Abstract
Objectives
Surveys on stroke prevalence may provide valuable information for planning of healthcare services. Few such studies have been conducted in Latinos and none have been performed in Los Angeles, a County that contains the largest population of Latinos in the United States. We sought to assess the prevalence of self-reported stroke in a population-based sample of community-dwelling Latinos in Los Angeles.
Patients and methods
The group comprised of self-identified Latinos aged 40 years and older from six census tracts in Los Angeles participating in a population-based cross-sectional study of ocular disease in Latinos, The Los Angeles Latino Eye Study (LALES). The prevalence of stroke and its association with demographic, biological and behavioral risk factors was determined. Univariate and multiple stepwise logistic regression models were used to calculate odds ratios (ORs).
Results
The prevalence of self-reported stroke in 6954 community-dwelling Latinos in Los Angeles was 3.3%. Stroke prevalence increased with age (1.4% age 40–50, 3.3% age 50–65, 7.1% age >65), history of hypertension (OR 2.6, p < 0.001), heart disease (OR 4.8, p < 0.001) and diabetic retinopathy (OR 2.1, p = 0.01).
Conclusions
Renewed efforts directed at early identification and treatment of hypertension and heart disease within the Latino community will mitigate the burden of stroke.
Keywords: Stroke, Latino, Prevalence
1. Introduction
Minority and ethnic groups are known to have higher rates of stroke and more severe strokes [1]. In addition, there are recognized regional ethnic variations in treatment and outcomes for cerebrovascular disease [2]. Few studies of stroke prevalence have been conducted in Latinos and none have been performed in Los Angeles County, which contains the largest population of Latinos in the United States.
We conducted a cross-sectional survey of stroke prevalence in community-dwelling Latinos, defined as individuals who are born into or have descended from a Spanish-speaking community regardless of race. Determination of the prevalence of cerebrovascular disease in Latinos in Los Angeles will allow for comparisons with studies performed in other communities and over time. As the fastest growing segment of the US population, understanding the prevalence and risk factors of cerebrovascular disease in this community can provide valuable information for planning of healthcare services.
2. Subjects and methods
The Los Angeles Latino Eye Study (LALES) is a population-based cross-sectional study of ocular disease in Latinos conducted between February 2000 and May 2003. All self-identified Latinos aged 40 years and older from six census tracts in the Los Angeles community of La Puente were invited to undergo a detailed interview and a physical examination [3]. La Puente was selected because it was primarily residential, with a large proportion (83%) of Latinos, a high level of local support from the community, and in close to the University of Southern California Medical Center. The demographic and socioeconomic characteristics of Latinos in the six census tracts of La Puente were similar to those of the Latino populations in Los Angeles County.
Residence was determined by the US Census definition as any-one who considers it his or her permanent residence, lives and sleeps at the residence most of the time, or lives in the household at least 6 months out of the year. Eligibility criteria were based on self-identification as Latino or of Latino heritage, age 40 years or older on the day of the household screening, and residency in one of the selected La Puente census tracts.
All data collected by the staff, including the screening and the home interview, were collected via computer-assisted in-person interviews in the preferred language (English or Spanish) of each individual. After informed consent was obtained, an in-home interview was conducted, in the participant’s native language. The standardized interview included an assessment of the history of stroke or brain hemorrhage and related demographic (age, gender), biological (history of hypertension, heart disease), and behavioral (smoking/alcohol use) risk factors.
The prevalence of stroke and its association with demographic, biological, and behavioral risk factors was determined. Univariate and multiple stepwise logistic regression models were used to calculate odds ratios (ORs).
3. Results
Of the 10,663 individuals screened, 7789 were eligible for LALES and 6954 participated in the in-home personal interview and answered the question of whether or not they had experienced a stroke or brain hemorrhage. Of survey respondants 58% were female, the average age was 54.9 years (S.D. ± 10.8), 24% were born in the US, and 94.7% were of Mexican origin. The overall prevalence of self-reported stroke was 3.3%. Stroke prevalence increased with age (1.4% age 40–50, 3.3% age 50–65, 7.1% age >65). Those who participated in the in-home interview were, on average, 2 years younger (54.9±11 years) and more likely to be women (58%) when compared with those who did not participate (n = 835; 56.8±11 years, female 47%; p < 0.0001).
On univariate analysis five factors were associated with a history of stroke (Table 1). These factors were age, a history of hypertension, diabetes, heart disease and the presence of diabetic retinopathy. After multiple stepwise regression analysis (Table 2) the risk factors (OR, 95% CI) that were independently associated with self-reported stroke were age OR= 1.04 (1.02–1.05), history of hypertension OR= 2.6 (1.9–3.5), history of heart disease OR= 4.8 (3.3–7.0), and diabetic retinopathy OR = 2.1 (1.2–3.5).
Table 1.
Baseline sociodemographic characteristics
| Characteristic | History of stroke (n = 227) | No history of stroke (n = 6727) | All subjects (n = 6954) | p-Value |
|---|---|---|---|---|
| Age (years), mean (S.D.) | 62.7 (12) | 54.7 (11) | 54.9(11) | <0.0001 |
| Hypertension | 68% (155) | 29% (1946) | 30%(2101) | <0.0001 |
| Diabetes | 40% (91) | 16% (1090) | 17% (1181) | <0.0001 |
| Heart disease | 23% (52) | 3% (184) | 3% (236) | <0.0001 |
| Smokinga | 43% (96) | 39% (2589) | 39% (2685) | 0.24 |
| Any alcohol | 61% (137) | 60% (4053) | 60% (4190) | 0.95 |
| Diabetic retinopathy | 10% (22) | 2% (140) | 2% (162) | <0.0001 |
Smoking defined as current or ex-smoker.
Table 2.
Multivariate stepwise logistic regression models of historical demographic factors and stroke
| Odds ratio | 95% confidence interval | |
|---|---|---|
| Age (per year) | 1.036 | 1.023–1.049 |
| Hypertention | 2.6 | 1.9–3.5 |
| Heart disease | 4.8 | 3.3–7.0 |
| Diabetic retinopathy | 2.1 | 1.2–3.5 |
4. Discussion
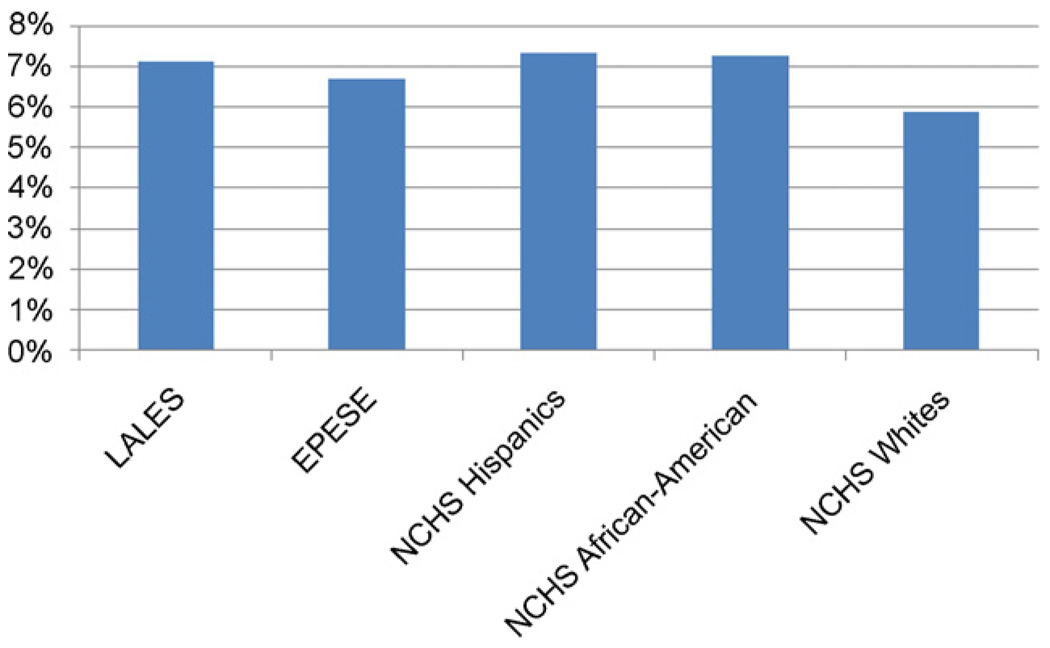
Our reported prevalence of stroke in community-dwelling Latinos in Los Angels is consistent with prior studies in other Hispanic populations (Fig. 1), confirming a high overall prevalence of stroke in this community relative to non-Hispanic whites.
Fig 1.
Comparison of prevalence studies for cerebrovascular disease among individuals aged ≥65 years old demonstrates a consistent and higher prevalence in Hispanics/Latinos in comparison to non-Hispanic whites. LALES: Los Angeles Latino Aging Study, 2000–2003; MHAS:Mexican Health and Aging Study, 2001; EPESE: Hispanic Established Population for the Epidemiologic Study of the Elderly, 1993–1994; NCHS: National Center for Health Statistics 1986–1988.
There have been large surveys of stroke prevalence in Hispanic population both within and outside of the United States. Baseline data from the 2001 Mexican Health and Aging Study (MHAS) provided data on a nationally representative probability sample of 15,186 Mexican adults aged 50 years and older living in Mexico. The 1993/1994 Hispanic Established Population for the Epidemiologic Study of the Elderly (HEPESE) is also a probability sample of 3050 Mexican Americans aged 65 years and older living in the southwestern region of the United States. Data in both studies were collected through in-home interviews with subjects or proxy-informants and provide comparable survey data for parallel analyses. MHAS reported an overall stroke prevalence of 4.4% in 4811Mexicans aged ≥50 years; the prevalence of stroke in LALES participants of this age group was 4.5% [4]. HEPESE found a stroke prevalence of 6.7% in a population aged ≥65 years, compared to a prevalence of 7.1% in a similar age group for LALES [4].
The National Center for Health Statistics reported the prevalence of self-reported stroke in a community-dwelling population aged ≥65 in their 1986–1988 survey. Stroke prevalence was found to be roughly equal among Hispanics and African-Americans (7.34% and 7.26%) and significantly higher than the prevalence in non-Hispanic whites (5.87%) [5]. This finding of excess stroke in Hispanics compared to non-Hispanic whites has been well documented in ongoing population-based studies such as the Brain Attack Surveillance in Corpus Christi (BASIC) project [1]. BASIC found that the Mexican Americans experience a substantially greater ischemic stroke and intracerebral hemorrhage incidence compared with non-Hispanic whites.
The increase in stroke among Latinos is not limited to Mexican–Americans [6]. A population-based stroke incidence study in northern Manhattan, New York City (NOMASS) found an annual age-adjusted stroke incidence rates per 100,000 people of 223 for blacks, 196 for Hispanics, and 93 for whites. The countries of origin for Hispanic participants in NOMASS are predominantly Caribbean (Puerto Rio and the Dominican Republic).
Limitations of this study include the reliance of self-report of stroke, which has the potential to underestimate prevalence in a given population. Studies evaluating self-report of stroke have found a sensitivity of 86%, a specificity of 100% in veterans [7], and a sensitivity of 80% and specificity of 99% in community-dwelling Norwegians [8]. Self-report of stroke does seem sufficiently accurate for use in preliminary epidemiological studies and health services research of cerebrovascular disease.
Latinos are the largest US minority group and the fastest growing segment; it is estimated that Latinos will make up 24.3% of the US population by the year 2050. Stroke prevalence rates are high in Latinos, regardless of the population studied. Hypertension, heart disease and poorly controlled diabetes are important conditions associated with stroke in Latino populations. Since Latinos are the fastest growing segment of the US population, renewed efforts directed at early identification and treatment of hypertension and heart disease within this community could mitigate the projected increase in the societal burden of stroke.
Acknowledgements
This work was supported by grants EY 11753 and EY 03040 from the National Eye Institute and National Center for Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD and an unrestricted grant from Research to Prevent Blindness, New York, NY.
Dr. Sanossian takes full responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Morgenstern LB, Smith MA, Lisabeth LD, Risser JMH, Uchino K, Garcia N, et al. Excess stroke in Mexican Americans compared with non-Hispanic whites: the brain attack surveillance in corpus Christi project. Am J Epidemiol. 2004;160:376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 3.Varma R, Paz SH, Azen SP, Globe D, Torres M, Shufelt C, et al. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–1131. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Patel KV, Peek MK, Wong R, Markides KS. Comorbidity and disability in elderly Mexican and Mexican American adults: findings from Mexico and the Southwestern United States. J Aging Health. 2006;18:315–329. doi: 10.1177/0898264305285653. [DOI] [PubMed] [Google Scholar]
- 5.Collins JG National Center for Health Statistics. Prevalence of selected chronic conditions, United States 1986–88. Vital Health Stat. 1992;10:182. [PubMed] [Google Scholar]
- 6.Northern Manhattan Stroke Study C, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: The Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 7.Horner RD, Cohen HJ, Blazer DG. Accuracy of self-reported stroke among elderly veterans. Aging Ment Health. 2001;5:275–281. doi: 10.1080/13607860120065041. [DOI] [PubMed] [Google Scholar]
- 8.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: The Tromso Study. Stroke. 2000;31:1602–1607. doi: 10.1161/01.str.31.7.1602. [DOI] [PubMed] [Google Scholar]