Abstract
OBJECTIVE
Knee extensor weakness has not been associated consistently with the risk for incident knee pain. Additionally, the balance of hamstring:quadriceps strength (H:Q ratio) may affect risk and has not been studied. We determined whether knee extensor weakness or muscle imbalance is a risk factor for development of frequent knee pain or stiffness and whether the effect is modified by lower limb alignment.
DESIGN
Observational study
SETTING
Community
PARTICIPANTS
Community-dwelling adults age 50–79 with or at risk of knee OA based on obesity, knee injury or surgery. A total of 1269 knees from women and 1006 knees from men without frequent knee symptoms at baseline and with 15- or 30- month follow-up outcome data were included.
ASSESSMENT OF RISK FACTORS
Isokinetic knee extensor and flexor strength as well as radiographic hip-knee-ankle alignment were measured at baseline. H:Q ratio was dichotomized, with normal being considered to be ≥0.6.
MAIN OUTCOME MEASURMENTS
Frequent knee symptoms at 15- or 30-month follow-up (frequent knee pain, aching or stiffness on most days of the past month reported at both telephone contact just prior to and at visit.)
RESULTS
Mean+SD age was 62.2±8.0 and mean BMI was 30.1±5.4 kg/m2. Mean peak KES was 132.6±42.4 and 76.9±25.3 N•m in men and women respectively. Approximately 50% of knees in men and 59% of knees in women had an H:Q ratio <0.6. 307 out of 2275 eligible knees developed frequent knee symptoms at follow-up. Logistic regression controlling for age, BMI, femoral neck bone mineral density, activity score and baseline KL grade revealed that neither KES nor H:Q ratio predicted the development of knee symptoms in sex stratified or combined analyses. These results were unaffected by adjusting for lower limb alignment.
CONCLUSIONS
Neither concentric quadriceps strength nor hamstring:quadriceps ratios predicted the development of frequent knee symptoms at 15- or 30-month follow-up in this cohort.
Key terms: quadriceps muscle weakness, knee pain, hamstrings to quadriceps strength ratio, knee osteoarthritis
INTRODUCTION
Knee pain and stiffness is common in older adults[1–8] and is associated with reduced physical function[9], balance, lower extremity strength[10], and chronic disability[11, 12]. In patients with knee osteoarthritis (OA), pain is the symptom with the greatest impact on quality of life and the most common reason for health care visits. However, not all people with radiographic findings of knee OA have knee symptoms[13–17]. The reason that some people with radiographic knee OA develop knee pain while knee pain is absent in others remains unclear.
Several lines of evidence suggest that quadriceps weakness may play an important role in the development of knee symptoms. Quadriceps weakness is frequently reported in patients with knee OA and has been cross-sectionally associated with increased disability [18] and existing knee pain in some [19, 20] but not all studies [18, 21]. In addition, some studies indicate that knee pain may be reduced by strengthening the quadriceps muscle [22, 23]. Data on whether quadriceps weakness precedes the onset of knee pain are limited to one report [24]. Longitudinal investigations may advance understanding of the temporal relationship between quadriceps weakness and knee symptoms.
As lower limb musculature is the natural brace for the knee joint, muscle dysfunction may arise from either quadriceps weakness or relative weakness of the hamstrings in comparison to the quadriceps, usually assessed as the hamstrings:quadriceps (H:Q) ratio. An H:Q ratio less than 0.6 is considered to be abnormal [25–29], and an imbalance in strength between the quadriceps and the hamstrings could potentially contribute to knee symptoms through reducing knee joint stability [28]. Weak quadriceps may hinder load dissipation across the knee with decreased flexion during the weight acceptance phase of gait. Co-activation of the hamstrings during quadriceps activation reduces the net torque exerted by quadriceps. Individuals with knee OA have been found to walk with increased hamstring and quadriceps co-activation, stiffening the knee and increasing the joint contact stress [30]. Such increased contact stress potentially could lead to changes in the local joint environment associated with knee symptoms.
If quadriceps weakness or muscle imbalance predicts the development of knee symptoms (pain and stiffness on most days over the past month), then strengthening may serve as a focus for therapy to prevent knee symptoms in at-risk older adults. Therefore, we sought to determine whether quadriceps weakness is a risk factor for onset of frequent knee symptoms among older men and women without pre-existing knee pain or stiffness. We also examined whether participants with low H:Q ratios were at increased risk for incident knee symptoms.
METHODS
We analyzed data from the Multicenter Osteoarthritis (MOST) Study, a prospective, longitudinal study of risk factors for knee osteoarthritis (OA). The MOST cohort is composed of 3026 men and women between 50 and 79 years of age. Enrollment was from a volunteer sample of individuals from two communities and surrounding regions in Iowa and Alabama. Subjects were eligible if they had any of the following characteristics: were overweight or obese, had a history of knee injury that made it difficult to walk for at least one week, or had a previous knee surgery. Subjects were defined as overweight if they weighed more than the Framingham Study median weight for their age and sex-specific group [31]. The Institutional Review Boards at each of the investigators’ institutions approved this study. Written, informed consent was obtained from all participants using IRB-approved consent forms prior to initiating study procedures.
Initial Assessment of Knee Symptoms
Questions modified from the National Health and Nutrition Examination Survey [1] and the Framingham Osteoarthritis study [32] were used to determine the presence or absence of pre-existing, frequent knee symptoms. These questions were asked during both the telephone screen and baseline clinic visit. The median number of days between the telephone screen and the clinic visit was 34 days at baseline. A knee was considered to not have frequent symptoms if responses to the following questions were negative at the baseline phone screen and clinic visit respectively:
“During the past 30 days, have you had any pain, aching or stiffness in or around either knee?”
“During the past 30 days, have you had pain, aching or stiffness in or around your right/left knee on most days?”
Definition of Frequent Knee Symptom Development
At 15- and 30-months following the baseline assessment, participants completed a telephone screen interview and those with incident symptoms as well as control subjects attended a clinic visit. The same questions as those above were asked at these times. Participants who answered affirmatively at both the telephone interview and clinic visit were defined as having frequent knee symptoms in that knee at that follow-up visit. The outcome in this study was defined as the development of frequent knee symptoms at 15 or 30 months in a knee that did not have frequent symptoms at baseline. The median number of days between the telephone interview and the clinic visit was 29 days at 15 months and 31 days at 30 months.
Baseline Measurement of Lower Limb Strength and Muscle Balance
Isokinetic knee flexor and extensor strength were measured in both lower limbs at baseline (Cybex 350, HUMAC software version 4.3.2/Cybex 300 for Windows98, Avocent, Huntsville, AL). A ratio of the peak torque of the knee flexors to knee extensors (hamstrings:quadriceps ratio) was calculated. A low H:Q ratio was defined as less than 0.6 [25–27]. Knee extensor strength was recorded as the peak concentric torque at 60° per second. Trained dynamometer operators assessed knee extensor and flexor concentric torque according to the MOST strength testing protocol as previously described [33]. Quality control measures included certification of the testers in the MOST strength testing protocol, annual recertification, and a standardized script for subject testing. Test-retest reliability was assessed through repeating the protocol for isokinetic strength testing once each month for 3 months and yielded an ICC (95% CI) of .94 (.82–.99) and a COV of 8% (6–12%).
BMI Measurement
BMI (kg/m2) was calculated from baseline measurements of height (stadiometer, Holtain, Wales, UK) and weight (balance beam) as previously described [34].
Physical Activity
At baseline, participants completed the validated Physical Activity Scale for the Elderly (PASE: New England Research Institute, Watertown, MA) questionnaire, and activity scores were calculated [35].
Radiographic Measurement
Weight-bearing, semi-flexed posteroanterior [36] and lateral [37] views of the knees were obtained at baseline and scored (Kellgren-Lawrence) by two independent readers as previously described [34]. Radiographs of the contralateral knee were completed in participants with unilateral knee replacement.
Femoral Neck Bone Mineral Density (BMD)
As femoral neck BMD has been related to both knee extensor strength and incident OA, we controlled for BMD in our analyses. We obtained a bone mineral density scan of the proximal femur in participants without a history of bilateral hip replacement using dual energy x-ray absorptiometry (DXA, Hologic, 4500a and 4500w, Bedford, MA). Bone mineral density of the femoral neck region was recorded in g/cm2 [33].
Statistical Methods
Participant characteristics were summarized with frequencies and means.
We categorized knee extensor strength into sex-specific quartiles. The H:Q ratio was dichotomized with ≥0.6 being considered normal [25–27], and additional confirmatory analyses were performed using ≥0.8 as a cutoff for dichotomization [26]. Knee symptom statuses at both the 15- and 30-month visits were used in the analyses. We used a logistic regression model to assess the relationship between development of frequent knee symptoms and ipsilateral (a) baseline knee extensor strength, and (b) baseline H:Q ratio. Both sex stratified and combined analyses were completed. Adjusted analyses also controlled for age, BMI, femoral neck BMD, physical activity level (PASE) [35, 38], history of knee surgery, and radiographic OA status at baseline. In a separate model we also adjusted for malalignment status (≤5° varus, neutral, ≥5° valgus) at baseline. To assess for an interaction between strength and alignment, we entered both strength (sex-specific tertile for knee extensor strength, dichotomous variable for H:Q ratio), alignment (varus/valgus/neutral), and their interaction term in the multi-adjusted model. Use of generalized estimating equations (GEE) is an accepted statistical method for using weighted combinations of observations to extract the appropriate amount of information, providing conservative calculations of standard errors in datasets with clusters of correlated data [39]. Thus, we used GEE to adjust for the correlation of knee symptom status between knees and visits within each subject.
RESULTS
Study Population
A total of 1308 out of 3026 participants reported knee symptoms at either telephone screen or screening clinic visit in both knees at baseline as described below and were excluded. As shown in Figure 1, an additional 122 participants were excluded at baseline due to inflammatory arthritis, missing muscle strength or radiographic data, or pain that prevented pushing during the strength measurement. 1540 men and women (2275 knees, 1269 in women and 1006 in men) without knee symptoms in at least one knee at baseline were evaluated for the development of frequent knee symptoms. Among the 1540 subjects eligible for the study, 20.2% had consistent frequent symptoms in the contralateral knee on both the phone screen and clinic visit and 23.3% had inconsistent frequent knee symptoms (yes at either the phone screen or clinic visit) at baseline.
Figure 1.
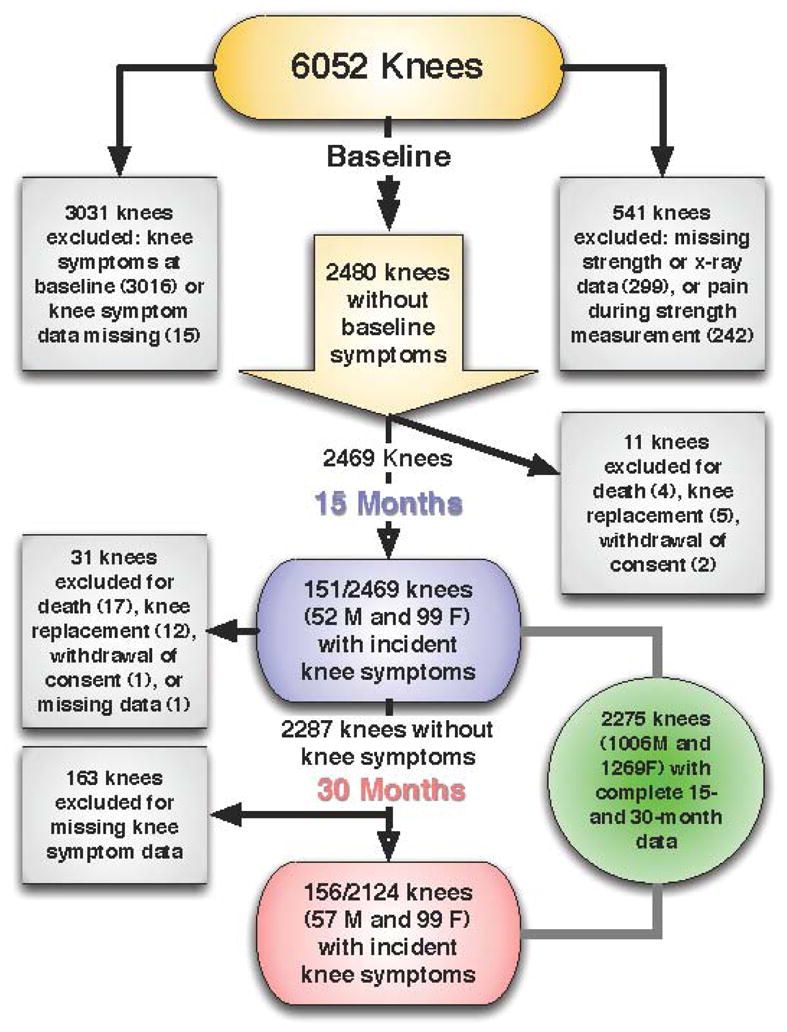
Subject Inclusion Diagram
All of these participants completed the 15-month follow-up visit while 20 participants withdrew consent or died prior to the 30-month visit. Excluded from the knee-based analyses were 3031 knees with symptoms at baseline, 507 knees with missing data in lower limb muscle strength or who reported pain when measuring muscle strength, 4 knees with missing data on baseline radiograph, 48 knees that had been replaced (30 at baseline, 5 before 15-month visit, and 13 before 30-month visit), 21 knees from participants who died before follow-up (4 before 15-month and 17 before 30-month visit), 3 knees from participants who withdrew consent during follow-up, and 163 knees that had incomplete knee pain surveys at 30-month follow-up visit. There were no significant differences in baseline age, BMI, or physical activity levels between participants who completed the study and those who did not.
Baseline characteristics of subjects are summarized in Table 1. At baseline, the mean knee extensor strength was 76.9±25.3 N•m in women, and 132.6±42.4 N•m in men. Over half of the knees in the women (58.9%) and the men (50%) had a baseline H:Q ratio <0.6 (Table 1).
Table 1. Baseline Characteristics.
(n=1540 subjects, 2275 knees.)
| Age (years) | BMI(Kg/m2) | KOOS score | PASE score | KL grade ≥2(%) | KES(N•m) | H:Q Ratio<0.6 (%) | |
|---|---|---|---|---|---|---|---|
| Men n=668 (1006 knees) | 61.8 ± 8.2 | 30.2 ± 4.8 | 5.1 ± 4.8 | 205.5 ± 94.0 | 22.5% | 132.6±42.4 | 50.0% |
| Women N =872 (1269 knees) | 62.5 ± 7.8 | 30.0 ± 5.8 | 5.7 ± 5.2 | 162.4 ± 77.8 | 25.5% | 76.9±25.3 | 58.6% |
• Mean±SD unless otherwise specified
A total of 109 out of 1006 knees (10.8%) in the men and 198 out of 1269 (15.6%) knees in the women developed frequent knee symptoms at follow-up. Mean BMI was slightly greater in women who developed knee symptoms (30.8 ± 6.0 kg/m2) compared with those who did not (29.8 ± 5.8 kg/m2, p>.05. A similar trend was observed in men, with those who developed knee symptoms having a mean BMI of 31.0 ± 6.1 kg/m2 and those who did not having a mean BMI of 30.1 ± 4.6 kg/m2, (p>.15). 42% of women and 24% of men with knee symptoms at follow-up also had radiographic knee OA at baseline while only 21% of women and 20% of men without frequent knee symptoms at follow-up had radiographic knee OA. The difference was significant in women (p<.0001) but not men (p>.34).
Knee Extensor Strength
As shown in Table 2, knee extensor strength categorized by tertiles or as a continuous variable was not predictive of development of knee symptoms at either 15 or 30 months either before or after adjusting for age, BMI, femoral neck BMD, KL grade, physical activity level and lower limb malalignment in men or women analyzed separately or combined. No significant interaction was observed among women or for men and women combined. In men, there were only 3 valgus knees in the highest tertile of knee extensor strength. None of these developed frequent symptoms, so the model with interaction term did not converge.
Table 2.
Quadriceps muscle strength association with incident knee symptoms
| Sex-specific tertiles | N of cases (%) | OR (95% CI), adjusting age, BMI, BMD, PASE, surgery, and KL at baseline | OR (95% CI), adjusting age, BMI, BMD, PASE, surgery, KL, and alignment at baseline | |
|---|---|---|---|---|
| Men | Lowest, 12–112 N•m (n=329) | 38 (11.6) | 1.00 (reference) | 1.00 (reference) |
| Middle, 113–148 N•m (n=344) | 40 (11.6) | 1.01 (0.62, 1.65) | 1.06 (0.64, 1.76) | |
| Highest, 149–276 N•m (n=333) | 31 (9.3) | 0.70 (0.38, 1.29) | 0.80 (0.43, 1.47) | |
| P for linear trend | 0.1117 | 0.2378 | ||
| 1SD | 0.82 (0.64, 1.05) | 0.86 (0.66, 1.11) | ||
| Women | Lowest, 12–64 N•m (n=415) | 76 (18.3) | 1.00 (reference) | 1.00 (reference) |
| Middle, 65–86 N•m (n=426) | 60 (14.1) | 0.79 (0.54, 1.16) | 0.81 (0.55, 1.20) | |
| Highest, 87–206 N•m (n=428) | 62 (14.5) | 0.75 (0.48, 1.17) | 0.80 (0.51, 1.24) | |
| P for linear trend | 0.5493 | 0.7739 | ||
| 1SD | 0.94 (0.77, 1.15) | 0.97 (0.80, 1.18) | ||
| All | Lowest (n=744) | 114 (15.3) | 1.00 (reference) | 1.00 (reference) |
| Middle (n=770) | 100 (13.0) | 0.85 (0.63, 1.15) | 0.88 (0.65, 1.20) | |
| Highest (n=761) | 93 (12.2) | 0.72 (0.51, 1.03) | 0.79 (0.55, 1.13) | |
| P for linear trend | 0.1097 | 0.2579 |
• using GEE to adjust correlations between knees
•P value for interaction between quadriceps muscle strength and malalignment was >0.4 among all subjects, and for each strata in which it could be estimated.
Hamstring:Quadriceps Ratio
In men and women, a hamstring:quadriceps strength ratio < 0.6 adjusted for age, BMI, femoral neck BMD, KL grade, knee joint malalignment and physical activity did not predict development of frequent knee symptoms at the 15– or 30–month follow-up visits (Table 3.) Use of an alternative cut-off for hamstring:quadriceps ratio (<0.8) also was not associated with the development of frequent knee symptoms. Hamstring:quadriceps ratio was not a statistically significant predictor of development of knee symptoms in combined or sex-stratified analyses. As for knee extensor strength, interaction terms with alignment were not significant for women alone or in combined analyses and were not possible to assess in men alone.
Table 3.
Hamstring: quadriceps ratio association with incident knee symptoms
| Gender-specific cut-offs | N of cases (%) | OR (95% CI), adjusting age, BMI, BMD, PASE, and KL at baseline | OR (95% CI), adjusting age, BMI, BMD, PASE, KL, and alignment at baseline | |
|---|---|---|---|---|
| Men | <0.6 (504) | 55 (10.9) | 1.00 (reference) | 1.00 (reference) |
| ≥0.6(502) | 54 (10.8) | 1.03 (0.68, 1.57) | 0.92 (0.61, 1.41) | |
| Women | <0.6 (744) | 115 (15.5) | 1.00 (reference) | 1.0 (reference) |
| ≥0.6(525) | 83 (15.8) | 1.05 (0.77,1.43) | 1.06 (0.78, 1.43) | |
| All | <0.6 (1248) | 170 (13.6) | 1.00 (reference) | 1.00 (reference) |
| ≥0.6(1027) | 137 (13.3) | 1.04 (0.81,1.33) | 1.00 (0.79, 1.30) |
• using GEE to adjust for correlations between knees
• P value for interaction between quadriceps muscle strength and malalignment: >0.2 among all subjects and for each strata in which it could be estimated.
DISCUSSION
In this study of community-dwelling adults, the main finding is that higher knee extensor strength did not appear to reduce risk for the development of frequent knee symptoms over 30-months. This result does not support the supposition that quadriceps muscle weakness may precede knee pain [40]. In another longitudinal study, baseline muscle strength contributed to neither incident nor progressive knee pain, though findings may have been limited by a small number of cases (16 women and 2 men with incident knee OA and 25 women and 9 men with progression) [21]. Our findings added additional information in that we found no evidence that imbalance of quadriceps and hamstrings strength at baseline contributed to incident knee symptoms at follow-up.
Strength determinations may have been a source of differing results with Slemenda et al, who adjusted strength by dividing knee extensor strength by body weight, assuming a linear ratio between strength and body size. In contrast, we used regression to control for BMI without assuming a linear ratio whereby strength would be expected to double with a doubling of body mass. Participants in our study were also younger by 8–10 years and as a result, possibly stronger. Muscle strength is known to decline with age [41] and individuals age 65 and older, as they develop knee pain, may experience significant reductions in strength over 30 months [10].
Although quadriceps strength was not protective against incident knee symptoms in this cohort, quadriceps muscle weakness remains a biologically plausible contributor to knee pain. During gait, the quadriceps muscle acts as a shock absorber and decreases loading rates. Increased loading rates, which may be harmful to the knee joint, have been found to be higher in individuals with knee pain compared with controls and are associated with knee OA [42]. In addition, there are numerous reports that exercise reduces knee pain [22, 23] and evidence that women who participated in strength training had lower rates of knee loading compared with sedentary controls [43]. Considering that reversal of weakness reduces knee pain, these reports may suggest that quadriceps muscle weakness is a contributor to knee pain. However, there are also numerous effects of exercise other than increased strength that could explain the pain-reduction effect, such as endorphin release, increased joint flexibility, improved sleep quality, improved fitness with increased energy level, weight loss reducing loading, improved tissue oxygenation, or increased central nervous system seratonin levels with enhanced mood. Furthermore, reducing pain in those who already have it may differ from preventing development of pain in those who do not.
Patients with knee OA commonly experience knee pain, but knee pain and/or stiffness may occur in the absence of radiographic knee osteoarthritis. According to a recent study, non-articular conditions such as widespread pain, low back pain with index leg referral, full-leg pain, hip arthritis, or bursitis were found commonly in older adults with knee pain and thought to bring about knee pain in addition to that due to radiographic knee OA alone [44]. This may help to explain why 72% of knees in men and 57% of knees in women that developed new knee pain had a KL grade <2 at baseline.
In the present study, participants were directly queried for the presence or absence of knee symptoms on most days of the preceding month at 3 exams: baseline, 15- and 30-months. For each exam, we asked subjects at two time-points, one by phone and another at the clinic approximately 1 month later. A potential limitation to this method of assessment is that intermittent symptoms may go unreported and there is no differentiation between participants with severe pain and those with mild or moderate pain. In addition, knee symptoms may resolve over time [45] or participants may avoid pain-inducing activities. While, our assessment of knee symptoms at two separate time points would be expected to reduce the likelihood of missed incident symptoms in participants in comparison with a single assessment there remains the possibility that some knees are misclassified with respect to the development of pain.
One additional difference in our study, in comparison with prior studies was the use of the cutoff of .6 for a concentric:concentric H:Q ratio [26]. Eccentric isokinetic strength testing involves maximal activation of the quadriceps while the knee is rapidly forced into flexion. This is known to be very challenging for healthy adults and could potentially injure older adults with knee OA. Therefore, for safety reasons, we elected to use a concentric:concentric H:Q ratio. In addition, studies of the H:Q ratio have been reported for younger adults. Therefore, normal values appropriate to our participants over age 50 were not available. We prospectively selected .6 as a cutoff, as this has been reported for younger adults [26], and then completed a sensitivity analysis using .8 as the cutoff [46], which also demonstrated lack of association with incident symptoms.
Since symptoms prompt clinical presentation, we prospectively chose to study whether strength led to incident symptoms. Although strength was not found to confer protection against incident knee symptoms in this population, these results do not preclude the possibility of other potential benefits of lower limb strength, such as effects on functional limitations or disability. In addition, this study used an isokinetic dynamometer to measure strength in a reliable, consistent manner. However, more functional measures of strength in future studies may further advance understanding.
There are several unique features of the MOST cohort that were strengths of this study. First, pain was not a confounder for strength since subjects who reported knee symptoms at baseline were not eligible to develop incident knee symptoms. Second, we utilized a community cohort from two regions in the United States and results are likely to be generalizable to adults with risk factors for knee OA. We also enrolled subjects at high risk of incident or progressive OA with 49.1% having a BMI ≥30. This is higher than the prevalence of obesity 31–40% for people age 50 and over in the United States [47, 48], but likely still contributes to the generalizability of the present findings, as there is a higher prevalence of obesity in people at risk for incident knee pain. In addition, the baseline characteristics of subjects who did not complete the study were similar to those who completed the study, strengthening internal validity. Finally, the availability of data for 6052 knees, and inclusion of 2275 knees of adults in the at-risk age group enhanced the power of this study to detect an association between knee extensor weakness and incident symptoms.
In conclusion, we found that neither concentric quadriceps strength nor hamstrings to quadriceps strength ratios predicted incident knee symptoms at 15- or 30-month follow-up.
Acknowledgments
The authors thank the participants and staff of the Multicenter Osteoarthritis (MOST) Study. This work was funded by the following NIH grants: U01 AG18820, R01 HD43502; U01 AG18832, U01 AG18947, U01 AG19069, and the Paul B. Beeson Career Development Awards Program (K23AG030945).
Abbreviations
- KL
Kellgren-Lawrence grade
- BMI
body mass index
- BMD
bone mineral density
- PASE
Physical Activity Scale for the Elderly
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Davis MA, Ettinger WH, Neuhaus JM, Barclay JD, Segal MR. Correlates of knee pain among US adults with and without radiographic knee osteoarthritis. J Rheumatol. 1992;19:1943–1949. [PubMed] [Google Scholar]
- 2.Dawson J, Linsell L, Zondervan K, et al. Epidemiology of hip and knee pain and its impact on overall health status in older adults. Rheumatology (Oxford) 2004;43:497–504. doi: 10.1093/rheumatology/keh086. [DOI] [PubMed] [Google Scholar]
- 3.Andersen RE, Crespo CJ, Ling SM, Bathon JM, Bartlett SJ. Prevalence of significant knee pain among older Americans: results from the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 1999;47:1435–1438. doi: 10.1111/j.1532-5415.1999.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell HL, Carr AJ, Scott DL. The management of knee pain in primary care: factors associated with consulting the GP and referrals to secondary care. Rheumatology (Oxford) 2006;45:771–776. doi: 10.1093/rheumatology/kei214. [DOI] [PubMed] [Google Scholar]
- 6.Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain. 2002;100:55–64. doi: 10.1016/s0304-3959(02)00239-7. [DOI] [PubMed] [Google Scholar]
- 7.Jinks C, Jordan K, Ong BN, Croft P. A brief screening tool for knee pain in primary care (KNEST). 2. Results from a survey in the general population aged 50 and over. Rheumatology (Oxford) 2004;43:55–61. doi: 10.1093/rheumatology/keg438. [DOI] [PubMed] [Google Scholar]
- 8.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community: (KNEST 3) Rheumatology (Oxford) 2007;46:877–881. doi: 10.1093/rheumatology/kem013. [DOI] [PubMed] [Google Scholar]
- 10.Messier SP, Glasser JL, Ettinger WH, Jr, Craven TE, Miller ME. Declines in strength and balance in older adults with chronic knee pain: a 30-month longitudinal, observational study. Arthritis Rheum. 2002;47:141–148. doi: 10.1002/art.10339. [DOI] [PubMed] [Google Scholar]
- 11.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall MC, Mockett SP, Doherty M. Relative impact of radiographic osteoarthritis and pain on quadriceps strength, proprioception, static postural sway and lower limb function. Ann Rheum Dis. 2006;65:865–870. doi: 10.1136/ard.2005.043653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27:1513–1517. [PubMed] [Google Scholar]
- 14.McAlindon T, Zhang Y, Hannan M, et al. Are risk factors for patellofemoral and tibiofemoral knee osteoarthritis different? J Rheumatol. 1996;23:332–337. [PubMed] [Google Scholar]
- 15.Lawrence JS, Bremner JM, Bier F. Osteoarthrosis. Prevalence in the population and relationship between symptoms and x-ray changes. Ann Rheum Dis. 1966;25:1–24. [PMC free article] [PubMed] [Google Scholar]
- 16.Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004;18:793–800. doi: 10.1191/0269215504cr754oa. [DOI] [PubMed] [Google Scholar]
- 17.Creamer P, Lethbridge-Cejku M, Hochberg MC. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology (Oxford) 2000;39:490–496. doi: 10.1093/rheumatology/39.5.490. [DOI] [PubMed] [Google Scholar]
- 18.Steultjens MP, Dekker J, van Baar ME, Oostendorp RA, Bijlsma JW. Muscle strength, pain and disability in patients with osteoarthritis. Clin Rehabil. 2001;15:331–341. doi: 10.1191/026921501673178408. [DOI] [PubMed] [Google Scholar]
- 19.Hall MC, Mockett SP, Doherty M. Relative impact of radiographic osteoarthritis and pain on quadriceps strength, proprioception, static postural sway and lower limb function. Ann Rheum Dis. 2006;65:865–870. doi: 10.1136/ard.2005.043653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madsen OR, Bliddal H, Egsmose C, Sylvest J. Isometric and isokinetic quadriceps strength in gonarthrosis; inter-relations between quadriceps strength, walking ability, radiology, subchondral bone density and pain. Clin Rheumatol. 1995;14:308–314. doi: 10.1007/BF02208344. [DOI] [PubMed] [Google Scholar]
- 21.Brandt KD, Heilman DK, Slemenda C, et al. Quadriceps strength in women with radiographically progressive osteoarthritis of the knee and those with stable radiographic changes. J Rheumatol. 1999;26:2431–2437. [PubMed] [Google Scholar]
- 22.Baker K, McAlindon T. Exercise for knee osteoarthritis. Curr Opin Rheumatol. 2000;12:456–463. doi: 10.1097/00002281-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Thomas KS, Muir KR, Doherty M, Jones AC, O’Reilly SC, Bassey EJ. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. Bmj. 2002;325:752. doi: 10.1136/bmj.325.7367.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slemenda C, Brandt KD, Heilman DK, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127:97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 25.Read MT, Bellamy MJ. Comparison of hamstring/quadriceps isokinetic strength ratios and power in tennis, squash and track athletes. Br J Sports Med. 1990;24:178–182. doi: 10.1136/bjsm.24.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aagaard P, Simonsen EB, Magnusson SP, Larsson B, Dyhre-Poulsen P. A new concept for isokinetic hamstring: quadriceps muscle strength ratio. Am J Sports Med. 1998;26:231–237. doi: 10.1177/03635465980260021201. [DOI] [PubMed] [Google Scholar]
- 27.Aagaard P, Simonsen EB, Trolle M, Bangsbo J, Klausen K. Isokinetic hamstring/quadriceps strength ratio: influence from joint angular velocity, gravity correction and contraction mode. Acta Physiol Scand. 1995;154:421–427. doi: 10.1111/j.1748-1716.1995.tb09927.x. [DOI] [PubMed] [Google Scholar]
- 28.Coombs R, Garbutt G. Developments in the use of the hamstring/quadriceps ratio for the assessment of muscle balance. Journal of Sports Science & Medicine. 2002;1:56–62. [PMC free article] [PubMed] [Google Scholar]
- 29.Heiser TM, Weber J, Sullivan G, Clare P, Jacobs RR. Prophylaxis and management of hamstring muscle injuries in intercollegiate football players. Am J Sports Med. 1984;12:368–370. doi: 10.1177/036354658401200506. [DOI] [PubMed] [Google Scholar]
- 30.Schmitt LC, Rudolph KS. Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Care & Research. 2007;57:1018–1026. doi: 10.1002/art.22889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 32.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 33.Segal NA, Torner JC, Yang M, Curtis JR, Felson DT, Nevitt MC. Muscle Mass Is More Strongly Related to Hip Bone Mineral Density Than Is Quadriceps Strength or Lower Activity Level in Adults Over Age 50Year. J Clin Densitom. 2008 doi: 10.1016/j.jocd.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Segal NA, Felson DT, Torner JC, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88:988–992. doi: 10.1016/j.apmr.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 36.Nevitt MC, Peterfy C, Guermazi A, et al. Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum. 2007;56:1512–1520. doi: 10.1002/art.22557. [DOI] [PubMed] [Google Scholar]
- 37.LaValley MP, McLaughlin S, Goggins J, Gale D, Nevitt MC, Felson DT. The lateral view radiograph for assessment of the tibiofemoral joint space in knee osteoarthritis: its reliability, sensitivity to change, and longitudinal validity. Arthritis Rheum. 2005;52:3542–3547. doi: 10.1002/art.21374. [DOI] [PubMed] [Google Scholar]
- 38.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 39.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 40.Slemenda C, Heilman DK, Brandt KD, et al. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41:1951–1959. doi: 10.1002/1529-0131(199811)41:11<1951::AID-ART9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 41.Schiller BC, Casas YG, Tracy BL, DeSouza CA, Seals DR. Age-related declines in knee extensor strength and physical performance in healthy Hispanic and Caucasian women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2000;55:B563–569. doi: 10.1093/gerona/55.12.b563. [DOI] [PubMed] [Google Scholar]
- 42.Radin EL, Rose RM. Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res. 1986:34–40. [PubMed] [Google Scholar]
- 43.Mikesky AE, Meyer A, Thompson KL. Relationship between quadriceps strength and rate of loading during gait in women. J Orthop Res. 2000;18:171–175. doi: 10.1002/jor.1100180202. [DOI] [PubMed] [Google Scholar]
- 44.Wood LR, Peat G, Thomas E, Duncan R. The contribution of selected non-articular conditions to knee pain severity and associated disability in older adults. Osteoarthritis Cartilage. 2008;16:647–653. doi: 10.1016/j.joca.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 45.Felson DT. The course of osteoarthritis and factors that affect it. Rheum Dis Clin North Am. 1993;19:607–615. [PubMed] [Google Scholar]
- 46.Aagaard P, Simonsen EB, Beyer N, Larsson B, Magnusson P, Kjaer M. Isokinetic muscle strength and capacity for muscular knee joint stabilization in elite sailors. Int J Sports Med. 1997;18:521–525. doi: 10.1055/s-2007-972675. [DOI] [PubMed] [Google Scholar]
- 47.HHS. With understanding and improving health and objectives for improving health. Washington (DC): 2000. [Google Scholar]
- 48.Obesity Among Adults in the United States--No Statistically Significant Change Since 2003–2004. 2007:8. [PubMed] [Google Scholar]


