By the mid-1950s, a period of tremendous innovation in aortic surgery, all sections of the aorta had been successfully replaced except for the aortic arch. The aortic arch had been particularly challenging to repair, largely because one had to somehow interrupt the natural flow of blood both to the brain and to the downstream organs. At that time, the surgical adjuncts for aortic surgery were in their infancy, and techniques commonly used in modern practice—namely, hypothermia and cardiopulmonary bypass—were so primitive as to be barely recognizable today.
Arch repair with aortic replacement was first attempted by Schafer and Hardin in 1951,1 but uncontrolled ventricular fibrillation (immediately after the final bypass shunt was placed) led to the patient's death 1 hour postoperatively. In 1955, Cooley, Mahaffey, and DeBakey2 used moderate hypothermia and bypass shunts together in an ultimately unsuccessful attempt at arch repair. What was notable about this case is that, although ventricular fibrillation occurred early in the repair (after aortic clamping), it spontaneously corrected itself. Regrettably, the patient did not regain consciousness and died on postoperative day 6. It was not until another emerging technique, cardiopulmonary bypass (which included an early form of antegrade cerebral perfusion), was added that DeBakey and colleagues3 were able to replace the aortic arch successfully. In the late 1960s, the island technique of brachiocephalic vessel reattachment was introduced, which simplified the procedure and reduced the number of anastomoses required.4
Despite these advances, arch-replacement operations were relatively infrequent and continued to have high rates of mortality and neurologic complications. In the mid-1970s, Griepp and colleagues' introduction of hypothermic circulatory arrest (HCA)5 was a major advance that greatly enhanced the safety of arch-replacement procedures, although visualization of the distal anastomosis, hemorrhage, embolization, and the threshold for acceptable durations of cerebral ischemia remained concerns.
Evolution of Open Aortic Arch Repair
Although Griepp's original arch strategy eliminated cannulation of the brachiocephalic vessels, the use of cerebral perfusion was reconsidered by Frist and colleagues.6 Subsequent advances focused on improving brain protection by defining an approximately 30-minute time limit for circulatory arrest,7 which could be extended with cerebral perfusion techniques such as retrograde (RCP) or antegrade cerebral perfusion (ACP).
Although cerebral perfusion has been investigated since the mid-1950s, definitive evidence of the superiority of either retrograde or antegrade perfusion is lacking both because of the prohibitive complexity of performing an adequately powered randomized trial and because of the absence of a universally agreed-upon outcome measure (oxygen saturation, postoperative cognitive performance, death, stroke, etc.). Regardless, selective antegrade cerebral perfusion via axillary artery cannulation appears to be the superior approach, on the basis of decreased oxygen saturation during RCP,8 decreased neurocognitive function after RCP (when compared with circulatory arrest alone9), and recent outcome data on aortic arch repair in which ACP (unlike RCP) appears to neutralize the impact of extended circulatory arrest time on rates of death and stroke.10 The development of softer and more flexible perfusion catheters (to clear the operative field and to minimize cannulation injury)—in addition to the improvement of cerebral monitoring—has greatly improved contemporary survival rates and outcomes after open aortic arch repair.11
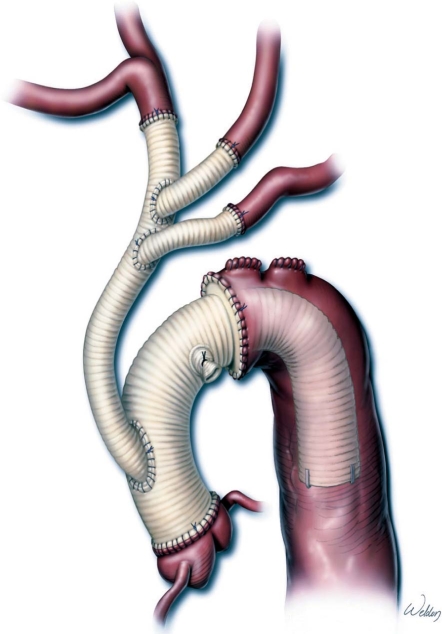
One of the most promising recent innovations in aortic arch repair is the trifurcated graft technique.12,13 In this approach, a trifurcated graft is anastomosed to the branch vessels and ultimately is anastomosed anterolaterally to the newly replaced ascending aorta, which avoids overmanipulation of diseased or atherosclerotic arch vessels and minimizes cerebral ischemia by enabling straightforward antegrade cerebral perfusion. This can be modified as an elephant trunk technique, either for traditional open completion or for “hybrid” endovascular completion. A benefit of this approach to elephant trunk repair is that the distal anastomosis can be brought forward (because it is no longer anatomically limited by the left subclavian artery); this enables better visualization and enhances hemostasis of the distal anastomosis while simultaneously expediting repair and reducing the period of circulatory arrest (Fig. 1).
Fig. 1 A completed aortic arch replacement using a trifurcated graft technique modified as an elephant trunk repair. With this technique, the brachiocephalic vessels are rerouted, and the distal anastomosis is created proximal to the origin of the left common carotid artery. The distal edge of the elephant trunk is marked with surgical clips to facilitate the second stage of the repair.
© 2009 by Baylor College of Medicine, Dr. Joseph Coselli. Used by permission.
Evolution of Endovascular Aortic Arch Repair
Current options for aortic arch repair have grown to encompass several distinct endovascular strategies, including both purely endovascular and “hybrid” endovascular and surgical approaches. Purely endovascular approaches are largely experimental and range from using single-branched endovascular devices (designed to incorporate the left subclavian artery) to using triple-branched or triple-fenestrated stent-grafts to repair the aortic arch.14–17 These techniques are performed only in highly specialized centers. Hybrid repairs, which are in wider use at more centers, involve “debranching” some or all of the brachiocephalic arteries—thereby essentially lengthening the branchless aorta—and then using standard “tube” stent-grafts to exclude the diseased portion of the aortic arch.
Theoretically, hybrid and purely endovascular aortic arch repairs should have lower short-term mortality and morbidity rates than does open surgery. However, these repairs are reserved for high-risk patients, so it is difficult to compare the results of these procedures with the results of traditional open operations. Although short-term morbidity appears to be reduced in hybrid repairs, it is not clear that early death is reduced. In addition to the uncertain long-term functionality and durability of endovascular devices,18–22 the substantial risk of stroke due to wire and device manipulation within the aortic arch is a drawback of hybrid approaches.
The process of debranching the aortic arch and rerouting the brachiocephalic circulation enables great flexibility. In general, however, the complexity of repair increases as more vessels are incorporated into the repair and as the repair moves proximally to incorporate the brachiocephalic trunk. To limit the number of rerouted vessels, many centers selectively occlude the left subclavian artery, but this carries some risk of ischemic complications.23 Recently, highly specialized arch-debranching grafts have been developed specifically for use in hybrid repairs. These grafts have an extra branch that serves as a conduit for antegrade stent-graft deployment in single-stage hybrid repair.19 In theory, using antegrade deployment reduces the risk of embolization and stroke. As an additional option, the surgeon may transpose the native left subclavian and left common carotid arteries onto the brachiocephalic trunk to lengthen the proximal landing zone for subsequent endovascular repair.24 The endovascular stage of repair can be performed either simultaneously or later, and either antegrade or retrograde. Among the newly evolving hybrid approaches is the “frozen elephant trunk” procedure, in which a hybrid device containing a Dacron graft attached to a stent-graft is deployed in an antegrade fashion under direct vision: the stent-graft covers the distal portion of the repair, and the proximal graft portion replaces the arch.25,26
Predictions for Future Aortic Arch Repair
The future of aortic arch repair will no doubt encompass the latest developments in both open and endovascular repair. In most centers, purely endovascular repair will remain a highly selective, infrequently used approach. However, hybrid repairs will continue to combine the most innovative aspects of open and endovascular repair. We foresee the trifurcated graft approach as the dominant mode of open arch repair, yet there will remain a need for continuing innovation in cerebral-protection techniques. The development of new custom and commercial debranching grafts, with and without conduit channels, will be a valuable advance. Current guidelines reserve hybrid repair for patients who are unable to withstand open repair, but if hybrid results improve, one would expect these procedures to be extended to low-risk patients as a direct alternative to open arch repair. Moreover, in part because our aging population is prone to atherosclerosis, we envision that greater numbers of arch repairs will be performed on high-risk elderly patients, with better results than previously could have been imagined.
Acknowledgments
The authors thank Scott A. Weldon, MA, CMI, for creating the medical illustration, and Stephen N. Palmer, PhD, ELS, for invaluable editorial support.
Footnotes
Address for reprints: Joseph S. Coselli, MD, Division of Cardiothoracic Surgery, Michael E. DeBakey Department of Surgery, Baylor College of Medicine, MS: BCM 390, 1 Baylor Plaza, Houston, TX 77030 E-mail: jcoselli@bcm.edu
Presented at the 16th International Symposium of the Denton A. Cooley Cardiovascular Surgical Society, Galveston, Texas, 4–7 June 2009.
References
- 1.Schafer PW, Hardin CA. The use of temporary polythene shunts to permit occlusion, resection, and frozen homologous graft replacement of vital vessel segments; a laboratory and clinical study. Surgery 1952;31(2):186–99. [PubMed]
- 2.Cooley DA, Mahaffey DE, De Bakey ME. Total excision of the aortic arch for aneurysm. Surg Gynecol Obstet 1955;101 (6):667–72. [PubMed]
- 3.De Bakey ME, Crawford ES, Cooley DA, Morris GC Jr. Successful resection of fusiform aneurysm of aortic arch with replacement by homograft. Surg Gynecol Obstet 1957;105(6): 657–64. [PubMed]
- 4.Bloodwell RD, Hallman GL, Cooley DA. Total replacement of the aortic arch and the “subclavian steal” phenomenon. Ann Thorac Surg 1968;5(3):236–45. [DOI] [PubMed]
- 5.Griepp RB, Stinson EB, Hollingsworth JF, Buehler D. Prosthetic replacement of the aortic arch. J Thorac Cardiovasc Surg 1975;70(6):1051–63. [PubMed]
- 6.Frist WH, Baldwin JC, Starnes VA, Stinson EB, Oyer PE, Miller DC, et al. A reconsideration of cerebral perfusion in aortic arch replacement. Ann Thorac Surg 1986;42(3):273–81. [DOI] [PubMed]
- 7.Svensson LG, Crawford ES, Hess KR, Coselli JS, Raskin S, Shenaq SA, Safi HJ. Deep hypothermia with circulatory arrest. Determinants of stroke and early mortality in 656 patients. J Thorac Cardiovasc Surg 1993;106(1):19–31. [PubMed]
- 8.Higami T, Kozawa S, Asada T, Obo H, Gan K, Iwahashi K, Nohara H. Retrograde cerebral perfusion versus selective cerebral perfusion as evaluated by cerebral oxygen saturation during aortic arch reconstruction. Ann Thorac Surg 1999;67 (4):1091–6. [DOI] [PubMed]
- 9.Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg 1995;59(5):1289–95. [DOI] [PubMed]
- 10.Sundt TM 3rd, Orszulak TA, Cook DJ, Schaff HV. Improving results of open arch replacement. Ann Thorac Surg 2008; 86(3):787–96. [DOI] [PubMed]
- 11.Coselli JS, LeMaire SA. Aortic arch surgery: principles, strategies, and outcomes. Chichester, UK: Wiley-Blackwell; 2008.
- 12.Kazui T, Bashar AH. Aortic arch replacement using a trifurcated graft. Ann Thorac Surg 2006;81(4):1552. [DOI] [PubMed]
- 13.Spielvogel D, Etz CD, Silovitz D, Lansman SL, Griepp RB. Aortic arch replacement with a trifurcated graft. Ann Thorac Surg 2007;83(2):S791-5; discussion S824–31. [DOI] [PubMed]
- 14.Baldwin ZK, Chuter TA, Hiramoto JS, Reilly LM, Schneider DB. Double-barrel technique for preservation of aortic arch branches during thoracic endovascular aortic repair. Ann Vasc Surg 2008;22(6):703–9. [DOI] [PubMed]
- 15.Chuter TA, Schneider DB. Endovascular repair of the aortic arch. Perspect Vasc Surg Endovasc Ther 2007;19(2):188–92. [DOI] [PubMed]
- 16.Criado FJ. Commentary: conquering zone zero: expanding endograft repair in the aortic arch. J Endovasc Ther 2008;15 (2):166–7. [DOI] [PubMed]
- 17.Moon MC, Morales JP, Greenberg RK. The aortic arch and ascending aorta: are they within the endovascular realm? [published erratum appears in Semin Vasc Surg 2007;20(3):195] Semin Vasc Surg 2007;20(2):97–107. [DOI] [PubMed]
- 18.Bozinovski J, LeMaire SA, Weldon SA, Coselli JS. Hybrid repairs of the distal aortic arch and proximal descending thoracic aorta. Op Tech Thorac Cardiovasc Surg 2007;12(3):167–77.
- 19.Diethrich EB, Ghazoul M, Wheatley GH 3rd, Alpern JB, Rodriguez-Lopez JA, Ramaiah VG. Great vessel transposition for antegrade delivery of the TAG endoprosthesis in the proximal aortic arch. J Endovasc Ther 2005;12(5):583–7. [DOI] [PubMed]
- 20.Hughes GC, Nienaber JJ, Bush EL, Daneshmand MA, McCann RL. Use of custom Dacron branch grafts for “hybrid” aortic debranching during endovascular repair of thoracic and thoracoabdominal aortic aneurysms. J Thorac Cardiovasc Surg 2008;136(1):21–8, 28.e1–6. [DOI] [PubMed]
- 21.Kpodonu J, Diethrich EB. Hybrid interventions for the treatment of the complex aortic arch. Perspect Vasc Surg Endovasc Ther 2007;19(2):174–84. [DOI] [PubMed]
- 22.Riesenman PJ, Tamaddon HS, Farber MA. Surgical bypass procedures to facilitate endovascular repair of aortic arch pathology. J Cardiovasc Surg (Torino) 2008;49(4):461–9. [PubMed]
- 23.Reece TB, Gazoni LM, Cherry KJ, Peeler BB, Dake M, Matsumoto AH, et al. Reevaluating the need for left subclavian artery revascularization with thoracic endovascular aortic repair. Ann Thorac Surg 2007;84(4):1201–5. [DOI] [PubMed]
- 24.Czerny M, Grabenwoger M. Alternative approaches: endovascular stent-grafts. In: Coselli JS, LeMaire SA, editors. Aortic arch surgery: principles, strategies, and outcomes. Chichester, UK: Wiley-Blackwell; 2008. p. 235–40.
- 25.Gorlitzer M, Weiss G, Thalmann M, Mertikian G, Wislocki W, Meinhart J, et al. Combined surgical and endovascular repair of complex aortic pathologies with a new hybrid prosthesis. Ann Thorac Surg 2007;84(6):1971–6. [DOI] [PubMed]
- 26.Karck M, Kamiya H. Progress of the treatment for extended aortic aneurysms; is the frozen elephant trunk technique the next standard in the treatment of complex aortic disease including the arch? Eur J Cardiothorac Surg 2008;33(6):1007–13. [DOI] [PubMed]