Abstract
Background
Long-term nursing home care is primarily funded by out-of-pocket payments and public Medicaid programs. Few studies have explored price growth in nursing home care, particularly trends in the real cost of a year spent in a nursing home.
Objectives
To evaluate changes in private and public prices for annual nursing home care from 1977 to 2004, and to compare nursing home price growth to overall price growth and growth in the price of medical care.
Research Design
We estimated annual private prices for nursing home care between 1977 and 2004 using data from the National Nursing Home Survey. We compared private nursing home price growth to public prices obtained from surveys of state Medicaid offices, and evaluated the Bureau of Labor Statistics Consumer Price Indexes to compare prices for nursing homes, medical care, and general goods and services over time.
Results
Annual private pay nursing homes prices grew by 7.5% annually from $8,645 in 1977 to $60,249 in 2004. Medicaid prices grew by 6.7% annually from $9,491 in 1979 to $48,056 in 2004. Annual price growth for private pay nursing home care outpaced medical care and other goods and services (7.5% vs. 6.6% and 4.4%, respectively) between 1977 and 2004.
Conclusions
The recent rapid growth in nursing home prices is likely to persist, due to an aging population and greater disability among the near-elderly. The result will place increasing financial pressure on Medicaid programs. Better data on nursing prices are critical for policy-makers and researchers.
Keywords: nursing homes, prices, inflation
Introduction
A great deal of attention has been paid to the rising real costs of hospital stays, physician services, and pharmaceuticals. All of these costs have been rising more rapidly than household and national income, placing pressure on public and household budgets. Less attention has been paid to the corresponding trends in nursing home expenditures, which totaled $115.2 billion in 2004, and accounted for 7.4 percent of national health expenditures.1 While Medicare covers short-term, post-acute nursing home care for its beneficiaries, most individuals who require custodial nursing home services pay for care in one of three ways. First, private long-term care insurance purchased at younger ages can be used to cover nursing home expenditures. However, the purchase of such insurance remains relatively rare in the U.S., constituting only 4% of overall nursing home expenditures.2 Second, individuals can pay for their care out-of-pocket. Private payment for nursing home care comprised approximately 40% of non-Medicare nursing home expenditures in 2005.3 Finally, individuals who qualify can turn to public insurance through the Medicaid program for their nursing home costs. Individuals must qualify for Medicaid by meeting income and asset criteria at the time of nursing home entry or by “spending down” during their stay. Medicaid paid approximately 52% of all long-stay nursing home expenditures in 2005.3
The combination of an aging population and increasing life expectancy suggests that the demand for long-term nursing home care will likely increase over the coming decades. These effects may be intensified by the declining health and increasingly unhealthy lifestyles of the near-elderly cohorts now approaching old-age.4 In addition, the demand for long-term care insurance is expected to remain relatively weak.5, 6 As a result, public and personal out-of-pocket expenditures will continue to account for the majority of spending on long-stay nursing home care.
We describe public and private prices of an annual nursing home stay from 1977 to 2004 to better understand historical trends and financial burdens on private and public payers for nursing home care. We also note some of the key limitations of current data sources on nursing home prices. In addition, we evaluate changes in household income, along with the prices of basic goods and services and medical care, between 1977 and 2004 to provide perspective on changes in the affordability of nursing home stays to public and private payers.
Methods
Theoretical Framework
We assess nominal changes in nursing home prices paid by private and public payers. Because the type of nursing and medical care services consumed by residents invariably changes over time, it is not relevant to discuss what would happen to prices if an individual received Year 2000 nursing home care for the next 50 years. This is conceptually different from measuring price growth, or inflation, in the usual sense, where consumers pay more for exactly the same good. For nursing homes, patients receive the standard of care that is current at the time. As a result, price growth in nursing care reflects both “inflation” in the sense of a rising price for the same good, and an increase in the quality of the good itself. Thus, the salient issue is how much it cost in Year X to obtain the standard of medical care that prevailed in Year X. This is actually a much simpler analysis than measuring pure price inflation, because we do not need to hold constant the quality, composition, and nature of the good. Rather, we ask the simpler questions: how much did a nursing home resident pay, and how did this payment change over time? This question bears upon changes in the affordability of nursing home stays to public and private payers. In separate analyses, we evaluate characteristics of nursing homes over time, including nurse staffing levels and dedicated space for residents with cognitive impairments, to determine whether changes in quality may have been an important factor in nursing home price growth.
Data
We used charge data from the current residents' public use file of the National Nursing Home Survey (NNHS) to estimate the price of an annual nursing home stay for private pay residents in 1977, 1985, 1995, 1997, 1999 and 2004. The NNHS is a nationwide survey of nursing homes and their residents conducted by the National Center for Health Statistics (NCHS). Residents whose care was fully or partially covered by Medicaid, Medicare or other payers (i.e. supplemental security income; other governmental assistance or welfare; religious organizations, foundations or agencies; VA contract, pensions or other VA compensation; lifecare; or unspecified) were excluded from these analyses. We calculated annual prices using NNHS re-coded per diem charges for past month or billing period (1997, 1999, and 2004 waves), re-coded total monthly charges (1985 wave), or using total charges billed for the most recent month or billing period (1977 and 1995 waves). We excluded 11 outliers from 1997, 1999 and 2004 waves (n=1, n=1 and n=9, respectively) whose annual nursing home costs were calculated to be more than $1 million. Our final sample included a total of n = 15,170 unweighted residents, including n=2,232 in 1977, n=1,870 in 1985, n=2,643 in 1995, n=3,060 in 1997, n = 3,013 in 1999 and n=2,352 in 2004.
To account for changes in residents' demographics and acuity over time,7 we estimated a linear regression model for annual prices, adjusting for survey year, age, sex, marital status (married vs. not married), race (white, non-hispanic vs. non-white, non-hispanic), primary diagnosis of Alzheimer's disease or related dementias, incontinence of the bowels or bladder, and the number of limitations in activities of daily living (ADLs, including bathing, dressing, eating, toileting, walking and bed and chair mobility). Appendix table 1 shows the survey questions and response categories used to measure these variables in each year. The question wording and response categories changed for several variables over the survey waves, and the dynamic nature of some of these variables may impact our adjusted price estimates. The ADL and dementia variables had the most notable changes in definition over time. In particular, for the ADLs, the NNHS asked whether residents “required” assistance in 1977 and 1985. From 1995 through 1999, the NNHS asked whether residents “currently receive” assistance. In 2004, the NNHS asked about residents' “level of performance” based on 6-levels. We categorized residents as ADL-disabled in 2004 if they required supervision or more. The model used survey weights for each year to reflect the national population of private pay residents.
Table 1.
Facility characteristics that may be related to quality, 1995–2004
| 1995 | 2004 | % Change | |
|---|---|---|---|
| N Homes (weighted)* | 16,717 | 16,081 | |
| Bedsize, % | |||
| 3–49 beds | 16.7 | 14.0 | −16.2% |
| 50–99 beds | 35.6 | 37.7 | 5.9% |
| 100–199 beds | 40.1 | 42.0 | 4.7% |
| 200+ beds | 7.5 | 6.3 | −16.0% |
| Ownership, % | |||
| For-profit | 66.1 | 61.6 | −6.8% |
| Chain member | 54.3 | 54.2 | −0.2% |
| Special beds/areas, % | |||
| Alzheimers and cognitively impaired | 17.6 | 26.8 | 52.3% |
| FTE nursing staff, mean | |||
| All homes | |||
| RNs | 7.7 | 8.8 | 14.3% |
| LPNs | 11.0 | 14.9 | 35.5% |
| CNAs / Nurses' aides | 35.5 | 48.9 | 37.7% |
| Homes with 3–49 beds | |||
| RNs | 3.8 | 4.1 | 7.9% |
| LPNs | 3.9 | 4.0 | 2.6% |
| CNAs / Nurses' aides | 10.3 | 13.1 | 27.2% |
| Homes with 50–99 beds | |||
| RNs | 4.9 | 5.7 | 16.3% |
| LPNs | 7.1 | 9.3 | 31.0% |
| CNAs / Nurses' aides | 24.7 | 31.1 | 25.9% |
| Homes with 100–199 beds | |||
| RNs | 9.4 | 10.3 | 9.6% |
| LPNs | 14.2 | 19.4 | 36.6% |
| CNAs /Nurses' aides | 45.7 | 62.0 | 35.7% |
| Homes with 200+ beds | |||
| RNs | 20.5 | 28.5 | 39.0% |
| LPNs | 27.6 | 43.4 | 57.2% |
| CNAs /Nurses' aides | 88.6 | 150.5 | 69.9% |
The facility weight was used to determine the number of facilities in the sample. The bed weight was used to determine other characteristics of the nursing home. For additional information, see: http://www.cdc.gov/nchs/nnhs.htm
We also evaluated the price of an annual nursing home stay for publicly-funded Medicaid residents from 1979 to 2004 using data from two surveys of state Medicaid offices.8–10 Medicaid typically pays below the private-pay price. Although the growth in Medicaid payment rates is a function of a number of non-market factors (mainly state budgets and the Medicaid rules and regulations), Medicaid payment rate growth is not completely distinct from nursing home market conditions. Many states have tied certain aspects of their rates to price growth in the nursing home sector.9 Thus, the growth in Medicaid rates provides another opportunity to examine spending growth in the nursing home sector. Given fiscal pressures faced by state Medicaid programs, it is expected that the Medicaid rate of growth will be lower than the private price growth. Nevertheless, the growth in Medicaid payment rates for nursing home care can provide a meaningful lower bound on private price growth. The trend data presented in this report exclude Alaska, Hawaii and the District of Columbia. These Medicaid rate data have been used in a number of academic studies.11, 12
We also compare private and Medicaid nursing home prices with U.S. Census Bureau data on median household income for all households and for households age 65 and older between 1977 and 2004.13 We report median household income in current dollars to facilitate comparisons with nursing home prices in each year. Median household income measures buying power for private payers, and also for public payers, whose tax base is driven by household income levels.
To provide some perspective on the observed nursing home price growth rate for private and public payers, we compare inflation rates based on the consumer-price index (CPI), as well as the medical and nursing home CPIs from 1977 to 2004.14 The CPI is a measure of the average change over time in the prices paid by urban consumers for a general market basket of consumer goods and services. In contrast to our analysis of nursing home prices, the general CPI does attempt to hold constant the quality, composition and nature of the goods measured. The medical and nursing home CPIs are a combination of prices paid by consumers either out-of-pocket or through premiums, deductibles and copayments for medical and nursing home care, with some adjustment for quality and composition of the goods and services measured.15 Prices paid by Medicaid or Medicare Part A are not included in the medical care and nursing home CPIs. Both the nursing home and medical care CPIs provide a window into price growth for private payers, but are not necessarily a direct measure of private-pay prices.
Finally, we compared characteristics of nursing homes that are likely related to quality. From the 1995 and 2004 NNHS facility file, we compared nursing home ownership and chain status, bed-size, dedicated space for cognitively impaired residents and the levels of full-time equivalent registered nurses, licensed practical nurses and certified nursing assistants and nurses' aides. The NNHS facility file contains facility-level information on all nursing homes participating in the NNHS. Data on nursing staff levels were not measured consistently between the 1977, 1985 and 2004 NNHS waves, which is why we evaluated nursing home characteristics over the 10 most recent years of the survey. We compare weighted characteristics between the 1995 and 2004 waves without reporting statistical significance, as the 1995 public use facility file does not contain sampling variables to appropriately adjust standard errors. This analysis reveals whether or not reductions in the affordability of nursing home stays are “buying” improvements in quality.
Results
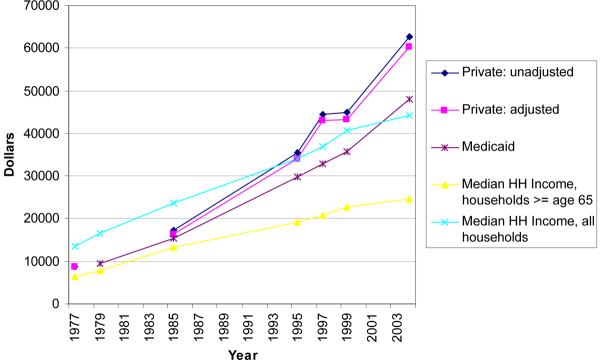
Unadjusted and adjusted NNHS private nursing home prices and Medicaid payments are summarized in Figure 1 along with median household income. Unadjusted private nursing home prices were higher than adjusted prices by $1,000, $1,300, $1500, $1,600 and $2,500 in 1985, 1995, 1997, 1999 and 2004, respectively. In 1977, the average annual adjusted and unadjusted price of private nursing home care was $8,645. The adjusted price increased to $16,306 in 1985, $34,156 in 1995, $42,996 in 1997, $43,212 in 1999 and $60,249 in 2004. Thus, these data indicate an annual average adjusted price growth of approximately 7.5% over the 1977–2004 period. Unadjusted price growth was 7.6% over this same time frame. Over the two most recent waves of the survey (1999–2004), the average annual rate of growth was 6.9%.
Figure 1.
Growth in private and public nursing home prices and household income, 1977–2004*
*Private prices were adjusted for survey year, age, sex, marital status (married vs. not married), race (white, non-hispanic vs. non-white, non-hispanic), primary diagnosis of Alzheimer's disease or related dementias, incontinence of the bowels or bladder, and the number of limitations in activities of daily living (ADLs, including bathing, dressing, eating, toileting, walking and bed and chair mobility).
Figure 1 also presents the annual Medicaid nursing home payment rates from 1979 through 2004. In 1979, the average annual Medicaid payment rate was $9,491. By 2004, the average annual rate was $48,056, implying that Medicaid payments grew at an annual rate of 6.7% over this period. Median household income among elderly households increased from $6,347 in 1977 to $24,516 in 2004, representing an annual growth rate of 5.1%. Among all household ages, median income grew at an annual rate of 4.5% from $13,572 in 1977 to $44,334 in 2004.13
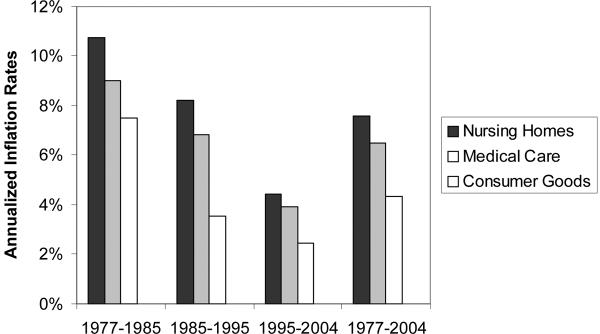
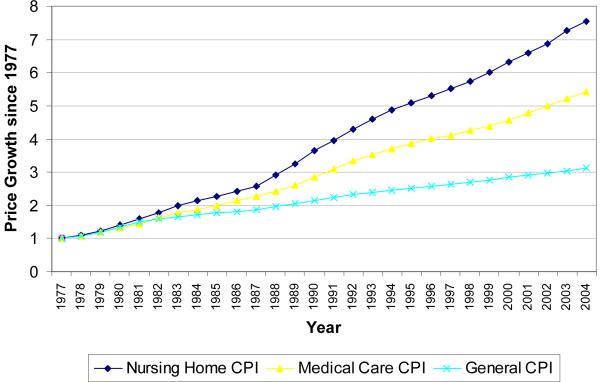
We compare average annual nursing home CPI growth with average annual price growth of the general and medical care CPIs from 1977–2004 as well as from 1977–1985, 1985–1995, and 1995–2004 in Figure 2. In every time period, private-pay nursing home prices grew the most rapidly. Over the entire study period from 1977 to 2004, the estimated annual inflation rate for nursing home care was approximately 7.6% compared to 6.5% for medical care and 4.3% for general goods and services. From 1995 to 2004, when the United States enjoyed historically low levels of overall inflation (2.5%), the annual inflation rate based on the nursing home and medical care CPIs was 4.4% and 3.9%, respectively. Comparing purchasing power over time, we find that $1.00 in 1977 has the same buying power in 2004 as $7.53 using the nursing home CPI, $5.44 using the medical CPI and $3.12 using the general CPI (Figure 3). One striking aspect of the exhibit is the uniformly higher rate of growth in nursing home prices, compared to the prices of other goods and medical care goods. With the exception of a brief period of deceleration in the middle of the 1980s, this pattern is widespread across the entire period of study.
Figure 2.
Annual Price Growth for Nursing Home, Medical Care and Other Goods, 1977–1985, 1985–1995, 1995–2004
Figure 3.
Growth in Nursing Home, Medical Care and overall CPI, 1977–2007
Table 1 describes facility-level characteristics for nursing homes participating in the 1995 and 2004 waves. The distribution of nursing homes by bed size remained similar over time. There were fewer for-profit homes in 2004 compared to 1995 (61.6% vs. 66.1%), although the share maintaining membership in a chain remained relatively constant. More homes had special areas for cognitively impaired residents in 2004 compared to 1995 (26.8% vs. 17.6%). The number of full-time equivalent (FTE) RNs, LPNs and CNAs and nurses' aides increased from 1995 to 2004 across all sizes of nursing homes, with the greatest increase among CNAs and nurses' aides; larger nursing homes generally experienced greater increases in FTEs in each of the nurse categories compared to smaller homes.
Discussion
Policymakers and the public remain continually concerned about the rising price of medical care. It is thus striking to observe that the annual rate of inflation from 1977 to 2004 was higher for nursing home care (range: 6.7% to 7.6%, depending on payer and data source) than medical care (6.6%), both of which far outpaced the rate of general inflation (4.4%) (Table 2). Across the various data sources, there is evidence that the growth rate may have slowed between 1999 and 2004. However, even for these more recent periods, price inflation for nursing home care (range: 4.5% to 6.9%) remained higher than medical care (4.2%) and general price inflation (2.5%). In addition, median household income grew at a slower rate than nursing home prices, underscoring affordability problems over time and the inability of rising household incomes to explain increased nursing home prices.
Table 2.
Summary of Annual NH Price Growth, various time frames
| Data Source | Time Period | Annual Growth |
|---|---|---|
| NNHS private prices* | 1977–2004 | 7.5% |
| NNHS private prices* | 1999–2004 | 6.9% |
| Medicaid payment | 1977–2004 | 6.7% |
| Medicaid payment | 1999–2004 | 5.7% |
| NH CPI | 1977–2004 | 7.6% |
| NH CPI | 1999–2004 | 4.5% |
| Medical care CPI | 1977–2004 | 6.6% |
| Medical care CPI | 1999–2004 | 4.2% |
| General CPI | 1977–2004 | 4.4% |
| General CPI | 1999–2004 | 2.5% |
The persistent growth in price is somewhat surprising from the point of view of the existing literature on nursing home demand, which has identified a number of factors that likely exerted downward pressure on prices. In particular, mortality and disability rates in the elderly population declined over the past 25 years.16–18 Because elderly individuals are at the highest risk of nursing home use, and people are now living longer and healthier lives,16, 17 these trends likely dampened demand for nursing home care and led to lower price growth.19 In addition, male life expectancy increased at a faster rate than female life expectancy, decreasing the gap in longevity between males and females. This trend kept married couples together longer and kept some disabled elderly people out of nursing homes19. Living spouses function as important substitutes for nursing home care: an individual who falls sick has a much greater chance of entering a nursing home if she is unmarried than if she is married.20, 21
Over the past ten to fifteen years, the emergence of alternative and less expensive forms of nursing care, including assisted living, board and care homes and adult day care may have exerted downward pressure on nursing home price growth. Long-term care consumers desire to receive care in the least restrictive setting possible,22 and this preference is reflected in the growth of private spending on services such as assisted living. Expansion in the supply of alternatives to nursing homes ought to have acted as a brake on price growth, at least theoretically. On the other hand, the expansion of alternatives' supply may have been overwhelmed by rising demand for care. The MetLife Survey of Assisted Living Costs indicated that the annual price of assisted living care grew from $25,910 in 2002 to $35,616 in 2006, representing an 8.3% annual growth rate.23, 24 This large growth rate suggests that growing demand for assisted living outpaced short-term supply over this period.
Theoretical work has also posited that variation in private-pay prices will be positively correlated to variation in public payment rates.25 There have been important changes in Medicaid and Medicare payment policies for nursing home care over our period study. On the Medicaid side, there has been widespread adoption of case-mix adjusted payment systems that may have led to increased acuity of Medicaid patients in the nursing home.26 On the Medicare side, the adoption of prospective payment for hospital care in 1983 provided an incentive for hospitals to discharge patients “sicker-and-quicker” to skilled nursing home units, causing tremendous growth in Medicare-financed short-stay nursing home care. 27, 28 In 1998, the Federal government adopted prospective payment for Medicare skilled nursing home services with the goal of slowing the rate of payment growth.29 In spite of these important changes, there has been relatively little research examining the effect of changes in Medicaid and Medicare payment rates on private-pay nursing home prices.30
Improved nursing home quality may be an important factor in rising private and public nursing home prices. For example, we found that almost twice as many nursing homes had dedicated areas for cognitively impaired residents in 2004 compared to 1995. Providing adequate space and staffing levels for these residents may require additional resources, particularly as certain cognitively impaired residents may require additional oversight for various daily activities.31 We also found that overall nurse staffing levels measured by full-time equivalents increased among all sizes of nursing homes between 1995 and 2004. However, most of the nurse staffing growth was among lower-paid CNAs and nurses' aides, who typically have high turnover rates. 32, 33 The increased staffing levels may have had a positive impact on nursing home quality, if patients received more direct nursing care. 34, 35 However, if the increased staffing of CNAs and nurses' aides were associated with greater staff turnover, the impact on quality is more ambiguous.
The federal government's Omnibus Budget Reconciliation Act of 1987 (OBRA) which required nursing homes to use the Resident Assessment Instrument (RAI), a standardized data collection instrument that measures residents' physical and emotional status, as well patient preferences for care,36 may have facilitated quality improvement by allowing nursing homes to more easily identify areas where nursing care may help residents improve or maintain current function. Several studies reported improved quality in various aspects of care after implementation of the OBRA regulations.37–39
Given the large increase in private-pay nursing home prices over time, it will be important to incorporate this measure into future research on nursing homes. Potential sources of private-pay date include public-use surveys, administrative data and market-level data collected by private companies such as the Met Life Survey of Nursing Homes40 and Genworth Financial current cost of care survey.41 Each of these sources has strengths and weaknesses from a research perspective. We chose to use the NNHS due to its large sample size and nationally representative nursing home sample. However, the NNHS has several limitations. As noted previously and in appendix table 1, the NNHS frequently changed the definition and measurement of key variables over survey waves in both the current resident and facility files. These changes make it more difficult to adjust nursing home prices, and there is likely some error in our estimates due to these varying definitions.
In addition, the content of the NNHS changed frequently, precluding use of some variables such as geographic location, certification status, ownership status and bed size as control variables in our model. We also did not have constant measures of nursing home staffing over all survey waves of the facility file and limited these analyses to the most recent decade. Although private price data were collected in each year, these data were re-coded in some waves and not in others, which may result in some inconsistencies. We also do not know which services are included in the private prices paid. Also, the NNHS does not collect information on private versus semi-private rooms in any of the waves, which is likely an important component of private pay prices. Finally, the NNHS public use data files do not allow researchers to link data across the different files, so we were unable to estimate the effect of changes in nursing home characteristics identified in the facility file with prices from the current residents' file. Future waves of the NNHS may want to consider standardizing the survey instruments and allowing linking the datasets to allow for better comparisons over time.
In terms of administrative data, Medicaid nursing home cost reports can be used to construct private prices at the facility, market or state level.42, 43 However, the barriers to using these data are typically high. For example, in order to obtain Medicaid nursing home cost reports, researchers must request data individually from each state and each state's system of data collection and reporting is unique. Grabowski and colleagues linked cost report data from seven states to the MDS and OSCAR systems,44 but most analyses have employed cost report data from a single state. Moreover, there has been relatively little effort to produce summary economic information at the market or state level from these cost reports.
The potential uses of private-pay price data are quite varied. In certain research applications, private prices are a potential omitted right-hand side variable. For example, there is a large nursing home literature examining Medicaid payment rates and nursing home quality.45 An issue in this literature involves the inclusion of private-pay price within the empirical framework. Based on the canonical model of the nursing home,46 private-pay price and quality are chosen jointly by individual nursing homes. However, nearly every study within the literature has taken a “reduced form” approach and excluded endogenous private-pay prices from the model. If a measure of private-pay prices was broadly available, researchers could take a more structural approach by incorporating an instrumented measure into the Medicaid payment-quality analysis.
In other research applications, private-pay prices would serve as an important outcome. For example, a large nursing home literature has examined differences in nonprofit and for-profit nursing homes, with the majority of recent research concluding that nonprofits provide superior quality.47 However, as Hirth (1999) notes, finding quality differences between the two ownership types does not constitute verification of the benefits associated with the nonprofit sector.48 Effectively, nonprofits may crowd high quality for-profits out of the market, ceding the low price/low quality portion of the market to their for-profit competitors. In this environment, quality differences between for-profit and nonprofit homes may be substantial, but prices reflect these differences. Unfortunately, given the lack of available private price data, researchers have not been able to test this conjecture directly.
It will be critical for researchers and public policy makers to have good and comparable data on nursing home prices as the population ages. Over the last 30 years, annual growth in nursing home prices has consistently outpaced the overall rate of inflation, and the rate of inflation in medical care prices. Moreover, this occurred despite favorable trends in household income, longevity, disability and alternative forms of care that depressed growth in the demand for nursing home care. Some of the price growth in nursing home care is likely attributable to improved quality over time. Even if quality remains constant over the coming decades, the growth in nursing home prices is likely to accelerate due to increased demand for nursing home care among the aging baby boom cohort. Thus, the recent history of nursing home price growth may provide a conservative guide to what we can expect in the near future.
Acknowledgments
Supported by a NIA career development award K01 AG024403 (to D.C.G.) and a NIA award R01AG021940 (to D.N.L.).
References
- 1.Health, United States 2006 with Chartbook on Trends in the Health of Americans. 2006 Accessed December 7, 2007, 2007, at http://www.cdc.gov/nchs/data/hus/hus06.pdf. [PubMed]
- 2.Financing Long Term Care for the Elderly. 2004 April; Accessed October 30, 2007, at http://www.cbo.gov/ftpdoc.cfm?index=5400&type=0.
- 3.Catlin A, Cowan C, Heffler S, Washington B, the National Health Accounts Team Trends: National Health Spending in 2005: The Slowdown Continues. Health Affairs. 2007;26(1):142–53. doi: 10.1377/hlthaff.26.1.142. [DOI] [PubMed] [Google Scholar]
- 4.Lakdawalla D, Goldman DP, Bhattacharya J, Hurd MD, Joyce GF, Panis CW. Forecasting the Nursing Home Population. Medical Care. 2003;41(1):8–20. doi: 10.1097/00005650-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Projections of Expenditures for Long-Term Care Services for the elderly. 1999 March; Accessed October 30, 2007, at http://www.cbo.gov/ftpdoc.cfm?index=1123&type=0&sequence=0.
- 6.Brown JR, Finkelstein A. The Interaction of Public and Private Insurance: Medicaid and the Long-Term Care Insurance Market. American Economic Review. 2008;98(3):1083–102. [Google Scholar]
- 7.The Changing Profile of Nursing Home Residents: 1985–1997. Centers for Disease Control and Prevention, National Center for Health Statistics. Accessed October 30, 2007, at http://origin.cdc.gov/nchs/data/ahcd/agingtrends/04nursin.pdf.
- 8.Harrington C, Swan JH, Wellin V, Clemena W, Carrillo HM. 1998 State Data Book on Long Term Care Program and Market Characteristics. Department of Social & Behavioral Sciences, University of California; San Francisco: 1999. [Google Scholar]
- 9.Grabowski DC, Feng Z, Intrator O, Mor V. Recent Trends in State Nursing Home Payment Policies. Health Affairs Suppl Web Exclusives. 2004:W4-363–73. doi: 10.1377/hlthaff.w4.363. [DOI] [PubMed] [Google Scholar]
- 10.Grabowski DC, Feng Z, Intrator O, Mor V. Medicaid Nursing Home Payment and the Role of Provider Taxes. Medical Care Research and Review. 2008 doi: 10.1177/1077558708315968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grabowski DC. Medicaid Reimbursement and the Quality of Nursing Home Care. Journal of Health Economics. 2001;20(4):549–69. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- 12.Intrator O, Mor V. Effect of State Medicaid Reimbursement Rates on Hospitalizations from Nursing Homes. Journal of the American Geriatrics Society. 2004;52(3):393–8. doi: 10.1111/j.1532-5415.2004.52111.x. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Census Bureau Historical Income Tables - Households. 2008 http://wwwcensusgov/hhes/www/income/histinc/h10arhtml Last accessed June 22.
- 14. Accessed at http://www.bls.gov/cpi/.
- 15.Explaining the Consumer Price Index. 2007 Accessed 3 October 2007, at http://www.cbo.gov/ftpdocs/82xx/doc8253/06-22-CPI.pdf.
- 16.Manton KG, Gu X, Lamb VL. Change in Chronic Disability from 1982 to 2004/2005 as Measured by Long-Term Changes in Function and Health in the U.S. Elderly Population. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(48):18374–9. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manton KG, Gu X. Changes in the Prevalence of Chronic Disability in the United States Black and Nonblack Population above age 65 from 1982 to 1999. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(11):6354–9. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cutler DM. Declining Disability among the Elderly. Health Affairs. 2001;20(6):11–27. doi: 10.1377/hlthaff.20.6.11. [DOI] [PubMed] [Google Scholar]
- 19.Lakdawalla D, Philipson T. The Rise in Old-Age Longevity and the Market for Long-Term Care. American Economic Review. 2002;92(1):295–306. doi: 10.1257/000282802760015739. [DOI] [PubMed] [Google Scholar]
- 20.Hungerford T, Rassette M, Iams H, Koenig M. Trends in the economic status of the elderly, 1976–2000. Soc Secur Bull. 2001;64:12–22. [PubMed] [Google Scholar]
- 21.Stern SN. Estimating family long-term care decisions in the presence of endogenous child characteristics. J Hum Resour. 1995;30:551–80. [Google Scholar]
- 22.Kane RL, Kane RA. What Older People Want from Long-Term Care, and How They Can Get It. Health Affairs. 2001;20(6):114–27. doi: 10.1377/hlthaff.20.6.114. [DOI] [PubMed] [Google Scholar]
- 23.MetLife Survey of Assisted Living Costs. Mature Market Institute; 2002. [Google Scholar]
- 24.MetLife Market Survey of Assisted Living Costs. MetLife Mature Market Institute in conjunction with LifePlans, Inc.; 2006. [Google Scholar]
- 25.Norton EC. Long Term Care. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Volume IB. Elsevier Science, B.V.; New York, NY: 2000. [Google Scholar]
- 26.Feng Z, Grabowski DC, Intrator O, Mor V. The effect of state Medicaid case-mix payment on nursing home resident acuity. Health Services Research. 2006;41(4):1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Medicare & Medicaid Services National Health Expenditure Data, Historical. 2008 http://cmshhsgov/NationalHealthExpendData/02_NationalHealthAccountsHistoricalasp#TopOfP age Last accessed June 30.
- 28.Dalton K, Howard HA. Market entry and exit in long-term care: 1985–2000. Health Care Financing Review. 2002;24(2):17–32. [PMC free article] [PubMed] [Google Scholar]
- 29.Konetzka RT, Norton EC, Sloane PD, Kilpatrick KE, Stearns SC. Medicare prospective payment and quality of care for long-stay nursing facility residents. Medical Care. 2006;44(3):270–6. doi: 10.1097/01.mlr.0000199693.82572.19. [DOI] [PubMed] [Google Scholar]
- 30.Nyman JA. The effects of market concentration and excess demand on the price of nursing home care. J Industrial Economics. 1994;42(2):193–204. [Google Scholar]
- 31.Fries BE, Mehr DR, Schneider D, Foley W, Foley J, Burke R. Mental dysfunction and resource use in nursing homes. Medical Care. 1993;31(10):898–920. doi: 10.1097/00005650-199310000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. Gerontologist. 2006;46(1):62–73. doi: 10.1093/geront/46.1.62. [DOI] [PubMed] [Google Scholar]
- 33.Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Medical Care. 2005;43(6):616–26. doi: 10.1097/01.mlr.0000163661.67170.b9. [DOI] [PubMed] [Google Scholar]
- 34.Konetzka R, Stearns S, Park J. The staffing-outcomes relationship in nursing homes. Health Services Research. 2008;43(3):1025–42. doi: 10.1111/j.1475-6773.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schnelle JF, Simmons SF, Harrington C, Cadogan M, Garcia E, Bates-Jensen BM. Relationship of nursing home staffing to quality of care. Health Services Research. 2004;39(2):225–50. doi: 10.1111/j.1475-6773.2004.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Omnibus Budget Reconciliation Act of 1987. Pub. L. No. 100–203, Subtitle C: Nursing Home Reform (1987)
- 37.Zhang X, Grabowski DC. Nursing home staffing and quality under the nursing home reform act. Gerontologist. 2004;44(1):13–23. doi: 10.1093/geront/44.1.13. [DOI] [PubMed] [Google Scholar]
- 38.Hawes C, Mor V, Phillips CD, et al. The OBRA-87 nursing home regulations and implementation of the resident assessment instrument: Effects on process quality. J Am Geriatr Soc. 1997;45(8) doi: 10.1111/j.1532-5415.1997.tb02970.x. [DOI] [PubMed] [Google Scholar]
- 39.Fries BE, Hawes C, Morris JN, Phillips CD, Mor V, Park PS. Effect of the national resident assessment instrument on selected health conditions and problems. J Am Geriatr Soc. 1997;45(8):994–1001. doi: 10.1111/j.1532-5415.1997.tb02972.x. [DOI] [PubMed] [Google Scholar]
- 40.MetLife Market Survey of Nursing Home and Home Care Costs. 2006. [Google Scholar]
- 41.Genworth Financial Genworth Financial 2008 Cost of Care Survey: Home Care Providers, Adult day Health Care Facilities, Assisted Living Facilities and Nursing Homes. 2008 http://wwwgenworthcom/content/etc/medialab/genworth/us/en/Long_Term_CarePar/14291/Filed at/37522%20CoC%20Brochurepdf Last accessed June 30, 2008.
- 42.Mukamel DB, Spector WD. The Competitive Nature of the Nursing Home Industry: Price Mark Ups and Demand Elasticities. Applied Economics. 2002;34(4):413–20. [Google Scholar]
- 43.Troyer JL. Cross-Subsidization in Nursing Homes: Explaining Rate Differentials among Payer Types. Southern Economic Journal. 2002;68(4):750–73. [Google Scholar]
- 44.Grabowski DC, Gruber J, Angelelli JJ. Nursing Home Quality as a Common Good. Review of Economics and Statistics. doi: 10.1162/rest.90.4.754. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grabowski DC, Norton EC. Nursing Home Quality of Care. Edward Elgar Publishing, Inc; Cheltenham, UK: 2006. [Google Scholar]
- 46.Norton EC. Long-Term Care. Elsevier Science, North-Holland; Amsterdam: 2000. [Google Scholar]
- 47.Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: is there any evidence of an association? Medical Care Research and Review. 2005;62(2):139–66. doi: 10.1177/1077558704273769. [DOI] [PubMed] [Google Scholar]
- 48.Hirth RA. Consumer information and competition between nonprofit and for-profit nursing homes. J Health Econ. 1999;18(2):219–40. doi: 10.1016/s0167-6296(98)00035-6. [DOI] [PubMed] [Google Scholar]