doctor’s office, and ratings of overall quality of care, adjusting for patient characteristics. Adjusted means were reported for each quality score.
RESULTS
CRC Survivor Population
Sociodemographic and clinical characteristics of the overall population are described in Table 1. More than a quarter (27%) of cancer survivors reported not being seen for follow-up cancer care at all. Comparing the survivors who saw a doctor for follow-up cancer care to those who did not, there were significant differences in mean age (64.0 vs. 68.2 years, p = 0.002), the proportion of women (51% vs. 39%, p = 0.03), private insurance (84% vs. 71%, p = 0.003), and stage I disease (51% vs. 29%, p < 0.001).
Table 1.
Patient Characteristics of Colorectal Cancer Survivors
| Cancer care follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Specialty of doctor seen most often for follow-up cancer care | |||||||
| Patient characteristics | Primary care (n = 50) | Oncology (n = 183) | Surgery (n = 29) | GI (n = 41) | Any physician (n = 303) | None (n = 113) | p value* |
| Sociodemographic | |||||||
| Age | |||||||
| <50 | 8% | 14% | 10% | 17% | 13% | 6% | |
| 50–64 | 30% | 39% | 45% | 29% | 37% | 35% | |
| 65–74 | 38% | 27% | 28% | 24% | 28% | 25% | |
| ≥75 | 24% | 20% | 17% | 29% | 22% | 34% | 0.588 |
| Female | 38% | 55% | 38% | 59% | 51% | 39% | 0.064 |
| Race/ethnicity | |||||||
| White | 58% | 73% | 66% | 73% | 70% | 69% | |
| Non-white | 42% | 27% | 34% | 27% | 30% | 31% | 0.187 |
| Total family income | |||||||
| <$40,000 | 43% | 31% | 30% | 28% | 33% | 47% | |
| $40,000–$99,999 | 34% | 42% | 44% | 50% | 42% | 40% | |
| ≥$100,000 | 23% | 27% | 26% | 22% | 25% | 13% | 0.755 |
| Education | |||||||
| High school or less | 16% | 22% | 14% | 24% | 20% | 27% | |
| Some college | 32% | 31% | 34% | 24% | 30% | 33% | |
| College or more | 52% | 47% | 52% | 51% | 49% | 40% | 0.863 |
| Insurance status | |||||||
| None or public | 24% | 13% | 24% | 12% | 16% | 29% | |
| Private | 76% | 87% | 76% | 88% | 84% | 71% | 0.154 |
| Clinical | |||||||
| Years since diagnosis | |||||||
| 2–3 years | 10% | 19% | 14% | 17% | 17% | 18% | |
| 3–4 years | 50% | 50% | 72% | 51% | 52% | 48% | |
| 4–5 years | 40% | 31% | 14% | 32% | 31% | 35% | 0.209 |
| AJCC Stage | |||||||
| Stage I | 38% | 17% | 45% | 63% | 29% | 51% | |
| Stage II | 40% | 38% | 34% | 29% | 37% | 32% | |
| Stage III | 22% | 42% | 21% | 7% | 32% | 15% | |
| Stage IV | 0% | 3% | 0% | 0% | 2% | 2% | <0.001 |
| Number of comorbidities | |||||||
| 0–2 | 30% | 47% | 48% | 61% | 46% | 44% | |
| ≥3 | 70% | 53% | 52% | 39% | 54% | 56% | 0.030 |
*Bivariate associations of specialty (four-category variable) with patient characteristics were evaluated with chi-squared tests
Physician Specialty and Patient Characteristics
The majority of CRC survivors identified an oncologist (60%) as the “specialty of the doctor you saw most often for follow-up cancer care in the last 12 months” (Fig. 2). Smaller proportions of survivors identified a PCP (16%), gastroenterologist (14%), or surgeon (10%) as the type of physician they saw most often. Almost half of CRC survivors (40%) reported seeing another physician for cancer-related issues (Table 2). More than half (57%) saw only one other physician, most commonly a gastroenterologist (46%).
Figure 2.
Distribution of patients by physician specialty.
Table 2.
Number of Other Doctors Seen for Cancer-related Issues and Their Specialty
| Specialty of doctor seen most often for follow-up cancer care | |||||
|---|---|---|---|---|---|
| Primary care (n = 50) | Oncology (n = 183) | Surgery (n = 29) | GI (n = 41) | Any physician (n = 303) | |
| Any other doctor for cancer-related issues | 52% (26) | 38% (70) | 35% (10) | 34% (14) | 40% (120) |
| Number of other doctors | |||||
| 1 | 46% | 61% | 67% | 50% | 57% |
| 2 | 31% | 23% | 11% | 36% | 25% |
| 3 | 15% | 10% | 22% | 14% | 13% |
| 4 | 4% | 6% | 0% | 0% | 4% |
| 5 | 4% | 0% | 0% | 0% | 1% |
| Specialty of other doctors seen for cancer-related issues | |||||
| Primary care | 0% | 22% | 30% | 0% | 16% |
| Medical oncologist/hematologist | 13% | 3% | 0% | 0% | 4% |
| Radiation oncologist | 0% | 2% | 0% | 7% | 2% |
| Surgeon | 9% | 8% | 30% | 0% | 9% |
| Gastroenterologist | 44% | 52% | 20% | 36% | 46% |
| Urologist | 4% | 6% | 10% | 0% | 5% |
| Cardiologist | 9% | 0% | 0% | 14% | 4% |
| Pulmonologist | 0% | 0% | 0% | 7% | 1% |
| Neurologist | 4% | 3% | 10% | 7% | 4% |
| Dermatologist | 13% | 2% | 0% | 29% | 7% |
| Psychiatrist | 4% | 2% | 0% | 0% | 2% |
Sociodemographic characteristics did not differ significantly among CRC survivors who most often saw any type of physician specialty, but clinical characteristics were significantly different (Table 1). A large majority of survivors seen primarily by PCPs (78%), surgeons (79%), or gastroenterologists (92%) had stage I or II disease, whereas oncologists were almost equally likely to see survivors with stage I or II (55%) and stage III or IV (45%) disease (p = 0.03). CRC survivors who primarily saw PCPs were significantly more likely to have three or more medical conditions than survivors who most often saw any subspecialist (70% vs. 51%, p = 0.012).
Content of Follow-up Care
Most patient-physician relationships in this cohort were of greater than 1 year’s duration (89%, Table 3). PCPs were more likely to have relationships of greater than 4 years’ duration than subspecialty physicians (36% vs. 3%, p < 0.001). The number of visits in the past year also varied by physician specialty (p < 0.001).
Table 3.
Physician Specialty Differences in Content of Follow-up Care
| Specialty of doctor seen most often for follow-up cancer care | ||||||
|---|---|---|---|---|---|---|
| Any physician (n = 303) | Primary care (n = 50) | Oncology (n = 183) | Surgery (n = 29) | GI (n = 41) | p value* | |
| Duration & frequency | ||||||
| Length of relationship | ||||||
| < 1 year | 11% | 16% | 5% | 14% | 27% | |
| 1–4 years | 81% | 48% | 91% | 86% | 71% | |
| ≥5 years | 8% | 36% | 4% | 0% | 2% | <0.001 |
| Number of visits | ||||||
| 1 | 27% | 36% | 13% | 38% | 73% | |
| 2 | 34% | 22% | 41% | 34% | 17% | |
| ≥3 | 39% | 42% | 46% | 28% | 10% | <0.001 |
| Reasons for visits | ||||||
| Symptoms/side effects | 7% | 14% | 6% | 0% | 7% | 0.099 |
| Follow-up tests | 85% | 68% | 92% | 79% | 83% | <0.001 |
| Physical exam | 40% | 58% | 39% | 34% | 27% | 0.017 |
| Health promotion activities | ||||||
| Discuss disease prevention | 67% | 82% | 64% | 62% | 63% | 0.095 |
| Help with lifestyle change | 67% | 83% | 65% | 69% | 52% | 0.041 |
| Discuss diet | 52% | 70% | 51% | 39% | 41% | 0.017 |
| Discuss exercise | 64% | 78% | 62% | 57% | 59% | 0.134 |
*Bivariate associations of specialty (four-category variable) with content of follow-up care were evaluated with chi-squared tests
Few CRC survivors reported seeing physicians for symptoms or side effects (7%) within the prior year (Table 3). Survivors who more often saw a PCP for follow-up cancer care than oncologists, surgeons, or gastroenterologists were significantly less likely to see a doctor for “follow-up medical tests” (68% vs. 89%, p < 0.001) and significantly more likely to see a doctor to receive a physical examination (58% vs. 36%, p = 0.004). In multivariable regression models adjusting for patient characteristics, CRC survivors who most often saw oncologists were still significantly more likely than those who saw PCPs to report seeing a doctor for follow-up tests and less likely to receive a physical exam (Table 4).
Table 4.
Association of Physician Specialty and Patient Characteristics with Reasons for Follow-up Care Visits
| Reasons for follow-up care visits* | |||
|---|---|---|---|
| Symptoms/side effects | Follow-up tests | Physical exam | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Specialty (ref. PCP) | |||
| Oncologist | 0.71 (0.23–2.23) | 4.21 (1.74–10.21) | 0.45 (0.23–0.91) |
| Surgeon | NA | 1.64 (0.52–5.14) | 0.33 (0.12–0.88) |
| Gastroenterologist | 0.85 (0.18–4.05) | 1.83 (0.62–5.47) | 0.24 (0.09–0.62) |
| Gender (ref. male) | |||
| Female | 0.53 (0.18–1.53) | 1.72 (0.80–3.69) | 0.74 (0.45–1.23) |
| Age (years) | 0.98 (0.93–1.02) | 0.96 (0.92–0.99) | 1.00 (0.98–1.03) |
| Race/ethnicity (ref. white) | |||
| Non-white | 2.55 (.86–7.51) | 0.43 (0.20–0.93) | 0.96 (0.55–1.69) |
| Education (ref. high school) | |||
| Some college | 1.86 (0.39–8.76) | 0.96 (0.36–2.56) | 1.34 (0.63–2.85) |
| College | 1.75 (0.39–7.74) | 1.39 (0.55–3.51) | 2.27 (1.13–4.55) |
| Insurance (ref. no insurance or public insurance) | |||
| Private insurance | 0.47 (0.12–1.59) | 0.51 (0.18–1.46) | 1.06 (0.50–2.24) |
| Cancer stage (ref. stage I/II) | |||
| Stage III/IV | 0.44 (0.13–1.50) | 1.37 (0.55–3.38) | 0.96 (0.55–1.67) |
| Years since diagnosis | 2.10 (0.96–4.57) | 1.23 (0.72–2.11) | 0.98 (0.67–1.42) |
| Comorbidity | 1.24 (0.96–1.61) | 0.92 (0.74–1.13) | 0.88 (0.75–1.03) |
*Multivariable logistic regression models tested the associations between reasons for follow-up care visits and physician specialty, gender, age (continuous variable), race/ethnicity, education, insurance, cancer stage; years since diagnosis and comorbidity (both continuous variables)
In terms of health promotion activities (Table 3), CRC survivors who most often saw PCPs for follow-up cancer care were significantly more likely than survivors who saw subspecialty physicians to report that their follow-up doctor helped with lifestyle (83% vs. 63%, p = 0.015) and discussed diet (70% vs. 48%, p = 0.005). In models adjusting for patient characteristics, oncologists were significantly less likely than PCPs to discuss disease prevention, provide help with lifestyle, and discuss diet (Table 5).
Table 5.
Association of Physician Specialty and Patient Characteristics with Health Promotion Activities
| Health promotion activities* | ||||
|---|---|---|---|---|
| Discuss prevention | Help with lifestyle | Discuss diet | Discuss exercise | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Specialty (ref. PCP) | ||||
| Oncologist | 0.41 (0.18–0.92) | 0.32 (0.12–0.84) | 0.44 (0.21–0.91) | 0.53 (0.24–1.16) |
| Surgeon | 0.36 (0.12–1.04) | 0.40 (0.10–1.59) | 0.26 (0.10–0.72) | 0.38 (0.13–1.09) |
| Gastroenterologist | 0.40 (0.15–1.07) | 0.23 (0.07–0.72) | 0.32 0.13–0.81) | 0.51 (0.20–1.34) |
| Gender (ref. male) | ||||
| Female | 0.84 (0.50–1.41) | 0.54 (0.28–1.05) | 0.52 (0.31–0.86) | 0.59 (0.35–0.99) |
| Age (years) | 1.01 (0.99–1.03) | 1.00 (0.97–1.03) | 1.01 (0.98–1.03) | 1.01 (0.99–1.04) |
| Race/ethnicity (ref. white) | ||||
| Non-white | 1.19 (0.67–2.11) | 0.95 (0.47–1.91) | 1.14 (0.66–1.99) | 1.74 (0.96–3.14) |
| Education (ref. high school) | ||||
| Some college | 1.17 (0.57–2.43) | 0.84 (0.34–2.07) | 0.67 (0.33–1.36) | 1.23 (0.58–2.60) |
| College | 1.00 (0.51–1.96) | 0.40 (0.17–0.95) | 0.57 (0.29–1.12) | 0.64 (0.32–1.28) |
| Insurance (ref. no insurance or public insurance) | ||||
| Private insurance | 1.22 (0.58–2.55) | 1.18 (0.46–2.99) | 1.37 (0.67–2.80) | 0.81 (0.37–1.74) |
| Cancer stage (ref. stage I/II) | ||||
| Stage III/IV | 0.89 (0.51–1.56) | 1.17 (0.57–2.40) | 1.09 (0.63–1.87) | 1.12 (0.63–1.96) |
| Years since diagnosis | 0.89 (0.61–1.30) | 0.65 (0.40–1.04) | 0.76 (0.52–1.10) | 0.83 (0.57–1.21) |
| Comorbidity | 1.01 (0.86–1.19) | 1.12 0.92–1.37) | 1.05 (0.90–1.22) | 1.07 (0.91–1.27) |
*Multivariable logistic regression models tested the associations between health promotion activities and physician specialty, gender, age (continuous variable), race/ethnicity, education, insurance, cancer stage, years since diagnosis, and comorbidity (both continuous variables)
Patient-centered Quality of Follow-up Care
There were no significant differences in the patient-centered quality of follow-up care among cancer survivors who saw different physician specialties (Table 6). Specifically, there were no significant specialty differences in the perceived quality of communication, care coordination, nursing care, or staff at the doctor’s office. There were also no significant differences in the perceived overall quality of care. Among sociodemographic and clinical characteristics, only older patient age was significantly associated with higher patient-centered quality of follow-up care for any domain of quality (p < 0.04 for all models).
Table 6.
Physician Specialty Differences† in Patient-centered Quality of Follow-up Care
| Scores and ratings* | Adjusted means | |
|---|---|---|
| Communication score | Primary care | 92.6 |
| Oncology | 92.7 | |
| Surgery | 91.9 | |
| Gastroenterology | 92.6 | |
| Coordination score | Primary care | 91.4 |
| Oncology | 91.2 | |
| Surgery | 90.6 | |
| Gastroenterology | 90.5 | |
| Nursing care score | Primary care | 92.8 |
| Oncology | 92.9 | |
| Surgery | 93.0 | |
| Gastroenterology | 93.4 | |
| Office staff score | Primary care | 90.5 |
| Oncology | 90.8 | |
| Surgery | 91.5 | |
| Gastroenterology | 92.8 | |
| Follow-up doctor | Primary care | 88.6 |
| rating | Oncology | 90.1 |
| Surgery | 90.3 | |
| Gastroenterology | 92.9 | |
| Follow-up doctor’s office | Primary care | 87.1 |
| rating | Oncology | 88.0 |
| Surgery | 88.2 | |
| Gastroenterology | 90.2 | |
*Multivariable linear regression models tested the associations between patient-centered quality of follow-up care and physician specialty, gender, age (continuous variable), race/ethnicity, education, insurance, cancer stage, years since diagnosis, and comorbidity (both continuous variables)
†Physician specialty was not statistically significant for any scale or rating
DISCUSSION
We conducted a population-based study of the follow-up cancer care received by CRC survivors 2–5 years after initial diagnosis. The majority of patients seen for follow-up cancer care in this study reported most often seeing an oncologist, while a minority reported most often seeing a PCP (16%). In a SEER-Medicare study among CRC survivors using administrative claims, 46% saw only a PCP9, although Snyder et al. measured visits to all doctors, not those seen for follow-up cancer care alone. The methodologies of the APECC patient survey and SEER-Medicare linked administrative data are largely complementary. APECC reports the survivor’s perception of the quality of care received from the doctor seen most often for follow-up cancer care specifically, while SEER-Medicare provides data about health-care utilization overall, but not the reason or perceived quality of the visits.
Patients were infrequently seen for symptoms or side effects (7%). Given the higher prevalence of symptoms in the CRC survivor population (31%)2, physicians seeing CRC survivors in follow-up may need to better ascertain patient symptoms. CRC survivors who most often saw PCPs were less likely than those who saw oncologists to report seeing a doctor for follow-up testing, even after adjusting for cancer stage and years since diagnosis. This contrast may be explained by different professional guidelines being accessed by different physician specialties. The American Society of Clinical Oncology5 has guidelines related to CRC surveillance, but the US Preventive Services Task Force has not addressed the topic of cancer follow-up testing, a decision that may be worth revisiting.
On the other hand, PCPs were more likely than oncologists, and other subspecialty physicians, to discuss prevention, help with lifestyle, and discuss diet. Our findings related to preventive practices are similar to complementary data in SEER-Medicare, demonstrating that CRC survivors seen only by a PCP were more likely to receive influenza vaccination, cholesterol screening, and bone densitometry compared to survivors seen only by an oncologist9,17. Overall, it appears as though neither primary care nor subspecialty physicians necessarily adjusted their practice styles to meet the needs of cancer survivors in a uniform manner, but instead, “played to type.”
The specialty of physicians seen by survivors was more important than patient characteristics in predicting the content of follow-up care they received, with only a few exceptions (Tables 4 and 5), for example, non-white patients were less likely to report being seen for follow-up tests. The clinical characteristics of patients were consistent with the clinical expertise of the specialties seen. Oncologists are trained to provide follow-up care to survivors with more advanced cancer and saw the majority of such patients. Yet it is worth noting that a non-trivial proportion of the overall sample with higher stage CRC reported seeing PCPs, or no one, for cancer care follow-up. PCPs may have more regular experience with the management of multiple, chronic diseases, and survivors seen by PCPs were more likely to have multiple comorbidities. Because overall median survival for patients with recurrent or metastatic CRC has increased significantly in the past several years, finding recurrences through active surveillance has taken on new importance18. Greater surveillance of appropriate patients is thus an area for potential quality improvement.
The patient experience of the quality of follow-up cancer care among PCP and subspecialty physicians was largely the same across the domains of communication, care coordination, nursing care, or staff at the doctor’s office. Overall, the quality scores were relatively high. While prior studies of the quality of care among CRC survivors have largely focused upon the technical quality of care9,17,19, our study is one of the first to focus upon the perceived quality of care received by cancer survivors using patient-centered measures20.
Limitations Selection bias may have influenced our observational results related to quality. However, our findings regarding perceived quality are similar to prior clinical trials that randomized cancer survivors to be seen by PCPs or subspecialty physicians. Our study also does not measure the health promotion or quality of care received from doctors (and offices) besides the doctor whom respondents saw most often for their follow-up cancer care; furthermore, this doctor may not necessarily be the doctor they saw most often overall. However, the strength of this approach is its specificity: the follow-up cancer care described can be directly attributed to the type of physician identified, with the exception of the reason for follow-up visits (symptoms, follow-up tests, or physical examinations).
A primary role for the PCP in follow-up cancer care appears to be uncommon. Nonetheless, interventions aimed at improving any gaps in the quality of survivorship care should take into account the apparent ability of the PCP, along with nursing and office staff, to deliver a relatively high-quality patient experience in terms of both communication and care coordination, even to complex patients with competing medical conditions. Different types of follow-up doctors appeared to deliver different types of services: CRC survivors most often seen by oncologists were more likely to receive follow-up tests, while PCPs were more likely to perform health promotion. A shared care model builds upon routine, regular communication between primary care and subspecialty physicians8, and may capitalize upon the complementary strengths of different types of physicians. A substantial proportion of CRC survivors saw more than one physician for cancer-related issues or problems (40%), and some survivors saw many more (up to 5); these patterns of care delivery highlight the need for care coordination. Shared care models should be considered for future research and demonstration projects in medical homes or integrated delivery systems in the US to further understand the potential value of primary care and need for care coordination when delivering follow-up care to CRC survivors.
Acknowledgments
Dr. Haggstrom is supported by VA HSR&D Career Development Award CD207016-2. This research was funded by NCI contract N01-PC-35136 at the NCCC. Preliminary results of the paper were presented at the American Society of Clinical Oncology Annual Meeting, May 2008. This work represents the opinion of the authors and cannot be construed to represent the opinion of the National Cancer Institute, the Department of Veterans Affairs, or the Federal Government.
Conflict of Interest None disclosed.
Appendix 1
Physician Communication
In the last 12 months, how often did your follow-up care doctor listen carefully to you? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor explain things in a way you could understand? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor show respect for what you had to say? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor encourage you to ask all the cancer-related questions you had? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor answer your cancer-related questions to your satisfaction? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor make sure that you understood all the information he or she gave you? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did your follow-up care doctor spend enough time with you? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did you feel rushed by your follow-up care doctor?
In the last 12 months, how often did your follow-up care doctor give you as much cancer-related information as you wanted? (Never, Sometimes, Usually, Always)
In the last 12 months, how often did you leave your follow-up care doctor’s office or clinic with unanswered questions related to your cancer? (Never, Sometimes, Usually, Always)
Care Coordination
In the last 12 months, how often did your follow-up care doctor seem informed and up-to-date about the care you received from any other doctors or health professionals you saw for cancer-related issues or problems? (Never, Sometimes, Usually, Always)
In the last 12 months, in your opinion, how often did your follow-up care doctor, the nurses, and other staff at your follow-up care doctor’s office or clinic seem to work well together as a team? (Never, Sometimes, Usually, Always)
Nursing Care
In the last 12 months, how often did nurses at your follow-up care doctor’s office or clinic treat you with courtesy and respect? (Never, Sometimes, Usually, Always)
In the last 12 months, how often were the nurses at your follow-up care doctor’s office or clinic as helpful as you thought they should be? (Never, Sometimes, Usually, Always)
Interactions with Office Staff
In the last 12 months, how often did office staff (such as receptionists and other personnel at the front office) at your follow-up care doctor’s office or clinic treat you with courtesy and respect? (Never, Sometimes, Usually, Always)
In the last 12 months, how often was office staff (such as receptionists and other personnel at the front office) at your follow-up care doctor’s office or clinic as helpful as you thought they should be? (Never, Sometimes, Usually, Always)
References
- 1.Hewitt M, Ganz P. From cancer patient to cancer survivor - lost in transition: An American Society of Clinical Oncology and Institute of Medicine Symposium. Washington, DC: The National Academies Press; 2006.
- 2.Schneider EC, Malin JL, Kahn KL, Ko CY, Adams J, Epstein AM. Surviving colorectal cancer: patient-reported symptoms 4 years after diagnosis. Cancer. 2007;110(9):2075–82. [DOI] [PubMed]
- 3.Sprangers MA, Taal BG, Aaronson NK, te Velde A. Quality of life in colorectal cancer. Stoma vs. nonstoma patients. Dis Colon Rectum. 1995;38(4):361–9. [DOI] [PubMed]
- 4.Rauch P, Miny J, Conroy T, Neyton L, Guillemin F. Quality of life among disease-free survivors of rectal cancer. J Clin Oncol. 2004;22(2):354–60. [DOI] [PubMed]
- 5.Desch CE, Benson AB 3rd, Somerfield MR, et al. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol. 2005;23(33):8512–9. [DOI] [PubMed]
- 6.Meyerhardt JA, Niedzwiecki D, Hollis D, et al. Association of dietary patterns with cancer recurrence and survival in patients with stage III colon cancer. Jama. 2007;298(7):754–64. [DOI] [PubMed]
- 7.Courneya KS, Friedenreich CM, Quinney HA, Fields AL, Jones LW, Fairey AS. A randomized trial of exercise and quality of life in colorectal cancer survivors. Eur J Cancer Care (Engl). 2003;12(4):347–57. [DOI] [PubMed]
- 8.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24(32):5117–24. [DOI] [PubMed]
- 9.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Trends in follow-up and preventive care for colorectal cancer survivors. J Gen Intern Med. 2008;23(3):254–9. [DOI] [PMC free article] [PubMed]
- 10.Grunfeld E, Levine MN, Julian JA, et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol. 2006;24(6):848–55. [DOI] [PubMed]
- 11.Grunfeld E, Fitzpatrick R, Mant D, et al. Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: results from a randomized controlled trial. Br J Gen Pract. 1999;49(446):705–10. [PMC free article] [PubMed]
- 12.Wattchow DA, Weller DP, Esterman A, et al. General practice vs surgical-based follow-up for patients with colon cancer: randomised controlled trial. Br J Cancer. 2006;94(8):1116–21. [DOI] [PMC free article] [PubMed]
- 13.Ayanian JZ, Zaslavsky AM, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23(27):6576–86. [DOI] [PubMed]
- 14.Hays RD, Shaul JA, Williams VS, et al. Psychometric properties of the CAHPS 1.0 survey measures. Consumer Assessment of Health Plans Study. Med Care. 1999;37(3 Suppl):MS22–31. [DOI] [PubMed]
- 15.Montgomery JE, Irish JT, Wilson IB, et al. Primary care experiences of medicare beneficiaries, 1998 to 2000. J Gen Intern Med. 2004;19(10):991–8. [DOI] [PMC free article] [PubMed]
- 16.Rodriguez HP, Rogers WH, Marshall RE, Safran DG. The effects of primary care physician visit continuity on patients’ experiences with care. J Gen Intern Med. 2007;22(6):787–93. [DOI] [PMC free article] [PubMed]
- 17.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26(7):1073–9. [DOI] [PubMed]
- 18.Grothey A, Sargent D, Goldberg RM, Schmoll HJ. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil-leucovorin, irinotecan, and oxaliplatin in the course of treatment. J Clin Oncol. 2004;22(7):1209–14. [DOI] [PubMed]
- 19.Earle CC, Neville BA. Under use of necessary care among cancer survivors. Cancer. 2004;101(8):1712–9. [DOI] [PubMed]
- 20.Arora NK. Importance of patient-centered care in enhancing patient well-being: a cancer survivor’s perspective. Qual Life Res. in press. [DOI] [PubMed]