Abstract
Objective
The socio-communicative abnormalities of young children with Williams syndrome (WS) with limited language were compared to those of children with clinical diagnoses of Autism, Pervasive-Developmental Disorder – Not Otherwise Specified (PDD-NOS), or nonspectrum developmental disability.
Method
Participants were 30 children with WS and individually matched groups of participants with autism (n = 28), PDD-NOS (n = 17), and mixed etiology nonspectrum developmental disabilities (ME group; n = 16). The autism, PDD-NOS and ME groups were matched individually to the children with WS for age, gender, and developmental level. All participants were administered the Autism Diagnostic Observation Schedule Module 1 and the Mullen Scales of Early Learning.
Results
As a group, children with WS with limited language showed fewer socio-communicative abnormalities than children with autism, about the same level as children with PDD-NOS, and more abnormalities in reciprocity social interaction than participants in the ME group. Examination of the subgroup of participants with WS matched and compared to children with PDD-NOS indicated that half showed fewer abnormalities than their individual matches with PDD-NOS, while half of the children with WS showed more abnormalities than their matches with PDD-NOS.
Conclusion
Socio-communicative difficulties are present for many children with WS and overlap with the autism spectrum. The results of this investigation suggest that these abnormalities are not accounted for by developmental delay alone, and care should be taken to avoid diagnostic overshadowing in young children with WS.
Keywords: Williams syndrome, Autism, PDD-NOS, developmental disability, ADOS
Williams syndrome (WS) is a neurodevelopmental disorder resulting from a hemizygous microdeletion of ~25 genes on chromosome 7q11.23 (1). Individuals with WS have distinctive medical and cognitive profile (2). Compared to children with other types of developmental disorders, children with WS are less reserved toward strangers, more approaching, more gregarious, overly friendly, and affectionate (see review in 3). These prosocial behaviors make it unlikely that one would suspect overlap with the autism spectrum. However, there is also evidence that children with WS experience difficulties with social interaction and social communication. Parents often report that their children with WS are often not attuned to others socially and experience difficulties establishing and maintaining friendships (4, 5) Significant conversational deficits (6), poor social skills (7), poor understanding of socially-relevant information (8, 9), and restricted interests (10) have been observed. Delayed language and gestural development are described (see review in 11).
Hence, many of the socio-communicative and behavioral difficulties observed are also characteristic of children with autism spectrum disorders (ASD) and may not be accounted for by developmental delay alone. Gillberg and Rasmussen (12) state, “…it is clear from the results of these preliminary investigations that this patient group [WS] does have several problems seen in autism. Included in this catalogue are hyperacusis, social isolation, and other types of social impairment…, distractibility, inflexibility, ritualism, obsessiveness, and pragmatic deficits…, all of which can be hallmarks of the autistic syndrome” (p. 382). There have been a few reports of children diagnosed with both WS and autism (12–16). Given the prevalence of WS (1 in 7,500 live births) (17) and the recently reported prevalence of ASD placed at 1 in 150 (18), it would be expected that some individuals with WS would also have an ASD. A recent investigation comparing the performance of young children with WS on the ADOS to participants with clinical diagnoses of autism (16) found that although participants with WS showed a number of socio-communicative deficits, they could reliably be distinguished from participants with clinical diagnoses of autism and had considerably fewer socio-communicative deficits. Ten percent of their sample of young children with WS met DSM-IV criteria for autism.
The possibility of overlap between children with WS and children with clinical diagnoses of PDD-NOS has not examined, however. The DSM-IV category of PDD-NOS is quite heterogeneous, with more varied ways to meet the diagnostic criteria for PDD-NOS than for Autistic Disorder. Although difficulties with social reciprocity need to be present for a diagnosis of PDD-NOS, some children with PDD-NOS do not have significant deficits in communication or do not show restricted and repetitive behaviors. Additionally, the nature of the socio-communicative deficits of people with PDD-NOS can be milder than for autism. Relatedly, individuals falling within the “Active But Odd” autism subtype do not necessarily avoid social interaction or prefer solitary activity (19, 20). Given the reported pattern of behavioral characteristics of young children with WS, they may be more likely to show overlap with the milder diagnostic category of PDD-NOS rather than with autism, which is characterized by more severe socio-communicative deficits.
Using the Autism Diagnostic Observation Schedule (ADOS) to assess the socio-communicative behavior of young children with WS with limited language (21), we recently found evidence of socio-communicative deficits overlapping with those typically seen in children with ASD. In the current investigation, we further examine how these difficulties compare to those of individually matched participants with autism, PDD-NOS, or developmental disabilities of other etiologies without spectrum diagnoses. Comparison to the Mixed Etiology (ME) group enables identification of the deficits of children with WS that are not explained by developmental delay alone. Comparisons to the PDD-NOS (PDD) and Autism (AUT) groups enable further exploration of the possibility that young children with WS show socio-communicative deficits that overlap with the autism spectrum.
Method
Participants
Thirty children with genetically-confirmed WS aged 2½ – 5½ years were assessed. The performance of 29 of these children was described in Klein-Tasman, Mervis, Lord et al. (21). One additional child subsequently assessed was also included, leading to a full sample of 30 children with WS (WS group). The ADOS classifications1 of these 30 participants were as follows: 3 Autism (A), 12 Autism Spectrum (AS), and 15 “nonspectrum.” Subsets of these participants were individually matched to 16 children with other developmental disabilities who do not have spectrum diagnoses (ME group); 17 children with clinical diagnoses of PDD-NOS (PDD group); and 28 children with clinical diagnoses of Autism (AUT group). Individual matches were made based on gender, CA (within 4 months), and intellectual abilities (Mullen Early Learning Composite (ELC) within ½ standard deviation for those above floor performance, age equivalent within 4 months for those at floor2). When more than one potential match existed, the closest match was used. See Table 1 for CA, gender, and age equivalent descriptive statistics related to the matched groups. All participants met the language use criteria for administration of Module 1 of the ADOS. The native language of all participants was English. Information about racial/ethnic background was available for 87 participants (97%). The constitution of the sample was 86% Caucasian, 1% Hispanic, 5% Asian, and 8% African American. Information regarding maternal education was available for 78 participants (87%). Of these mothers, 51% had a college degree, an additional 46% had graduated from high school, and 3% had not completed high school. No child had had cardiac surgery within the previous 6 months.
Table 1.
Descriptive statistics for whole Williams syndrome group and matched Mixed Etiology, PDD-NOS, and Autism groups
| Whole Williams Syndrome Group | ||
| WS (n = 30) | ||
| Gender | 19 male, 11 female | |
| Mean CA in months (range) | 41.23 (30–63) | |
| Mean AE (range) | 22.23 (12.5–35.5) | |
| Mean Mullen ELC (range) | 58.37 (49–99) | |
| Williams Syndrome/Mixed Etiology Matched Groups | ||
| WS (n = 16) | ME (n = 16) | |
| Gender | 11 male, 5 female | 11 male, 5 female |
| Mean CA in months (range) | 40.44 (33–63) | 41.63 (31–60) |
| Mean AE (range) | 23.30 (13–35.5) | 22.92 (10–35.75) |
| Mean Mullen ELC (range) | 61.63 (49–99) | 58.15 (49–100) |
| Williams Syndrome/PDD-NOS Matched Groups | ||
| WS (n = 17) | PDD-NOS (n = 17) | |
| Gender | 12 male, 5 female | 12 male, 5 female |
| Mean CA in months (range) | 42.65 (31–63) | 43.35 (35–61) |
| Mean AE (range) | 21.53 (12.5–31.25) | 21.29 (9–32) |
| Mean Mullen ELC (range) | 55.65 (49–73) | 54.33 (49–71) |
| Williams Syndrome/Autism Matched Groups | ||
| WS (n = 28) | AUT (n = 28) | |
| Gender | 18 male, 10 female | 18 male, 10 female |
| Mean CA in months (range) | 41.68 (30–63) | 41.00 (30–62) |
| Mean AE (range) | 21.57 (12.5–31.25) | 21.09 (11.5–32.25) |
| Mean Mullen ELC (range) | 56.29 (49–76) | 55.78 (49–86) |
Note. WS = Williams syndrome; PDD-NOS = Pervasive Developmental Disorder – Not Otherwise Specified; AUT = Autism; AE = Average age equivalent in months of Mullen subdomains; ELC = Early Learning Composite standard score.
Participants in the WS group were recruited through the Williams Syndrome Association or through C. Mervis’s longitudinal project at the University of Louisville (UofL) and were assessed at local and national conferences, as well as at the University of Wisconsin – Milwaukee and UofL. Two participants in the ME group were recruited by contacting Milwaukee area early intervention organizations and affiliated professionals and requesting permission to supply them with flyers describing the project to distribute to potential participants. In addition, 3 participants were recruited from the UofL longitudinal project described above; this project also includes children with other developmental disabilities. Eleven children with developmental disabilities of mixed etiology were assessed by C. Lord’s group. The ME group consisted of 11 children with developmental disability of unknown etiology, 3 with Down syndrome, and 2 with Kabuki syndrome.
Participants in the PDD and AUT groups were clinically diagnosed by experienced clinicians according to DSM-IV criteria on the basis of administration of the Autism Diagnostic Interview – Revised (23) and the ADOS, as well as developmental testing and general clinical interview. Examiners were certified in the use of the ADI-R and ADOS for research. None of the participants in the PDD or AUT groups had been diagnosed with a genetic disorder.
Measures
Autism Diagnostic Observation Schedule, Module 1
The Autism Diagnostic Observation Schedule (ADOS: 24) is a structured, play-like interaction with an examiner designed to assess abnormalities in communication, reciprocal social interaction, creativity and imagination, and the presence of “restricted and repetitive behaviors.” Module 1 is administered to children with no language or beginning language skills (maximum of simple phrases). The examiner engages in a set of play activities designed to elicit social communication (e.g., bubble play, pretend birthday party, activation of motorized bunny). Individual target behaviors (e.g., eye contact, gestures, pointing) are coded according to operational definitions chosen to capture abnormalities typically seen in children with ASD. Behavior clearly indicating abnormality according to the operational definition provided is scored 2 or 3, depending on severity. Behavior that shows no indication of abnormality is scored 0. Behavior indicating more mild abnormality (with clear criteria specific to each item) is scored 1. A subset of the items scored makes up the “ADOS Algorithm,” empirically derived during the validation of the ADOS to distinguish between children with ASDs and children without ASDs. Two cutoffs are available for the Deficits in Communication (COM) domain and the Deficits in Reciprocal Social Interaction (SOC) domain, as well as for the Total algorithm score (TOT): one to identify children with behavior likely indicative of “autism” (A) and one to identify children with deficits likely indicative of a milder autism spectrum disorder “PDD-NOS” (AS). In addition, although not factored into the diagnostic algorithm, scores are available for Imagination and Creativity (Play) and for Restricted and Repetitive Interests (RR). The ADOS was administered and scored according to standardization by certified examiners.
Mullen Scales of Early Learning
The Mullen (25) is an individually administered measure of intellectual abilities for infants, toddlers, and preschoolers consisting of four core subtests measuring visual reception and nonverbal reasoning (VR), fine motor skills (FM), receptive language (RL), and expressive language (EL). T-scores and age equivalent (AE) scores are yielded for subtests and an “Early Learning Composite” provides an overall developmental quotient.
Results
Comparison to ME Group
Individual matches with non-spectrum developmental disabilities of mixed etiology (ME group) were identified for 16 participants with WS. As indicated in Table 2, the distribution of classifications on the ADOS was significantly different for the WS and the ME groups (χ2(2) = 6.02, p = .049). Wilcoxon Signed Ranks tests were conducted to evaluate group differences in algorithm scores. The two groups did not differ significantly in COM. However, the children with WS showed significantly more abnormality than the ME group on all of the remaining algorithm totals, including SOC, TOT, RR, and Play (see Table 3). For the item-level analyses, an alpha level of .01 was used due to the number of comparisons conducted. (See Table 4 for a summary of the item results and Supplementary Table 1 for detailed descriptive and inferential item statistics.) Results of the t-tests indicated a significant group difference for two items, Unusual Eye Contact (t (14) = 3.42, p =.004, Hedges g = .81) and Imagination/Creativity (t (14) = 4.57, p < .001, Hedges g = 1.08), with the WS group demonstrating greater abnormality for both. Given that the Unusual Eye Contact item showed a much larger effect size than any of the other algorithm items, group differences in algorithm scores (Social and Total) with this item removed were examined, with persistent significant differences found (See Table 3).
Table 2.
Distributions of ADOS classification for matched participant groups.
| Groups Compared | ADOS Classification | |||
|---|---|---|---|---|
|
WS/ME (n = 16) |
Autism | AS | Nonspectrum | |
| WS | 1 | 7 | 8 | |
| ME | 2 | 1 | 13 | |
|
WS/PDD-NOS (n = 17) |
Autism | AS | Nonspectrum | |
| WS | 2 | 6 | 9 | |
| PDD-NOS | 4 | 6 | 7 | |
|
WS/Autism (n = 28) |
Autism | AS | Nonspectrum | |
| WS | 3 | 11 | 14 | |
| Autism | 25 | 3 | 0 | |
WS = Williams syndrome; ME = Mixed etiology; PDD-NOS = children with clinical diagnoses of Pervasive Developmental Disorder-Not Otherwise Specified; Autism = children with clinical diagnoses of autism; AS = Autism Spectrum
Table 3.
Matched group comparisons of ADOS mean algorithm scores (SD in parentheses).
| WS/ME Comparison | ||||||
|---|---|---|---|---|---|---|
| WS mean(SD) |
ME mean(SD) |
Wilcoxon z |
p | Hedge’s g (effect size) |
||
| Communication | 2.31 (1.89) | 2.13 (2.13) | .60 | .548 | 0.12 | |
| Social | 4.88 (3.65) | 2.44 (3.50) | 2.63 | .009 | ** | 0.77 |
| Total | 7.19 (5.24) | 4.56 (5.37) | 2.59 | .010 | * | 0.62 |
| R/R Interests | 2.75 (1.92) | 1.63 (1.86) | 2.12 | .034 | * | 0.71 |
| Play | 2.69 (1.08) | 1.75 (1.57) | 2.41 | .016 | * | 0.58 |
| Social (no EC) | 3.75 (2.86) | 2.19 (2.90) | 2.32 | .040 | * | 0.60 |
| Total (no EC) | 6.06 (4.49) | 4.31 (4.81) | 2.11 | .035 | * | 0.46 |
| WS/PDD Comparison | ||||||
| WS mean(SD) |
PDD mean(SD) |
Wilcoxon z |
p | Hedge’s g (effect size) |
||
| Communication | 2.65 (2.37) | 3.24 (2.33) | −.54 | .586 | −0.19 | |
| Social | 5.18 (3.99) | 6.47 (3.45) | −1.00 | .319 | −0.25 | |
| Total | 7.82 (6.05) | 9.71 (5.11) | −1.09 | .276 | −0.25 | |
| R/R Interests | 2.82 (2.13) | 2.35 (1.37) | .60 | .546 | 0.16 | |
| Play | 2.82 (1.01) | 2.06 (1.35) | 2.06 | .039 | * | 0.52 |
| Social (no EC) | 4.12 (3.26) | 5.18 (3.11) | −1.01 | .312 | −0.25 | |
| Total (no EC) | 6.76 (5.32) | 8.41 (4.82) | −1.14 | .253 | −0.25 | |
| WS/Autism Comparison | ||||||
| WS mean(SD) |
AUT mean(SD) |
Wilcoxon z |
p | Hedge’s g (effect size) |
||
| Communication | 2.39 (2.07) | 6.32 (1.70) | −4.56 | <.001 | *** | −1.78 |
| Social | 4.79 (3.69) | 11.29 (1.92) | −4.57 | <.001 | *** | −1.65 |
| Total | 7.18 (5.51) | 17.61 (2.66) | −4.55 | <.001 | *** | −2.03 |
| R/R Interests | 2.68 (1.87) | 3.11 (1.57) | −.75 | .456 | −0.13 | |
| Play | 2.79 (2.01) | 3.25 (0.93) | −1.60 | .110 | −0.30 | |
| Social (no EC) | 3.71 (2.97) | 9.29 (1.92) | −4.50 | <.001 | *** | −1.66 |
| Total (no EC) | 6.11 (4.79) | 15.61 (2.66) | −4.55 | <.001 | *** | −2.10 |
p < .10
p < .05
p < .01
p < .001
Note. WS = Williams syndrome; PDD = Pervasive Developmental Disorder – Not Otherwise Specified; AUT = Autism; ME = Mixed etiology; Social = Reciprocal social interaction; R/R Interests = Restricted and Repetitive Behaviors and Interests; no EC = Eye Contact code excluded from total.
Table 4.
Summary of Comparisons of ADOS Item Results Between Williams Syndrome Group and Matched Contrast Groupsa
| Domain Itemb |
WS/ME Comparison |
WS/PDD Controlling for EL |
WS/PDD Controlling for RL |
WS/AUT Controlling for EL |
WS/AUT Controlling for RL |
|---|---|---|---|---|---|
| (16 pairs) | (17 pairs) | (16 pairs) | (24 pairs) | (24 pairs) | |
| Communication | WS<AUT** | WS<AUT** | |||
| Overall Lang | |||||
| Freq Voc | WS<AUT** | WS<AUT** | |||
| Intonation | WS<AUT* | WS<AUT** | |||
| Echolalia | WS<AUT* | WS<AUT* | |||
| Stereotyped | |||||
| Use Others Body | WS<AUT** | ||||
| Pointing | WS<AUT** | WS<AUT** | |||
| Gestures | WS<AUT* | ||||
| Reciprocal Social | WS>ME* | WS<AUT** | WS<AUT** | ||
| Unusual EC | WS>ME* | WS<AUT** | WS<AUT* | ||
| Social Smile | WS<AUT** | WS<AUT** | |||
| Facial Directed | WS<AUT** | WS<AUT** | |||
| Integration Gaze | WS<AUT** | WS<AUT** | |||
| Shared Enjoy | WS<AUT** | WS<AUT** | |||
| Response Name | WS<AUT** | WS<AUT* | |||
| Requesting | WS<AUT** | WS<AUT** | |||
| Giving | |||||
| Showing | |||||
| Initiation JA | WS<AUT** | WS<AUT** | |||
| Response JA | WS<AUT* | ||||
| Quality Soc Ov | WS<AUT** | WS<AUT** | |||
| Play | WS>ME | ||||
| Functional Play | |||||
| Imag/Creat | WS>ME** | ||||
| Repetitive Behaviors | WS>ME* | WS>PDD | WS>PDD | ||
| Unusual Sens | |||||
| Other Mann | |||||
| Self-Injurious | |||||
| Repetitive/Rest |
p < .01
p < .001
Full item descriptive and inferential statistics are available in online Supplementary Tables. Blank cells indicate no significant difference.
ADOS algorithm items are in italics
Note: Higher item scores mean greater abnormality. WS = Williams syndrome; PDD = Pervasive Developmental Disorder – Not Otherwise Specified; AUT = Autism; EL = Mullen Expressive Language; RL = Mullen Receptive Language; Overall Language = Overall level of non-echoed language; Vocal Directed = Frequency of vocalizations directed to others; Intonation = Intonation of vocalizations or verbalizations; Echolalia = Immediate echolalia; Stereotyped Lang = Stereotyped/idiosyncratic use of words or phrases; Use Others’ Body = Use of other’s body to communicate; Unusual Eye = Unusual eye contact; Facial Directed = Facial expressions directed to others; Integration Gaze = Integration of gaze and other behaviors during social overtures; Initiation JA = Spontaneous initiation of joint attention; Response JA = Response to joint attention; Qual Social Ov. = Quality of social overtures; Functional Play = Functional play with objects; Imag/Creat = Imagination/Creativity; Unusual Sensory = Unusual sensory interest in play material/person; Other Mannerisms = Hand and finger and other complex mannerisms; Repetitive/Restrict. = Unusually repetitive interests or stereotyped behaviors
Role of language level
Paired samples t-tests (see Table 5) revealed that the participants with ME did not differ significantly from the individuals with WS on Mullen raw scores for either RL or EL. Additionally, the direction of these differences indicated somewhat stronger abilities in the WS group, which would be expected to be associated with fewer socio-communicative difficulties. Analyses controlling for language were therefore not conducted.
Table 5.
Descriptive statistics for Mullen subtest and overall AE for participant groups individually matched for AE.
| WS | ME | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mullen subtest | M | (SD) | M | (SD) | t | df | p |
Hedge’s g |
|
| VR | 26.67 | (6.16) | 26.07 | (6.73) | 0.51 | 15 | .616 | 0.12 | |
| FM | 21.67 | (3.29) | 24.20 | (5.40) | −2.24 | 15 | .042 | * | −0.54 |
| RL | 24.67 | (4.72) | 23.53 | (6.61) | 1.23 | 14 | .241 | 0.30 | |
| EL | 21.75 | (8.61) | 18.88 | (7.29) | 1.80 | 15 | .091 | 0.43 | |
| AE | 23.30 | (6.19) | 22.92 | (6.69) | 0.80 | 15 | .435 | 0.19 | |
| WS | PDD | ||||||||
| M | (SD) | M | (SD) | t | df | p |
Hedge’s g |
||
| VR | 24.76 | (5.09) | 27.35 | (6.13) | −2.62 | 16 | .019 | * | −0.60 |
| FM | 21.38 | (3.30) | 25.81 | (6.93) | −3.22 | 15 | .006 | ** | −0.76 |
| RL | 23.00 | (5.73) | 18.19 | (5.59) | 3.74 | 15 | .002 | ** | 0.89 |
| EL | 18.63 | (7.82) | 15.38 | (4.92) | 2.03 | 15 | .060 | 0.48 | |
| AE | 21.54 | (5.60) | 21.29 | (5.75) | 0.58 | 16 | .573 | 0.13 | |
| WS | AUT | ||||||||
| M | (SD) | M | (SD) | t | df | p |
Hedge’s g |
||
| VR | 25.00 | (4.69) | 27.60 | (4.56) | −3.27 | 24 | .003 | ** | −0.63 |
| FM | 20.74 | (2.64) | 26.33 | (4.28) | −8.85 | 26 | <.001 | *** | −1.65 |
| RL | 22.96 | (5.78) | 16.33 | (6.93) | 5.79 | 23 | <.001 | *** | 1.14 |
| EL | 19.57 | (8.10) | 15.79 | (5.51) | 4.66 | 27 | <.001 | *** | 0.86 |
| AE | 21.58 | (5.43) | 21.09 | (5.47) | 1.63 | 27 | .114 | 0.31 | |
p < .05
p < .01
p < .001
Note. WS = Williams syndrome; AUT = Autism; PDD = Pervasive Developmental Disorder – Not Otherwise Specified; ME = Mixed Etiology; VR = Mullen Visual Reception subdomain; FM = Mullen Fine Motor subdomain; RL = Mullen Receptive Language subdomain; EL = Mullen Expressive Language subdomain; AE = Average age equivalent in months of Mullen subdomains
Exploration of subgroups
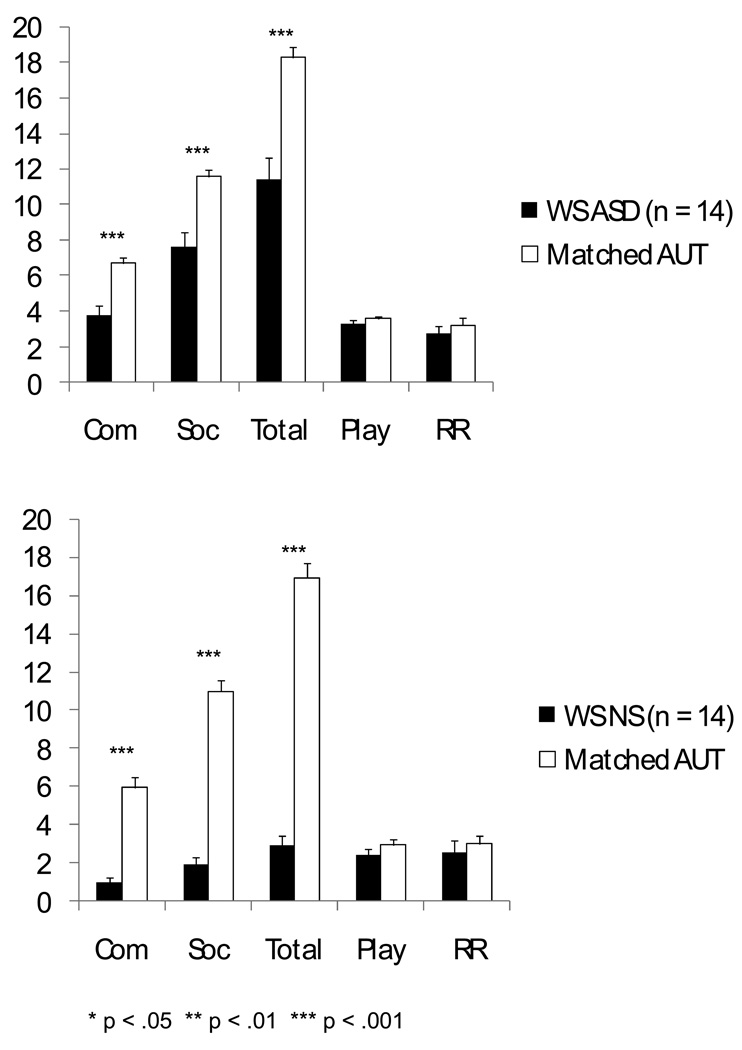
Given that half of the children with WS were classified nonspectrum and half were classified AS or A (referred to here as ASD), an exploratory analysis was conducted to compare the WS+ASD (n = 8) and the WS nonspectrum (n = 8) groups at the domain level. The participants with WS were compared to their individually matched participants in the ME group, regardless of the ADOS classification of the children in the ME group (see Figure 1). The WS+ASD group showed significantly more SOC abnormalities than did the corresponding ME group. No significant group differences were found in COM, Play, RR, or TOT. Although both groups showed very few abnormalities overall, the WS nonspectrum group showed significantly more abnormality in SOC, TOT and RR than did the corresponding ME group.
Figure 1.
Exploratory comparison of ADOS domain scores of children with WS with and without Autism or Autism Spectrum ADOS classifications to matched participants in ME group: WS NS = Williams syndrome with nonspectrum ADOS classification; Matched ME = Mixed Etiology group participants matched individually to the WS participants in the respective group; WS ASD = Williams syndrome with autism spectrum ADOS classification.
Summary
Although were very few differences between the WS and ME groups at the item level, the cumulative effect of socio-communicative difficulties at this level produced a group difference at the SOC domain level, suggesting that young children with WS have greater difficulties with social and emotional reciprocity than would be expected based on developmental delay alone. This difference was present both for children with WS classified AS by the ADOS and those classified nonspectrum, and persisted even when the item showing the largest group difference, unusual eye contact, was removed from the algorithm.
Comparison to PDD Group
Individual matches with clinical diagnoses of PDD-NOS were identified for 17 participants with WS. The distribution of classifications on the ADOS for the WS and PDD groups did not differ significantly, χ2(2) = .92, p = .632 (see Table 2). The WS and PDD groups did not significantly differ in COM, SOC, or RR totals, but the WS group showed significantly more difficulty in Play (See Table 3). The two groups showed, on average, approximately the same level of socio-communicative difficulties on the ADOS. At the item level, results indicated a significant group difference for only one item, Responsive Social Smile (t(16) = −3.17, p = .006, Hedges g = .73), with less difficulty for the WS group (see Supplementary Table 2).
Role of developmental level
Paired samples t-tests revealed that although the participants were individually matched for Mullen AE, participants in the PDD group had significantly stronger nonverbal reasoning and fine motor abilities and significantly weaker RL than the participants in the WS group (see Table 5)3. The groups did not differ significantly in EL raw scores, though a trend was evident (t (15) = 2.03, p = .060). Analyses were conducted controlling for RL and EL; one participant pair was not included in the RL analysis due to missing data. No variables showed significant group differences at the p < .01 level once RL or EL were included as covariates. Hence, the difference in Social Smile did not persist once RL or EL was controlled. (See Table 4 for a summary of the item results and Supplementary Table 2 for detailed descriptive and inferential item statistics.)
Exploration of subgroups
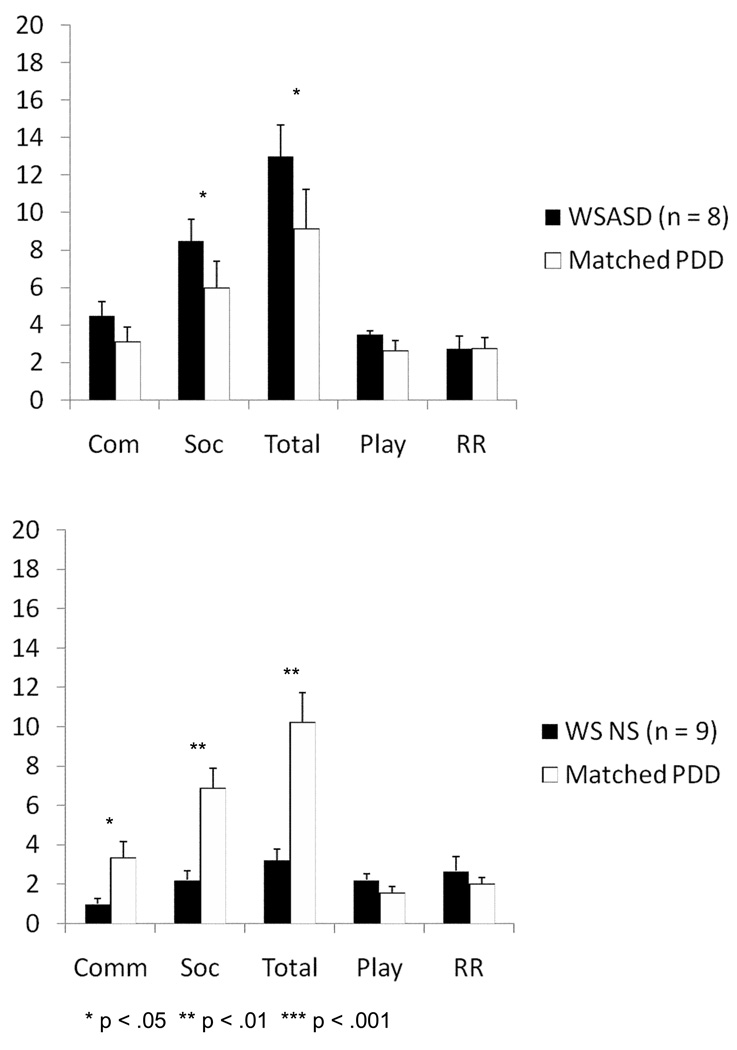
An exploratory analysis was conducted to examine the WS+ASD (n = 8) and the WS nonspectrum groups (n = 9), at the domain level, in comparison to their respective PDD matches. See Figure 2. The WS+ASD group showed significantly poorer SOC and TOT domain scores than did the matched participants with PDD-NOS. The WS nonspectrum group showed significantly milder difficulties for COM, SOC, and TOT than did the matched participants with PDD-NOS. The groups did not differ in Play or RR algorithm totals, regardless of ADOS classification.
Figure 2.
Exploratory comparison of ADOS domain scores of children with WS with and without Autism or Autism Spectrum ADOS classifications to matched participants in PDD group. WS NS = Williams syndrome with nonspectrum ADOS classification; Matched PDD = PDD group participants matched individually to the WS participants in the respective group; WS ASD = Williams syndrome with autism spectrum ADOS classification.
Summary
There were very few significant differences between the WS and PDD-NOS groups at either the domain or item levels. However, once the WS group was divided by ADOS classification, the participants with WS with nonspectrum classification showed significantly fewer socio-communicative abnormalities than the PDD group, while the participants with WS with ADOS ASD classifications showed significantly more difficulties with reciprocal social interaction than the participants in the PDD group.
Comparison to Autism Group
Individual matches with clinical diagnoses of Autism were identified for 28 of the 30 participants with WS. As expected, almost all of the children with autism were classified in the autism range on all aspects of the ADOS. More variability was observed within the sample of children with WS, with approximately half of the WS group classified as AS or A on the ADOS (see Table 2). These distributions were significantly different, χ2(2) = 35.86, p < .001. Comparison of algorithm scores indicated that the children with autism scored significantly higher in all three algorithm areas – COM, SOC, and TOT. There were no significant differences between the groups in either RR or Play (See Table 3). At the item level, the WS group received significantly lower mean scores, indicating less abnormality, on nearly all the COM and SOC items, with the following exceptions, for which no group differences were noted: Echolalia, Stereotyped Language, Unusual Intonation, and Giving objects to others (See Supplementary Table 3). In the Play domain, the Autism group showed significantly more abnormality in Imagination/Creativity (t (27) = 2.93, p = .007, Hedges g = .54), but the groups did not differ significantly in Functional Play. No group differences were found in the RR domain.
Role of developmental level
Paired samples t-tests revealed that the participants with clinical diagnoses of autism, although individually matched to the participants with WS for overall AE, had significantly stronger nonverbal reasoning and fine motor skills and significantly weaker expressive and receptive language skills than did the children with WS (see Table 5). Hence it is possible that the poorer socio-communicative abilities seen in the autism group are related to poorer language abilities. A series of univariate regressions controlling for expressive and receptive language was conducted to examine group differences at the item level, with alpha level set at .01 given the large number of comparisons. (See Table 4 for item results and Supplementary Table 3 for detailed descriptive and inferential item statistics.) Controlling for EL, significant group differences continued to be present at the algorithm level and for the vast majority of socio-communicative items, with the exception of Giving, Overall Level of Language, Stereotyped Language, and Showing. Four individuals with autism, as well as their WS matches, were excluded from the RL analyses because of missing data. Significant group differences, controlling for RL, continued to be present for many of the socio-communicative items, although Giving, Showing, Stereotyped Language, Use of Gestures, Use of Others’ Body to Communicate, and Response to Joint Attention did not show significant group differences once RL was controlled.
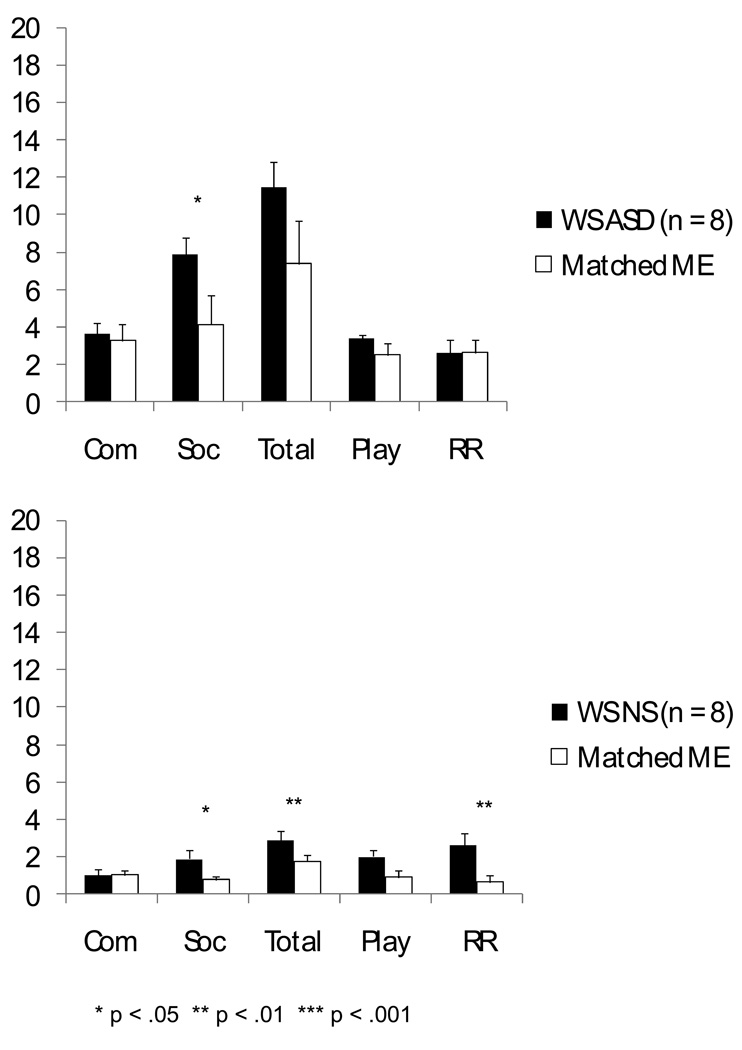
Exploration of subgroups
An exploratory analysis was conducted to examine the WS+ASD (n = 14) and the WS nonspectrum groups (n = 14), at the domain level, in comparison to their respective AUT contrast groups (see Figure 3). The participants in both WS groups showed significantly less impaired COM, SOC, and TOT domain scores than did their respective AUT groups. The matched subgroups did not differ in Play or RR algorithm item raw totals.
Figure 3.
Exploratory comparison of ADOS domain scores of children with WS with and without Autism or Autism Spectrum ADOS classifications to matched participants in AUT group. WS NS = Williams syndrome with nonspectrum ADOS classification; Matched AUT = Autism group participants matched individually to the WS participants in the respective group; WS ASD = Williams syndrome with autism spectrum ADOS classification.
Summary
The children with WS showed fewer socio-communicative deficits than did the participants with autism at both the domain and item levels. The children with WS had significantly stronger RL and EL than the children with clinical diagnoses of autism. Even after RL and EL were statistically controlled, the WS group continued to show significantly milder socio-communicative difficulties, although some group differences were no longer evident.
Discussion
Autism spectrum disorders are currently defined based on a pattern of behavioral characteristics and developmental history including impairments in communication and reciprocal social interaction and the presence of restricted and repetitive behavior. Overlaps with the autism spectrum have been identified for children with a wide variety of genetically-based neurodevelopmental disorders including Down syndrome (26), Fragile-X syndrome (27) Angelman syndrome (28), Inverted Duplication 15 syndrome (29) and others. The study of ASD characteristics in populations with known genetic etiologies has grown in an effort to better understand the pathophysiology of ASD. Recently, for example, abnormalities in amygdala connectivity have been observed for both WS (30) and autism (31).
In our prior paper examining the socio-communicative difficulties of young children with WS using the ADOS (21) we found that about half of the young children with WS with limited language showed significant socio-communicative deficits. Difficulties with declarative pointing, showing objects, and giving were common for young children with WS, whereas difficulties with directed vocalizations and facial expressions, modulated eye contact, and initiation of joint attention were less frequent. We suggested that the presence of these latter difficulties may indicate a need for consideration of a comorbid diagnosis of an autism spectrum disorder. In the present investigation, we extended our prior findings by comparing the performance of children with WS to individually-matched contrast participants with clinical diagnoses of AUT or PDD-NOS and to a ME nonspectrum group.
Developmental Delay Alone Does Not Account for the Socio-Communicative Deficits Seen in Williams Syndrome
Comparison to the ME group indicated that children with WS with limited language show more difficulties with reciprocal social interaction than would be expected based on developmental delay. Difficulties with modulated eye contact were particularly evident. Notably, eye contact abnormalities as assessed by the ADOS can reflect any poor modulation of eye contact (including overly intense eye contact) such that further research about the nature of the gaze abnormalities in young children with WS is warranted. Results of exploratory analyses indicated that even the children with WS with nonspectrum ADOS classifications showed more social interaction deficits than would be expected based on developmental delay alone. Communication difficulties were equally present for both the WS and ME groups, consistent with the ADOS standardization data (24). No comparative difficulties with pointing were observed. However, prior research indicates less frequent pointing in children with WS than for children with other developmental disabilities (32) and the threshold for pointing on the ADOS requires only one clear declarative point.
Socio-Communicative Deficits of Children with Williams Syndrome: Comparison to Autism and PDD-NOS
Children with WS showed markedly fewer abnormalities than the children with autism, consistent with prior research (16). There were some socio-communicative behaviors that did not yield group differences. These tended to be items that were minimally endorsed for either group, likely due to the language level of the participants which may not have allowed for observation of these difficulties (echolalia, stereotyped language, intonation of vocalizations) in either group. Both groups failed to give objects to others throughout the interaction. These group-based results certainly do not rule out the possibility of a comorbid autism diagnosis for some individuals with WS. While comprehensive autism diagnostic assessments were not conducted for the majority of the sample, a few participants were indeed also diagnosed clinically with comorbid autism based on ADOS, ADI-R, and clinical judgment (see 21, for further discussion).
Lincoln and colleagues (16) recently demonstrated that children with WS show lower levels of socio-communicative abnormality in comparison to children with autism. While these results converge with ours, the level of difficulties shown by the children with WS in their sample was considerably milder than that observed in the children included in the current study. Their description of the intellectual abilities of the children in their sample suggests that some of the children with WS may have had stronger language abilities than are appropriate for the administration of Module 1, which is designed for children with no expressive language or who use single words or simple phrases. Administration of a module with fewer language demands might provide an underestimate of the difficulties present (33). Furthermore, no comparisons were made to children with PDD-NOS, who generally show milder socio-communicative abnormalities.
Indeed, in the present investigation, the level of socio-communicative deficits observed for the children with WS was most similar to that of the children with PDD-NOS. The distribution of classifications on the ADOS for these groups did not differ significantly, and the groups did not differ in the level of abnormalities in either communication or reciprocal social interaction. When there was a difference from the PDD-NOS group, not unexpectedly it centered on somewhat stronger affective reciprocity in young children with WS (less difficulty with reciprocal social smiling). Notably, not all participants with WS displayed socio-communicative difficulties suggestive of overlap with the autism spectrum. Exploration of the patterns of performance of subgroups of the participants indicated that on average the participants with WS with nonspectrum ADOS classifications showed less socio-communicative abnormality than did their individually matched PDD-NOS controls, whereas those with ASD classifications on average showed more socio-communicative abnormality than their PDD-NOS controls.
Repetitive Behavior and Play Behavior
Although not the primary focus of this investigation, the ADOS provides indication of other behaviors associated with ASD diagnosis, including the quality of play behavior and the presence of restricted and repetitive behaviors and interests. All participant groups showed difficulty in these areas. Notably, the WS group showed significantly greater difficulties with play, and more restricted and repetitive behaviors, on average, than did the ME group. While the level of restricted and repetitive behaviors for the WS group did not differ from that of the participants with clinical diagnoses of autism or PDD-NOS, the participants with WS showed more abnormal play behavior, on average, than the children with PDD-NOS. The measurement of repetitive behavior and play behavior in the ADOS is not very detailed, but these results nevertheless point to the importance of examining play behaviors and repetitive behaviors in young children with WS using a more comprehensive approach.
Limitations
The ADOS was chosen here because it is a well-researched observational measure of socio-communicative difficulties with broad coverage. Nevertheless, this measure has several limitations. First, total scores are used to determine classification. While higher scores are associated with more socio-communicative difficulties, these total scores were not developed as measures of severity per se. Second, the general desire of individuals with WS to interact with others did not emerge from the pattern of findings presented. The ADOS coding provides minimal opportunity to find areas of strength, as it is designed to identify areas of weakness. Third, the threshold for “no abnormality” on items reflecting social engagement (e.g., Shared Enjoyment) is very low on the ADOS as these items are meant to capture the extreme difficulties of children with ASD with social connectedness. Future investigations would benefit from more comprehensive comparisons of the behavior of children with WS and children with PDD-NOS that go beyond the ADOS codes themselves.
There are also several potential design limitations. Due to the stringent matching used in this investigation to control the roles of development and cognitive abilities, and the inclusion of children in a narrow age range all administered the same ADOS module, the matched groups were of small numbers and represent a small proportion of their respective populations. Information regarding history of services was not available, and such history could affect the level of socio-communicative difficulties observed. Additionally, we report here only results for children administered Module 1 of the ADOS. Examination of consecutive ADOS assessments at the University of Louisville indicated that some children with WS in this age range were administered Module 2, intended for children with at least phrase speech. While 2-year-olds were consistently given Module 1, about 1/3 of children ages 3 and 4 completed Module 2 rather than Module 1, as did most of the 5-year-olds. Hence, these results do not represent the rate of socio-communicative abnormality in WS more generally, but rather reflect the rate of such abnormalities in children with limited language, including older toddlers and younger preschoolers in general, and older children with greater language delays. These findings warrant replication with larger samples and developmental follow-up. Finally, a possible limitation is the ratio of boys to girls in the current sample (approximately 2:1), which is different from that found in large-scale epidemiological studies. However, studies suggest that apart from intellectual functioning, negligible gender differences in socio-communicative deficits as assessed by expert ratings are observed (34, 35).
Conclusion and Implications
The results of this study deepen our understanding of the level of socio-communicative abnormality that is often present for young children with WS who have limited language. The presence of these difficulties cannot be accounted for solely by developmental delay. In our prior article, we indicated that socio-communicative deficits are indeed seen in young children with WS and cautioned against diagnostic overshadowing when assessing children with WS. The results of the current study further indicate that some children with WS show more deficits in reciprocal social interaction than expected based on developmental delay alone. Furthermore, although preliminary, young children with WS classified ASD on the ADOS on average showed greater socio-communicative deficits than children with PDD-NOS diagnoses matched for CA, developmental level, and gender. Despite their socio-communicative difficulties, there was indeed some evidence of the affiliative nature of children with WS as they were found to be somewhat more likely to show reciprocal smiling than the children with PDD-NOS.
As was the case for our previous report with this WS dataset (21), the intention of this study is not to indicate that a large proportion of children with WS should be diagnosed with PDD-NOS. Such a diagnosis could not be made based on the data collected here, but instead would best be based on the administration of the ADOS together with administration of the ADI-R (23) and consideration of clinical judgment (36). Furthermore, there are multiple levels of analysis of disorder, including the genetic level, the brain level, and the phenotypic level. Our current conceptualization of PDD-NOS and Autism diagnoses is based entirely on behavior without regard to etiology. This study provides evidence for overlap at the phenotypic level only.
Not only did children with WS with limited language on average show about the same level of socio-communicative abnormality as children with clinical diagnoses of PDD-NOS, those children with WS who were classified ASD showed significantly more difficulties in reciprocal social interaction than did children with clinical diagnoses of PDD-NOS. We therefore reiterate our caution regarding diagnostic overshadowing, as lack of ASD diagnosis often precludes these children from access to treatments developed for use with children with PDD-NOS which may also be beneficial and appropriate for many children with WS. When children with WS do show difficulties that overlap with the autism spectrum, a full diagnostic evaluation is warranted to carefully examine whether the difficulties present are fully explained by WS alone. Children with WS who meet clinical criteria for PDD-NOS or Autism should be diagnosed with these disorders and not excluded based on their genetic diagnosis. Additional research regarding issues of differential diagnosis in this population is warranted.
Supplementary Material
Acknowledgements
We would like to thank the children who participated in this research and their families. Thank you also to Susan Risi and Shanping Qiu for assistance with compilation of data from the UMACC site, to Joanie Robertson for compilation of data from the UofL site, and to Jill Kelderman for assistance with data collection through UWM. This research was supported by grants NIMH R03 MH069400 and a University of Wisconsin – Milwaukee Graduate School Research Committee Award to Bonnie Klein-Tasman, grants NIMH R01 MH066469 and NIMH K05 MH01196-01 to Catherine Lord, and NICHD R37 HD29957 and NINDS R01 NS35102 to Carolyn Mervis.
Footnotes
In this manuscript, the ADOS classification of “autism” will be abbreviated as A, while the ADOS classification of “autism spectrum,” which is indicative of fewer difficulties than its “autism” category and is related to diagnoses of PDD-NOS, will abbreviated as “AS.” The abbreviation “ASD” will be used to refer to the whole autism spectrum, including behaviors characteristic of both autism and PDD-NOS/AS.
Age equivalents rather than standard scores were used when participants performed at floor on the Mullen (SS = 49). In Mervis and Klein-Tasman (22), we caution against the use of age equivalents. We use them here with reservation, in an effort to avoid a floor effect in our participant matching. In the current investigation, participants were individually matched on both CA and age equivalents, which is likely to make the use of age equivalents, which can be misleading due to different developmental trajectories for different abilities, less problematic.
Note that such a difference would be most likely to result in the PDD group showing more impairment than the WS group, given that poorer language skills are generally associated with poorer socio-communicative skills.
Contributor Information
Bonita P. Klein-Tasman, University of Wisconsin – Milwaukee
Kristin D Phillips, Medical College of Wisconsin
Catherine E. Lord, University of Michigan
Carolyn B. Mervis, University of Louisville
Frank Gallo, University of Wisconsin - Milwaukee.
References
- 1.Hillier LW, Fulton RS, Fulton LA, Graves TA, Pepin KH, Wagner-McPherson C, et al. The DNA sequence of human chromosome 7. Nature. 2003;424(6945):157–164. doi: 10.1038/nature01782. [DOI] [PubMed] [Google Scholar]
- 2.Mervis CB, Morris CA. Williams syndrome. In: Mazzocco MM, Ross JL, editors. Neurogenetic Developmental Disorders: Variations of manifestations in childhood. London, England: MIT Press; 2007. [Google Scholar]
- 3.Klein-Tasman BP, Mervis CB. Distinctive personality characteristics of 8-, 9-, and 10-year-olds with Williams syndrome. Dev Neuropsychol. 2003;23(1–2):269–290. doi: 10.1080/87565641.2003.9651895. [DOI] [PubMed] [Google Scholar]
- 4.Einfeld SL, Tonge BJ, Florio T. Behavioral and emotional disturbance in individuals with Williams syndrome. Am J Ment Retard. 1997;102(1):45–53. doi: 10.1352/0895-8017(1997)102<0045:BAEDII>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Udwin O, Yule W. A cognitive and behavioural phenotype in Williams syndrome. J Clin Exper Neuropsychol. 1991;13(2):232–244. doi: 10.1080/01688639108401040. [DOI] [PubMed] [Google Scholar]
- 6.Stojanovik V. Social interaction deficits and conversational inadequacy in Williams syndrome. J Neurolinguistics. 2006;19(2):157–173. [Google Scholar]
- 7.Mervis CB, Klein-Tasman BP, Mastin ME. Adaptive behavior of 4- through 8-year-old children with Williams syndrome. Am J Ment Retard. 2001;106(1):82–93. doi: 10.1352/0895-8017(2001)106<0082:ABOTYO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan K, Winner E, Tager-Flusberg H. Can adolescents with Williams syndrome tell the difference between lies and jokes? Dev Neuropsychol. 2003;23(1–2):85–103. doi: 10.1080/87565641.2003.9651888. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan K, Tager-Flusberg H. Second-order belief attribution in Williams syndrome: intact or impaired? Am J Ment Retard. 1999;104(6):523–532. doi: 10.1352/0895-8017(1999)104<0523:SBAIWS>2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laws G, Bishop D. Pragmatic language impairment and social deficits in Williams syndrome: a comparison with Down's syndrome and specific language impairment. Int J Lang Commun Disord. 2004;39(1):45–64. doi: 10.1080/13682820310001615797. [DOI] [PubMed] [Google Scholar]
- 11.Mervis CB, Becerra AM. Language and communicative development in Williams syndrome. Ment Retard Dev Disabil Res Rev. 2007;13:3–15. doi: 10.1002/mrdd.20140. [DOI] [PubMed] [Google Scholar]
- 12.Gillberg C, Rasmussen P. Brief report: four case histories and a literature review of Williams syndrome and autistic behavior. J Autism Dev Disord. 1994;24(3):381–393. doi: 10.1007/BF02172235. [DOI] [PubMed] [Google Scholar]
- 13.Gosch A, Pankau R. "Autistic" behavior in two children with Williams-Beuren syndrome. Am J Med Genet. 1994;53(1):83–84. doi: 10.1002/ajmg.1320530118. [DOI] [PubMed] [Google Scholar]
- 14.Reiss AL, Feinstein C, Rosenbaum KN, Borengasser-Caruso MA, Goldsmith BM. Autism associated with Williams syndrome. J Pediatr. 1985;106(2):247–249. doi: 10.1016/s0022-3476(85)80296-1. [DOI] [PubMed] [Google Scholar]
- 15.Herguner S, Motavalli Mukaddes N. Autism and Williams syndrome: a case report. World J Biol Psychiatry. 2006;7(3):186–188. doi: 10.1080/15622970600584221. [DOI] [PubMed] [Google Scholar]
- 16.Lincoln AJ, Searcy YM, Jones W, Lord C. Social interaction behaviors discriminate young children With Autism and Williams syndrome. J Am Acad Child Adolesc Psychiatry. 2007;46(3):323–331. doi: 10.1097/chi.0b013e31802b9522. [DOI] [PubMed] [Google Scholar]
- 17.Stromme P, Bjornstad PG, Ramstad K. Prevalence estimation of Williams syndrome. J Child Neurol. 2002;17(4):269–271. doi: 10.1177/088307380201700406. [DOI] [PubMed] [Google Scholar]
- 18.Investigators AaDDMNSYP. Prevalence of autism spectrum disorders--autism and developmental disabilities monitoring network, six sites, United States, 2000. MMWR Surveill Summ. 2007:1–11. [PubMed] [Google Scholar]
- 19.Borden MC, Ollendick TH. An examination of the validity of social subtypes in autism. J Autism Dev Disord. 1994;24(1):23–37. doi: 10.1007/BF02172210. [DOI] [PubMed] [Google Scholar]
- 20.Waterhouse L, Morris R, Allen D, Dunn M, Fein D, Feinstein C, et al. Diagnosis and classification in autism. J Autism Dev Disord. 1996;26(1):59–86. doi: 10.1007/BF02276235. [DOI] [PubMed] [Google Scholar]
- 21.Klein-Tasman BP, Mervis CB, Lord CE, Phillips KD. Socio-communicative deficits in young children with Williams syndrome: Performance on the Autism Diagnostic Observation Schedule. Child Neuropsychol. 2007;13:444–467. doi: 10.1080/09297040601033680. [DOI] [PubMed] [Google Scholar]
- 22.Mervis CB, Klein-Tasman BP. Methodological issues in group-matching designs: alpha levels for control variable comparisons and measurement characteristics of control and target variables. J Autism Dev Disord. 2004;34(1):7–17. doi: 10.1023/b:jadd.0000018069.69562.b8. [DOI] [PubMed] [Google Scholar]
- 23.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 24.Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule (ADOS) manual. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- 25.Mullen EM. Manual for the Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 26.Molloy CA, Murray DS, Kinsman A, Castillo H, Mitchell T, Hickey FJ, et al. Differences in the clinical presentation of trisomy 21 with and without autism. Journal of Intellectual Disabilities Research. 2009;53:143–151. doi: 10.1111/j.1365-2788.2008.01138.x. [DOI] [PubMed] [Google Scholar]
- 27.Clifford S, Dissanayake C, Bui QM, Huggins R, Taylor AK, Loesch DZ. Autism spectrum phenotype in males and females with fragile X full mutation and permutation. J Autism Dev Disord. 2007;37:738–747. doi: 10.1007/s10803-006-0205-z. [DOI] [PubMed] [Google Scholar]
- 28.Peters SU, Beaudet AL, Madduri N, Bacino CA. utism in Angelman syndrome: implications for autism research. Clin Genet. 2004;66(6):530–536. doi: 10.1111/j.1399-0004.2004.00362.x. [DOI] [PubMed] [Google Scholar]
- 29.Borgatti R, Piccinelli P, Passoni D, Raggi E, Ferrarese C. Pervasive developmental disorders and GABAergic system in patients with inverted duplicated chromosome 15. J Child Neurol. 2001;16(12):911–914. doi: 10.1177/088307380101601209. [DOI] [PubMed] [Google Scholar]
- 30.Meyer-Lindenberg A, Hariri AR, Munoz KE, Mervis CB, Mattay VS, Morris CA, et al. Neural correlates of genetically abnormal social cognition in Williams syndrome. Nat Neurosci. 2005;8(8):991–993. doi: 10.1038/nn1494. [DOI] [PubMed] [Google Scholar]
- 31.Boucher J, Cowell P, Howard M, Broks P, Farrant A, Roberts N, et al. A combined clinical, neuropsychological, and neuroanatomical study of adults with high functioning autism. Cognit Neuropsychiatry. 2005;10(3):165–213. doi: 10.1080/13546800444000038. [DOI] [PubMed] [Google Scholar]
- 32.Laing E, Butterworth G, Ansari D, Gsodl M, Longhi E, Panagiotaki G, et al. Atypical development of language and social communication in toddlers with Williams syndrome. Dev Sci. 2002;5:233–246. [Google Scholar]
- 33.Klein-Tasman BP, Risi S, Lord CE. Effect of Language and Task Demands on the Diagnostic Effectiveness of the Autism Diagnostic Observation Schedule: The Impact of Module Choice. J Autism Dev Disord. 2006;37:1224–1234. doi: 10.1007/s10803-006-0266-z. [DOI] [PubMed] [Google Scholar]
- 34.Holtmann M, Bölte S, Poustka F. Autism spectrum disorders: sex differences in autistic behavior domains and coexisting psychopathology. Developmental Medicine and Child Neurology. 2007;49:361–366. doi: 10.1111/j.1469-8749.2007.00361.x. [DOI] [PubMed] [Google Scholar]
- 35.Volkmar FR, Szatmari P, Sparrow SS. Sex differences in pervasive developmental disorders. J Autism Dev Disord. 1993;23:579–591. doi: 10.1007/BF01046103. [DOI] [PubMed] [Google Scholar]
- 36.Risi S, Lord C, Gotham K, Corsello C, Chrysler C, Szatmari P, et al. Combining information from multiple sources in the diagnosis of autism spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1094–1103. doi: 10.1097/01.chi.0000227880.42780.0e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.