Abstract
Hippocampal integrity is essential for cognitive functions. On the other hand, induction of metallothionein (MT) by ZnSO4 and its role in neuroprotection has been documented. The present study aimed to explore the effect of MT induction on carmustine (BCNU)-induced hippocampal cognitive dysfunction in rats. A total of 60 male Wistar albino rats were randomly divided into four groups (15/group): The control group injected with single doses of normal saline (i.c.v) followed 24 h later by BCNU solvent (i.v). The second group administered ZnSO4 (0.1 µmol/10 µl normal saline, i.c.v, once) then BCNU solvent (i.v) after 24 h. Third group received BCNU (20 mg/kg, i.v, once) 24 h after injection with normal saline (i.c.v). Fourth group received a single dose of ZnSO4 (0.1 µmol/10 µl normal saline, i.c.v) then BCNU (20 mg/kg, i.v, once) after 24 h. The obtained data revealed that BCNU administration resulted in deterioration of learning and short-term memory (STM), as measured by using radial arm water maze, accompanied with decreased hippocampal glutathione reductase (GR) activity and reduced glutathione (GSH) content. Also, BCNU administration increased serum tumor necrosis factor-alpha (TNFα), hippocampal MT and malondialdehyde (MDA) contents as well as caspase-3 activity in addition to histological alterations. ZnSO4 pretreatment counteracted BCNU-induced inhibition of GR and depletion of GSH and resulted in significant reduction in the levels of MDA and TNFα as well as the activity of caspase-3. The histological features were improved in hippocampus of rats treated with ZnSO4 + BCNU compared to only BCNU-treated animals. In conclusion, MT induction halts BCNU-induced hippocampal toxicity as it prevented GR inhibition and GSH depletion and counteracted the increased levels of TNFα, MDA and caspase-3 activity with subsequent preservation of cognition.
Key words: metallothionein, carmustine, hippocampus, learning, memory, oxidative stress, TNFα, apoptosis
Introduction
It is increasingly apparent that neurological disorders including disruption of brain functions associated with the systemic delivery of chemotherapeutic agents used for treatment of central nervous system (CNS) and non-CNS tumors.1,2 There is a growing evidence that standard-dose chemotherapy can impact cognitive function.3 Previous studies suggested that 18% of all breast cancer patients receiving standard-dose chemotherapy show cognitive defects on post-treatment evaluation,4 and such problems were reported in more than 30% of patients examined two years after treatment with high-dose chemotherapy.5,6 In addition, Vardy and Tannock7 have reported impaired cognitive functions during treatment of solid brain tumors in animal models and in humans. It has been concluded that administration of methotrexate and 5-FU in combination induced impairments in tests of spatial memory and other cognitive tasks in mice.8 Also, a single dose of cyclophosphamide produced a transient acute memory impairment in mice.9 Moreover, adriamycin has been demonstrated to increase oxidative stress in the brain, which may lead to cell dysfunction or cell death and thus contribute to cognitive dysfunction.10 Furthermore, it has been reported that long-term exposure to 13-cis-retinoic acid, which is often used in chemotherapy regimens, was associated with decreased neurogenesis and cell proliferation in the hippocampus and subventricular zone and impaired spatial learning and memory in young and adult mice.11
Vardy et al.12 reported that the etiology of cognitive impairment after chemotherapy remains unknown although a number of mechanisms have been postulated.13 Candidate mechanisms include: direct neurotoxic effects (e.g., injury to neurons or surrounding cells, altered neurotransmitter levels),14 oxidative stress and DNA damage,15 immune dysregulation and/or release of cytokines13,16 and blood clotting in small CNSvessels.12
Carmustine (BCNU) is an alkylating agent used in the treatment of brain tumors, myeloma, and both Hodgkin and non-Hodgkin lymphoma.17 The ability of BCNU to cross blood-brain barrier (BBB) may explain its neurotoxicity.18 Studies on the incidence and the mechanisms of cognitive dysfunction after BCNU administration are rare. Among these studies, Dietrich et al.17 explained that the cognitive dysfunction induced by the three widely used chemotherapy agents (carmustine, cisplatin and cytosine arabinoside) is due to their toxic effects on CNS progenitor cells and non-dividing oligodendrocytes in vitro.19 They also found that these agents caused increased cell death and decreased cell division in the subventricular zone, the dentate gyrus of the hippocampus and the corpus callosum in mice.
Metallothioneins (MTs) are a family of low molecular weight cysteine-rich, proteinsthat are associated with transition metal cations including Zn, Cd, Cu and Hg.20 Previous studies have indicated the role of MT in protecting cells, tissues and organisms from environmental toxicant-induced damage.21,22 Three isoforms of metallothioneins (MT-I, MT-II and MT-III) are expressed in the central nervous system.23 Previous studies reported that brain MT-I/II are upregulated by different stressful stimuli including psychogenic stress,24 administration of bacterial endotoxin,25 glutamate analogues,26 metal toxicity27 and stroke/ischemia.28 In particular MT I and II could protect neuroglial cells from oxidative damage.29 The authors conclude that lack of this protection has been found to potentiate excitotoxicity and neurodegeneration in the hippocampus.
A common feature seen in a number of studies is that MT-I, II reduces delayed cerebral damage and cell death, as well as promotes brain repair, angiogenesis and functional recovery.30 Interestingly, MT-I, II were shown to act directly as neurotrophic agents after treatment of neurons with exogenous MT-I, II proteins, which enhance neuronal survival and axonal outgrowth in both cortical, hippocampal and dopaminergic cultures.31,32
Regulation of metallothionein gene expression by zinc has been documented.33 Free zinc induces the accumulation of large amount of zinc-containing metallothioneins.34 A number of studies have suggested that zinc status affects metallothionein concentration and its mRNA synthesis in the various tissues of growing and adult rats and mice.35 It has been reported that metallothionein induced by zinc exhibits protective effects on the cardiac apoptosis of doxorubicin,36 anthracycline-induced cardiac toxicity37 and adriamycin-induced myocardial injury.38 Increased MT expression in some tissues after in vivo treatment with DNA alkylating agents has been reported.39 It was found that rat hepatocytes with elevated MT levels are resistant to N-methyl-N'-nitro-nitrosoguanidine cytotoxicity.40 Also, overexpressed human MT-IIA gene protects Chinese hamster ovary cells from killing by alkylating agents.34 Moreover, treatment of tumor-bearing mice with ZnSO4 increased hepatic, renal and tumor MT and protected them from cytotoxic actions of cisplatin.35
However few studies have been carried out to explore the role of MT in neurocognitive functions,41,42 the relationship between MT induction and cognition deficits by chemotherapeutic agents is still not clear. The current study aimed to address the effect and mechanism of centrally-induced MT on the impact of BCNU on learning and memory in rats.
Results
Brain metallothionein (MT).
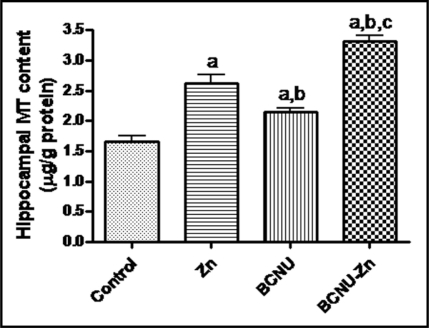
Data in Figure 1 explains that injection of ZnSO4 markedly increased hippocampal MT content (53%) when compared to the corresponding control group. Also, administration of BCNU significantly increased MT level in the hippocampus of control rats by an extent of 29% but still at a lower significant level in comparison with ZnSO4-treated group. The group of rats pretreated with ZnSO4 then 24 hours later with BCNU show marked increases in the level of hippocampal MT content up to110%, 36.5% and 61% if compared to the control, ZnSO4-treated or BCNU-treated groups respectively (Fig. 1).
Figure 1.
Effect of ZnSO4 and/or carmustine (BCNU) on the level of hippocampal metallothionein (MT) in rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). Animals were sacrificed after three weeks where MT was measured in hippocampal homogenates. (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
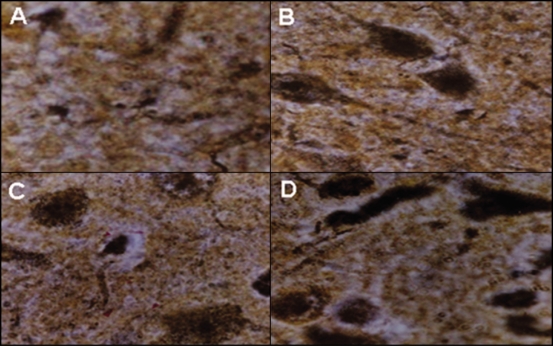
Immunohistochemical staining of MT in brain sections by using specific antibodies revealed that the level of brain MT was obviously increased in the tested groups of rats in the order of ZnSO4-pretreated-BCNU-treated (D) >ZnSO4-treated (B) >BCNU-treated (C) >control (A) groups (Fig. 2).
Figure 2.
A photomicrograph for immunohistochemical staining of metallothionein (MT) in hippocampal sections from control (A), ZnSO4-treated (B), BCNU-treated (C) and ZnSO4-pretreated-BCNU-treated rats (D) shows increased MT level in the order of ZnSO4-pretreated-BCNU-treated (D) >ZnSO4-treated (B) >BCNU-treated (C) >control (A). ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). Staining of MT in hippocampal sections was carried out by using MT-specific antibodies and ABC detection kit.
Learning and memory.
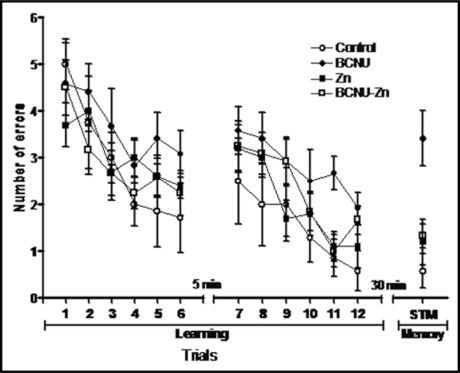
Behavioral tests in the present study show that there is direct correlation between the good learning and short-term memory (STM) of rats on one hand and the number of learning trials on the other hand where the number of errors were decreased as the number of trials increased in all tested groups (Fig. 3). BCNU administration deteriorated both learning and memory when compared to the corresponding control groups. However, ZnSO4 administration before BCNU obviously improved both learning and memory (Fig. 3).
Figure 3.
Effect of single doses of ZnSO4 and/or carmustine (BCNU) on learning and short-term memory (STM) in rats. Raw data are presented as mean values (n = 15). ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). Learning and short-term memory (STM) were assessd by using radial arm water maze where the number of errors for each group was calculated in 12 trials to indicate learning behaviour. After 30 min from leaning phase STM for each group was assessed by measuring the number of errors.
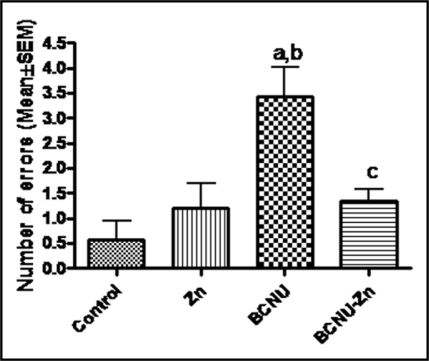
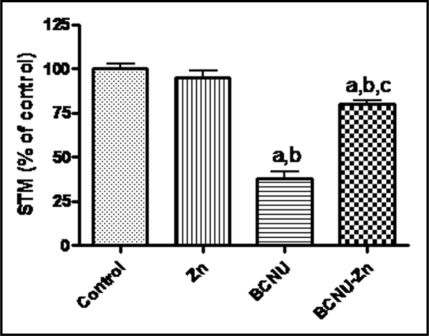
Statistical analysis of data (Fig. 4) explain that the group of rats injected with BCNU showed a markedly impaired learning behavior by the extents of 32% from the control group and 39% from ZnSO4-treated group. Administration of ZnSO4 before BCNU normalized the decreased learning behavior (Fig. 4). Also, BCNU administration significantly reduced STM in rats to be 31% and 35% of control and ZnSO4-treated rats respectively (Fig. 5). Rats pretreated with ZnSO4 then BCNU showed significant improvement in STM if compared to rats treated with BCNU without ZnSO4 preadministration as it was increased to reach 81% of the control group and 85% of ZnSO4-treated rats (Fig. 5).
Figure 4.
Effect of ZnSO4 and/or carmustine (BCNU) on learning of rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). Learning was assessed by using radial arm water maze where the number of errors for each group was calculated in 12 trials to indicate learning behaviour. (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
Figure 5.
Effect of ZnSO4 and/or carmustine (BCNU) on short-term memory (STM) in rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). STM was assessed after 30 min from leaning phase by using radial arm water maze where the number of errors for each group was calculated to indicate STM behaviour. (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
Glutathione reductase (GR) activity and reduced glutathione (GSH) content.
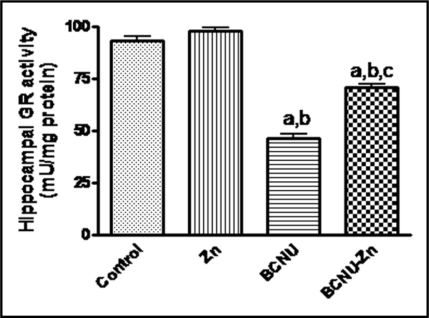
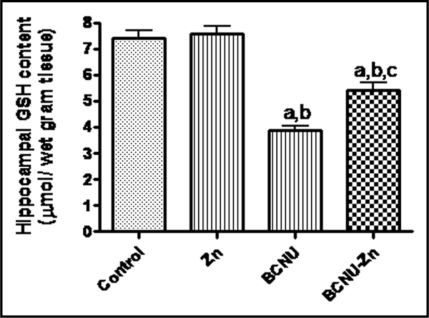
The present data explain that the activity of GR (Fig. 6) and the level of GSH (Fig. 7) in rat hippocampus was aggressively reduced by administration of BCNU to the extents of 49% and 53% of the control group; and 47% and 51% of ZnSO4-treated rats respectively. Treatment of rats with ZnSO4 before BCNU resulted in marked increases in the activity of GR (to the extents 76% and 72% of the control and ZnSO4-treated groups respectively) and GSH content (to the extents of 73% and 71% of the control and ZnSO4-treated groups respectively).
Figure 6.
Effect of ZnSO4 and/or carmustine (BCNU) on hippocampal glutathione reductase (GR) activity in rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). GR activity was assessed in hippocampal homogenates at the end of the experiment period (3 weeks). (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
Figure 7.
Effect of ZnSO4 and/or carmustine (BCNU) on the level of reduced glutathione (GSH) in the hippocampus of rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). GSH content was assessed in hippocampal homogenates at the end of the experiment period (3 weeks). (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
Malondialdehyde (MDA).
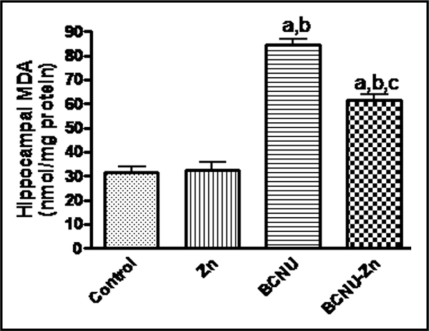
In Figure 8 MDA showed 2.5 fold increase in the hippocampus BCNU-treated animals when compared to either control or ZnSO4-treated groups. In the group of rats preinjected with ZnSO4 then BCNU there was up to 60% reduction in the level of MDA compared to BCNU-treated rats but still at a higher level of significance in comparison with either control or ZnSO4-trated animals.
Figure 8.
Effect of ZnSO4 and/or carmustine (BCNU) on the level of malondialdehyde (MDA) in the hippocampus of rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). MDA content was assessed in hippocampal homogenates at the end of the experiment period (three weeks). (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
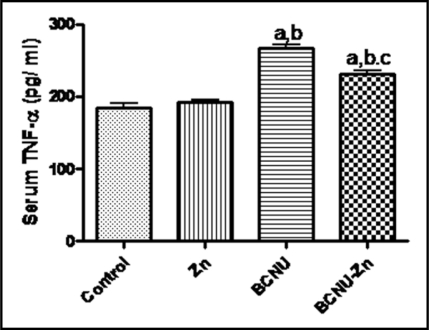
TNFα.
Evaluation of serum TNFα revealed that BCNU produced significant increases in the level of TNFα up to 44% and 39% when compared with control or ZnSO4-trated animals respectively. On the other hand, this level showed a marked reduction (15%) in ZnSO4-pretrated-BCNU-treated rats in comparison with only BCNU-treated animals although it was still at a significant higher level if compared to control or ZnSO4-trated groups (Fig. 9).
Figure 9.
Effect of ZnSO4 and/or carmustine (BCNU) on the level of reduced tumour necrosis factor-alpha (TNFα) in the serum of rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). TNFα level was assessed in the serum at the end of the experiment period (3 weeks). (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
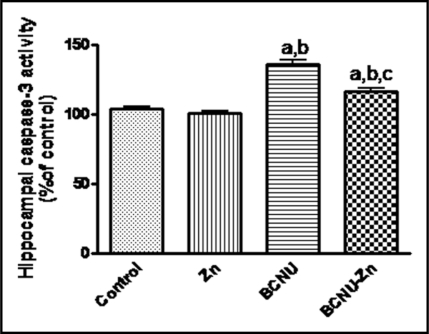
Caspase-3 enzyme activity.
Figure 10 explains that the activity of caspase-3 enzyme was markedly increased in the hippocampus of rats treated with BCNU compared to either control (by 31%) or ZnSO4-treated (by 34%) animals. In ZnSO4-pretreated-BCNU-trated rats, the activity of caspase-3 was significantly decreased to the extents of 12% and 15% from of the control and ZnSO4-treated groups respectively.
Figure 10.
Effect of ZnSO4 and/or carmustine (BCNU) on the activity of caspase-3 enzyme in the hippocampus of rats. Data are presented as mean ± SEM (n = 10) and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v). Caspase-3 activity was assessed in hippocampal homogenates at the end of the experiment period (3 weeks). (a–c): Indicate significant differences from control, BCNU-treated and ZnSO4-pretreated-BCNU-treated groups respectively at p < 0.05.
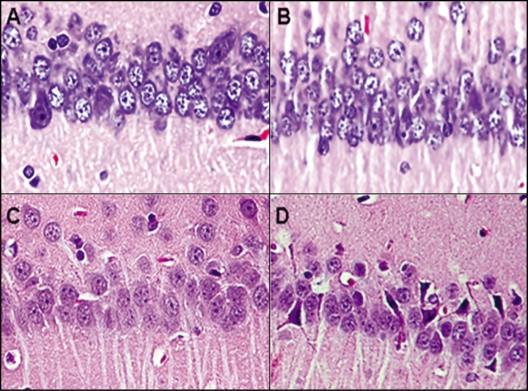
Histological examination.
Figure 11 explains that administration of BCNU resulted in massive neuronal damage manifested as an apparent decrease (45%) in the number of normal-appearing neurons in the middle hippocampus CA1 in which most pyramidal cells died (Fig. 11C) compared with either control (Fig. 11A) or ZnSO4-treated animals (Fig. 11B). Animals pretreated with ZnSO4 and 24 hours later with BCNU (Fig. 11D) showed an obvious increase (30%) in the number of intact neurons as compared to BCNU-treated animals. A photomicrograph of rat brain sections stained with Hx & E (X 40) shows CA1 region of the hippocampus from control (A), ZnSO4-treated (B), BCNU-treated rats (C) and ZnSO4-pretreated-BCNU-treated rats (D).
Figure 11.
A photomicrograph of rat brain sections stained with Hx & E (X 40) shows CA1 region of the hippocampus from control (A), ZnSO4-treated (B), BCNU-treated rats (C) and ZnSO4-pretreated-BCNU-treated rats (D) explains that administration of BCNU resulted in massive neuronal damage manifested as a decrease (45%) in the number of normal-appearing neurons (as calculated as mean number/10 fields) in the middle hippocampus CA1 in which most pyramidal cells died (C) compared with either control (A) or ZnSO4-treated animals (B). Animals pretreated with ZnSO4 and 24 hours later with BCNU (D) shows an obvious increase (30%) in the number of intact neurons as compared to BCNU-treated animals. ZnSO4 was injected as a single dose (0.1 µmol/10 µl saline, i.c.v). BCNU was injected in a single dose (20 mg/kg i.v).
Discussion
Impaired cognitive functions after administration of chemotherapeutic agents have been reported in animal models and in humans.7 The present data revealed that injection of BCNU into rats resulted in impairment of learning and STM. This effect is in consistence with the previous study of Reiriz et al.9 who reported that a single dose of cyclophosphamide produced a transient acute memory impairment in mice. Also, it was found that adriamycin produced cognitive dysfunction in experimental animals.10 In addition, exposure to13-cis-retinoic acid, impaired spatial learning and memory in mice.11 Moreover, the present data are in close agreement with the study of Dietrich et al.17 who reported cognitive dysfunction after administration of carmustine, cisplatin and cytosine arabinoside in mice.
The relationship between the integrity of hippocampus and normal learning and memory pattern has been documented.17 The present study showed that BCNU induced oxidative stress in the hippocampus of rats as indicted by aggressive inhibition of GR enzyme activity, reduction of GSH content and increased hippocampal content of MDA in comparison with the control groups. In addition, serum TNFα and the activity of caspase-3 showed significant higher hippocampal levels in BCNU-treated animals compared to corresponding control values. Moreover, microscopic examination of hippocampal sections showed deteriorated histological features in rats treated with BCNU if compared to control groups. These data are in harmony with the previous investigations that reported BCNU as a potent GR inhibitor and GSH depletor in several tissues.43,44 It has been explained that depletion of GSH, as a consequence of GR inhibition will increase cellular oxidative damage.45
The increased extent of lipid peroxidation and apoptosis (as indicated by increased caspase-3 activity) in the hippocampus as well as the level of serum TNFα after BCNU administration in the present study is supported by previous studies on various tissues. In this respect, it was found that incubation of BCNU with rat brain slices for two hours produced marked depletion of GSH (up to 70%) accompanied with increased extent of lipid peroxides.46 Also, BCNU was found to inhibit the activity of GR and promoted the oxidative damage in the nigrostriatal system.47 In addition, BCNU could inhibit GR, depleted GSH and induced apoptosis in PC12 cells.48 It has been reported that BCNU administration, as one of common breast cancer regimen, resulted in apparent inhibition of lung GR activity and GSH content with increased levels of TNFα and lipid peroxidation with marked histological alterations.49 Moreover, the interrelation between oxidative stress and release of inflammatory cytokines including TNFα and subsequent tissue damage has been proved.50 GSH depletion was reported to be associated with augmentation of an oxidative stress-mediated proinflammatory state in alveolar epithelial cells by an oxidative stress-dependent mechanism.51 Recently, it has been concluded that BCNU induced lung fibrosis in rats, an effect mediated by increased oxidative stress and induction of the proinflammatory cytokine TNFα.52 On the other hand, Ali-Osman et al.53 explained that, BCNU metabolites are very reactive electrophiles capable of depleting GSH and inducing apoptosis. It was also stated that the cognitive dysfunction induced by the three widely used chemotherapy agents (carmustine, cisplatin and cytosine arabinoside) is due to their toxic effects on CNS progenitor cells and nondividing oligodendrocytes of in vitro.19 In addition, BCNU was found to increased cell death and decreased cell division in the hippocampus of mice.17 Since neurotoxicity, DNA damage, Oxidative stress and release of cytokines were reported as mechanisms of impairment of cognitive functions after chemotherapy,12 it could be suggested that BCNU administration resulted in hippocampal toxicity in the form of apoptosis, increased level of lipid peroxidation and histological alterations with subsequent impairment of learning and memory.
The involvement of MT in protection against various stress insults has been reported.33,39,54 Imuunohistochemical and biochemical techniques in the present study showed that BCNU administration markedly increased the level of MT in the hippocampus of rats. Also, i.c.v injection of ZnSO4 into either control animals or 24 hours before administration of BCNU resulted in significant increase in the level of MT in the hippocampus of both groups in the order of BCNU-ZnSO4-pretreated >control. It is generally accepted that the expression of MT-I/II proteins is highly inducible in response to a range of stimuli, including metals, hormones, cytokines, oxidative agents, inflammation and stress.22 The induced MT in response to BCNU administration is in harmony with the reported role of MT in resistance to alkylating agents during treatment of cancers such as bladder cancer55 and esophageal cancer.56 Also, recent studies strongly suggested a significant role of MT during neurodegenerative diseases and in response to brain injury.57 In addition, Schroder et al.39 have considered that tissue induction of MT as a mechanism of resistance to oxidative stress produced by alkylating agents. Therefore, the increased level of MT in BCNU-treated animals may represents an acute phase response to act against increased oxidative stress produced by BCNU.
It has been stated that, metal-induced synthesis of MT is mediated by activation of metal response element-binding transcription factor (MTF-1), a zinc-sensitive trans-acting factor.57,58 The increased level of MT after ZnSO4 injection in the present work is in close agreement with the early study of Ebadi and Swanson59 who found that i.c.v injection of zinc induced brain MT. In addition, several studies have suggested that zinc status affects metallothionein concentration and its mRNA synthesis in the various tissues of growing and adult rats and mice.60 Recently, it has concluded that administration of Zn2+ (i.v) during reperfusion phase of cerebral ischemia could pass BBB and induced hippocampal MT.28
Although MT has been documented to protect against neuronal injury,61 its role in neurobehavioral function have not been well characterized.57 Behavioral tests in the present study showed marked potentiation of learning and memory in rats pretreated with ZnSO4 (i.c.v), 24 hours before BCNU, compared to those without ZnSO4 preadministration. These data may explain the decisive role of MT induction in the improvement of cognition during BCNU administration. In this respect, West et al.57 believed that alterations in MT function could alter neural function in ways that would impair behavioral function. The authors explained that MTs play a significant role in zinc homeostasis in the hippocampus which is essential in maintenance of normal cognitive functions. Also, it was concluded that the hippocampus, which plays a central role in cognitive functions such as memory depends on correct physiological actions of zinc, which is heavily concentrated in the hippocampal mossy fiber system.41 In addition, MT-I/II were found to protect against the adverse effects of both zinc under and overload.62 Moreover, metallothionein-null mice showed learning deficits in passive avoidance and water maze escape learning.63
The obtained data revealed that pretreatment of rats with ZnSO4 (i.c.v) before BCNU conferred protection of the hippocampus against BCNU-induced damage as the levels of caspase-3 and MDA were markedly reduced but the contents of MT and GSH as well as the activity of GR in the hippocampus were significantly higher if compared to only BCNU-treated rats. Also, serum TNFα showed apparent reduction in rats preinjected with ZnSO4. This protection was further confirmed by histological examination. These data are in line with the previous studies in which neuronal injury was reported to be implicated in cognitive dysfunction.17 On the other hand, MT-I, II were shown to enhance neuronal survival and axonal outgrowth in both cortical, hippocampal and dopaminergic cultures.30,32 In addition, MT was found to protect against neuronal damage via its powerful antioxidant and antiapoptic properties.9,64 Moreover, MT counteracted oxidative stress and apoptosis in animals treated with DNA alkylating agents.39 Furthermore, treatment of tumor-bearing mice with ZnSO4 increased hepatic, renal and tumor MT and protected them from cytotoxic actions of cisplatin.35 It is important to note that MT-I, II are powerful scavengers of free radicals, likely as a function of their cysteine residues.30 In addition, it was concluded that MT induction creates a new pool of thiol groups in the cell cytosol that can attenuate damaging effects of GSH depletors in rat hepatocytes.65 Further studies indicated that the released Zn+2 from MT might suppress free radical-mediated damage by its ability to induce the metalloenzyme superoxide dismutase or to stabilize the cell membrane function.66 In addition, it has been shown MT induced by zinc exhibited protective effects from doxorubicin-induced myocardial apoptosis36 and adriamycin-induced myocardial injury by inhibition of oxidative stress-mediated mitochondrial cytochrome c release and caspase-3.38 On the other hand, the oxidative stress-dependent pathway for increased levels of TNFα and other cytokines and their implication in neuronal injury has been reported.30,51 MT-I, II were reported to inhibit the expression of proinflammatory cytokines such as interleukins IL-1β, IL-6, IL-12 and TNFα with subsequent suppression of the inflammatory responses of leukocytes.30 It was found that exogenous administration of metallothionein reduced pro-inflammatory cytokines IL-6 and TNFα and apoptotic cell death during experimental autoimmune encephalomyelitis.67 Herein, it could be proposed that among the key mechanisms for improvement of BCNU-induced learning and memory deficits after induction of brain MT by administration of ZnSO4 is the buffering effect of MT against BCNU-induced hippocampal damage through rebalancing of oxidant/antioxidant equilibrium (as the levels of GR activity and GSH content were preserved), anti-inflammatory effect (as the level of TNFα was markedly reduced) and antiapoptotic effect (as it produced marked reduction in caspase-3 activity).
In conclusion, the obtained data may suggest that MT induction can act against BCNU-induced hippocampal cognitive deficits. This effect is mediated at least in part by antioxidant, antiapoptotic and anti-inflammatory mechanisms as well as maintenance of zinc homeostasis. This may help to understand the role of metallothionein in chemotherapy-induced neurocognitive dysfunction which may be considered for the improvement of behavioral pattern during administration of anticancer agents.
Methods
Animals.
Adult male Wistar albino rats weighing 150–180 g were obtained from the Animal Care Center, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia. The animals were housed in metabolic cages under standard laboratory conditions (12 h light/dark cycle at 25 ± 2°C) with free access to pulverized standard rat pellet food and tap water.
Experimental protocol.
A total of 60 male Wistar albino rats were randomly divided into four groups (15/group): The first group served as a control group in which the animals received a single intracerbrovenricular (i.c.v) dose of normal saline (10 µl) followed 24 h later with an i.v injection of BCNU solvent (normal saline containing 10% ethanol). The second group administered a single dose of ZnSO4 (0.1 µmol/10 µl normal saline, i.c.v) followed 24 h later with an injection of BCNU solvent (i.v). Rats in the third group received a single dose of BCNU (20 mg/kg, i.v) 24 h after an injection (i.c.v) of normal saline (10 µl). Fourth group received a single dose of ZnSO4 (0.1 µmol/ 10 µl normal saline, i.c.v) followed 24 h later with an injection of BCNU (20 mg/kg, i.v). After three weeks, animals in all groups were subjected to behavioral tests for learning and short-term (STM) memory using radial arm water maze then anaesthetized with ether and sacrificed where five rats from each group were used for histological analysis. The remaining ten rats were used for biochemical analysis where BCNU toxicity was evaluated by measuring MDA (as a marker for lipid peroxidation), caspase-3 activity (as a marker for apoptosis) as well as the possible mechanisms for this toxicity by measuring GR activity and GSH content in the hippocampus as well as serum TNFα level. The ability of MT to counteract BCNU-induced hippocampal toxicity was evaluated by measuring the previous parameters after MT induction by ZnSO4. In each group, blood samples from each animal were collected separately, centrifuged and used for determination of TNFα. The two lobes of hippocampus in each animal were rapidly dissected out on ice, washed with saline and cut into small pieces and used for biochemical analysis. Hippocampal pieces from each animal in each group were homogenized and used for determination of the activity of hippocampal glutathione reductase (GR) and the contents of MT, reduced glutathione (GSH), malodialdehyde (MDA) as well as total protein. Another portion of pieced was dissociated into free cells by trypsinization where the activity of caspase-3 was assessed in the cell lysate.
Intracerebroventricular (i.c.v) injection of ZnSO4.
Rats were anaesthetized by administration of sodium pentobarbital (60 mg/kg, i.p) then placed gently in a stereotaxic apparatus68 with the tooth bar 5 mm above the ear bar. Sagittal incision was made and the scalp was exposed. By using brain map and stereotaxic coordinates, the bony calcaneum was penetrated with dental drill to allow access into the brain. ZnSO4 solution was slowly infused using Hamilton microsyringe where the syrnge was left in place for 5 min. After removal of the syringe, the wounds were sutured.
The radial arm water maze procedure.
The radial arm water maze consisted of a black circular water tub with six V-shaped stainless steel structures arranged to form a swimming field of an open central area and six arms.69 The water temperatures was maintained at 25°C. A goal arm is one that has a black platform submerged 1cm below the water level. Starting from a start arm (any arm other than the goal arm), the rat must find the submerged platform by swimming to the end of the goal arm. Each rat was allowed 12 consecutive training trials (learning phase) followed by a short-term memory (STM) test trial (30 min delay periods). Rats were allowed to take rest for 5 min to avoid exhaustion at the end of the 6th trial. Rats were allowed 1 min per trial to find the submerged platform. A trial ended when the rat located the submerged platform, where it was allowed to stay trial 15 sec on the platform before removal to begin the next trial in a different start arm. If the rat did not find the submerged platform in the goal arm after one min, it was guided the goal arm and allowed to stay on the platform for 15 sec before removal to begin the next trial. A correct selection occurred when the rat swam directly to the goal arm, while error was registered when the rat entered into an arm other than the goal arm. All experiments were done in dimly lit room and the rat had to use cues in the room to spatially memorize the location of the platform. After the last trial the mean umber of errors was calculated for each group to indicate the learning behavior.
Histological examination and immunohistochemical staining for brain MT.
Rats were anaesthetized with ether and brains were dissected out on ice and fixed in 10% formalin saline solution then embedded in paraffin. The 5 µm sections were stained on glass slides by Hx & E and examined under light microscope for histological alterations in the hippocampus. The mean number of 10 microscopic fields of normally-appeared hippocampal neurons was calculated.
Expression of brain MT was evaluated by immunohistochemical staining of brain tissues using monoclonal mouse anti-MT antibody (Dako, Carpentaria, CA, USA) and vectastain ABC kit (Vector Laboratories, Burlingame, CA, USA). After deparaffinization, brain sections on glass slides were subjected to quenching of endogenous peroxidase activity using 3% H2O2 for 10 min at room temperature. Non-specific binding sites were blocked by 5% normal rabbit serum for 1 h, then washed with PBS buffer for 10 min. Sections were incubated with primary MT antibodies (diluted 1:500 in 10 mmol/L PBS) overnight at 4°C and then washed with PBS buffer for 10 min. Sections were incubated with biotinylated rabbit anti-mouse Ig G (secondary antibodies) for 1 h and then washed with PBS buffer for 10 min, followed by the addition of vectastain ABC reagent and incubation for 1 h, with a final wash using PBS buffer. The substrate solution in the kit, diaminobenzedine (DAB), was added and the color was produced within 2–7 min. Stained sections were washed under tap water, air dried and photographed under a light microscope.
Determination of hippocampal MT.
Hippocampal content of MT was measured by ELISA.23 Briefly, in a microtiter plate, 150 µl of 10% tissue homogenate from each sample in coating buffer (0.015 M Na2CO3, 0.023 M NaHCO3, 0.02% Na azide in 80 ml H2O, pH 9.8) added to the wells and left at 4°C overnight. The wells were then washed three times with phosphate buffered saline (PBS) solution containing 1% Tween (pH, 7.4). To each well 150 µl of MT primary antibodies (diluted 1:500 in PBS-Tween solution) and incubated on a shaker for 2 h. Anti-mouse Ig G secondary antibodies diluted in PBS-Tween were added (150 µl/well) and the plate was incubated at room temperature for 2 h followed by washing of the wells with PBS-Tween three times. The substrate solution (p-nitrophenol) was added (150 µl/well) and incubated in dark at room temperature for 30 min. The reaction was stopped by addition of 50 µl 3N NaOH solution to each well. The absorbance of produced color was read at 405 nm in ELISA reader where MT concentration (µg/g protein) was calculated from a standard calibration curve of MT protein.
Determination of hippocampal GR activity and GSH content.
GR activity was measured by the method of Carlberg and Mannervick.70 Briefly, 100 µl of 0.2 M sodium phosphate, pH 7.6 (containing 1 mM EDTA), 25 µl 20 mM GSSG and 25 µl 2 mM NADPH were incubated at 30°C for 10 min. 50 µl of 5% hippocampus homogenate sample (in 50 mmol/L phosphate buffer, pH 7.0 containing 0.1 mmol/L EDTA) were added into a reaction cuvette, and the rate of change of absorbance at 340 nm was measured for 3 min. The activity of GR was expressed as mU/mg protein.
Tissue levels of acid soluble thiols, mainly reduced glutathione (GSH), were determined calorimetrically at 412 nm according to Ellman.7 In briefl, 0.5 ml of previously prepared homogenate was added to 0.5 ml of 5% trichloroacetic acid, centrifuged at 1,000 xg for 5 min. The supernatant (200 µl) was added to a tube contains 1,750 µl of 0.1 M potassium phosphate buffer (pH 8) and 50 µl of 5,5 dithiobis-2-nitrobenzoic acid (DTNB) reagent. The tubes were mixed and the developed yellow color was measured against standard curve of reduced glutathione. Protein thiols (protein-SH) were expressed as µmol/g tissue.
Determination of serum TNFα.
Serum TNFα, was assayed by using ELISA kit purchased from R&D Systems (Minneapolis, MN, USA) according to the protocol provided by the manufacturer. Briefly, in a microplate, 50 µl of the assay diluent added to each well. Then 50 µl of the diluted serum sample (2-fold dilution in the calibrator diluent) were added to each well and mixed gently by tapping the plate frame for 1 min then the plate was covered and incubated for 2 h at room temperature. After incubation, each well in the plate was then aspirated and washed five times with the kit washing buffer followed by addition of 100 µl substrate solution and incubated in dark for 30 min at room temperature. The optical density was then read at 450 nm using a 96-well plate spectrometer (Spectra Max 190, Molecular Devices Corp., Sunnyvale, CA, USA). TNFα level (pg/ml) was calculated from a standard curve and multiplied by the dilution factor.
Determination of hippocampal caspase-3 activity.
Hippocampal cell suspension was prepared from hippocampal tissue following the method described by Sameto.72 Briefly, hippocampi from each animal were dissected out, cut into small pieces and suspended in 10 mL sterile saline solution (12.38 mmol/L NaCl, 5.4 mmol/L KCl, 1.1 mmol/L Na2HPO4, 1.1 mmol/L KH2PO4, 22 mmol/L glucose and 0.9 CaCl2), containing 0.25% v/v trypsin, in a Petri dish. The suspension was then aspirated two to three times using glass pipette and transferred to a screw-capped Erlenmeyer flask and shaken on a rotary shaker (80 r.p.m. for 15 min at 37°C). Trypsinization was then halted by the addition of 10 mL serum supplemental medium (SSM) containing 10% v/v fetal bovine serum (FBS) and the disrupted tissue was then gently aspirated three times using a 10 ml glass pipette. The aspirated suspension was carefully filtered through Nitex 210 then Nitex 130 filters (TetKo, Elmeford, NY, USA) by gravity. The entire filtrate was then centrifuged at 800 g for 5 min at room temperature and the pellet was resuspended in fresh SSM. Viable cells were counted using a haemocytometer and trypan blue 0.4% diluted in phosphate-buffered saline (PBS) containing 1 mmol/L EDTA (1:16).
Hippocampal caspase-3 activity was measured by using Caspase-3/CPP32 activity Colorimetric Assay Kit (Biovision Incorporate, USA) according the procedure supplied by the manufacturer. Briefly, the prepared cell suspension was centrifuged. Then cells were resuspended in chilled cell lysis buffer (1–5 × 106 cells/50 µl) and incubated on ice for 10 min, centrifuged for 1 min in a microcentrifuge (10,000 xg). To each sample pellet, 50 µl cell lysis buffer was added followed by addition of 50 µl of 2X reaction buffer (containing 10 mM DTT). 5 µl of the 4 mM DEVD-pNA substrate (200 µM final conc.) was added and to each sample and incubated at 37°C for 2 h. Samples were read at 405-nm in a microtiter plate ELISA reader. The absorbance of the produced color (pNA) from treated animals was compared with control animals to determinate the percentage of caspase-3 activity changes.
Determination of hippocampal MDA.
Hippocampal lipid peroxides were determined colorimetrically using thiobarbituric acid (TBA), as described by Uchiyama and Mihara,73 where lipid peroxides expressed in terms of MDA concentration (nmol/mg protein). In brief, hippocampus lobes were homogenized separately in 50 mmol/L phosphate buffer (pH 7.0) containing 0.1 mmol/L EDTA to obtain a 5% homogenate. In a Teflon-stoppered test tube, 2.5 ml of 20% acetic acid and 1 ml TBA solution were added to the tissue homogenate and allowed to boil at 100°C for 30 min in a water bath. After cooling to room temperature under tap water, 4 ml n-butanol was added and samples were shaken vigorously and centrifuged at 600 g for 5 min. The absorbance of the upper colored layer was measured at 532 nm and the concentration of MDA was calculated from a standard calibration curve and expressed as nmol/g protein.
Total protein assay.
Total protein was determined according to the method of Lowery et al.74 In brief, 1.0 ml of alkaline copper solution (prepared by mixing 50 ml of 2% Na2CO3 in 0.10 N NaOH with 1.0 ml of 0.50% CuSO4. 5 H2O in 1% sodium tartrate) was added to a test tube containing 0.20 ml of 10% hippocampus homogenate (w/v), mixed well and allowed to stand for 10 min at room temperature. Then, 0.10 ml of Folin's reagent (phospho-molybdic-phosphotungstic reagent diluted 1:1 in H2O before use) was added and thoroughly mixed. After 30 min the optical density was measured against blank at 500 nm. Protein concentration was calculated from a standard calibration curve in which bovine albumin was used in different concentrations.
Statistical analysis.
Data were presented as mean ± SEM and analyzed using Graph Pad Instat software by one way ANOVA followed by Tukey Kramer post-test at p < 0.05.
Acknowledgements
The present work was supported by grant (B.R.C. 205) from Research Center, college of Pharmacy, King Saud University, Saudi Arabia.
Footnotes
Previously published online as an Oxidative Medicine and Cellular Longevity E-publication: http://www.landesbioscience.com/journals/oximed/article/7901
References
- 1.Keime-Guibert F, Napolitano M, Delattre JY. Neurological complications of radiotherapy and chemotherapy. J Neurol. 1998;245:695–708. doi: 10.1007/s004150050271. [DOI] [PubMed] [Google Scholar]
- 2.Wefe JS, Kayl AE, Meyers CA. Neuropsychological dysfunction associated with cancer and cancer therapies: A conceptual review of an emerging target. Br J Cancer. 2004;90:1691–1696. doi: 10.1038/sj.bjc.6601772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shilling V, Jenkins V, Morris R, Deutsch G, Bloomfield D. The effects of adjuvant chemotherapy on cognition in women with breast cancer preliminary results of an observational longitudinal study. Breast. 2005;2:142–150. doi: 10.1016/j.breast.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Meyers CA, Abbruzzese JL. Cognitive functioning in cancer patients: effect of previous treatment. Neurology. 1992;42:434–436. doi: 10.1212/wnl.42.2.434. [DOI] [PubMed] [Google Scholar]
- 5.Macdonald DR. Neurologic complications of chemotherapy. Neurol Clin. 1991;9:955–967. [PubMed] [Google Scholar]
- 6.van Dam FS, Schagen SB, Mulle MJ, Boogerd W, van der Wall E, Droogleever Fortuyn ME, Rodenhuis S. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: High-dose versus standard-dose chemotherapy. J Natl Cancer Inst. 1998;90:210–218. doi: 10.1093/jnci/90.3.210. [DOI] [PubMed] [Google Scholar]
- 7.Vardy J, Tannock L. Cognitive function after chemotherapy in adults with solid tumours. Critical Rev Oncol Hematol. 2007;63:183–202. doi: 10.1016/j.critrevonc.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Meyers CA. How chemotherapy damages the central nervous system. J Biol. 2008;7:11. doi: 10.1186/jbiol73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reiriz AB, Reolon GK, Preissler T, Rosado JO, Henriques JAP, Roesler R, et al. Cancer chemotherapy and cognitive function in rodent models: Memory impairment induced by cyclophosphamide in mice. Clin Cancer Res. 2006;12:5000. doi: 10.1158/1078-0432.CCR-06-0138. [DOI] [PubMed] [Google Scholar]
- 10.Joshi G, Sultana R, Tangpong J, Cole MP, St Clair DK, Vore M, et al. Free radical mediated oxidative stress and toxic side effects in brain induced by the anti cancer drug adriamycin: Insight into chemobrain. Free Radical Res. 2005;39:1147–1154. doi: 10.1080/10715760500143478. [DOI] [PubMed] [Google Scholar]
- 11.Crandall J, Sakai Y, Zhang J, Koul O, Mineur Y, Crusio WE, et al. 13-cis-retinoic acid suppresses hippocampal cell division and hippocampal-dependent learning in mice. Proc Natl Acad Sci USA. 2004;101:5111–5116. doi: 10.1073/pnas.0306336101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vardy J, Wefel JS, Ahles T, Tannock IF, Schagen SB. Cancer and cancer-therapy related cognitive dysfunction: An international perspective from the Venice cognitive workshop. Ann Oncol. 2008;19:623–629. doi: 10.1093/annonc/mdm500. [DOI] [PubMed] [Google Scholar]
- 13.Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7:192–201. doi: 10.1038/nrc2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuxen MK, Hansen SW. Neurotoxicity secondary to antineoplastic drugs. Cancer Treat Rev. 1994;20:191–194. doi: 10.1016/0305-7372(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 15.Joseph JA, Denisova N, Fisher D, et al. Age-related neurodegeneration and oxidative stress: putative nutritional intervention. Neurol Clin. 1998;16:747–755. doi: 10.1016/s0733-8619(05)70092-x. [DOI] [PubMed] [Google Scholar]
- 16.Fillit HM, Butler RN, O'Connell AW, et al. Achieving and maintaining cognitive vitality with aging. Mayo Clin Proc. 2002;77:681–686. doi: 10.4065/77.7.681. [DOI] [PubMed] [Google Scholar]
- 17.Dietrich J, Han R, Yin Y, Mayer-Pröschel M, Noble M. CNS progenitor cells and oligodendrocytes are targets of chemotherapeutic agents in vitro and in vivo. J Biol. 2006;5:22. doi: 10.1186/jbiol50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagahiro S, Yamamoto YL, Diksic M, Mitsuka S, Sugimoto S, Feindel W. Neurotoxicity after intracarotid 1,3-bis(2-chloroethyl)-1-nitrosourea administration in the rat: hemodynamic changes studied by double-tracer autoradiography. Neurosurgery. 1991;29:19–25. doi: 10.1097/00006123-199107000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Nutt CL, Noble M, Chambers AF, Cairncross JG. Differential expression of drug resistance genes and chemosensitivity in glial cell lineages correlate with differential response of oligodendrogliomas and astrocytomas to chemotherapy. Cancer Res. 2000;60:4812–4818. [PubMed] [Google Scholar]
- 20.Hamer DH. Metallothionein. Annu Rev Biochem. 1986;55:913–951. doi: 10.1146/annurev.bi.55.070186.004405. [DOI] [PubMed] [Google Scholar]
- 21.Kagi JHA, Schaffer A. Biochemistry of Metallothionein. Biochemistry. 1988;23:8509–8515. doi: 10.1021/bi00423a001. [DOI] [PubMed] [Google Scholar]
- 22.Sato M, Bremner I. Oxygen free radicals and metallothionein. Free Radic Biol Med. 1993;14:325–337. doi: 10.1016/0891-5849(93)90029-t. [DOI] [PubMed] [Google Scholar]
- 23.Voller BD, Bartlett A. Enzyme-linked immunosorbent assay. In: Manual of clinical immunology. American Soci for microbiology. 1980:45. [Google Scholar]
- 24.Hidalgo J, Borras M, Garvey JS, Armario A. Liver, brain and heart Metallothionein induction by stress. J Neurochem. 1990;55:651–654. doi: 10.1111/j.1471-4159.1990.tb04182.x. [DOI] [PubMed] [Google Scholar]
- 25.Palmiter RD, Findley SD, Whitmore TE, Durnam DM. MT-III, a brain-specific member of the metallothionein gene family. Proc Natl Acad Sci USA. 1992;89:6333–6337. doi: 10.1073/pnas.89.14.6333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dalton T, Pazdernik TL, Wagner J, Samson F, Andrews GK. Temporal spatial patterns of expression of metallothionein-I and -III and other stress related genes in rat brain after kainic acid-induced seizures. Neurochem Int. 1995;27:59–71. doi: 10.1016/0197-0186(94)00168-t. [DOI] [PubMed] [Google Scholar]
- 27.Masters BA, Kelly EJ, Quaife CJ, Brinster RL, Palmiter RD. Targeted disruption of metallothionein I and II genes increases sensitivity to cadmium. Proc Natl Acad Sci USA. 1994;91:584–588. doi: 10.1073/pnas.91.2.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Helal GK. Systemic administration of Zn2+ during reperfusion phase of transient cerebral ischaemia protects rat hippocampus against iron-catalysed postischaemic injury. Clin Exper Pharmacol and Physiol. 2008;35:775–781. doi: 10.1111/j.1440-1681.2007.04858.x. [DOI] [PubMed] [Google Scholar]
- 29.Penkowa M, Giralt M, Camats J, Hidalgo J. Metallothionein 1 + 2 protect the CNS during neuroglial degeneration induced by 6-aminonicotinamide. J Comp Neurol. 2002;444:174–189. doi: 10.1002/cne.10149. [DOI] [PubMed] [Google Scholar]
- 30.Stankovic RK, Chung RS, Penkowa M. Metallothioneins I and II: Neuroprotective significance during CNS pathology. Inatl J Biochem Cell Biol. 2007;39:484–489. doi: 10.1016/j.biocel.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 31.Carrasco J, Penkowa M, Hadberg H, Molinero A, Hidalgo J. Enhanced seizures and hippocampal neurodegeneration following kainic acid-induced seizures in metallothionein-I + II-deficient mice. Eur J Neurosci. 2000;12:2311–2322. doi: 10.1046/j.1460-9568.2000.00128.x. [DOI] [PubMed] [Google Scholar]
- 32.Chung RS, Vickers JC, Chuah MI, West AK. Metallothionein-IIA promotes initial neurite elongation and postinjury reactive neurite growth and facilitates healing after focal cortical brain injury. J Neurosci. 2003;23:3336–3342. doi: 10.1523/JNEUROSCI.23-08-03336.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaina B, Lohrer H, Karen M, Herrlich P. Overexpressed human metallothionein-IIA gene protects chinese hamster ovary cells from killing dy alkylating agent. Proc Natl Acad Sci USA. 1990;87:2110–2114. doi: 10.1073/pnas.87.7.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robson T, Grindley H, Hall A, Vormoor J, Lohrer H. Increased DNA-repair capacity and the modulation of two proteins in Metallothionein overexpressing chinese hamster cell line. Mutat Res. 1994;314:143–157. doi: 10.1016/0921-8777(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 35.Satoh M, Kondo Y, Mita M, Naganuma A, Imura N. Prevention of carcinogenicity of anticancer drugs by metallothionein induction. Cancer Res. 1993;53:4767–4768. [PubMed] [Google Scholar]
- 36.Shuai Y, Guo J, Peng SQ, Zhang LS, Sichuan DA. Metallothionein inhibited DOX-induced cardiac apoptosis in mice. Xue Xue Bao Yi Xue Ban. 2007;38:620–623. [PubMed] [Google Scholar]
- 37.Kang YJ. Antioxidant defense gainst anthracycline cardiotoxicity by metallothionein. Cardiovasc Toxicol. 2007;7:95–100. doi: 10.1007/s12012-007-0007-3. [DOI] [PubMed] [Google Scholar]
- 38.Wang GW, Klein JB, Kang YJ. Metallothionein inhibits doxorubicin-induced mitochondrial cytochrome c release and caspase-3 activation in cardiomyocytes. J Pharmacol Exp Ther. 2001;298:461–468. [PubMed] [Google Scholar]
- 39.Schroder CP, Godwin AK, Odwyer PJ, Tew KD, Hamelton TC, Ozols RF. Glutathione and drug resistance. Cancer invest. 1996;14:158–168. doi: 10.3109/07357909609018891. [DOI] [PubMed] [Google Scholar]
- 40.Moffat P, Plaa GL, Denizeu F. Rat hepatocyte with elevated metallothionein expression are resistant to N-N′-nitrosoguanidine cytotoxicity. Toxicol Appl Pharmacol. 1996;136:200–207. doi: 10.1006/taap.1996.0025. [DOI] [PubMed] [Google Scholar]
- 41.Daumas S, Halley H, Lassalle JM. Disruption of hippocampal CA3 network: effects on episodic-like memory processing in C57BL/6J mice. Eur J Neurosci. 2004;20:597–600. doi: 10.1111/j.1460-9568.2004.03484.x. [DOI] [PubMed] [Google Scholar]
- 42.Yoshida M, Watanabe C, Horie K, Satoh M, Sawada M, Shimada A. Neurobehavioral changes in metallothionein-null mice prenatally exposed to mercury vapor. Toxicol Lett. 2005;155:361–368. doi: 10.1016/j.toxlet.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 43.Kehrer JP, Klein-Szanto AJ. Enhanced acute lung damage in mice following administration of 1,3-bis (2-chloroethyl)-1-nitrosourea. Cancer Res. 1985;45:5707–5713. [PubMed] [Google Scholar]
- 44.Wu M, Kelley MR, Hansen WK, Martin WJ. Reduction of BCNU toxicity to lung cells by high-level expression of O(6)-methylguanine-DNA methyltransferase. Am J Physiol Lung Cell Mol Physiol. 2001;280:755–761. doi: 10.1152/ajplung.2001.280.4.L755. [DOI] [PubMed] [Google Scholar]
- 45.Meister A. Glutathione-ascorbic acid antioxidant system in animals. J Biol Chem. 1994;269:9397–9400. [PubMed] [Google Scholar]
- 46.Bizzozero OA, Ziegler JL, De Jesus G, Bolognani F. Acute depletion of reduced glutathione causes extensive carbonylation of rat brain proteins. J Neurosci Res. 2006;83:656–667. doi: 10.1002/jnr.20771. [DOI] [PubMed] [Google Scholar]
- 47.Romero-Ramos M, Venero JL, Garcia-Rodriguez S, Ayala A, Machado A, Cano J. Semichronic inhibition of glutathione reductase promotes oxidative damage to proteins and induces both transcription and translation of tyrosine hydroxylase in the nigrostriatal system. Free Radic Res. 2003;37:1003–1012. doi: 10.1080/10715760310001598574. [DOI] [PubMed] [Google Scholar]
- 48.Doroshenko D, Doroshenko P. The glutathione reductase inhibitor carmustine induces an influx of Ca2+ in PC12 cells. Eur J Pharmacol. 2004;497:17–24. doi: 10.1016/j.ejphar.2004.06.043. [DOI] [PubMed] [Google Scholar]
- 49.Abushamaa AM, Sporn TA, Folz RJ. Oxidative stress and inflammation contribute to lung toxicity after a common breast cancer chemotherapy regimen. Am J Physiol Lung Cell Mol Physiol. 2002;283:336–345. doi: 10.1152/ajplung.00012.2002. [DOI] [PubMed] [Google Scholar]
- 50.Oikonomou N, Harokopos V, Zalevsky J, Valavanis C, Kotanidou A, Szymkowski DE, et al. Soluble TNF mediates the transition from pulmonary inflammation to fibrosis. PLoS ONE. 2006;1:108. doi: 10.1371/journal.pone.0000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haddad JJ. Glutathione depletion is associated with augmenting a proinflammatory signal: evidence for an antioxidant/pro-oxidant mechanism regulating cytokines in the alveolar epithelium. Cytokines Cell Mol Ther. 2000;6:177–187. doi: 10.1080/mccm.6.4.177.187. [DOI] [PubMed] [Google Scholar]
- 52.Helal GK, Helal OK. Metallothionein attenuates carmustine-induced oxidative stress and protects against pulmonary fibrosis in rats. Arch Toxicol. 2009;83:87–94. doi: 10.1007/s00204-008-0325-7. [DOI] [PubMed] [Google Scholar]
- 53.Ali-Osman F, Caughlan J, Gray GS. Decreased DNA interstrand cross-linking and cytotoxicity induced in human brain tumor cells by 1,3-bis(2-chloroethyl)-1-nitrosourea after in vitro reaction with glutathione. Cancer Res. 1989;49:5954–5958. [PubMed] [Google Scholar]
- 54.Penkowa M. Metallothioneins are multipurpose neuroprotectants during brain pathology. FEBS J. 2006;273:1857–1870. doi: 10.1111/j.1742-4658.2006.05207.x. [DOI] [PubMed] [Google Scholar]
- 55.Wülfing C, van Ahlen H, Eltze E, Piechota H, Hertle L, Schmid KW. Metallothionein in bladder cancer: correlation of overexpression with poor outcome after chemotherapy. World J Urol. 2007;25:199–205. doi: 10.1007/s00345-006-0141-8. [DOI] [PubMed] [Google Scholar]
- 56.Hishikawa Y, Abe S, Kinugasa S, Yoshimura H, Monden N, Igarashi M, et al. Overexpression of metallothionein correlates with chemoresistance to cisplatin and prognosis in esophageal cancer. Oncology. 1997;54:342–347. doi: 10.1159/000227714. [DOI] [PubMed] [Google Scholar]
- 57.West AK, Hidalgo J, Eddins D, Levin ED, Aschner M. Metallothionein in the central nervous system: Roles in protection, regeneration and cognition. Neuro Toxicol. 2008;29:489–503. doi: 10.1016/j.neuro.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Andrews GK. Regulation of metallothionein gene expression by oxidative stress and metal ions. Biochem Pharmacol. 2000;59:95–104. doi: 10.1016/s0006-2952(99)00301-9. [DOI] [PubMed] [Google Scholar]
- 59.Ebadi M, Swanson S. Characterization of metallothionein-like protein in rat brain. Experientia Suppl. 1987;52:289–291. doi: 10.1007/978-3-0348-6784-9_24. [DOI] [PubMed] [Google Scholar]
- 60.Chen WY, John JA, Lin CH, Chang CY. Expression pattern of metallothionein, MTF-1 nuclear translocation and its dna-binding activity in zebra fish (Danio rerio) induced by zinc and cadmium. Environ Toxicol Chem. 2007;26:110–117. doi: 10.1897/06-153r.1. [DOI] [PubMed] [Google Scholar]
- 61.Trendelenburg G, Prass K, Priller J, Kapinya K, Polley A, Muselmann C, et al. Serial analysis of gene expression identifies metallothionein-II as major neuroprotective gene in mouse focal cerebral ischemia. J Neurosci. 2002;22:5879–5888. doi: 10.1523/JNEUROSCI.22-14-05879.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kelly EJ, Quaife CJ, Froelick GJ, Palmiter RD. Metallothionein I and II protect against zinc deficiency and zinc toxicity in mice. J Nutr. 1996;126:1782–1790. doi: 10.1093/jn/126.7.1782. [DOI] [PubMed] [Google Scholar]
- 63.Levin ED, Perraut C, Pollard N, Freedman JH. Metallothionein expression and neurocognitive function in mice. Physiol Behav. 2006;87:513–518. doi: 10.1016/j.physbeh.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 64.West AK, Chuah MI, Vickers JC, Chung RS. Protective role of metallothioneins in the injured mammalian brain. Rev Neurosci. 2004;15:157–166. doi: 10.1515/revneuro.2004.15.3.157. [DOI] [PubMed] [Google Scholar]
- 65.Haïdara K, Moffatt P, Denizeau F. Metallothionein induction attenuates the effects of glutathione depletors in rat hepatocytes. Toxicol Sci. 1999;49:297–305. doi: 10.1093/toxsci/49.2.297. [DOI] [PubMed] [Google Scholar]
- 66.Ebadi M, Srinvasan SK, Baxi MD. Oxidative stress and antioxidant therapy in Parkinson disease. Prog Neurobiol. 1996;48:1–19. doi: 10.1016/0301-0082(95)00029-1. [DOI] [PubMed] [Google Scholar]
- 67.Penkowa M, Hidalgo J. Metallothionein I + II expression and their role in experimental autoimmune encephalomyelitis. Glia. 2000;32:247–263. doi: 10.1002/1098-1136(200012)32:3<247::AID-GLIA50>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 68.Cough RW, Rodruguez-Sierra JF, Hoppe LB. Kianic acid lesioning of the preoptic area alters positive feedback of estrogen in prepuberal female rats. Biol repro. 1986;35:1269–1276. doi: 10.1095/biolreprod35.5.1269. [DOI] [PubMed] [Google Scholar]
- 69.Diamond DM, et al. “Exposing rats to a predator impairs spatial working memory in the radial arm water maze.”. Hippocampus. 1999;9:542–552. doi: 10.1002/(SICI)1098-1063(1999)9:5<542::AID-HIPO8>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 70.Carlberg I, Mannervik B. Purification and characterization of the flavoenzyme glutathione reductase from rat liver. J Biol Chem. 1975;14:5475–5480. [PubMed] [Google Scholar]
- 71.Ellman GL. Tissue sulfhydryl groups. Arch Biochem Biophys. 1959:70–77. doi: 10.1016/0003-9861(59)90090-6. [DOI] [PubMed] [Google Scholar]
- 72.Sameto RP. Preparation of highly purified populations of neurons, astrocytes and oligodendrocytes. In: Conn PM, editor. Methods in Neurosciences, Cell. New York: Academic Press; 1990. p. 2. [Google Scholar]
- 73.Uchiyama M, Mihara M. Determination of malondialdehyde precursor in tissues by thiobarbituric acid test. Anal Biochem. 1978;86:271–278. doi: 10.1016/0003-2697(78)90342-1. [DOI] [PubMed] [Google Scholar]
- 74.Lowery OH, Rosenbrough NJ, Randall RJ. Protein measurement with Folin phenol reagent. J Biol Chem. 1995;1950:256–275. [PubMed] [Google Scholar]