A 40-year-old Hispanic man without conventional risk factors for coronary artery disease presented with an inferior ST-elevation myocardial infarction and underwent emergent intervention with a drug-eluting stent deployed to his occluded mid right coronary artery (RCA). Four months later, he returned with a large, painful, right femoral artery pseudoaneurysm (Fig. 1) at the site of the collagen-plug vascular closure device that had been used during this cardiac catheterization; the pseudoaneurysm required surgical intervention. During this hospitalization, the patient was noted to have low-grade fevers and oral ulcers, which he had also experienced intermittently in the past. An extensive infectious-disease and rheumatologic evaluation revealed only an elevated erythrocyte sedimentation rate and C-reactive protein level. The possibility of Behçet syndrome was considered but was deemed unlikely, due to the patient's non-European descent and the lack of genital and ocular involvement. A presumptive diagnosis of atypical recurrent aphthous stomatitis was made based on the absence of lymphadenopathy.
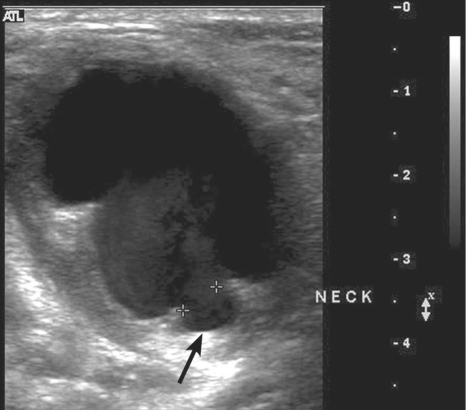
Fig. 1 Ultrasonographic image of the right femoral artery shows a large pseudoaneurysm (arrow).
+ symbols denote the neck of the pseudoaneurysm.
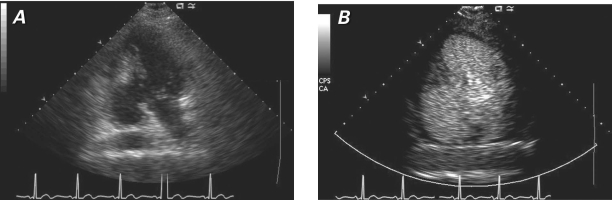
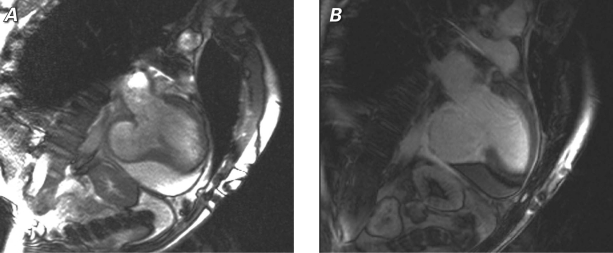
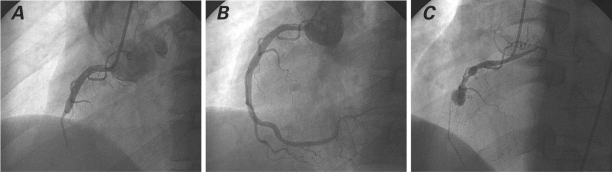
One month later (5 months after his initial myocardial infarction), the patient presented again—this time with atypical chest pain. Echocardiography showed a large inferobasilar ventricular pseudoaneurysm (Fig. 2). Chest radiography showed nonspecific cardiomegaly. Cardiac magnetic resonance imaging, performed in preparation for surgical pseudoaneurysmectomy, further delineated the inferobasilar ventricular pseudoaneurysm in the setting of prior inferior-wall myocardial infarction (Fig. 3). Coronary angiography revealed a large RCA pseudoaneurysm and thrombotic occlusion of the RCA stent (Fig. 4). The patient underwent successful surgical repair of the ventricular pseudoaneurysm, with resection and ligation of the RCA pseudoaneurysm. Histopathologic analysis of the RCA pseudoaneurysm suggested Behçet syndrome (Fig. 5). More than a year later, he was doing well on methotrexate and infliximab therapy for Behçet syndrome.
Fig. 2 Two-chamber echocardiographic views show the large inferobasilar pseudoaneurysm with a narrow neck pathognomonic for a pseudoaneurysm: A) without contrast, and B) contrast-enhanced.
Fig. 3 Corresponding cardiac magnetic resonance imaging 2-chamber views show the inferobasilar ventricular pseudoaneurysm and a moderate anterior pericardial effusion: A) cine image, and B) delayed-enhancement image after gadolinium infusion, which shows the transmural myocardial infarction and scar surrounding the pseudoaneurysm.
Fig. 4 Coronary angiograms of the right coronary artery A) at the time of acute inferior ST-elevation myocardial infarction, B) immediately after percutaneous intervention with a drug-eluting stent, and C) before surgical repair of the ventricular pseudoaneurysm, showing a coronary pseudoaneurysm at the site of the previously placed drug-eluting stent with total stent occlusion.
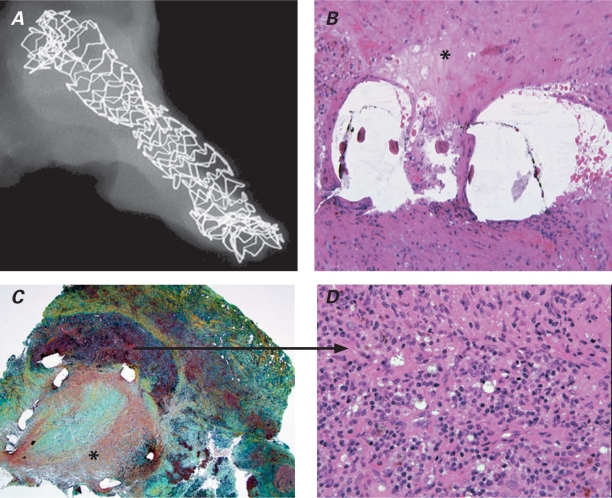
Fig. 5 A) Scanning electron microscopic view of the right coronary artery (RCA) stent. B) Hematoxylin & eosin stain (orig. ×40) of RCA pseudoaneurysm, in which the asterisk (*) shows stent struts with overlying thrombus. C) Photomicrograph (H & E, orig. ×10) of the RCA pseudoaneurysm, in which the asterisk (*) denotes organizing luminal thrombus, and D) the arrow demonstrates a magnified view (H & E, orig. ×60) of the arterial media with chronic inflammation. Findings are consistent with Behçet syndrome.
Comment
Behçet syndrome is a multisystem vasculitis that affects all sizes of arteries and veins. This systemic, inflammatory disorder is chronic and relapsing, and is characterized by aphthous stomatitis, genital ulcers, and ocular lesions. There are no laboratory results that are pathognomonic for Behçet syndrome; consequently, the diagnosis is made on the basis of the clinical findings. The prevalence of coronary involvement in Behçet syndrome is 0.5%.1,2 The pathologic findings include arteritis and inflammatory obliterative endarteritis of the vasa vasorum with fibrotic deterioration of the media, all of which predispose the arterial wall to aneurysm formation.3,4
Acknowledgments
The histopathology slides were prepared and analyzed by Renu Virmani, MD, and Elena Ladich, MD, of CV Path, Gaithersburg, Maryland.
Footnotes
Address for reprints: Alex Harrison, MD, 1510 E. Main St., Ste. 101, Santa Maria, CA 93454 E-mail: alexharrisonmd@hotmail.com
Dr. Harrison is now at Marian Medical Center, Santa Maria, California. Dr. Ahsan is at the Nevada Heart & Vascular Center, Las Vegas, Nevada.
References
- 1.Lie JT. Cardiac and pulmonary manifestations of Behcet syndrome. Pathol Res Pract 1988;183(3):347–55. [DOI] [PubMed]
- 2.Le Thi Huong D, Wechsler B, Papo T, Piette JC, Bletry O, Vitoux JM, et al. Arterial lesions in Behcet's disease. A study in 25 patients. J Rheumatol 1995;22(11):2103–13. [PubMed]
- 3.Matsumoto T, Uekusa T, Fukuda Y. Vasculo-Behcet's disease: a pathologic study of eight cases. Hum Pathol 1991;22(1):45–51. [DOI] [PubMed]
- 4.Ozeren M, Dogan OV, Dogan S, Yucel E. True and pseudo aneurysms of coronary arteries in a patient with Behcet's disease. Eur J Cardiothorac Surg 2004;25(3):465–7. [DOI] [PubMed]