Abstract
BACKGROUND
The possible advantage for weight loss of a diet that emphasizes protein, fat, or carbohydrates has not been established, and there are few studies that extend beyond 1 year.
METHODS
We randomly assigned 811 overweight adults to one of four diets; the targeted percentages of energy derived from fat, protein, and carbohydrates in the four diets were 20, 15, and 65%; 20, 25, and 55%; 40, 15, and 45%; and 40, 25, and 35%. The diets consisted of similar foods and met guidelines for cardiovascular health. The participants were offered group and individual instructional sessions for 2 years. The primary outcome was the change in body weight after 2 years in two-by-two factorial comparisons of low fat versus high fat and average protein versus high protein and in the comparison of highest and lowest carbohydrate content.
RESULTS
At 6 months, participants assigned to each diet had lost an average of 6 kg, which represented 7% of their initial weight; they began to regain weight after 12 months. By 2 years, weight loss remained similar in those who were assigned to a diet with 15% protein and those assigned to a diet with 25% protein (3.0 and 3.6 kg, respectively); in those assigned to a diet with 20% fat and those assigned to a diet with 40% fat (3.3 kg for both groups); and in those assigned to a diet with 65% carbohydrates and those assigned to a diet with 35% carbohydrates (2.9 and 3.4 kg, respectively) (P>0.20 for all comparisons). Among the 80% of participants who completed the trial, the average weight loss was 4 kg; 14 to 15% of the participants had a reduction of at least 10% of their initial body weight. Satiety, hunger, satisfaction with the diet, and attendance at group sessions were similar for all diets; attendance was strongly associated with weight loss (0.2 kg per session attended). The diets improved lipid-related risk factors and fasting insulin levels.
CONCLUSIONS
Reduced-calorie diets result in clinically meaningful weight loss regardless of which macronutrients they emphasize.
There is intense debate about what types of diet are most effective for treating overweight — those that emphasize protein, those that emphasize carbohydrates, or those that emphasize fat.1–3 Several trials showed that low-carbohydrate, high-protein diets resulted in more weight loss over the course of 3 to 6 months than conventional high-carbohydrate, low-fat diets,4–12 but other studies did not show this effect.13–17 A smaller group of studies that extended the follow-up to 1 year did not show that low-carbohydrate, high-protein diets were superior to high-carbohydrate, low-fat diets.6,10,16,18–21 In contrast, other researchers found that a very-high-carbohydrate, very-low-fat vegetarian diet was superior to a conventional high-carbohydrate, low-fat diet.22–24 Among the few studies that extended beyond 1 year, one showed that a very-low-fat vegetarian diet was superior to a conventional low-fat diet,24 one showed that a low-fat diet was superior to a moderate-fat diet,25 two showed that a moderate-fat, Mediterranean-style diet was superior to a low-fat diet,12,26 one showed that a low-carbohydrate diet was superior to a low-fat diet,12 and another showed no difference between high-protein and low-protein diets.10 Small samples, underrepresentation of men, limited generalizability, a lack of blinded ascertainment of the outcome, a lack of data on adherence to assigned diets, and a large loss to follow-up limit the interpretation of many weight-loss trials.27 The novelty of the diet, media attention, and the enthusiasm of the researchers could affect the adherence of participants to any type of diet. The crucial question is whether overweight people have a better response in the long term to diets that emphasize a specific macronutrient composition. Thus, we recognized the need for a large trial that would be designed to overcome the limitations of previous trials and that would compare the effects of three principal dietary macronutrients. We studied weight change over the course of 2 years, since weight loss typically is greatest 6 to 12 months after initiation of the diet, with steady regain of weight subsequently.28
METHODS
STUDY DESIGN AND SITES
We designed a randomized clinical trial to compare the effects on body weight of energy-reduced diets that differed in their targets for intake of macronutrients — low or high in fat, average or high in protein, or low or high in carbohydrates — and otherwise followed recommendations for cardiovascular health.29 The trial was conducted from October 2004 through December 2007. An expanded description of the methods is available in the Supplementary Appendix, available with the full text of this article at NEJM.org. The trial was conducted at two sites: the Harvard School of Public Health and Brigham and Women’s Hospital, Boston; and the Pennington Biomedical Research Center of the Louisiana State University System, Baton Rouge. The data coordinating center was at Brigham and Women’s Hospital. The project staff of the National Heart, Lung, and Blood Institute also participated in the development of the protocol, monitoring of progress, interpretation of results, and critical review of the manuscript.
PARTICIPANTS
Our goal was to recruit 800 overweight and obese subjects (400 at each site), of whom about 40% would be men. Participants had to be 30 to 70 years of age and have a body-mass index (the weight in kilograms divided by the square of the height in meters) of 25 to 40. Major criteria for exclusion were the presence of diabetes or unstable cardiovascular disease, the use of medications that affect body weight, and insufficient motivation as assessed by interview and questionnaire. The study was approved by the human subjects committee at each institution and by a data and safety monitoring board appointed by the National Heart, Lung, and Blood Institute. All participants gave written informed consent. They were informed that the study would be comparing diets with different fat, protein, and carbohydrate contents and that they would be assigned a diet at random. Mass mailings were the primary means of recruitment; names were identified with the use of lists of registered voters or drivers. Random assignments to one of four diet groups were generated by the data manager at the coordinating center on request of a study dietitian, after eligibility of a participant was confirmed.
WEIGHT-LOSS INTERVENTION
The nutrient goals for the four diet groups were: 20% fat, 15% protein, and 65% carbohydrates (low-fat, average-protein); 20% fat, 25% protein, and 55% carbohydrates (low-fat, high-protein); 40% fat, 15% protein, and 45% carbohydrates (high-fat, average-protein); and 40% fat, 25% protein, and 35% carbohydrates (high-fat, high-protein). Thus, two diets were low-fat and two were high-fat, and two were average-protein and two were high-protein, constituting a two-by-two factorial design. The four diets also allowed for a dose–response test of carbohydrate intake that ranged from 35 to 65% of energy. Other goals for all groups were that the diets should include 8% or less of saturated fat, at least 20 g of dietary fiber per day, and 150 mg or less of cholesterol per 1000 kcal. Carbohydrate-rich foods with a low glycemic index were recommended in each diet. Each participant’s caloric prescription represented a deficit of 750 kcal per day from baseline, as calculated from the person’s resting energy expenditure and activity level.
Blinding was maintained by the use of similar foods for each diet. Staff and participants were taught that each diet adhered to principles of a healthful diet29 and that each had been recommended for long-term weight loss, thereby establishing equipoise.1,2,26 Investigators and staff who measured outcomes were unaware of the diet assignment of the participants.
Group sessions were held once a week, 3 of every 4 weeks during the first 6 months and 2 of every 4 weeks from 6 months to 2 years; individual sessions were held every 8 weeks for the entire 2 years. Daily meal plans in 2-week blocks were provided (see the Supplementary Appendix). Participants were instructed to record their food and beverage intake in a daily food diary and in a Web-based self-monitoring tool that provided information on how closely their daily food intake met the goals for macronutrients and energy. Behavioral counseling was integrated into the group and individual sessions to promote adherence to the assigned diets. Contact among the groups was avoided.
The goal for physical activity was 90 minutes of moderate exercise per week. Participation in exercise was monitored by questionnaire30 and by the online self-monitoring tool.
MEASUREMENTS
Body weight and waist circumference were measured in the morning before breakfast on 2 days at baseline, 6 months, and 2 years, and on a single day at 12 and 18 months. Dietary intake was assessed in a random sample of 50% of the participants, by a review of the 5-day diet record at baseline and by 24-hour recall during a telephone interview on 3 nonconsecutive days at 6 months and at 2 years.31 Questionnaires that asked for information on satiety, food craving, eating behavior, and satisfaction with the diet32,33 were administered at baseline (except for diet satisfaction) and at 6 months and 2 years. Fasting blood samples, 24-hour urine samples, and measurement of resting metabolic rate were obtained on 1 day, and blood-pressure measurement on 2 days, at baseline, 6 months, and 2 years. Levels of serum lipids, glucose, insulin, and glycated hemoglobin were measured at the clinical laboratory at the Pennington Biomedical Research Center. Blood pressure was measured with the use of an automated device (HEM-907XL, Omron). The participants were evaluated for the presence of the metabolic syndrome, which was defined by the presence of at least three of the following five criteria: waist circumference of more than 102 cm in men or more than 88 cm in women, a triglyceride level of 150 mg per deciliter (1.69 mmol per liter) or more, a high-density lipoprotein (HDL) cholesterol level of less than 40 mg per deciliter (1.03 mmol per liter) in men or less than 50 mg per deciliter (1.29 mmol per liter) in women, a blood pressure of 130/85 mm Hg or more, and a fasting glucose level of 110 mg per deciliter (6.1 mmol per liter) or more.
STATISTICAL ANALYSIS
The primary outcome of the study was the change in body weight over a period of 2 years, and the secondary outcome was the change in waist circumference. Data were pooled from the diets for the two factorial comparisons: low fat versus high fat and average protein versus high protein. The analysis also included a comparison of two of the four diets, the diet with the lowest carbohydrate content and the diet with the highest carbohydrate content, and included a test for trend across the four levels of carbohydrates. The effects of protein, fat, and carbohydrate levels were evaluated independently with the use of two-sample t-tests at a two-sided significance level of 0.05. Exploratory post hoc analyses were performed with threshold amounts of weight loss as outcomes, with Bonferroni’s adjustment for multiple comparisons. Associations between adherence to the fat and protein goals and weight loss were also explored in post hoc analyses (see Methods in the Supplementary Appendix).
We performed an intention-to-treat analysis in which long-term weight loss for persons who withdrew from the study early (after at least 6 months of participation) was imputed on the basis of a rate of 0.3 kg per month of regained weight34 and a rate of 0.3 cm per month of regained waist circumference after withdrawal (see Methods in the Supplementary Appendix). Risk factors for cardiovascular disease and diabetes were also analyzed according to the intention-to-treat principle, with zero change from baseline imputed for missing data. The study was powered to detect a 1.67-kg weight loss as an effect of the level of protein or fat in the diet over the 2-year period, assuming a withdrawal rate of 40%.
RESULTS
PARTICIPANTS
Of 1638 participants who were screened, 811 (50%) were randomly assigned to a diet, and 645 (80% of those assigned) completed the study (i.e., provided a body-weight measurement at 2 years) (Fig. 1 in the Supplementary Appendix). Baseline characteristics were similar among participants assigned to the four diets and between those who were assigned to a diet and those who completed the study (Table 1).
Table 1.
Baseline Characteristics of the Study Participants.*
| Characteristic | Low-Fat, Average- Protein Group (N = 204) | Low-Fat, High-Protein Group (N = 202) | High-Fat, Average- Protein Group (N = 204) | High-Fat, High-Protein Group (N = 201) | All Participants (N = 811) | Participants Who Completed the Study (N = 645) |
|---|---|---|---|---|---|---|
| Age — yr | 51±9 | 50±10 | 52±9 | 51±9 | 51±9 | 52±9 |
| Sex — no. (%) | ||||||
| Female | 126 (62) | 135 (67) | 125 (61) | 129 (64) | 515 (64) | 397 (62) |
| Male | 78 (38) | 67 (33) | 79 (39) | 72 (36) | 296 (36) | 248 (38) |
| Race or ethnic group — no. (%)† | ||||||
| White | 159 (78) | 158 (78) | 165 (81) | 161 (80) | 643 (79) | 525 (81) |
| Black | 33 (16) | 33 (16) | 28 (14) | 33 (16) | 127 (16) | 88 (14) |
| Asian | 1 (<1) | 1 (<1) | 1 (<1) | 2 (1) | 5 (1) | 3 (<1) |
| Hispanic | 8 (4) | 7 (3) | 9 (4) | 5 (2) | 29 (4) | 23 (4) |
| Other | 3 (1) | 3 (1) | 1 (<1) | 0 | 7 (1) | 6 (1) |
| Height — m | 1.69±0.09 | 1.67±0.08 | 1.68±0.09 | 1.68±0.09 | 1.68±0.09 | 1.68±0.09 |
| Weight — kg | 94±16 | 92±13 | 92±17 | 94±16 | 93±16 | 93±16 |
| Body-mass index‡ | ||||||
| Mean | 33±4 | 33±4 | 32±4 | 33±4 | 33±4 | 33±4 |
| 25.0–29.9 — no. (%) | 51 (25) | 54 (27) | 60 (29) | 58 (29) | 223 (27) | 183 (28) |
| ≥30.0 — no. (%) | 153 (75) | 148 (73) | 144 (71) | 143 (71) | 588 (73) | 462 (72) |
| Waist circumference — cm | 104±13 | 102±12 | 103±14 | 104±13 | 103±13 | 104±13 |
| Hypertension — no. (%) | 70 (34) | 70 (35) | 67 (33) | 80 (40) | 287 (35) | 233 (36) |
| Use of medication — no. (%) | ||||||
| Antihypertensive agents | 54 (26) | 58 (29) | 55 (27) | 61 (30) | 228 (28) | 192 (30) |
| Lipid-lowering agents | 32 (16) | 48 (24) | 40 (20) | 31 (15) | 151 (19) | 128 (20) |
| Smoking status — no. (%) | ||||||
| Current smoker | 8 (4) | 5 (2) | 8 (4) | 10 (5) | 31 (4) | 24 (4) |
| Former smoker | 84 (41) | 59 (29) | 80 (39) | 75 (37) | 298 (37) | 241 (37) |
| Never smoked | 112 (55) | 138 (68) | 116 (57) | 116 (58) | 482 (59) | 380 (59) |
| Educational level — no. (%) | ||||||
| High school or less | 23 (11) | 15 (7) | 19 (9) | 19 (9) | 76 (9) | 65 (10) |
| Some college | 47 (23) | 47 (23) | 45 (22) | 41 (20) | 180 (22) | 132 (20) |
| College graduate or beyond | 134 (66) | 140 (69) | 140 (69) | 141 (70) | 555 (68) | 448 (69) |
| Marital status — no. (%) | ||||||
| Married | 132 (65) | 146 (72) | 144 (71) | 143 (71) | 565 (70) | 448 (69) |
| Divorced or separated | 36 (18) | 24 (12) | 33 (16) | 29 (14) | 122 (15) | 94 (15) |
| Widowed | 8 (4) | 4 (2) | 4 (2) | 2 (1) | 18 (2) | 16 (2) |
| Never married | 28 (14) | 28 (14) | 23 (11) | 27 (13) | 106 (13) | 87 (13) |
| Household income — no. (%) | ||||||
| <$50,000 | 56 (27) | 45 (22) | 48 (24) | 46 (23) | 195 (24) | 153 (24) |
| $50,000 to <$100,000 | 79 (39) | 82 (41) | 78 (38) | 84 (42) | 323 (40) | 260 (40) |
| $100,000 to $150,000 | 46 (23) | 43 (21) | 43 (21) | 32 (16) | 164 (20) | 123 (19) |
| >$150,000 | 21 (10) | 30 (15) | 33 (16) | 36 (18) | 120 (15) | 100 (16) |
| Information not provided | 2 (1) | 2 (1) | 2 (1) | 3 (1) | 9 (1) | 9 (1) |
| Risk factors | ||||||
| Blood pressure — mm Hg | ||||||
| Systolic | 118±13 | 120±13 | 120±13 | 120±15 | 119±13 | 119±14 |
| Diastolic | 75±9 | 75±9 | 76±9 | 76±10 | 75±9 | 75±9 |
| Glucose — mg/dl | 93±12 | 92±17 | 92±12 | 92±13 | 92±14 | 92±12 |
| Insulin — μU/ml | 12±7 | 12±8 | 12±7.5 | 12±8 | 12±8 | 12±7 |
| HOMA | 2.8±1.9 | 2.8±2.2 | 2.9±1.9 | 2.8±1.9 | 2.8±2 | 2.8±1.9 |
| Cholesterol — mg/dl | ||||||
| Total | 199±38 | 203±36 | 203±37 | 204±35 | 202±37 | 202±37 |
| LDL | 124±33 | 126±32 | 128±32 | 126±31 | 126±32 | 125±32 |
| HDL | 49±15 | 49±13 | 48±12 | 51±16 | 49±14 | 49±15 |
| Triglycerides — mg/dl | 135±82 | 144±79 | 147±93 | 141±85 | 142±85 | 144±87 |
| Dietary intake per day§ | ||||||
| No. of participants who provided information | 103 | 106 | 105 | 102 | 416 | 330 |
| Energy — kcal | 2015±505 | 1862±566 | 2012±597 | 1979±599 | 1966±570 | 1978±563 |
| Carbohydrate — % | 44±8 | 46±8 | 45±8 | 44±7 | 45±8 | 45±8 |
| Fat — % | 38±6 | 36±6 | 37±5 | 38±6 | 37±6 | 37±6 |
| Saturated fat — % | 12±3 | 12±3 | 12±3 | 12±2 | 12±3 | 12±3 |
| Protein — % | 18±4 | 18±4 | 18±3 | 18±3 | 18±3 | 18±3 |
| Dietary fiber — g | 18±7 | 17±7 | 18±6 | 17±6 | 17±7 | 18±7 |
| Cholesterol — mg | 303±121 | 278±120 | 306±135 | 305±134 | 298±128 | 298±128 |
| Alcohol — g | 6±8 | 4±7 | 6±9 | 6±9 | 5±8 | 5±8 |
| Respiratory quotient | 0.84±0.04 | 0.84±0.04 | 0.85±0.05 | 0.84±0.04 | 0.84±0.04 | 0.84±0.04 |
Plus–minus values are means ±SD. To convert the values for glucose to millimoles per liter, multiply by 0.05551. To convert the values for cholesterol to millimoles per liter, multiply by 0.02586. To convert the values for triglycerides to millimoles per liter, multiply by 0.01129. HDL denotes high-density lipoprotein, HOMA homeostasis model assessment of insulin sensitivity, and LDL low-density lipoprotein.
Race or ethnic group was reported by the participants.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Data are from a 50% random sample.
WEIGHT LOSS
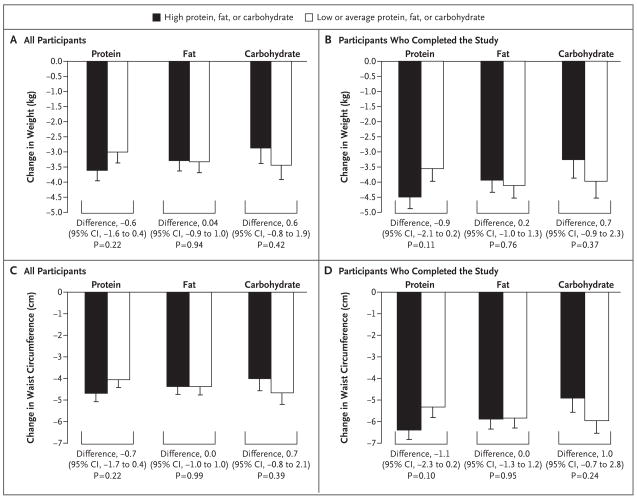
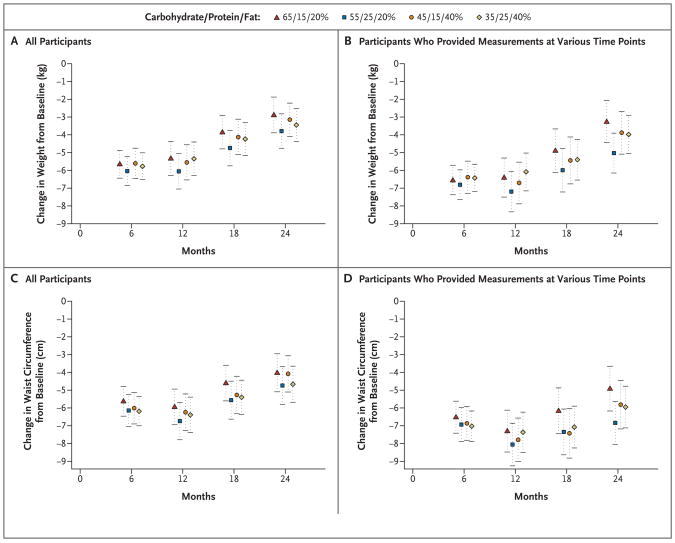
The amount of weight loss after 2 years was similar in participants assigned to a diet with 25% protein and those assigned to a diet with 15% protein (3.6 and 3.0 kg, respectively; P = 0.22) and among those who completed each of those diets (4.5 and 3.6 kg, respectively; P=0.11) (Fig. 1). Weight loss was the same in those assigned to a diet with 40% fat and those assigned to a diet with 20% fat (3.3 kg, P=0.94) and was similar among those who completed each of those diets (3.9 and 4.1 kg, respectively; P = 0.76). There was no effect on weight loss of carbohydrate level through the target range of 35 to 65% (Fig. 1 and 2). The change in waist circumference did not differ significantly among the diet groups (Fig. 1 and 2).
Figure 1. Mean Change in Body Weight and Waist Circumference from Baseline to 2 Years According to Dietary Macronutrient Content.
Solid bars represent high-protein, high-fat, or highest-carbohydrate diets. Open bars represent average-protein, low-fat, or lowest-carbohydrate diets. T bars indicate standard errors. Panels A and C show the change in body weight and the change in waist circumference, respectively, for all participants who were randomly assigned to a diet (a total of 811); missing data were imputed. A total of 403 participants were assigned to a high-protein diet and 408 to an average-protein diet, 405 were assigned to a high-fat diet and 406 to a low-fat diet, and 204 were assigned to the highest-carbohydrate diet and 201 to the lowest-carbohydrate diet. Panel B shows the change in body weight for the 645 participants who provided measurements at 2 years. Of these participants, 325 were assigned to a high-protein diet and 320 to an average-protein diet, 319 were assigned to a high-fat diet and 326 to a low-fat diet, and 169 were assigned to the highest-carbohydrate diet and 168 to the lowest-carbohydrate diet. Panel D shows the change in waist circumference for the 599 participants who provided measurements at 2 years. Of these participants, 303 were assigned to a high-protein diet and 296 to an average-protein diet, 292 were assigned to a high-fat diet and 307 to a low-fat diet, and 159 were assigned to the highest-carbohydrate diet and 155 to the lowest-carbohydrate diet.
Figure 2. Mean Changes in Body Weight and Waist Circumference at Various Time Points.
Panels A and C show the mean changes in body weight and waist circumference, respectively, for all participants who were assigned to a diet (a total of 811 at every time point); missing data were imputed. Panel B shows the change in body weight for participants who provided measurements at various time points: 176 to 180 participants at 6 months, 157 to 167 at 12 months, 140 to 152 at 18 months, and 151 to 168 at 2 years. Panel D shows the change in waist circumference for participants who provided measurements at various time-points: 176 to 179 at 6 months, 154 to 166 at 12 months, 135 to 148 at 18 months, and 137 to 159 at 2 years. I bars in all panels indicate standard errors.
Most of the weight loss occurred in the first 6 months. Changes from baseline differed among the diet groups by less than 0.5 kg of body weight and 0.5 cm of waist circumference (Fig. 2). After 12 months, all groups, on average, slowly regained body weight. A total of 185 of the participants (23%) continued to lose weight from 6 months to 2 years; the mean (±SD) additional weight loss was 3.6±3.5 kg, for a mean total loss from baseline of 9.3±8.2 kg, with no significant differences among the diet groups. At 2 years, 31 to 37% of the participants had lost at least 5% of their initial body weight, 14 to 15% of the participants in each diet group had lost at least 10% of their initial weight, and 2 to 4% had lost 20 kg or more (P>0.20 for the comparisons between diets).
RISK FACTORS FOR CARDIOVASCULAR DISEASE AND DIABETES
All the diets reduced risk factors for cardiovascular disease and diabetes at 6 months and 2 years (Table 2). At 2 years, the two low-fat diets and the highest-carbohydrate diet decreased low-density lipoprotein cholesterol levels more than did the high-fat diets or the lowest-carbohydrate diet (low-fat vs. high-fat, 5% vs. 1% [P = 0.001]; highest-carbohydrate vs. lowest-carbohydrate, 6% vs. 1% [P = 0.01]). The lowest-carbohydrate diet increased HDL cholesterol levels more than the highest-carbohydrate diet (9% vs. 6%, P = 0.02). All the diets decreased triglyceride levels similarly, by 12 to 17%. All the diets except the one with the highest carbohydrate content decreased fasting serum insulin levels by 6 to 12%; the decrease was larger with the high-protein diet than with the average-protein diet (10% vs. 4%, P = 0.07). Blood pressure decreased from baseline by 1 to 2 mm Hg, with no significant differences among the groups (P>0.59 for all comparisons). These changes in risk factors in the intention-to-treat population were about 30 to 40% smaller than the changes seen among participants who provided data at 2 years, reflecting the effect of the imputation of missing values (Table 1 in the Supplementary Appendix). The metabolic syndrome35 was present in 32% of the participants at baseline, and the percentage was lower at 2 years, ranging from 19 to 22% in the four diet groups (P = 0.81 for the four-way comparison).
Table 2.
Risk Factors, Nutrient Intake, and Biomarkers of Adherence, According to Diet, at 6 Months and 2 Years.*
| Variable | Low Fat, Average Protein | Low Fat, High Protein | High Fat, Average Protein | High Fat, High Protein | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6-Mo Value | Change from Baseline |
2-Yr Value |
Change from Baseline |
6-Mo Value | Change from Baseline |
2-Yr Value |
Change from Baseline |
6-Mo Value | Change from Baseline |
2-Yr Value |
Change from Baseline |
6-Mo Value | Change from Baseline |
2-Yr Value |
Change from Baseline |
|
| Risk factors† | ||||||||||||||||
| Cholesterol (mg/dl) | ||||||||||||||||
| Total | 188±36 | −5.9 | 192±37 | −3.7 | 193±39 | −4.9 | 197±40 | −2.9 | 195±39 | −3.7 | 202±39 | −0.3 | 199±35 | −2.3 | 202±38 | −0.8 |
| LDL | 116±29 | −6.6 | 117±31 | −5.9 | 120±33 | −4.8 | 121±33 | −3.9 | 123±33 | −3.2 | 127±33 | −0.2 | 124±31 | −1.1 | 124±31 | −1.3 |
| HDL | 49±13 | −0.4 | 51±15 | 5.6 | 51±13 | 2.7 | 53±15 | 6.5 | 49±13 | 2.9 | 51±13 | 6.3 | 53±15 | 4.0 | 55±17 | 8.8 |
| Triglycerides (mg/dl) | 116±73 | −14.2 | 120±83 | −11.5 | 114±63 | −20.4 | 120±67 | −16.6 | 120±88 | −18.1 | 129±89 | −12.4 | 114±71 | −19.5 | 118±71 | −16.7 |
| Blood pressure (mm Hg) | ||||||||||||||||
| Systolic | 116±12 | −1.2 | 117±12 | −0.8 | 117±12 | −2.6 | 118±13 | −1.7 | 118±12 | −1.5 | 118±12 | −1.3 | 119±12 | −1.7 | 120±14 | −0.7 |
| Diastolic | 74±9 | −1.4 | 74±9 | −0.8 | 73±9 | −3.1 | 74±9 | −1.3 | 74±9 | −2.3 | 75±9 | −1.5 | 74±9 | −1.8 | 76±9 | −0.3 |
| Glucose (mg/dl) | 90±11 | −3.0 | 94±12 | 1.1 | 90±16 | −2.6 | 93±17 | 1.0 | 90±12 | −1.9 | 93±13 | 1.6 | 91±12 | −1.2 | 94±15 | 2.8 |
| Insulin (μU/ml) | 10±7 | −16.2 | 12±10 | −2.4 | 10±6 | −19.9 | 11±8 | −11.5 | 10±7 | −18.2 | 12±8 | −6.4 | 10±9 | −14.4 | 11±7 | −9.2 |
| HOMA | 2.3±1.6 | −18.7 | 2.8±2.3 | −1.4 | 2.2±1.6 | −22.7 | 2.5±2.2 | −10.4 | 2.4±1.8 | −18.6 | 2.8±2.1 | −3.5 | 2.4±2.9 | −13.4 | 2.6±1.9 | −6.3 |
| Nutrient intake per day | ||||||||||||||||
| Energy (kcal) | 1636±484 | −477 | 1531±480 | −554 | 1572±568 | −353 | 1560±461 | −402 | 1607±499 | −456 | 1521±530 | −434 | 1624±484 | −385 | 1413±427 | −389 |
| Carbohydrate (%) | 57.5±11.1 | 12.8 | 53.2±11 | 9.3 | 53.4±8.5 | 7.4 | 51.3±9.2 | 6.8 | 49.1±8.6 | 5.0 | 48.6±10 | 2.4 | 43±6.7 | −0.2 | 42.9±8.3 | −0.4 |
| Protein (%) | 17.6±3.4 | 0.2 | 19.6±3.9 | 2.1 | 21.8±3.8 | 3.9 | 20.8±4 | 2.5 | 18.4±4.5 | 0.5 | 19.6±5.2 | 2.1 | 22.6±4.4 | 4.3 | 21.2±5.2 | 3.4 |
| Fat (%) | 6.2±8 | −11.8 | 26.5±8 | −12.0 | 25.9±6.8 | −10.1 | 28.4±8.1 | −8.4 | 33.9±6.7 | −3.8 | 33.3±8.2 | −3.5 | 34.3±7.8 | −3.7 | 35.1±7 | −3.4 |
| Saturated fat (%) | 7.5±3.2 | −4.9 | 8±3.1 | −4.3 | 7.9±2.7 | −3.9 | 8.9±3.8 | −3.1 | 9±2.5 | −3.0 | 9.8±3.3 | −2.1 | 9±2.6 | −3.7 | 10.5±2.7 | −1.7 |
| Biomarkers of adherence | ||||||||||||||||
| Urinary nitrogen (g)‡ | 11.1±4.1 | −11.5 | 11.8±4.6 | −9.1 | 11.9±4.3 | −2.5 | 11.8±3.9 | −2.8 | 10.3±4.4 | −17.3 | 11.2±3.8 | −8.8 | 12.6±4.7 | 0.7 | 12.5±5.3 | −1.9 |
| Respiratory quotient§ | 0.84±0.04 | 0.58 | 0.83±0.04 | −0.48 | 0.84±0.04 | 0.16 | 0.84±0.04 | −0.84 | 0.84±0.04 | −1.58 | 0.83±0.04 | −3.16 | 0.84±0.04 | −0.52 | 0.83±0.04 | −1.92 |
Plus–minus values are means ±SD. Change from baseline is percent change in the case of risk factors and biomarkers of adherence and actual change in the case of nutrient intake per day. Nutrient intake was determined by three 24-hour recalls. To convert the values for cholesterol to millimoles per liter, multiply by 0.02586. To convert the values for triglycerides to millimoles per liter, multiply by 0.01129. To convert the values for glucose to millimoles per liter, multiply by 0.05551. HDL denotes high-density lipoprotein, HOMA homeostasis model assessment of insulin sensitivity, and LDL low-density lipoprotein.
Data were included for 201 participants per group; missing values were imputed.
Data were included for 200 to 204 participants per group at baseline, 139 to 153 at 6 months, and 88 to 109 at 2 years.
Data were included for 201 to 204 participants per group at baseline, 157 to 164 at 6 months, and 113 to 132 at 2 years.
ADHERENCE, DIET ACCEPTABILITY, SATIETY, AND SATISFACTION
Mean reported intakes at 6 months and 2 years did not reach the target levels for macronutrients (Table 2). The reported intakes represented differences from target levels of fat, protein, and carbohydrate intake of 8.0, 4.2, and 14.4 percentage points, respectively, at 6 months and 6.7, 1.4, and 10.2 percentage points, respectively, at 2 years. Reported energy intakes and physical activity were similar among the diet groups. The participants who completed the study had a mean weight loss of 6.5 kg at 6 months, which corresponds to a reduction in daily energy intake of approximately 225 kcal.
There was a larger increase from baseline in the HDL cholesterol level, a biomarker for dietary carbohydrate, in the lowest-carbohydrate group than in the highest-carbohydrate group (a difference in the change of 2 mg per deciliter at 2 years) (Table 1 in the Supplementary Appendix); this difference corresponds to a predicted difference in carbohydrate intake of 6%.36 There was a larger decrease in urinary nitrogen excretion from baseline in the average-protein group than in the high-protein group (a difference in the change of 1.6 g at 6 months and 0.8 g at 2 years) (Table 3); these differences correspond to a difference in dietary protein of 10 g per day and 5 g per day, respectively. The respiratory quotient was 0.84 at baseline in both the high-fat and low-fat groups, and the between-group difference in the change at 2 years (the value in the high-fat group minus the value in the low-fat group) was −0.02 (P = 0.002) (Table 3). Thus, changes in biomarkers confirmed that differences among the groups in macronutrient intake were consistent with those recorded in the dietary reports and that participants modified their intake of macronutrients in the direction of the goals, although the targets were not fully achieved.
Table 3.
Factorial-Design Estimates of Effect of Diet Type on Mean Changes from Baseline in Risk Factors, Nutrient Intake, and Biomarkers of Adherence.*
| Variable | Change with High Fat minus Change with Low Fat | Change with High Protein minus Change with Average Protein | Change with Highest Carbohydrate minus Change with Lowest Carbohydrate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At 6 Mo | P Value | At 2 Yr | P Value | At 6 Mo | P Value | At 2 Yr | P Value | At 6 Mo | P Value | At 2 Yr | P Value | |
| Risk factors† | ||||||||||||
| Cholesterol (mg/dl) | ||||||||||||
| Total | 4.7±1.8 | 0.01 | 5.6±1.9 | 0.003 | 2.3±1.8 | 0.20 | 0.2±1.9 | 0.92 | −7.0±2.6 | 0.007 | −5.8±2.6 | 0.02 |
| LDL | 4.4±1.6 | 0.005 | 5.1±1.6 | 0.001 | 2.4±1.6 | 0.13 | 0.5±1.6 | 0.74 | −6.8±2.3 | 0.003 | −5.7±2.2 | 0.01 |
| HDL | 1.1±0.5 | 0.01 | 0.7±0.5 | 0.12 | 1.1±0.5 | 0.02 | 0.9±0.5 | 0.05 | −2.2±0.6 | 0.001 | −1.7±0.7 | 0.01 |
| Triglycerides (mg/dl) | −2.8±4.3 | 0.52 | −1.2±4.0 | 0.76 | −5.4±4.3 | 0.21 | −6.7±4.0 | 0.10 | 8.1±5.0 | 0.10 | 7.9±6.0 | 0.19 |
| Blood pressure (mm Hg) | ||||||||||||
| Systolic | 0.4±0.7 | 0.59 | 0.3±0.7 | 0.64 | −1.0±0.7 | 0.14 | −0.2±0.7 | 0.77 | 0.6±0.9 | 0.51 | −0.1±0.9 | 0.89 |
| Diastolic | 0.1±0.5 | 0.77 | 0.1±0.5 | 0.85 | −0.5±0.5 | 0.32 | 0.2±0.5 | 0.59 | 0.3±0.7 | 0.62 | −0.3±0.7 | 0.61 |
| Glucose (mg/dl) | 1.2±0.6 | 0.04 | 1.1±0.5 | 0.05 | 0.5±0.6 | 0.38 | 0.5±0.6 | 0.34 | −1.7±0.9 | 0.04 | −1.6±0.8 | 0.06 |
| Insulin (μU/ml) | 0.2±0.4 | 0.68 | −0.1±0.4 | 0.77 | 0.0±0.4 | 0.91 | −0.7±0.4 | 0.07 | −0.2±0.7 | 0.74 | 0.8±0.6 | 0.19 |
| HOMA | 0.13±0.13 | 0.31 | 0.03±0.10 | 0.78 | 0.03±0.13 | 0.84 | −0.16±0.10 | 0.12 | −0.15±0.21 | 0.46 | 0.13±0.16 | 0.42 |
| Nutrient intake per day | ||||||||||||
| Energy (kcal) | 11.4±53.9 | 0.83 | −75.6±70.9 | 0.29 | −23.2±53.9 | 0.67 | −35.5±71.0 | 0.62 | 11.1±71.8 | 0.88 | 118.1±96.6 | 0.23 |
| Carbohydrate (%) | −9.5±1.0 | <0.001 | −6.4±1.5 | <0.001 | −5.2±1.1 | <0.001 | −3.6±1.5 | 0.02 | 14.4±1.4 | <0.001 | 10.2±2.1 | <0.001 |
| Protein (%) | 0.9±0.5 | 0.06 | 0.2±0.7 | 0.77 | 4.2±0.4 | <0.001 | 1.4±0.7 | 0.05 | −5.0±0.6 | <0.001 | −1.6±1.0 | 0.10 |
| Fat (%) | 8.0±0.8 | <0.001 | 6.7±1.2 | <0.001 | 0.2±0.9 | 0.82 | 1.8±1.3 | 0.15 | −8.1±1.2 | <0.001 | −8.6±1.6 | <0.001 |
| Saturated fat (%) | 1.3±0.3 | <0.001 | 1.7±0.5 | <0.001 | 0.2±0.3 | 0.43 | 0.8±0.5 | 0.12 | −1.5±0.4 | 0.001 | −2.5±0.6 | <0.001 |
| Biomarkers of adherence | ||||||||||||
| Urinary nitrogen (g)‡ | −0.11±0.39 | 0.77 | 0.08±0.42 | 0.84 | 1.64±0.38 | <0.001 | 0.81±0.42 | 0.06 | −1.50±0.55 | 0.006 | −0.89±0.65 | 0.18 |
| Respiratory quotient§ | −0.01±0.00 | 0.005 | −0.02±0.00 | 0.002 | 0.00±0.00 | 0.52 | 0.00±0.00 | 0.51 | 0.01±0.01 | 0.13 | 0.01±0.01 | 0.07 |
Plus–minus values are means ±SE. Nutrient intake was determined by three 24-hour recalls. To convert the values for cholesterol to millimoles per liter, multiply by 0.02586. To convert the values for triglycerides to millimoles per liter, multiply by 0.01129. To convert the values for glucose to millimoles per liter, multiply by 0.05551. HDL denotes high-density lipoprotein, HOMA homeostasis model assessment of insulin sensitivity, and LDL low-density lipoprotein.
Data were included for 201 participants per group; missing values were imputed.
Data were included for 200 to 204 participants per group at baseline, 139 to 153 at 6 months, and 88 to 109 at 2 years.
Data were included for 201 to 204 participants per group at baseline, 157 to 164 at 6 months, and 113 to 132 at 2 years.
Craving, fullness, and hunger and diet-satisfaction scores were similar at 6 months and at 2 years among the diets (Table 2 in the Supplementary Appendix).
WEIGHT CHANGE ACCORDING TO ATTENDANCE AT GROUP SESSIONS AND DIETARY ADHERENCE
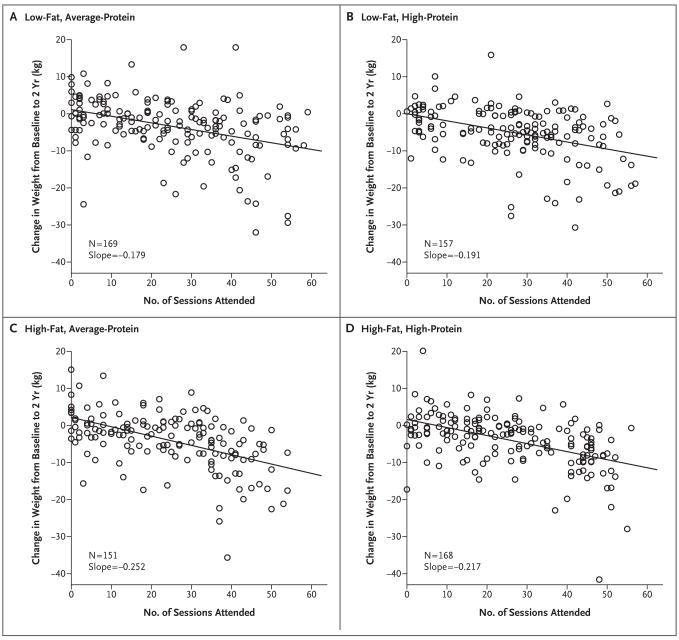
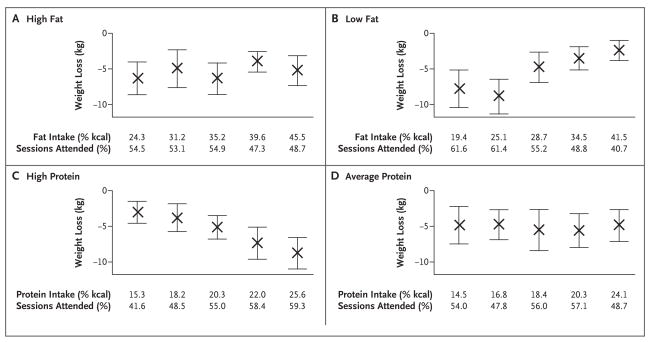
Attendance at group sessions strongly predicted weight loss at 2 years (0.2 kg for every session attended) and was similar among the diet groups (P = 0.22 for a test of difference in slopes) (Fig. 3). Adherence to the goal for protein intake was associated with more weight loss only in the high-protein groups, and adherence to the goal for fat intake was associated with more weight loss only in the low-fat groups (P<0.001) (Fig. 4). The ranges of protein and fat intakes overlapped substantially in the diet groups. Thus, a low-fat intake of 25% was associated with increased weight loss in the low-fat groups but not in the high-fat groups, and a high-protein intake of 24 to 25% was associated with increased weight loss in the high-protein groups but not in the average-protein groups. Attendance at group sessions was associated with adherence to the fat and protein goals only in the high-protein and low-fat groups (Fig. 4).
Figure 3. Change in Body Weight from Baseline to 2 Years According to Attendance at Counseling Sessions for Weight Loss, among the 645 Participants Who Completed the Study.
Panel A shows data for the low-fat, average-protein group; Panel B, for the low-fat, high-protein group; Panel C, for the high-fat, average-protein group; and Panel D, for the high-fat, high-protein group. There were no significant differences among the regression coefficients (P>0.2 for all comparisons; R2 = 0.2 for total cohort).
Figure 4. Weight Loss at 2 Years According to Adherence to Dietary Fat and Protein Goals.
Intake was determined from three 24-hour diet recalls. Quintiles of fat and protein intakes are shown for the combined high-fat groups (Panel A), low-fat groups (Panel B), high-protein groups (Panel C), and average-protein groups (Panel D); there were 45 to 51 participants per quintile. Rates of attendance at group sessions (percent of total sessions attended over the 2-year period) are shown for the quintiles of fat and protein intake. I bars indicate 95% confidence intervals. P values for a trend in weight loss across quintiles are as follows: P<0.001 for fat intake in low-fat groups, P<0.001 for protein intake in high-protein groups, P = 0.36 for fat intake in high-fat groups, and P = 0.83 for protein intake in average-protein groups. The results were similar when determined within each of the four diet groups (data not shown).
ADVERSE EFFECTS
Serious adverse events were reported by 57 participants (7%); there were no significant differences in the rates among diets. The ratio of urinary microalbumin to creatinine was more than 30 in five participants in the average-protein group and in five participants in the high-protein group at 6 months and in seven participants, all in the average-protein groups, at 2 years.
DISCUSSION
In this population-based trial, participants were assigned to and taught about diets that emphasized different contents of carbohydrates, fat, and protein and were given reinforcement for 2 years through group and individual sessions. The principal finding is that the diets were equally successful in promoting clinically meaningful weight loss and the maintenance of weight loss over the course of 2 years. Satiety, hunger, satisfaction with the diet, and attendance at group sessions were similar for all diets. The diets improved lipid risk factors and fasting insulin levels in the directions that would be expected on the basis of macronutrient content. The study had a large sample, a high rate of retention, and the sensitivity to detect small changes in weight. The population was diverse with respect to age, income, and geography and included a large percentage of men. The participants were eager to lose weight and to attempt whatever type of diet they were assigned, and they did well in screening interviews and questionnaires that evaluated their motivation. Thus, the findings should be directly applicable to both clinicians’ recommendations for weight loss in individual patients and the development of population-wide recommendations by public health officials.
Despite the intensive behavioral counseling in our study, participants had difficulty achieving the goals for macronutrient intake of their assigned group. The mean differences among the groups in fat, carbohydrate, or protein intake at 6 months were nevertheless often greater than those in several previous trials comparing diets for weight loss.11,12,19,21,26 Substantially diminished adherence after the first few months is typical in weight-loss trials5,6,8,10–12,19,21,24,26 and occurred between 6 months and 2 years in our trial. Only two trials have reported dietary intake beyond 1 year,12,26 and one of them provided foods to the participants.12 In addition, trials of low-carbohydrate diets have reported a very low incidence of urinary ketosis after 6 months,6,8,12 suggesting that in most overweight people, it is futile to sustain a low intake of carbohydrates. Overall, these findings with respect to adherence to macronutrient goals suggest that participants in weight-loss programs revert to their customary macronutrient intakes over time but may nonetheless be able to maintain weight loss.
We explored the association of achieved nutrient intakes with weight loss. We caution that these post hoc analyses do not have the strong validity of the main analysis of this controlled trial, which compared randomized groups. Protein and fat intakes overlapped among the groups. A high-protein intake was associated with weight loss only in the high-protein groups, and a low-fat intake was associated with weight loss only in the low-fat groups. The protein and fat contents of the participants’ usual diet were closer to the goals for the average-protein and high-fat diets than to those for the high-protein and low-fat diets. Thus, the participants assigned to an average-protein or high-fat diet did not have to change their customary level of dietary protein and fat very much and could focus more on reducing dietary intake. In contrast, the participants in the high-protein or low-fat groups had more challenging dietary goals. It is therefore not surprising that attendance at group sessions was strongly related to adherence to high-protein or low-fat goals but not to the goals in the average-protein or high-fat groups. However, attendance had a strong association with weight loss, and the association was similar across diet groups. We view attendance at counseling sessions as a proxy for commitment to achieving weight loss and for engagement in the program. Study participants who attended two thirds of the sessions over the course of 2 years lost about 9 kg of weight. Regain after 6 to 12 months was about 20% of the regain reported in earlier trials.28 Several recent trials have also shown that continued contact with participants after weight loss is associated with less regain.12,24,37,38 These findings together point to behavioral factors rather than macronutrient metabolism as the main influences on weight loss.
Conformity to cultural norms, scientific novelty, and media attention are nonbiologic reasons for the success of specific diets. We used a generic approach to developing each diet and the instructions for following it, in order to minimize such influences. No diet was considered to be a control diet, and the dietary counseling and the attention that we provided were the same for all diet groups throughout the study period. We did not confirm previous findings that low-carbohydrate or high-protein diets caused increased weight loss at 6 months3–12 and that the advantage of these diets usually eroded by 12 months, with weight loss that was nearly or fully equivalent to that with low-fat diets6,11,18 or other diets.12 Other studies showed increased weight loss at 1 to 2 years with diets that were high in unsaturated fat12,21,26 or with low-fat, high-carbohydrate vegetarian diets.22,24 These divergent results suggest that any type of diet, when taught for the purpose of weight loss with enthusiasm and persistence, can be effective. When nonnutritional influences are minimized, as they were in our study, the specific macronutrient content is of minor importance, as was suggested many years ago.39
In conclusion, diets that are successful in causing weight loss can emphasize a range of fat, protein, and carbohydrate compositions that have beneficial effects on risk factors for cardiovascular disease and diabetes.29,40 Such diets can also be tailored to individual patients on the basis of their personal and cultural preferences and may therefore have the best chance for long-term success.
Supplementary Material
Acknowledgments
Supported by grants from the National Heart, Lung, and Blood Institute (HL073286) and the General Clinical Research Center, National Institutes of Health (RR-02635).
Dr. Greenway reports receiving consulting fees from or serving on a paid advisory board for Anian, Bristol-Myers Squibb, Clarus Health, Encore Pharmaceutical, Leptos Biomedical, MDRNA, Novo Nordisk, General Nutrition Corporation, Catalyst, Jenny Craig, Orexigen, Lithera, and Basic Research, receiving lecture fees from BAROnova, Lazard, and Biologene, and owning equity in Lithera. No other potential conflict of interest relevant to this article was reported. Dr. Ryan is chairperson of the Obesity Committee of the National Heart, Lung, and Blood Institute’s Clinical Guidelines for Cardiovascular Risk Reduction Expert Panel; Dr. Loria is a member of that committee; and Dr. Sacks is a member of the Lifestyle Working Group of the Expert Panel that interacts with the Obesity Committee. Dr. Sacks is also vice-chair of the Nutrition Committee of the American Heart Association, which advises the Association on nutrition topics, including those related to overweight and obesity.
We thank the participants in the trial for their dedication and contribution to the research; the following research staff members for their assistance in conducting the trial: Jungnam Joo, Ph.D., and Charlotte A. Pratt, Ph.D., at the National Heart, Lung, and Blood Institute; Patricia Copeland, M.S., R.D., at Harvard School of Public Health; Cassandra Carrington, Jacqueline Gallagher, Clota Heazel, Megan Reddy, Alison Barr, M.S., R.D., Mary Dinehart, M.S., R.D., Marit Pywell, R.D., Dawn Quintino, M.S., R.D., Audrey Shweky, M.S., R.D., Benjamin Harshfield, and Melissa McEnery-Stonelake at Brigham and Women’s Hospital; and Julia St. Amant, Elizabeth Tucker, Heidi K. Millet, Marisa M. Smith, Sara J. Schoen, R.D., L.D.N., Betsy B. Bernhard, Courtney Brock, R.D., Laura DeCuir Moran, R.D., Katherine Lastor, R.D., Erma Levy, M.P.H., R.D., Lisa Miller, R.D., Gina Pennington, R.D., Dana Vieselmeyer, M.P.H., R.D., Marlene Afton, Lindsay Coates, Dawn Turner, Richard Dale Achord, Bridget Conner, Margaret Graves, Doris Hoffpauir, Carla Kimmel, Steve Lee, Kelli Melancon, Sandra Richard, Stacey Roussel, Elizabeth Soroe, Denise Stein, Jamie Tuminello, and Connie Murla at Pennington Biomedical Research Center; and the members of the data and safety monitoring board: Barbara V. Howard, Ph.D. (chair), Phyllis E. Bowen, Ph.D., Daniel W. Jones, M.D., Michael G. Perri, Ph.D., David M. Reboussin, Ph.D., and Marcia L. Stefanick, Ph.D.
References
- 1.Jéquier E, Bray GA. Low-fat diets are preferred. Am J Med. 2002;113(Suppl):41S–46S. doi: 10.1016/s0002-9343(01)00991-3. [DOI] [PubMed] [Google Scholar]
- 2.Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med. 2002;113(Suppl):47S–59S. doi: 10.1016/s0002-9343(01)00992-5. [DOI] [PubMed] [Google Scholar]
- 3.Freedman MR, King J, Kennedy E. Popular diets: a scientific review. Obes Res. 2001;9(Suppl):1S–40S. doi: 10.1038/oby.2001.113. [DOI] [PubMed] [Google Scholar]
- 4.Skov AR, Toubro S, Rønn B, Holm L, Astrup A. Randomized trial of protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord. 1999;23:528–36. doi: 10.1038/sj.ijo.0800867. [DOI] [PubMed] [Google Scholar]
- 5.Brehm BJ, Seeley RJ, Daniels SR, D’Alessio DA. A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. J Clin Endocrinol Metab. 2003;88:1617–23. doi: 10.1210/jc.2002-021480. [DOI] [PubMed] [Google Scholar]
- 6.Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082–90. doi: 10.1056/NEJMoa022207. [DOI] [PubMed] [Google Scholar]
- 7.Samaha FF, Iqbal N, Seshadri P, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003;348:2074–81. doi: 10.1056/NEJMoa022637. [DOI] [PubMed] [Google Scholar]
- 8.Yancy WS, Jr, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. 2004;140:769–77. doi: 10.7326/0003-4819-140-10-200405180-00006. [DOI] [PubMed] [Google Scholar]
- 9.Volek J, Sharman M, Gómez A, et al. Comparison of energy-restricted very low-carbohydrate and low-fat diets on weight loss and body composition in overweight men and women. Nutr Metab (Lond) 2004;1:13. doi: 10.1186/1743-7075-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Due A, Toubro S, Skov AR, Astrup A. Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord. 2004;28:1283–90. doi: 10.1038/sj.ijo.0802767. [DOI] [PubMed] [Google Scholar]
- 11.Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A to Z Weight Loss Study: a randomized trial. JAMA. 2007;297:969–77. doi: 10.1001/jama.297.9.969. [Erratum, JAMA 2007;298: 178.] [DOI] [PubMed] [Google Scholar]
- 12.Shai I, Schwarzfuchs D, Henkin Y, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–41. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 13.Noakes M, Keough JB, Foster PR, Clifton PM. Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional low-fat, high-carbohydrate diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr. 2005;81:1298–306. doi: 10.1093/ajcn/81.6.1298. [DOI] [PubMed] [Google Scholar]
- 14.McLaughlin T, Carter S, Lamendola C, et al. Effects of moderate variations in macronutrient composition on weight loss and reduction in cardiovascular disease risk in obese, insulin-resistant adults. Am J Clin Nutr. 2006;84:813–21. doi: 10.1093/ajcn/84.4.813. [DOI] [PubMed] [Google Scholar]
- 15.McMillan-Price J, Petocz P, Atkinson F, et al. Comparison of 4 diets of varying glycemic load on weight loss and cardiovascular risk reduction in overweight and obese young adults: a randomized controlled trial. Arch Intern Med. 2006;166:1466–75. doi: 10.1001/archinte.166.14.1466. [DOI] [PubMed] [Google Scholar]
- 16.Das SK, Gilhooly CH, Golden JK, et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am J Clin Nutr. 2007;85:1023–30. doi: 10.1093/ajcn/85.4.1023. [DOI] [PubMed] [Google Scholar]
- 17.Lecheminant JD, Gibson CA, Sullivan DK, et al. Comparison of a low carbohydrate and low fat diet for weight maintenance in overweight or obese adults enrolled in a clinical weight management program. Nutr J. 2007;6:36. doi: 10.1186/1475-2891-6-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. 2004;140:778–85. doi: 10.7326/0003-4819-140-10-200405180-00007. [DOI] [PubMed] [Google Scholar]
- 19.Dansinger ML, Gleason JA, Griffith JL, Selker JP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293:43–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 20.Luscombe-Marsh ND, Noakes M, Wittert GA, Keough JB, Foster P, Clifton PM. Carbohydrate restricted diets high in either monounsaturated fat or protein are equally effective in promoting fat loss and improving blood lipids. Am J Clin Nutr. 2005;81:762–72. doi: 10.1093/ajcn/81.4.762. [DOI] [PubMed] [Google Scholar]
- 21.Keogh JB, Luscombe-Marsh ND, Noakes M, Wittert GA, Clifton PM. Long-term weight maintenance and cardiovascular risk factors are not different following weight loss on carbohydrate-restricted diets high in either monounsaturated fat or protein in obese hyperinsulinemic men and women. Br J Nutr. 2007;97:405–10. doi: 10.1017/S0007114507252687. [DOI] [PubMed] [Google Scholar]
- 22.Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–7. doi: 10.1001/jama.280.23.2001. [Erratum, JAMA 1999;281: 1380.] [DOI] [PubMed] [Google Scholar]
- 23.Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29:1777–83. doi: 10.2337/dc06-0606. [DOI] [PubMed] [Google Scholar]
- 24.Turner-McGrievy GM, Barnard ND, Scialli AR. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity (Silver Spring) 2007;15:2276–81. doi: 10.1038/oby.2007.270. [DOI] [PubMed] [Google Scholar]
- 25.Toubro S, Astrup A. Randomized comparison of diets for maintaining obese subjects’ weight after major weight loss: ad lib, low fat, high carbohydrate diet v fixed energy intake. BMJ. 1997;314:29–34. doi: 10.1136/bmj.314.7073.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McManus K, Antinoro L, Sacks F. A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, low-energy diet for weight loss in overweight adults. Int J Obes Relat Metab Disord. 2001;25:1503–11. doi: 10.1038/sj.ijo.0801796. [DOI] [PubMed] [Google Scholar]
- 27.Simons-Morton DG, Obarzanek E, Cutler JA. Obesity research — limitations of methods, measurements, and medications. JAMA. 2006;295:826–8. doi: 10.1001/jama.295.7.826. [DOI] [PubMed] [Google Scholar]
- 28.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147:41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- 29.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [Errata, Circulation 2006;114(1): e27, 114(23):e629.] [DOI] [PubMed] [Google Scholar]
- 30.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–42. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 31.Champagne CM, Bogle ML, McGee BB, et al. Dietary intake in the lower Mississippi delta region: results from the Foods of Our Delta Study. J Am Diet Assoc. 2004;104:199–207. doi: 10.1016/j.jada.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 32.Flint A, Raben A, Blundell JE, Astrup A. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord. 2000;24:38–48. doi: 10.1038/sj.ijo.0801083. [DOI] [PubMed] [Google Scholar]
- 33.Urban N, White E, Anderson GL, Curry S, Kristal AR. Correlates of maintenance of a low-fat diet among women in the Women’s Health Trial. Prev Med. 1992;21:279–91. doi: 10.1016/0091-7435(92)90027-f. [DOI] [PubMed] [Google Scholar]
- 34.Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C. Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med. 2001;161:218–27. doi: 10.1001/archinte.161.2.218. [DOI] [PubMed] [Google Scholar]
- 35.Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Bethesda, MD: National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, 2002. (NIH publication no. 02–5215.)
- 36.Mensink RP, Zock PL, Kester AD, Katan MB. Effect of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146–55. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 37.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355:1563–71. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 38.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the Weight Loss Maintenance randomized controlled trial. JAMA. 2008;299:1139–48. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 39.Kinsell LW, Gunning B, Michaels GD, Richardson J, Cox SE, Lemon C. Calories do count. Metabolism. 1964;13:195–204. doi: 10.1016/0026-0495(64)90098-8. [DOI] [PubMed] [Google Scholar]
- 40.de Souza RJ, Swain JF, Appel LJ, Sacks FM. Alternatives for macronutrient intake and chronic disease: a comparison of the OmniHeart diets with popular diets and with dietary recommendations. Am J Clin Nutr. 2008;88:1–11. doi: 10.1093/ajcn/88.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.