Abstract
Objective
Adults with mood disorders are at elevated risk for suicide. Psychological features such as hopelessness increase their risk for suicide ideation. Few studies have examined psychological constructs posited to lower risk for suicide ideation. The authors tested the hypothesis that reasons for living (RFL) are inversely related to suicide ideation.
Design
This report is a secondary analysis of cross-sectional data.
Setting
Participants were recruited from the clinical services of three teaching hospitals in Rochester, NY.
Participants
The sample consisted of 125 adults 50 years or older receiving treatment for a mood disorder.
Measurements
A diagnostic interview and measures of suicide ideation, depression, hopelessness, and RFL were included in the assessment battery. Dependent variables were presence and severity of suicide ideation. Data were analyzed using multivariate logistic and linear regressions.
Results
Patients who reported higher levels of fear of suicide were less likely to report suicide ideation. The relationships between hopelessness and both the presence and severity of suicide ideation were stronger among those who reported greater levels of responsibility to family.
Conclusions
Clinicians working with at-risk older adults are encouraged to explore their patients’ RFL. These cross-sectional findings point to the need for prospective research examining the associations among different RFL, hopelessness, and suicide ideation in depressed older adults.
Keywords: Aging, suicide ideation, reasons for living, hopelessness, depression
More than 12,000 adults in the United States over the age of 50 die by suicide annually,1 most of whom suffer from a mood disorder, typically major depression.2,3 Many depressed adults, however, never consider suicide,4 suggesting the need to examine psychological processes that may confer or reduce risk for suicide ideation in this population.
Hopelessness, defined as a system of negative beliefs and expectancies concerning oneself and one's future,5 is an important risk factor for both suicide ideation and death by suicide in depressed adults over 50. It is associated with suicide ideation in diverse samples.6-10 Prospective studies of patients seen in mental health treatment settings suggest that it also confers risk for death by suicide.11,12
Reasons for living (RFL) are beliefs or expectancies thought to mitigate risk for suicide, and include survival and coping beliefs, responsibility to family, child-related concerns, fear of suicide, fear of social disapproval, and moral objections.13 Few studies have examined these constituent components,14-18 and most have focused on younger adults,13,14,16 but older and younger adults may have different RFL.19
RFL may also weaken the association between hopelessness and suicide ideation. Individuals who believe they have more RFL may be better prepared to buffer the negative effects of hopelessness. Just as optimism and attitudes toward suicide have been demonstrated to moderate the relation between hopelessness and suicide ideation,20,21 so may RFL.
The present study tested the hypotheses that RFL are negatively associated with suicide ideation among depressed adults over the age of 50. Instead of merely examining an overall summary score of RFL, we examined its components, to investigate potentially important distinctions among survival and coping beliefs, fear of suicide, responsibility to family, and moral objections. Their moderating effects on the relationships between hopelessness and indicators of suicide ideation were also examined. We hypothesized that these relationships would be attenuated among those who endorsed higher levels of RFL.
METHODS
Participants
Six hundred thirty-three patients over 50 years of age with suspected mood disorder diagnoses who were receiving clinical services from three teaching hospitals in Rochester, NY were invited to participate.22 Two hundred fifty (40%) patients consented, all of whom met criteria for a mood disorder as established by the Structured Clinical Interview for DSM–IV Axis I disorders (SCID-I23). Forty-eight (20%) participants diagnosed with dementia, psychoses, or current mania, and one (<1%) who was later determined to have alcohol withdrawal rather than a mood disorder were excluded. Seventy-six participants (30%) were excluded from the analyses, most (N = 60) because they did not complete the hopelessness scale.
Data from the 125 remaining participants were analyzed for the current report. Sixty-seven participants were women (54%), and 121 (97%) were white. One hundred two (82%) met criteria for major depressive disorder, 11 (9%) for bipolar I disorder most recent episode depressed, 3 (2%) for bipolar I disorder most recent (but not currently) manic, mixed, or unspecified, 3 (2%) for bipolar II disorder, 3 (2%) for substance induced mood disorder, 2 (2%) depression not otherwise specified, and 1 (<1%) for dysthymia. Mean standard deviation (SD) age was 60.9 (10.1) years and ranged from 50 to 88. Fifty-one (41%) participants lived alone, and 56 (45%) were married. Seventy-six (61%) participants were either retired or receiving disability benefits. Mean (SD) level of education was 13.3 (2.5) years. There were no statistically significant age or gender differences in those with and without complete data.
Measures
RFL12 were assessed with 25 items derived from a version of the RFL for older adults.24 These items were taken from Linehan et al's original RFL. Items were rated on a 6-point Likert scale and combined into summary scores, with higher scores reflecting greater RFL. Four items tapping future orientation were examined in a prior publication and excluded from these analyses.25 The lone item tapping fear of social disapproval was excluded because of concerns about reliability. The 25-item measure consisted of four internally consistent subscales tapping survival and coping beliefs (14 items; α = 0.95), fear of suicide (four items; α = 0.62), responsibility to family (three items; α = 0.81), and moral objections (four items; α = 0.88). Correlations among subscales ranged from 0.28 to 0.63. Examples of items in each of these respective domains are as follows: “I believe I can find other solutions to my problems,” “I am afraid of death,” “It would hurt my family too much and I would not want them to suffer,” and “My religious beliefs forbid it.”
Depressive symptoms were assessed with the Hamilton Rating Scale for Depression,26 a 24-item interviewer-administered measure of the presence and severity of depressive symptoms in the past week. The item assessing suicide ideation was omitted to avoid overlap with the dependent variable (α = 0.71).
Hopelessness was assessed with the Beck Hopelessness Scale,27 a 20-item True or False measure of negative expectancies regarding one's future (α = 0.93).
Suicide ideation was assessed with the Scale for Suicide Ideation,28 a 19-item interviewer-rated measure of the presence and severity of suicide ideation assessed for the last 7 days. Suicide ideation was coded as present if the respondent received a total score of 1 or greater. To quantify the severity of suicide ideation, items were summed (α = 0.95).
Statistical Analyses
Multivariate logistic regression analysis was used to examine the dichotomous dependent variable, presence or absence of suicide ideation. Model fit was evaluated using the Hosmer-Lemeshow statistic.29 Odds ratios and asymmetric confidence intervals were computed using the method of profile likelihood.30 Variables that were included in interaction terms were centered before entry.31-33 Interaction terms were entered into the model separately and the significant terms were included in the models.
Multivariate linear regression was used to analyze the severity of suicide ideation on a continuum. Not unexpectedly, the distribution of suicide ideation scores was positively skewed. A transformation (inverse of the Scale for Suicide Ideation score +1) was applied to approximate a normal distribution.34
RESULTS
Descriptive statistics are provided in Table 1.
TABLE 1.
Descriptive Statistics and Logistic Regression Analyses Predicting the Presence of Suicide Ideation (N = 125)
| Suicide Ideation |
|||
|---|---|---|---|
| Variables | Mean (SD) or N (%) | Univariate OR (95% CI) | Multivariate OR (95% CI) |
| Age | 60.86 (10.43) | .97 (.94−1.01) | .99 (.96−1.03) |
| Gender | 58 (46.4%) | .95 (.46−1.93) | .97 (.43−2.18) |
| HRSD | 26.33 (7.50) | 1.05 (1.01−1.11)a | 1.05 (.98−1.11) |
| BHS | 11.33 (6.33) | 1.07 (1.01−1.14)a | 1.02 (.94−1.12) |
| RFL-SC | 57.11 (18.38) | .96 (.94−.99)b | .99 (.96−1.03) |
| RFL-RF | 13.42 (4.40) | .92 (.84−1.00) | 1.00 (.87−1.14) |
| RFL-FS | 14.50 (4.91) | .89 (.82−.96)b | .90 (.81−.99)a |
| RFL-MO | 14.10 (6.50) | .91 (.86−.96)b | .95 (.87−1.03) |
| RFL-RF X BHS |
– | – | 1.02 (1.00−1.04)a |
Note: Gender = male; HRSD = Hamilton Rating Scale for Depression without the suicide ideation item; BHS = Beck Hopelessness Scale; RFL = Reasons for Living; SC = Survival and Coping; RF = Responsibility to Family; FS = Fear of Suicide; MO = Moral Objections. All variables were entered simultaneously into the multivariate analysis. Hosmer-Lemeshow tests (28) suggested an acceptable fit of the logistic models for current suicide ideation, X2(8, 125) = 7.95, p = .44. Wald tests were used for significance testing (df = 1).
p < .05.
p < .01.
Presence of Suicide Ideation
Seventy-two (58%) participants reported suicide ideation. Suicide ideation was more common among patients with higher scores on the Hamilton Rating Scale for Depression and Beck Hopelessness Scale (BHS) (Table 1). The survival and coping beliefs, fear of suicide, and moral objections subscales of the RFL scale were negatively associated with the presence of suicide ideation. Multivariate analyses revealed that patients with higher levels of fear of suicide were less likely to report suicide ideation. The responsibility to family and hopelessness interaction was also significant. Unexpectedly, responsibility to family strengthened rather than attenuated the association between hopelessness and suicide ideation. Because the direction of that interaction was counter to our prediction, we reran the multivariate analysis, replacing the RFL subscales with the full 25-item RFL score. Our reanalysis yielded an odds ratio (95% confidence interval) for the full RFL of 0.98 (0.96−0.99), showing that patients with more reasons reported less suicidal ideation. The interaction between overall RFL and BHS was not significant.
Severity of Suicide Ideation
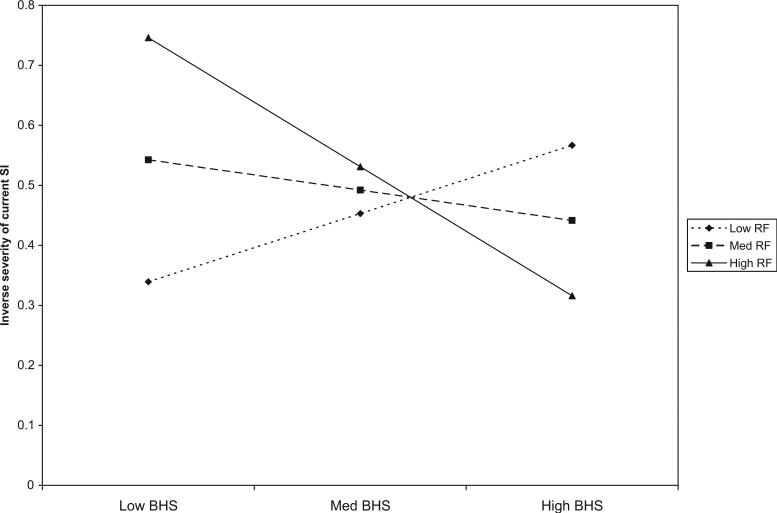
The mean (SD) for current suicide ideation was 5.41 (8.88) and the range was 0−31. Table 2 shows an interaction between responsibility to family and hopelessness on severity of suicide ideation. As suggested by Aiken and West,35 the interaction was depicted using the centered mean for scores at the centered mean as well as those falling one SD above and below (Fig. 1). Results suggested that responsibility to family strengthened the association between hopelessness and suicide ideation. Fear of suicide was associated with less severe suicidal ideation; the probability value did not achieve the conventional level of statistical significance, however [t(124) = 1.91, p = 0.06]. We also repeated the analysis for the severity of SI using the full RFL inventory. The RFL was associated with the severity of SI [t(124) = 3.53, p = 0.001], indicating that greater RFL were associated with less severe SI. Again, the interaction with BHS was not significant.
TABLE 2.
Linear Regression for Severity of Suicide Ideation (N = 125)
| Severity of Suicide Ideation |
||||
|---|---|---|---|---|
| Univariate |
Multivariate |
|||
| Variables | Unstandardized Beta (SE) | Standardized Beta | Unstandardized Beta (SE) | Standardized Beta |
| Age | .009 (.003) | .242b | .004 (.003) | .110 |
| Gender | −.019 (.072) | −.024 | −.008 (.064) | −.011 |
| HRSD | −.012 (.005) | −.231b | −.007 (.005) | −.134 |
| BHS | −.019 (.005) | −.297b | −.008 (.006) | −.130 |
| RFL-SC | .008 (.002) | .368c | .001 (.003) | .060 |
| RFL-RF | .024 (.008) | .266b | .004 (.010) | .043 |
| RFL-FS | .021 (.007) | .262b | .015 (.008) | .181 |
| RFL-MO | .021 (.005) | .339c | .009 (.007) | .143 |
| RFL-RF X BHS |
– | – | −.003 (.001) | −.198a |
Note: Gender = male; HRSD = Hamilton Rating Scale for Depression without the suicide ideation item; BHS = Beck Hopelessness Scale; RFL = Reasons for Living; SC = Survival and Coping; RF = Responsibility to Family; FS = Fear of Suicide; MO = Moral Objections.
All variables were entered simultaneously into the multivariate analysis. A transformation (inverse of the SSI score +1) was applied to approximate a normal distribution.
Consequently, unlike the analyses reported in Table 1, in this Table lower scores reflect higher levels of suicide ideation. Analyses of Variance (ANOVA) suggested an acceptable fit of the multiple regression model for the severity of current suicide ideation [F (9, 115) = 4.76, p < .001], which accounted for 27% of the variance (adjusted = .21).
T-tests were used for significance testing (df = 124).
p < .05.
p < .01.
p < .001.
FIGURE 1. Inverse of Severe SI.
Responsibility to Family (RF) Moderating the Relationship between Hopelessness (BHS) and the Inverse Severity of Current Suicide Ideation
Note: Higher scores on the y axis reflect lower SI. Scores on the y axis reflect severity of SI, but are not identical to SSI scores.
DISCUSSION
To our knowledge, this is the first study to examine the association between different RFL and suicide ideation in adults 50 years of age or older receiving treatment for a mood disorder. Prior studies have shown that RFL are negatively associated with suicide ideation in younger adults,13-15 with the exception of fear of suicide which was found to have a negative association with suicide ideation in a clinical sample but a positive association in a nonclinical sample.13 Our findings indicated that fear of suicide, construed by the authors of the RFL as an amalgam of the fear of death and fear of the act of killing oneself, diminishes the likelihood of suicide ideation in older adults with a mood disorder. The fear of death and of killing oneself may be an important deterrent of suicide ideation in older depressed adults. None of the other RFL were associated with the presence or severity of suicidal ideation.
Unexpectedly, depressed older adults’ concern that their suicide would hurt family members increased the association between hopelessness and the presence and severity of suicide ideation. These findings require replication; however, there are reasonable post hoc explanations. Depressed and hopeless older adults with a sense of responsibility to family may feel overwhelmed by real or perceived inadequacies, increasing thoughts about suicide to end their own suffering. Their sense of burdening their loved ones may also increase thoughts about killing themselves to bring relief to their family.36 In the presence of hopelessness, cognitions that are thought to reduce risk, such as responsibility to family, may be rendered inert or even harmful.
In general, RFL may reflect a sense of purpose and meaning,37 that enables people to live through difficult circumstances.38 However, our preliminary findings also suggest that RFL involving family obligations may enhance the negative effects of hopelessness. Clearly, more research on the apparently complex relations between responsibility to family, hopelessness, and suicide ideation is warranted.
Clinicians should explore what each RFL means for each patient rather than assume they are protective. Understanding the subjective value of RFL may improve clinicians’ ability to evaluate whether RFL are indicative of resilience or risk. Open-ended questions about specific RFL may encourage patient elaboration and reveal critical details and insights that could improve clinicians’ ability to determine risk. This exploration may also enhance patients’ understanding of their motivation to live. Frank and empathetic discussion with family and friends about patients’ RFL may provide additional information that could be crucial to estimating risk accurately.
Limitations of this study include cross-sectional data analysis, exploratory analysis with multiple independent variables, and exclusive focus on a treatment-seeking sample. Analyses included a relatively small sample of potential participants and may have been biased. Interestingly, 61 (80%) of the 76 participants who were excluded due to missing data were missing BHS scores, perhaps reflecting nonrandom missingness among people who are especially concerned about the future, a phenomenon that has been documented previously.39
In conclusion, this is the first study to investigate different RFL, hopelessness, and presence and severity of current suicide ideation in a sample of depressed older adults. Our findings support the possibility that fear of suicide may decrease suicide risk and responsibility to family may accentuate the pathogenic effects of hopelessness. These preliminary findings underscore the need for prospective research examining the associations among different RFL, hopelessness, and suicide ideation in depressed older adults. Clinicians working with at-risk older adults are encouraged to explore their patients’ RFL.
Acknowledgments
The authors thank Xin Tu, Ph.D., Hua He, Ph.D., and Benjamin P. Chapman, Ph.D. of the University of Rochester Medical Center for statistical consultation.
This work was supported by United States Public Health Service grants R01MH51201, R01MH54682, R01MH60285, K24MH72712, T32 MH20061, and an American Foundation for Suicide Prevention (AFSP) Young Investigator Award.
These findings were presented at the annual American Association of Suicidology conference in New Orleans, LA, April 13, 2007.
References
- 1.Centers for Disease Control and Prevention WISQARS Injury Mortality Reports 1999−2004. Centers for Disease Control and Prevention. 2006 [Google Scholar]
- 2.Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence D, Almeida OP, Hulse GK, et al. Suicide and attempted suicide among older adults in Western Australia. Psychol Med. 2000;30:813–821. doi: 10.1017/s0033291799002391. [DOI] [PubMed] [Google Scholar]
- 4.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 5.Stotland E. The Psychology of Hope. Jossey-Bass; San Francisco: 1969. [Google Scholar]
- 6.Uncapher H, Gallagher-Thompson D, Osgood NJ, et al. Hopelessness and suicidal ideation in older adults. Gerontologist. 1998;38:62–70. doi: 10.1093/geront/38.1.62. [DOI] [PubMed] [Google Scholar]
- 7.Uncapher H. Cognitive biases and suicidal ideation in elderly psychiatric inpatients. Omega: J Death Dying. 2001;42:21–36. [Google Scholar]
- 8.Heisel MJ, Flett GL. A psychometric analysis of the geriatric hopelessness scale (GHS): towards improving assessment of the construct. J Affect Disord. 2005;87:211–220. doi: 10.1016/j.jad.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 9.Szanto K, Mulsant BH, Houck PR, et al. Treatment outcome in suicidal vs non-suicidal elderly patients. Am J Geriatr Psychiatry. 2001;9:261–268. [PubMed] [Google Scholar]
- 10.Vannoy S, Duberstein P, Cukrowicz K, et al. The relationship between suicide ideation and late-life depression. Am J Geriatr Psychiatry. 2007;15:1024–1033. doi: 10.1097/JGP.0b013e3180cc2bf1. [DOI] [PubMed] [Google Scholar]
- 11.Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. J Consult Clin Psychol. 1989;57:309–310. doi: 10.1037//0022-006x.57.2.309. [DOI] [PubMed] [Google Scholar]
- 12.Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68:371–377. [PubMed] [Google Scholar]
- 13.Linehan MM, Goodstein JL, Nielsen SL, et al. Reasons for staying alive when you are thinking of killing yourself: the reasons for living inventory. J Consult Clin Psychol. 1983;51:276–286. doi: 10.1037//0022-006x.51.2.276. [DOI] [PubMed] [Google Scholar]
- 14.Dean PJ, Range LM. The escape theory of suicide and perfectionism in college students. Death Stud. 1996;20:415–424. doi: 10.1080/07481189608252790. [DOI] [PubMed] [Google Scholar]
- 15.Dean PJ, Range LM. Testing the escape theory of suicide in an outpatient clinical population. Cognit Ther Res. 1999;23:561–572. [Google Scholar]
- 16.Dean PJ, Range LM, Goggin WC. The escape theory of suicide in college students: testing a model that includes perfectionism. Suicide Life Threat Behav. 1996;26:181–186. [PubMed] [Google Scholar]
- 17.Malone KM, Oquendo MA, Haas GL, et al. Protective factors against suicidal acts in major depression: reasons for living. Am J Psychiatry. 2000;157:1084–1088. doi: 10.1176/appi.ajp.157.7.1084. [DOI] [PubMed] [Google Scholar]
- 18.Mann JJ, Waternaux C, Haas GL, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 19.Miller JS, Segal DL, Coolidge FL. A comparison of suicidal thinking and reasons for living among younger and older adults. Death Stud. 2001;25:357–365. doi: 10.1080/07481180126250. [DOI] [PubMed] [Google Scholar]
- 20.Gibb BE, Andover MS, Beach SR. Suicidal ideation and attitudes toward suicide. Suicide Life Threat Behav. 2006;36:12–18. doi: 10.1521/suli.2006.36.1.12. [DOI] [PubMed] [Google Scholar]
- 21.Hirsch JK, Conner KR. Dispositional and explanatory style optimism as potential moderators of the relationship between hopelessness and suicidal ideation. Suicide Life Threat Behav. 2006;36:661–669. doi: 10.1521/suli.2006.36.6.661. [DOI] [PubMed] [Google Scholar]
- 22.Heisel MJ, Duberstein PR, Conner KR, et al. Personality and reports of suicide ideation among depressed adults 50 years of age or older. J Affect Disord. 2006;90:175–180. doi: 10.1016/j.jad.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM–IV Axis I Disorders–Patient Edition (SCID-I/P, Version 2.0, 4/97 Revision). Biometrics Research Department, N.Y. State Psychiatric Institute; New York: 1997. [Google Scholar]
- 24.Edelstein BA, McKee DR, Martin RR. Development of the reasons for living scale for older adults: a suicide assessment instrument.. Poster presented at the Harvard Symposium on Future Research Trends and Opportunities in Aging.; Boston, MA. 2000. [Google Scholar]
- 25.Hirsch JK, Duberstein PR, Conner KR, et al. Future orientation and suicide ideation and attempts in depressed adults ages 50 and over. Am J Geriatr Psychiatry. 2006;14:752–757. doi: 10.1097/01.JGP.0000209219.06017.62. [DOI] [PubMed] [Google Scholar]
- 26.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Weissman A, Lester D, et al. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the scale for suicidal ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 29.Hosmer DW, Lemeshow S. Applied Logistic Regression. Wiley; New York: 1989. [Google Scholar]
- 30.McCullagh P, Nelder JA. Generalized Linear Models. Chapman and Hall; London: 1989. [Google Scholar]
- 31.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J, Cohen P, West SG, et al. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3rd ed Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2003. [Google Scholar]
- 33.Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol. 2004;51:115–134. [Google Scholar]
- 34.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Allyn & Bacon; Needham Heights, MA: 2001. [Google Scholar]
- 35.Aiken LS, West SG. Multiple regression: Testing and Interpreting Interactions. Sage Publications; Thousand Oaks, CA: 1991. [Google Scholar]
- 36.Joiner TEJ, Pettit JW, Walker RL, et al. Perceived burdensomeness and suicidality: two studies on the suicide notes of those attempting and those completing suicide. J Soc Clin Psychol. 2002;21:531–545. [Google Scholar]
- 37.Heisel MJ, Flett GL. Purpose in life, satisfaction with life, and suicide ideation in a clinical sample. J Psychopathol Behav Assess. 2004;26:127–135. [Google Scholar]
- 38.Frankl VE. Man's Search For Meaning: An Introduction to Logo-therapy. 4th ed. Beacon Press; Boston, MA: 1992. I. Lasch trans. [Google Scholar]
- 39.Shmotkin D. The apprehensive respondent: failing to rate future life satisfaction in older adults. Psychol Aging. 1992;7:484–486. doi: 10.1037//0882-7974.7.3.484. [DOI] [PubMed] [Google Scholar]