Abstract
Despite some evidence showing that readiness to change substance use predicts reductions in substance use among treated adolescents, there is little research on month-to-month changes in adolescents’ thoughts about abstinence and marijuana use during and after substance use treatment. The current study provides a test of the “snares” hypothesis, which posits that time-varying changes in adolescents’ motivation to abstain and perceived difficulty to abstain from marijuana use hinder, or snare, the return of regular marijuana use during and after treatment. Monthly data on thoughts about abstinence, marijuana use, and treatment utilization were collected over 6-month follow-up from 142 adolescents recruited from intensive outpatient treatment for substance use. Results provided some support for the snares hypothesis in that higher motivation to abstain (but not perceived difficulty) predicted fewer days of marijuana use, over and above both the adolescent’s average trajectory of marijuana use, the initial severity of their marijuana involvement, and the effects of treatment utilization. Moreover, this association was bi-directional, such that past-month marijuana use influenced both motivation to abstain and perceived difficulty to abstain. Study findings highlight the importance of abstinence-related cognitions as a key target of intervention during and after addictions treatment, and underscore the importance of considering recovery from substance use disorders as a dynamic process of change over time.
Keywords: adolescent, treatment outcome, substance use, motivation to abstain
Among the factors influencing treated adolescents’ substance use outcomes, motivational constructs, such as readiness to change substance use and motivation to abstain, have gained increasing attention as key cognitive factors that may precede and predict change in substance use behavior. The greater focus on motivational constructs as predictors of change in substance use behavior aligns with a revised cognitive-behavioral model of relapse (Witkiewitz & Marlatt, 2004), which proposes that motivation for abstinence and self-efficacy to abstain from substance use applied to high risk situations reduce the likelihood of relapse. In addition, motivational enhancement interventions that have been developed for use with youth have demonstrated some effectiveness in reducing adolescent substance involvement (e.g., Becker & Curry, 2008; Dennis et al., 2004). However, little is known about how treated adolescents’ motivation to abstain, and perceived difficulty to abstain from substance use, changes during treatment and over short-term follow-up, specifically in relation to substance use behavior.
Adolescent treatment outcome studies show that marijuana use generally declines over short-term follow-up among treated adolescents, but that use may increase for some youth over longer-term follow-up, with as many as two-thirds returning to regular marijuana use within the next three to six months after treatment (Dennis et al., 2004; Waldron, Slesnick, Brody, Turner, & Peterson, 2001). The return to substance use for some adolescents over longer-term follow-up suggests the potential value of “booster sessions” to maintain treatment gains for certain adolescents as part of a program of continuing care. However, few studies have collected data to inform the optimal timing and content of posttreatment booster sessions provided to adolescent substance users.
One content area that could be addressed in a brief booster session format involves motivational enhancement to reduce substance use. Previous research has shown that greater readiness to change substance use assessed at the start of treatment predicted less substance use at follow-up. For example, subscales from the Stages of Change Readiness and Treatment Eagerness Scale (Miller & Tonigan, 1996) have been found to predict level of alcohol use at 1-year follow-up in treated youth (Maisto, Chung, Cornelius, & Martin, 2003). In another study, Marijuana Contemplation Ladder scores at the start of incarceration (which included substance abuse services) predicted the severity of adolescents’ marijuana use three months after discharge (Slavet et al., 2006). Although these studies indicate that readiness to change predicts marijuana use over follow-up, the extent to which adolescents’ thoughts about abstinence change over time, as well as the roles that these cognitive factors play in delaying or dampening a return to more regular marijuana use has received little attention, despite the implications of understanding the processes of relapse and recovery for improving treatment outcomes.
Recent research in developmental psychopathology has provided a conceptual framework to test hypotheses regarding factors, such as thoughts about abstinence, which may have time-specific impacts on an individual’s trajectory of marijuana use. Specifically developed to explain how substance use hinders the desistence of antisocial behaviors across late adolescence, the “snares model” proposes that certain factors (i.e., “snares”) interfere with changes in problematic behaviors (Hussong, Curran, Moffitt & Carrig, 2004). Applied to the process of recovery, factors such as thoughts about abstinence (i.e., motivation to abstain, perceived difficulty of abstaining) and continuing involvement in treatment are proposed to retard, or snare, increases in adolescents’ marijuana use following the initiation of treatment. In other words, these factors exert a continuing, time-specific influence on marijuana use during and after treatment, and can help to explain deflections from an increasing trajectory of marijuana use during and after treatment. The current study tests whether the time-varying effects of motivation to abstain and perceived difficulty of abstaining snare, or hinder, the return of regular marijuana use in treated youth, reducing the frequency of marijuana use over and above the adolescent’s average trajectory of marijuana use during and after outpatient treatment for substance use.
Few adolescent substance use treatment outcome studies have collected repeated measures data on cognitive variables (e.g., motivation to abstain) in relation to substance use that can be used to test the snares hypothesis. In the relatively limited literature that exists on treated adolescents’ motivation to change substance use behavior, small increases, on average, have been reported from baseline (i.e., during treatment or incarceration) to post-treatment follow-up (e.g., 3-month follow-up) for variables representing readiness to change substance use and ratings of the importance of abstinence (e.g., Kelly, Meyers & Brown, 2000; Slavet et al., 2006). In addition, although self-efficacy or confidence to abstain did not change, on average, during or 9-months after treatment in one study of adolescents, greater self-efficacy to abstain did predict lower levels of substance involvement over post-treatment follow-up (Burleson & Kaminer, 2005). To date, month-to-month data on how adolescents’ motivation to abstain and perceived difficulty to abstain from substance use changes during and after treatment have not been reported, although such data can usefully inform the extent to which treatment impacts these cognitive variables.
This is one of the first studies to prospectively examine, in a sample of treated adolescents, month-to-month changes in cognitive factors related to marijuana use, such as motivation to abstain and perceived difficulty of abstaining, which may predict level of marijuana use during and after intensive outpatient treatment. Consistent with national statistics that marijuana is the most commonly reported primary drug among adolescents in publicly funded treatment in the United States (SAMHSA, 2007), this study focuses on changes in treated adolescents’ marijuana use. We also consider how treatment utilization (i.e., attendance at outpatient and 12-step meetings) and residential placement (i.e. inpatient or residential treatment or incarceration) impacts adolescents’ readiness to change marijuana use, since some residential placements (e.g., incarceration) restrict an adolescent’s opportunity to engage in substance use, and treatment in general may impact readiness to change (McCaffrey, Morral, Ridgeway & Griffin, 2007). We hypothesize that, according to the snares model, monthly changes in level of motivation to abstain and perceived difficulty to abstain will produce deflections from a treated adolescent’s trajectory of marijuana use over 6-month follow-up. We also predict that there will be a bi-directional association between motivation to abstain and level of marijuana use over 6-month follow-up, as well as a bi-directional association between difficulty to abstain and level of marijuana use. These bi-directional associations are hypothesized based on the idea that readiness to change and marijuana use will reciprocally influence one another over time (e.g., a “relapse” may erode motivation to abstain, and lower motivation to abstain will in turn predict marijuana use). Study findings have implications for understanding dynamic associations between readiness to change and level of marijuana use that can inform the optimal timing and content of booster sessions to maintain and enhance treatment gains.
Methods
Participants
142 adolescent substance users (ages 14-18) were recruited immediately prior to attending their first Intensive Outpatient (IOP) treatment session to participate in a longitudinal study tracking changes in substance use behavior and related cognitions (e.g., motivation to abstain, perceived difficulty of abstaining) during and after treatment. The majority of participants were male (63.4%), and Caucasian (88.7%). African-American individuals constituted 5.6% of the sample, and 5.7% of the sample represented other ethnic groups (e.g., Asian, multi-racial). Participants were, on average, 16.7 years old (SD = 1.2) at baseline, and represented a wide range of socioeconomic status (SES; range = 1-5, 1=high SES; mean = 2.6, SD = 1.1) (Hollingshead, 1975). Participant demographic characteristics, particularly with regard to gender representation and mean age at treatment entry, were similar to those reported for adolescent admissions to publicly funded treatment (SAMHSA, 2007).
At the baseline assessment, which occurred, on average, 2 weeks after the first IOP session (mean=15.1 days, SD=11.9; range=0 to 65 days; 90% completed baseline within one month of recruitment), a majority of the adolescents had a current (past 6-months) DSM-IV marijuana diagnosis (79.6%; 36.6% abuse, 43.0% dependence), with less than half of the adolescents meeting criteria for a current alcohol diagnosis (46.5%; 37.3% abuse, 9.2% dependence). All adolescents reported lifetime marijuana use. Only five adolescents were diagnosed with a substance use disorder (SUD) that was not related to alcohol or marijuana. These five participants had SUD diagnoses related to cocaine (n=2), an opiate (n=1), cocaine and an opiate (n=1), or polysubstance dependence (n=1), which supports the focus on marijuana use in the analyses1.With regard to the most common forms of current (past 6 months) psychopathology at baseline, 33.1% met DSM-IV criteria for conduct disorder, 31.7% had a diagnosis of attention deficit hyperactivity disorder, and 23.9% met criteria for a depression diagnosis (i.e., major depression or dysthymia). A minority of the sample (16%) reported receiving inpatient or residential treatment for substance use or being incarcerated in the month prior to the baseline interview.
Study recruitment and assessment procedures
Adolescents were recruited from six addictions treatment sites in Western Pennsylvania offering IOP treatment for adolescent substance users. All treatment sites adhered to an outcome goal of abstinence from alcohol and other non-prescribed drugs, with program content that included the development of relapse prevention skills and the facilitation of 12-step meeting attendance. Treatment protocols varied across sites, but typically included group, family and individual therapy components. The core of IOP treatment at each site involved group sessions three times per week, with each session lasting three hours. Recommended duration of IOP treatment across sites was 6-8 weeks. Adolescents were recruited prior to attending the first IOP session by research staff. Written informed consent for the adolescent’s study participation was obtained from the minor adolescent’s parent (with the minor adolescent providing assent for study participation), or from the 18-year old adolescent, prior to data collection. Among adolescents approached for study participation, 65% provided informed consent for study participation and were scheduled for a baseline assessment; it is not possible to compare demographic characteristics of those who declined study participation to those who provided consent. Among adolescents who provided informed consent for participation at the initial assessment, 89% (n = 142) completed the baseline assessment, with no differences by gender or age (ethnicity was not obtained at the initial assessment) between those who did versus did not complete the baseline assessment.
Immediately prior to attending the first IOP session, adolescent participants completed an “initial” assessment (lasting about 20 minutes) that included measures of motivation to abstain and perceived difficulty to abstain from marijuana in the next month. The baseline assessment was scheduled to be completed shortly after attendance at the first IOP session (e.g., typically within 2 weeks). At the baseline assessment, which lasted roughly 2-3 hours, the adolescent reported on their lifetime history of substance use and substance-related problems, co-occurring psychopathology, and thoughts about abstinence (e.g., motivation to abstain, perceived difficulty to abstain). Five monthly phone follow-ups, each lasting about 15 minutes, were timed to begin after completion of the baseline assessment and collected information since the last assessment on the adolescent’s daily substance use, treatment utilization (e.g., outpatient and 12-step meeting attendance), residential placement (i.e. whether or not the adolescent was in inpatient or residential substance use treatment or was incarcerated) and thoughts about abstinence in relation to marijuana use for the next 30 days. Adolescents also completed a 6-month follow-up interview (lasting about 1.5 hours) that was timed to occur six months after completion of baseline. The 6-month follow-up interview collected updated information on the same domains covered in the baseline assessment. Adolescents received compensation for completed assessments. The university’s Institutional Review Board approved the research protocol.
Measures
Motivation to Abstain and Perceived Difficulty of Abstaining from Marijuana
At each assessment (i.e., initial assessment prior to the first IOP session, baseline, 5 monthly follow-ups, and 6-month follow-up), adolescents responded to items that asked “How motivated are you to abstain from marijuana use in the next 30 days?” and “How difficult will it be for you to abstain from marijuana for the next 30 days?” on a 10-point scale. For the motivation to abstain question, response anchors were “1” = not motivated to abstain, 5= “somewhat motivated,” and “10” = very motivated to abstain in the next 30 days. For the difficulty of abstaining question, response anchors were “1” = very easy to abstain, 5= “somewhat difficult,” and “10” = very difficult to abstain from marijuana in the next 30 days. Single item measures of readiness and motivation to change substance use behavior have demonstrated satisfactory validity in adult samples, and in relation to tobacco use (e.g., Biener & Abrams, 1991; Amodei & Lamb, 2004; Miller & Johnson, 2008).
Time Line Follow-Back (TLFB; Sobell & Sobell, 1995; Sobell, Brown, Leo, Sobell, 1996) interview
At baseline, each monthly phone follow-up, and at 6-month follow-up, the TLFB calendar method was used to collect daily data on marijuana use, as well as treatment utilization and residential placement (at baseline, adolescents reported on the past 30 days). The TLFB data provided summary variables for each monthly follow-up interval on the number of days of marijuana use, treatment attendance (e.g., number of 12-step meetings attended) and residential placement (i.e. whether or not the adolescent was in a setting that restricted their access to marijuana such as inpatient, residential substance use treatment, incarceration). Because most (89%) residential placements were related to substance use,2 and because so few adolescents reported spending time in any of those settings (28.2%; among those who reported residential placement, mean days in any month ranged from 1.10-7.09), detecting unique effects of inpatient or residential treatment or incarceration would have been difficult. Thus, for each month we computed an aggregate “residential placement” variable reflecting the number of days of placement in that particular month. Substance use data collected using the TLFB method with adolescents have good reliability and validity (e.g., Donohue et al., 2007; Waldron et al., 2001; Lewis-Esquerre et al., 2005). Results of urine drug screens at baseline indicated no cases in which the drug screen identified someone as using marijuana who did not report this during the assessment. In one case, at 6-month follow-up, the urine drug screen identified an adolescent who did not report marijuana use over follow-up as positive for marijuana use. We tested whether removing this data point (and the case) impacted the overall findings; results were not substantively different with or without this case in the analyses. Thus we present the results for the full sample.
DSM-IV SUD diagnoses and symptoms
An adapted version of the Structured Clinical Interview for DSM-IV SUDs (SCID; First, Spitzer, Gibbon & Williams, 1997; Martin, Pollock, Bukstein & Lynch, 1995) was used to determine the presence of SUD diagnoses and SUD symptom counts. Adaptations to the SCID addressed developmental considerations in symptom assessment with adolescents, and included, for example, providing examples of youth-relevant symptoms (e.g., school grades dropping due to substance use). The adapted SCID demonstrated moderate to high interrater reliability for symptom ratings and ages of symptom onset and offset, as well as good concurrent validity in adolescents (Martin, Kaczynski, Maisto, Bukstein & Moss, 2000; Chung, Martin, San Pedro & Cornelius, 2004). Internal consistency reliability for total number of DSM-IV marijuana symptoms at baseline was .73.
Co-occurring Psychopathology
Participants completed the adolescent version of the Schedule for Affective Disorders and Schizophrenia (K-SADS, Clark et al., 1997; Kaufman et al., 1997) to assess lifetime and current (past 6 months) occurrence of other DSM-IV Axis I psychopathology (e.g., conduct disorder, major depression) at baseline. The K-SADS demonstrated good interrater reliability in adolescent substance users (Clark et al., 1997).
Analytic Strategy
Descriptive analyses characterizing change in frequency of marijuana use and marijuana-related cognitions over 6-month follow-up were performed using SPSS 13.0. Tests of hypotheses regarding the snares model and bi-directional associations between marijuana use and thoughts about abstinence (i.e., motivation to abstain, perceived difficulty to abstain) were conducted using hierarchical linear modeling with the restricted maximum likelihood estimator (HLM, version 6.06; Raudenbush, Bryk, Cheong & Congdon, 2004). In the HLM framework, growth models are represented as a series of hierarchical regression equations estimated simultaneously across all time points within each individual (Raudenbush & Bryk, 2002).
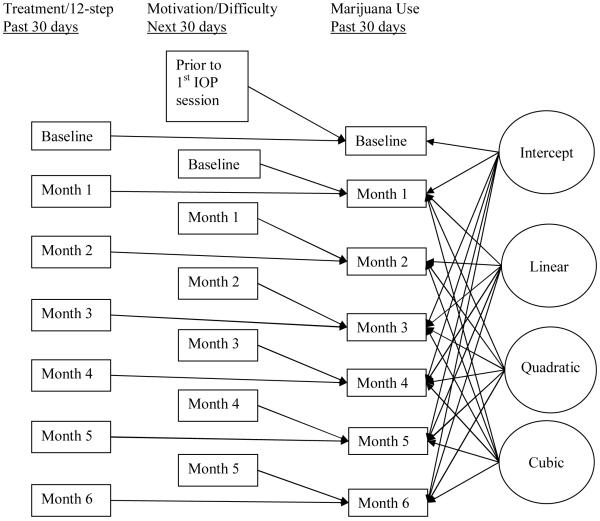
In the first set of HLM analyses, we developed a model of how marijuana use changes as a function of time. To test the snares hypothesis, we then added to this model the monthly measures of motivation to abstain and perceived difficulty of abstaining as time-varying predictors of the past month frequency of marijuana use, controlling for the effects of time, past-month treatment attendance (i.e. the number of days in outpatient or 12-step treatment in the past month) and past month residential placement. We predicted past month marijuana use from motivation and perceived difficulty measured at the previous month, such that the cognition measurements preceded the time period covered by the TLFB of marijuana use. For example, motivation and perceived difficulty measures at Month 1 were used to predict past-month marijuana use at Month 2, controlling for treatment experiences reported at Month 2. Treatment attendance and residential placement variables were included as concurrent predictors of marijuana use (i.e., treatment attendance in the past month, reported at Month 1 was used to predict past-month marijuana use reported at Month 1). These equations (estimated at Level 1 in the HLM framework and detailed below) modeled within-individual variation in marijuana use, and were used to test the snares hypothesis that the level of motivation and perceived difficulty at the beginning of a month would produce deflections in marijuana use in the next month over and above an individual’s rate of change through 6-month follow-up, according to Figure 13. In addition, we controlled for the effects of severity of marijuana involvement (i.e. the number of marijuana symptoms from the SCID) on variation in the intercept at Level 2. However, because the current study focused on the effects of certain time-varying covariates on intra-individual variation, rather than inter-individual differences across marijuana use trajectories, we did not include other fixed predictors of effects at Level 2.4
Figure 1. Hypothesized model of the effects of motivation to abstain and difficulty to abstain on marijuana use controlling for past-month treatment.
The effects of motivation/difficulty reflect their residual influence on marijuana use over and above both variation explained by the level of marijuana use at baseline (intercept) and change over time (linear, quadratic and cubic change) and treatment in the past month.
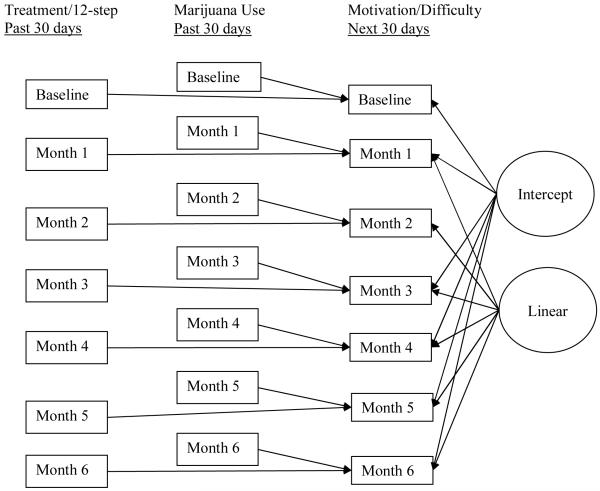
In the second set of HLM analyses, which provided information relevant to determining the extent of possible bi-directional associations between marijuana use and thoughts about abstinence, we first developed separate unconditional models of motivation to abstain and perceived difficulty of abstaining as a function of time over 6-month follow-up. We then tested the time-varying effects of frequency of marijuana use over the past month on motivation to abstain and perceived difficulty of abstaining reported at the beginning of a month (in separate models, see Figure 2 for an example of this analysis), controlling for past-month treatment attendance. These models predicted intra-individual differences in motivation to abstain and difficulty to abstain, explaining how frequency of marijuana use in a given month, controlling for treatment and 12-step attendance, impacted an adolescent’s thoughts about abstinence over and above the adolescent’s average rate of change in these cognitions over follow-up.
Figure 2. Hypothesized model of the effects of past month marijuana use and past-month treatment on motivation to abstain and difficulty to abstain in the next 30 days.
The effects of marijuana use and treatment reflect their residual influence on motivation and difficulty use over and above both variation explained by individual differences in the average level of motivation and difficulty (intercept), and in the case of motivation, linear change over time.
Attrition Analyses
HLM can handle missing data in repeated measures analyses at Level 1 (the observation, which is nested within the individual). Thus, we included all participants who had any data collected at any time point, giving us a potential total of 994 observations nested within 142 individuals. Participant retention was excellent for a high risk clinical sample; 742 observations were retained across all waves of data collection, or 75% of all possible observations5. Moreover, 89% of participants in these analyses contributed 3 or more time points. We tested whether a tendency for missing observations (measured as the number of waves with complete data) was associated with any demographic, substance use, or psychiatric characteristics assessed either at recruitment or baseline. A tendency to have missing observations was uncorrelated with age, SES, frequency of alcohol or marijuana use, number of substance-related problems assessed at baseline, and motivation to abstain or perceived difficulty to abstain at recruitment (all ps >.05). Moreover, diagnosis of marijuana and alcohol use disorders, depression, conduct disorder, ADHD and oppositional defiant disorder were unrelated to the number of missing observations (all ps >.05). Thus, missing data were unrelated to any variables of interest in the current study.
Results
Frequency of marijuana use, thoughts about abstinence, and treatment utilization over follow-up
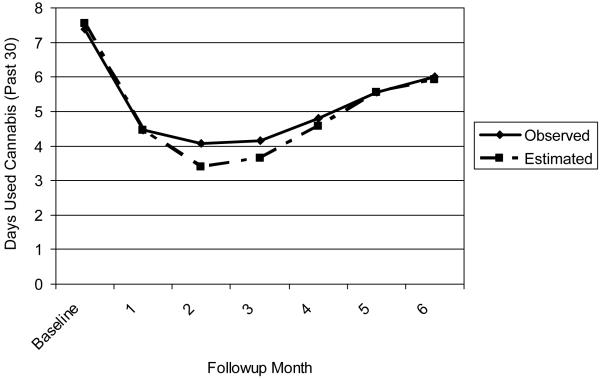
The average number of days of marijuana use declined from baseline (shortly after treatment entry) to follow-up months 3-4, but began to increase in months 5-6 (Table 1 and Figure 3). Over 6-month follow-up, average ratings for motivation to abstain from marijuana in the next month ranged from 6.8 (month 6) to 8.0 (month 1), and average ratings of perceived difficulty of abstaining from marijuana in the next month ranged from 3.8 (month 3) to 4.9 (baseline, i.e., around the start of treatment), with little apparent change in perceived difficulty to abstain, on average, from month to month (Table 1). The average number of outpatient treatment days peaked in month 1 (generally coinciding with participation in the IOP episode which had a recommended duration of 6-8 weeks), and dropped to an average of about 1 day of outpatient treatment per month in months 4-5 (Table 1), with over 50% of participants reporting no outpatient treatment from months 3 to 6, less than 15% reporting more than 3 days of outpatient treatment (approximately 1 week of out patient sessions) in any month from months 3 to 6. The average number of days of 12-step meeting attendance peaked in parallel with the number of days of outpatient treatment attendance, in months 1-2. However, outpatient treatment was only weakly correlated with 12-step attendance across follow-up (ranging from r = .10, p = ns, to r = .22, p < .05). As an indication of the high-risk nature of this treatment sample, 28% reported some residential placement between baseline and month 6 (around 10% with some placement in any month), with a mean of 5 days of placement per month in all follow-up months among those who reported residential placement.
Table 1. Descriptive statistics for marijuana use, thoughts about abstinence, and treatment utilization over 6-month follow-up.
| Days Used Marijuana (Past 30) |
Motivation to Abstain in the next month | Difficulty to Abstain in the next month | Outpatient days (Past 30) |
Placement days (Past 30) |
Participants With Any Placement | 12-Step attendance (Past 30) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | M | SD | % | M | SD | |
| Recruitment | -- | -- | 7.52 | 3.07 | 4.44 | 3.25 | -- | -- | -- | -- | -- | -- | -- |
| Baseline | 7.39 | 10.52 | 7.60 | 2.92 | 4.87 | 3.33 | 5.65 | 3.30 | 1.41 | 4.23 | 14.0 | 1.04 | 2.57 |
| Month 1 | 4.45 | 8.59 | 8.04 | 2.82 | 4.73 | 3.32 | 9.36 | 4.41 | 0.31 | 1.97 | 4.3 | 2.30 | 5.35 |
| Month 2 | 4.07 | 8.05 | 7.89 | 2.89 | 4.46 | 2.99 | 4.40 | 4.18 | 1.25 | 4.65 | 12.6 | 2.67 | 5.96 |
| Month 3 | 4.17 | 8.27 | 7.43 | 3.21 | 3.85 | 2.86 | 1.87 | 2.75 | 1.82 | 6.82 | 11.4 | 1.63 | 3.72 |
| Month 4 | 4.81 | 8.95 | 7.32 | 3.31 | 4.41 | 3.03 | 1.23 | 1.97 | 1.98 | 7.00 | 11.4 | 1.52 | 4.05 |
| Month 5 | 5.55 | 9.54 | 7.56 | 3.25 | 4.36 | 3.11 | 1.48 | 2.89 | 1.69 | 6.80 | 8.3 | 1.30 | 3.96 |
| Month 6 | 6.01 | 9.22 | 6.84 | 3.50 | 4.60 | 3.21 | 1.25 | 2.48 | 1.78 | 6.78 | 9.3 | 1.36 | 4.50 |
Notes: M=Mean, SD=Standard Deviation, Past 30 = Past 30 days, Ns = 117-142
Figure 3. HLM model estimated and observed trajectories of marijuana use over 6-month follow-up.
Correlations between frequency of marijuana use and thoughts about abstinence
Across all time points, the number of days an adolescent reported smoking marijuana in the past month were positively correlated (r = .33-.81, all p < .001), with stronger correlations between adjacent time points relative to non-adjacent time points. Similarly, adolescents’ ratings of motivation to abstain from marijuana use in the next month were positively correlated with one another over follow-up (r = .26-.89, all p < .001), as were ratings of perceived difficulty of abstaining from marijuana use in the next month (r = .32-.72, all p < .001). Motivation to abstain from marijuana use in the next month was negatively associated with the number of days of marijuana use in the past month at all time points (r = -.17 to -.70, all p < .05), and perceived difficulty of abstaining in the next month was positively correlated with frequency of marijuana use in the past month (r = .19-.53, all p < .05). Interestingly, motivation and perceived difficulty’s correlation with past month marijuana use seemed to strengthen over time rather than weaken (r = -.34 & .30 at baseline to r = -.52 and .55, all p < .001, at Month 6 for difficulty and motivation, respectively). Finally, motivation to abstain and perceived difficulty of abstaining were negatively related at each time point, with weaker initial correlations that strengthened over time (r = -.16 to -.53, all p < .05). The correlations indicate associations, in expected directions, between frequency of marijuana use and thoughts regarding abstinence from marijuana, but do not provide information on the direction of influence, if any, between level of marijuana use and thoughts related to abstinence from marijuana.
Longitudinal Modeling of Marijuana Use
Unconditional model of marijuana use
Based on the observed sample means that show an initial decline in marijuana use followed by an increase and a final leveling off, we fitted a growth model with intercept, slope, quadratic and cubic effects, capturing variation in the initial level of use, the linear change over time, the subsequent deceleration and acceleration of use across time, and the flattening of the overall trend, respectively. The unconditional equations were (where L = the linear trend in months, ranging from 0 to 6, Q = the quadratic trend in months, ranging from 0 to 36, and C = the cubic trend in months, ranging from 0 to 216):
Where:
Yti = the outcome (marijuana use) for an individual i at time t
π = the coefficient for the effect of a Level 1 predictor (intercept, linear trend, quadratic trend or cubic trend) on the outcome.
e = the Level 1 error term, reflecting variation in the outcome not explained by the predictors
β = the coefficient for the intercept, or average effect across individuals, of the Level 1 predictor
r = the Level 2 error term, reflecting inter-individual variation in the Level 1 predictor
Likelihood ratio testing indicated that this model provided a significant improvement in model fit over a model without a cubic effect, χ2Δ = 68.48, p< .001. The results of this model indicated that all growth effects had significant (i.e., non-zero) means and variances (Table 2). Specifically, the intercept and quadratic effect were positive, while the linear and cubic slope effects were negative. Figure 3 displays the model implied trajectory of marijuana use compared to the observed means of marijuana use during and after treatment. There was also significant variability in each of the growth parameters, indicating that there were significant inter-individual differences in terms of how adolescents’ marijuana use changed from baseline through 6-month follow-up. Moreover, the ratios of parameter variance to error variance in the growth parameters (also called the reliabilities of the parameters) ranged from high (.89) to moderate (.55), suggesting that modeling these parameters in terms of individual differences is warranted. However, the growth effects were highly collinear, with correlations as high as -.98, suggesting that their relation to the criterion was non-independent. This is an artifact of how HLM handles time (by treating time as data rather than estimated parameters, see Muthen & Curran 1997). It is interpreted to mean that the linear and quadratic growth effects may only be interpreted in the context of the cubic effect. Although the intercorrelation between the linear and quadratic effects may be attenuated by centering the time variable, such centering does not correct the high correlation between the linear and cubic effect.
Table 2. Unconditional Growth Model of Marijuana Use.
| Fixed Effects | π | UCL | LCL | t | df | p value |
|---|---|---|---|---|---|---|
| Intercept | 7.30 | 9.01 | 5.59 | 8.41 | 141 | 0.000 |
| Linear | -3.53 | -1.86 | -5.20 | -4.13 | 141 | 0.000 |
| Quadratic | 1.08 | 1.73 | 0.43 | 3.26 | 141 | 0.002 |
| Cubic | -0.09 | -0.03 | -0.15 | -2.54 | 141 | 0.012 |
| π = the Level 1 coefficient of the fixed effect on the outcome |
| UCL and LCL = 95% upper and lower confidence limits |
| Random Effects | Variance Component | df | χ2 | p value |
|---|---|---|---|---|
| Intercept | 95.00 | 130 | 1081.93 | 0.000 |
| Linear | 69.26 | 130 | 407.96 | 0.000 |
| Quadratic | 9.29 | 130 | 344.97 | 0.000 |
| Cubic | 0.10 | 130 | 312.30 | 0.000 |
| Level 1 error | 13.60 |
| Reliability | Estimate |
|---|---|
| Intercept | 0.89 |
| Linear | 0.65 |
| Quadratic | 0.59 |
| Cubic | 0.55 |
Conditional model of marijuana use: Fixed and random effects
To test the snares hypothesis, Level 1 predictors were added to the unconditional model of frequency of marijuana use over follow-up. In the Level 1 equations, we examined the effects that motivation to abstain, perceived difficulty of abstaining, and number of days of outpatient treatment, residential placement, and 12-step program attendance had on marijuana use, over and above variation explained by the effects of time and initial severity. Because we did not hypothesize individual differences in the effects of these predictors on marijuana use, we treated the Level 1 predictors as fixed effects and did not allow them to randomly vary across individuals6. These Level 1 effects represent how the covariates predict within-individual difference in marijuana use, or how an individual’s marijuana use at any one time point might vary from their individual trajectory of marijuana use over follow-up, effectively ensnaring, or curbing, the return of regular marijuana use. The Level 1 and Level 2 equations for the conditional model of marijuana use are noted, below:
Results of this model generally supported the snares hypothesis. Among the Level 1 predictors, motivation to abstain and the number of days in outpatient treatment and residential placement in the past month were related to lower levels of marijuana use. See Table 3 for a summary of Level 1 coefficients for this model. Specifically, for each additional day spent in residential placement, adolescents reported .34 fewer days of marijuana use during that same month. For each additional day in outpatient treatment, adolescents reported .24 fewer days of marijuana use. For every one point increase in motivation to abstain from marijuana use at the beginning of a month, adolescents reported nearly half a day (.39) less of marijuana use at the next month. However, perceived difficulty was unrelated to marijuana use over time. All of these effects were over and above the effect of initial severity of involvement, which predicted about two more days of marijuana use at each month for every additional symptom of marijuana use disorder reported at baseline (b = 2.08, UCL= 2.47, LCL = 1.69, p< .001). Thus, both month-to-month levels of motivation to abstain and treatment involvement hamper the return of marijuana use during and after treatment.
Table 3. Conditional Model Predicting Past Month Marijuana Use.
| Level 1 Predictors | ||||||
|---|---|---|---|---|---|---|
| π | UCL | LCL | t | df | p | |
| Intercept | 11.33 | 13.87 | 8.80 | 8.77 | 127 | 0.00 |
| Linear Slope | -2.95 | -1.03 | -4.87 | -3.01 | 128 | 0.00 |
| Quadratic Slope | 0.72 | 1.45 | 0.00 | 1.96 | 128 | 0.05 |
| Cubic Slope | -0.05 | 0.03 | -0.12 | -1.29 | 128 | 0.20 |
| Days in Placement | -0.34 | -0.21 | -0.46 | -5.12 | 699 | 0.00 |
| Days in Outpatient | -0.24 | -0.12 | -0.35 | -3.89 | 699 | 0.00 |
| Days in Twelve Step | -0.02 | 0.08 | -0.12 | -0.40 | 699 | 0.69 |
| Motivation | -0.39 | -0.19 | -0.58 | -3.85 | 699 | 0.00 |
| Difficulty | 0.09 | 0.23 | -0.04 | 1.32 | 699 | 0.19 |
π = the Level 1 coefficient of the fixed effect on the outcome
UCL and LCL = 95% upper and lower confidence limits
Longitudinal modeling of motivation to abstain from marijuana use
Unconditional model of motivation to abstain
We next developed an unconditional model of motivation to abstain from marijuana use over 6-month follow-up. For motivation to abstain, likelihood ratio testing suggested that trimming the linear effect from the model significantly degraded model fit (χ2 = 35.04, df = 2, p < .001); thus, we retained a linear growth effect for this model. Results indicated that motivation to abstain from marijuana use declined over time (b = -0.15, UCL = -0.05, LCL = -0.25, p < .001) by .15 per month (on a 1-10 scale), suggesting that from baseline to the six month follow-up, motivation to abstain decreased by an average of a full point on that scale. However, individuals differed in their rate of decline in motivation (variance component = 0.33, df = 118, χ2 = 196.73, p < .001), suggesting that some adolescents’ motivation declined more rapidly, and more slowly for others (and may have even increased over time for some individuals).
Conditional model of motivation to abstain
We next tested whether marijuana use in the previous month predicted deflections in individuals’ trajectories of motivation to abstain while controlling for previous month treatment and residential placement, concurrent report of perceived difficulty to abstain, and initial severity. Technically, this analysis modeled concurrent effects (i.e., all variables were reported at the same assessment, as depicted in Figure 2), but reflected what we presumed to be a prospective process in that we tested how marijuana use in the past month influenced the adolescent’s report on thoughts about abstinence (i.e., motivation to abstain) for the upcoming month. Results (Table 4) indicated that the more days of past month marijuana use the adolescent reported, the less motivated the adolescent was to abstain in the next month. For each additional day of marijuana use in the past month, motivation declined by almost 0.1 points over and above the decline accounted for by time, effectively accelerating the decline in motivation to abstain from marijuana use. On the other hand, neither severity of initial marijuana involvement (b = -0.11, UCL= 0.02, LCL = -0.24, p = .11) or time spent in treatment influence month to month variations in motivation to abstain. Finally, concurrent report of perceived difficulty to abstain was negatively associated with motivation to abstain; for every 1 point increase in perceived difficulty, motivation to abstain was reduced by .17.
Table 4. Prediction of Thoughts About Abstinence over 6-month follow-up.
| Predicting Motivation to Abstain from Marijuana Use | ||||||
|---|---|---|---|---|---|---|
| π | UCL | LCL | t | df | p | |
| Intercept | 8.88 | 9.43 | 8.33 | 31.52 | 138 | 0.00 |
| Slope | -0.11 | -0.02 | -0.21 | -2.29 | 139 | 0.02 |
| Days in Placement | 0.02 | 0.08 | -0.03 | 0.92 | 725 | 0.36 |
| Days in Outpatient | 0.02 | 0.06 | -0.02 | 0.86 | 725 | 0.39 |
| Days in Twelve Step | 0.03 | 0.06 | -0.01 | 1.43 | 725 | 0.15 |
| Days Used Marijuana | -0.09 | -0.06 | -0.13 | -5.65 | 725 | 0.00 |
| Perceived Difficulty | -0.17 | -0.09 | -0.24 | -4.41 | 725 | 0.00 |
| Predicting Perceived Difficulty to Abstain from Marijuana Use | ||||||
|---|---|---|---|---|---|---|
| π | UCL | LCL | t | df | p | |
| Intercept | 4.60 | 5.51 | 3.68 | 9.87 | 122 | 0.00 |
| Days in Placement | 0.00 | 0.05 | -0.06 | -0.09 | 726 | 0.93 |
| Days in Outpatient | 0.09 | 0.13 | 0.05 | 4.46 | 726 | 0.00 |
| Days in Twelve Step | 0.04 | 0.07 | 0.00 | 1.86 | 726 | 0.06 |
| Days Used Marijuana | 0.08 | 0.11 | 0.05 | 5.17 | 726 | 0.00 |
| Motivation to Abstain | -0.19 | -0.11 | -0.28 | -4.60 | 726 | 0.00 |
π = the Level 1 coefficient of the fixed effect on the outcome
UCL and LCL = 95% upper and lower confidence limits
Longitudinal modeling of perceived difficulty of abstaining from marijuana use
Unconditional model of perceived difficulty of abstaining
Based on the observed data, we began with an intercept only model for perceived difficulty of abstaining, and tested whether adding a linear slope improved the fit of the model using likelihood ratio testing. For perceived difficulty of abstaining, an intercept-only model provided the best fit to the data, when compared to a model with an intercept plus a linear slope effect (χ2 = 5.85, df = 2, p > .05). On average, adolescents reported moderate difficulty to abstain from marijuana (Intercept = 4.44; SE = .22, p < .001), but varied around that intercept over short-term follow-up (variance component = 4.82, df = 125, χ2 = 743.65, p < .001). Results suggest that, on average, perceived difficulty to abstain did not change over time, but that adolescents varied from month to month around that average in terms of perceived difficulty to abstain.
Conditional model of perceived difficulty of abstaining
Frequency of marijuana use was included as a predictor of perceived difficulty of abstaining in the next month, while controlling for monthly reports of treatment and 12-step attendance, and motivation to abstain (see Figure 2). Severity of marijuana involvement predicted higher perceived difficulty over time (b = 0.24, UCL= 0.42, LCL = 0.11, p < .001): for every additional symptom of marijuana use disorder reported at the baseline, perceived difficulty was a quarter point higher over time. Also, greater frequency of marijuana use in the previous month was associated with greater perceived difficulty of abstaining at the next month. For each additional day of marijuana use in the past month, perceived difficulty increased by about one eighth of a point (Table 4). Similar to the results for motivation to abstain, perceived difficulty to abstain was unrelated to time spent in residential placement in the previous month. On the other hand, outpatient treatment was unexpectedly related to increased perceived difficulty to abstain, and 12-step meeting attendance had a similar effect that approached significance (p = .06). Specifically, the more days an adolescent spent in outpatient treatment or attending 12-step meetings in the past month, the more difficult they reported abstaining would be. However, the magnitude of this effect was small: results suggested that even if an adolescent spent a full 30 days in outpatient treatment in one month (a highly unlikely scenario), perceived difficulty would increase by 2.7 points (on a 1-10 scale) at the beginning of the next month. Finally, concurrent motivation to abstain was negatively associated with perceived difficulty of abstaining; for every 1 point increase in motivation, perceived difficulty of abstaining was reduced by .19.
Discussion
This study characterized longitudinal associations between thoughts about abstinence from marijuana (i.e., motivation to abstain, perceived difficulty to abstain) and marijuana use in treated adolescents over short-term follow-up, and provided a test of the snares hypotheses applied to the process of recovery from marijuana use. Consistent with the adolescent substance use treatment outcome literature (reviews: Williams & Chang, 2000; Chung & Maisto, 2006), frequency of marijuana use showed an overall decline following treatment entry. However, monthly follow-up data collected in this study also indicated a gradual increase, on average, in frequency of marijuana use in months 5-6, although average frequency of use at the end of the follow-up period did not yet return to the baseline level. Of some concern, treated adolescents’ motivation to abstain from marijuana use declined, on average, over follow-up. In contrast, perceived difficulty of abstaining from marijuana use remained stably moderate over short-term follow-up. Importantly, only motivation to abstain (but not perceived difficulty to abstain) from marijuana use was independently associated with deflections from an individual’s trajectory of marijuana use, providing some support for the snares model. Moreover, longitudinal associations between motivation to abstain and marijuana use were bi-directional. Study findings highlight the central and dynamic role that an adolescent’s thoughts about abstinence play in relation to marijuana use during and following an index episode of intensive outpatient treatment. These findings suggest that targeting motivation to abstain both during and following treatment may potentially enhance and maintain treatment gains.
An important advance provided by the monthly follow-ups used in this study involved the documentation of month-to-month changes in thoughts about abstinence, specifically in relation to marijuana use. Motivation to abstain generally declined over follow-up, but the overall frequency of marijuana use does not begin to increase until about months 5-6. Although speculative, given the observed patterns of change in motivation to abstain and frequency of marijuana use it appears that the decrease in motivation to abstain may precede the increase in frequency of marijuana use in this sample of treated adolescents. Results of the longitudinal analyses suggest that motivation to abstain and frequency of marijuana use reciprocally influence one another, suggesting that as marijuana use returns to pre-treatment levels, it is both driven by and drives decreasing motivation to abstain, which in turn may accelerate the return to regular use, as would be predicted by the snares model. Given that motivation to abstain begins to decline around the time of discharge from the IOP, and that marijuana use begins to increases at around months 5-6, interventions designed to extend the gains achieved during the index treatment episode may be useful. For example, booster sessions that enhance or maintain motivation to abstain may be indicated by months 3-4 to improve treatment outcomes (e.g., Kaminer & Napolitano, 2004; Miller & Rollnick, 2002).
In contrast to changes in motivation to abstain and frequency of marijuana use over short-term follow-up, perceived difficulty to abstain from marijuana use remained stably moderate in this sample of treated youth. Moreover, both past month marijuana use and involvement in treatment (outpatient and, moderately, 12-step) predicted time specific increases in perceived difficulty to abstain, and as noted above increases in marijuana use were associated with reductions in motivation to abstain. It is not surprising that the more an adolescent uses marijuana, the more difficult abstaining would seem and the less important abstaining might feel. This finding may reflect a dissonance reduction process, where an adolescent shapes their thoughts about abstaining in response to failures to attain treatment goals. In addition, the finding that involvement in treatment amplified difficulty to abstain may reflect the effect of extended periods of abstinence enforced by the monitoring that occurs during treatment. Alternately, given that many adolescents begin to return to regular marijuana use following their initial declines, continuing to attend treatment in spite of a failure to abstain may make future attempts to abstain seem even more difficult. Finally, it could be that being in treatment is typically associated with initial reductions in substance use, a period during which difficulty to abstain may peak because behavior change is being initiated.
There was some evidence for a bi-directional longitudinal association between perceived difficulty to abstain and motivation to abstain. Specifically, greater motivation to abstain predicted lower perceived difficulty to abstain, and greater perceived difficulty to abstain predicted lower motivation to abstain. This finding highlights the inter-connected nature of adolescents’ thoughts about abstinence, and suggests that dimensions of an individual’s readiness to change their substance use behavior fluctuate somewhat together over time. Thus, interventions aimed at increasing self-efficacy to abstain may have the side benefit of increasing motivation to abstain, and vice versa. Importantly, the community-based treatment programs from which adolescents in the study were recruited did not provide an individually delivered motivational enhancement intervention. Specifically, IOP treatment was delivered in group-based format, and the mechanisms in group-based treatment that enhance adolescents’ motivation to abstain from substance use warrant investigation. In general, these findings suggest that motivation to abstain and self-efficacy are important targets of treatment, supporting the further integration of Motivational Interviewing (Miller & Rollnick, 2002) into adolescent treatment approaches. Moreover, given the widespread utilization of group-based treatments for adolescent substance use, these finding imply that further development of group-based motivational enhancement interventions for adolescents (e.g. Battjes, Baker, Webster & Lewin, 2004; Bailey, Baker, Webster & Lewin, 2004) are an important area of further study.
In this sample of treated adolescents, treatment utilization and residential placement were associated with deflections in an individual’s trajectory of marijuana use, motivation to abstain, and perceived difficulty to abstain from marijuana use. In particular, both number of days in outpatient and residential placement predicted lower marijuana use. Although the association of placement and marijuana use is not surprising given the impact of reduced opportunity to engage in substance use due to residence in a controlled environment, the impact of higher attendance in outpatient treatment on marijuana use is consistent with reviews of the treatment outcome literature, which indicate that longer retention in treatment is associated with better outcomes (Williams & Chang, 2000), and support recommendations for continuing care to maintain treatment gains in adolescent substance users (Godley, Godley & Dennis, 2001). In addition, the finding that greater outpatient and 12-step meeting attendance (moderately) predicted greater difficulty to abstain warrants further study with regard to possible explanations for these unexpected associations. Specifically, the mechanisms through which outpatient treatment and residential placement result in increased motivation to abstain and lower levels of marijuana use in treated youth remain to be determined.
Certain study limitations warrant comment. Given that the study sample was primarily Caucasian and male, study results may have limited generalizability to more ethnically diverse samples of treated youth, adolescent females in substance abuse treatment, youth who were recruited from other levels of care, and to substances other than marijuana (e.g., alcohol, tobacco). Motivational processes in adolescent substance users also likely differ from adults in substance use treatment. The impact of concurrent alcohol or other drug use also may influence trajectories during and following treatment, and will be examined in subsequent analyses. Moreover, the current analyses did not control for the stability of the predictors over time; thus the observed processes may reflect an influence of initial associations carrying through to later time points. However, as correlations between marijuana use and cognitions seemed to strengthen over time, this possibility seems less likely. Further, this study relied on self-reports of marijuana use and treatment attendance, which may be subject to bias, although care was taken to probe reports of substance use that were discrepant with the results of a urine drug screen, and the use of monthly follow-up intervals reduced bias due to retrospection over relatively long intervals. Moreover, the assessment of motivation and perceived difficulty were single-item measures that are used to represent complex constructs. In addition, other predictors of post-treatment substance use, such as peer substance use and social support for abstinence, which have been shown to attenuate growth in substance use following treatment (e.g., Godley, Kahn, Dennis, Godley, & Funk, 2005), will be examined in the future.
Frequency of marijuana use in treated adolescents generally declined over short-term follow-up, but an increase, on average, in frequency of marijuana use at follow-up months 5-6 highlights the potential utility of booster sessions to maintain treatment gains. The decline in motivation to abstain from marijuana use, and its prediction of frequency of marijuana use, further suggest that the content of booster sessions target methods to increase motivation to abstain. Support for a dynamic snare model, in which low motivation to abstain and greater perceived difficulty to abstain “snare” a return to more regular marijuana use in treated youth, further emphasize the importance of interventions that are designed to enhance and maintain motivation to abstain in order to improve adolescent treatment outcomes.
Acknowledgements
This study was supported by National Institute on Alcohol Abuse and Alcoholism grants AA014357 and AA017128 to Tammy Chung, and AA016928 to Stephen Maisto. Portions of these analyses were presented at the 2007 Annual Meeting of the Research Society on Alcoholism.
Footnotes
In the total sample, 3.5% had a current DSM-IV hallucinogen abuse diagnosis, 14.8% cocaine diagnosis (6.3% abuse, 8.5% dependence), 18.3% opiate diagnosis (5.6% abuse, 12.7% dependence), 4.8% sedative diagnosis (2.1% abuse, 2.8% dependence), 4.2% stimulant diagnosis (1.4% abuse, 2.8% dependence), 1.4% polysubstance dependence, and 45.8% nicotine dependence. Across six other drug categories (hallucinogen, cocaine, opiate, sedative, stimulant, polydrug), the average number of other drug diagnoses was 0.47 (SD=0.86, range 0-5).
Exclusion of youth with no current marijuana diagnosis (n=5) from the analyses generated results that were identical to those obtained in the larger sample, thus we report results for the total sample (n=142).
We inspected the records for all cases that reported being in residential placement. Across all cases and episodes of a stay in residential placement, only 3 were psychiatric inpatient stays unrelated to substance use and only 2 episodes involved conduct problems that did not also involve substance use (e.g., placement in juvenile detention for a reason that did not involve substance use). Thus, the majority of (89%) reported episodes of being in residential placement involved substance use.
To maximize the number of time points included in analyses, we used past month marijuana use at baseline as the initial time point, predicted by motivation and perceived difficulty reported at recruitment. However, unlike subsequent time points (which were scheduled to be collected at one month intervals), recruitment was an average of 15 days prior to baseline. Thus at the initial time point, thoughts about abstaining are not measured entirely prior to the time period that report of past month marijuana use covers. To test the impact of this effect, we reanalyzed the models predicting marijuana use excluding observations from the initial time point. The results of this model were nearly identical to the models including all available time points; thus we present the models that use all time points.
Not including predictors of the intercept at Level 2 may bias the other Level 1 predictors in the model by failing to control for inter-individual differences in month-to-month marijuana use. We tested this assumption by comparing the models in the current study to models that included predictors of the intercept at Level 2 (including demographics such as gender, age, SES, ethnicity, and initial diagnosis of conduct disorder, ADHD, or depression). Because the sample also varied in how much time had elapsed from their baseline assessment at the start of the IOP to their first full assessment at Month 0, we also included “time since baseline” in these analyses. However, including any of these predictors did not substantively change the effects of the other Level 1 predictors on the outcomes; thus we present the results of the simplified model.
Among those participants who did not complete the six-month assessment (n = 30, or 21% of the current sample), 15 (11%) were assessed at a longer term follow-up (e.g., 12 or 18 month follow-up), and 12 (8%) declined to continue study participation at some point after baseline. The overall long-term retention rate for the sample is 89%. Adolescents tended to have missing data at specific time points most often due to residential placement, reflecting the high-risk nature of this clinical sample.
Although we did not hypothesize individual differences in the time-varying effects of the covariates, it is possible that such effects exist. Accordingly, we tested whether including a random effect for each of the covariates provided an improvement in model fit over the fixed effect. For all time-varying covariates, the estimated random effect was close to zero, and the likelihood ratio test was not significant. This suggested that the more parsimonious model, which treated all time-varying covariates as fixed effects, provided the best fit to the data.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/ccp.
Contributor Information
Kevin M. King, University of Washington
Tammy Chung, University of Pittsburgh Medical Center.
Stephen A. Maisto, Syracuse University
References
- Amodei N, Lamb RJ. Convergent and concurrent validity of the Contemplation Ladder and URICA scales. Drug and Alcohol Dependence. 2004;73:301–306. doi: 10.1016/j.drugalcdep.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Bailey KA, Baker AL, Webster RA, Lewin TJ. Pilot Randomized Controlled Trial of a Brief Alcohol Intervention Group for Adolescents. Drug and Alcohol Review. 2004;23(2):157–166. doi: 10.1080/09595230410001704136. [DOI] [PubMed] [Google Scholar]
- Battjes RJ, Gordon MS, O’ Grady KE, Kinlock TW, Katz EC, Sears EA. Evaluation of a Group-Based Substance Abuse Treatment Program for Adolescents. Journal of Substance Abuse Treatment. 2004;27(2):123–134. doi: 10.1016/j.jsat.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: A quality of evidence review. Journal of Consulting and Clinical Psychology. 2008;76:531–543. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to change to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Burleson JA, Kaminer Y. Self-efficacy as a predictor of treatment outcome in adolescent substance use disorders. Addictive Behaviors. 2005;30:1751–1764. doi: 10.1016/j.addbeh.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Burleson JA, Kaminer Y. Adolescent alcohol and marijuana use: concordance among objective-, self-, and collateral-reports. Journal of Child and Adolescent Substance Abuse. 2006;16:53–68. [Google Scholar]
- Chung T, Maisto SA. Review and reconsideration of relapse as a change point in clinical course in treated adolescents. Clinical Psychology Review. 2006;26:149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, San Pedro R, Shriberg RF, Cornelius JR. Retest reliability and discrepancy interview for DSM-IV alcohol, cannabis, and nicotine diagnoses in treated adolescents. Alcohol Clinical and Experimental Research. 2004;28(supplement):111A. [Google Scholar]
- Clark DB, Pollock NA, Bromberger JT, Bukstein OG, Mezzich AC, Donovan JE. Gender and comorbid psychopathology in adolescents with alcohol use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1195–1203. doi: 10.1097/00004583-199709000-00011. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Donohue B, Azrin NH, Strada M, Silver NC, Teichner G, Murphy H. Psychometric evaluation of self- and collateral timeline follow-back reports of drug and alcohol use in a sample of drug-abusing and conduct disordered adolescents and their parents. Psychology of Addictive Behaviors. 2004;18:184–189. doi: 10.1037/0893-164X.18.2.184. [DOI] [PubMed] [Google Scholar]
- Donohue B, Hill HH, Azrin NH, Cross C, Strada MJ. Psychometric support for contemporaneous and retrospective youth and parent reports of adolescent marijuana use frequency in an adolescent outpatient treatment population. Addictive Behaviors. 2007;32:1787–1797. doi: 10.1016/j.addbeh.2006.12.005. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Godley MD, Kahn JH, Dennis ML, Godley SH, Funk RR. The stability and impact of environmental factors on substance use and problems after adolescent outpatient treatment for cannabis abuse or dependence. Psychology of Addictive Behaviors. 2005;19:62–70. doi: 10.1037/0893-164X.19.1.62. [DOI] [PubMed] [Google Scholar]
- Godley SH, Godley MD, Dennis ML. The assertive aftercare protocol for adolescent substance abusers. In: Wagner E, Waldron H, editors. Innovations in adolescent substance abuse interventions. Elsevier Science; New York: 2001. [Google Scholar]
- Hollingshead A. Four-factor index of social status. Author; New Haven: 1975. [Google Scholar]
- Hussong AM, Curran PJ, Moffitt TE, Caspi A, Carrig MM. Substance abuse hinders desistance in young adults’ antisocial behavior. Development and Psychopathology. 2004;16:1029–1046. doi: 10.1017/s095457940404012x. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Napolitano C. Dial for therapy: Aftercare for adolescent substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1171–1174. doi: 10.1097/01.chi.0000133260.98666.bf. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Meyers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychology of Addictive Behaviors. 2000;14:376–389. [PMC free article] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, Tevyaw TO, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug and Alcohol Dependence. 2005;79:33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Chung TA, Cornelius JR, Martin CS. Factor structure of the SOCRATES in a clinical sample of adolescents. Psychology of Addictive Behaviors. 2003;17:98–107. doi: 10.1037/0893-164x.17.2.98. [DOI] [PubMed] [Google Scholar]
- Martin CS, Kaczynski NA, Maisto SA, Bukstein OG, Moss HB. Patterns of DSM-IV alcohol abuse and dependence symptoms in adolescent drinkers. Journal of Studies on Alcohol. 1995;56:672–680. doi: 10.15288/jsa.1995.56.672. [DOI] [PubMed] [Google Scholar]
- Martin CS, Pollock NK, Bukstein OG, Lynch KG. Inter-rater reliability of the SCID alcohol and substance use disorders section among adolescents. Drug and Alcohol Dependence. 2000;59:173–176. doi: 10.1016/s0376-8716(99)00119-2. [DOI] [PubMed] [Google Scholar]
- McCaffrey DF, Morral AR, Ridgeway G, Griffin BA. Interpreting treatment effects when cases are institutionalized after treatment. Drug and Alcohol Dependence. 2007;89:126–138. doi: 10.1016/j.drugalcdep.2006.12.032. [DOI] [PubMed] [Google Scholar]
- Miller WR, Johnson WR. A natural language screening measure for motivation to change. Addictive Behaviors. 2008;33:1177–1182. doi: 10.1016/j.addbeh.2008.04.018. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10:81–89. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd Ed. Guildford Press; New York: 2002. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong Y, Congdon RT. HLM 6: Hierarchical Linear and Non-Linear Modeling. Scientific Software International; Chicago: 2004. [Google Scholar]
- Sampl S, Kadden R. Motivational enhancement therapy and cognitive behavioral therapy (MET-CBT-5) for adolescent cannabis users. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. [Google Scholar]
- Slavet JD, Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, et al. The Marijuana Ladder: Measuring motivation to change marijuana use in incarcerated adolescents. Drug and Alcohol Dependence. 2006;83:42–48. doi: 10.1016/j.drugalcdep.2005.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Assessment of drinking behavior. In: Allen JP, Columbus M, editors. Assessing alcohol problems. Humana Press; Bethesda, MD: 1995. pp. 55–74. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies . Treatment Episode Data Set (TEDS) Highlights—2006 National Admissions to Substance Abuse Treatment Services. Rockville, MD: 2007. OAS Series #S-40, DHHS Publication No. (SMA) 08-4313. [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- Williams RJ, Chang SY, Addiction Centre Adolescent Research Group A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7:138–166. [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]