Abstract
Aims
Adverse childhood events (ACEs) are associated with negative health outcomes. We examined ACEs as risk factors for substance dependence (SD) and the mediating effects of mood and anxiety disorders on the relations between ACEs and SD risk.
Design
We compared early life experiences in 2,061 individuals with a lifetime diagnosis of alcohol, cocaine, or opioid dependence and 449 controls.
Measurements
Diagnostic and ACE data were obtained using the Semi-Structured Assessment for Drug Dependence and Alcoholism.
Findings
Childhood abuse or exposure to violent crime was positively related to the number of lifetime mood and anxiety disorders and to SD risk. Mood and anxiety disorders had their first onset a mean of nearly 3 years before the first SD diagnosis and mediated the effect of ACEs on SD risk.
Conclusion
ACEs appear to contribute additively to the risk of SD, with mood and anxiety disorders in the causal path for a portion of this risk. The identification and effective treatment of mood and anxiety disorders associated with ACEs could reduce the risk of developing SD.
Keywords: Adverse Childhood Events, Substance Dependence, Family Environment, Child Abuse
1. INTRODUCTION
A substantial body of literature indicates that adolescents and adults who experience adverse events in childhood, such as abuse or neglect, are at increased risk to develop a wide range of enduring health problems. Maltreated children face a greater risk of medical illness in adulthood, including cardiovascular disease and obesity (Anda et al., 2006; Felitti et al., 1998; Springer, Sheridan, Kuo, & Carnes, 2007). A strong association also exists between negative childhood experiences and psychiatric illness, particularly depression and post-traumatic stress disorder (PTSD) (Chapman et al., 2004; Molnar, Buka, & Kessler, 2001; Penza, Heim, & Nemeroff, 2003; Widom, DuMont, & Czaja, 2007). Moreover, early childhood abuse is a significant risk factor for alcohol and drug abuse (Dube et al., 2003; Kendler et al., 2000; Nelson et al., 2002).
Childhood sexual abuse (CSA), specifically, is a strong predictor of psychopathology in adulthood, especially major depression, PTSD, and alcohol dependence (Dinwiddie et al., 2000; Langeland, Draijer, & van den Brink, 2004; Spak, Spak, & Allebeck, 1997). In a population-based sample of 1,411 female adult twins, 30.4% of subjects reported some form of childhood sexual abuse (CSA); those who experienced such abuse had a three-fold elevated risk of alcohol and drug dependence (Kendler et al., 2000). In a prospective study of 113 African-American women, having experienced multiple episodes of CSA was a better predictor of heavy drinking than was the nature of the abuse itself (Jasinski, Williams, & Siegel, 2000).
Other adverse childhood experiences may also play a role in the development of substance use disorders. A retrospective cohort study of 8,613 adults showed that individuals who experienced five or more adverse childhood events (ACEs; i.e., emotional, physical, or sexual abuse; domestic violence; and household dysfunction) were 7–10 times more likely to report illicit drug use and addiction, with the attributable risk fractions for ACEs being 56% and 63%, respectively (Dube et al., 2003). ACEs also contributed to an earlier onset of substance use, with each category of adverse experience associated with an elevated risk of illicit drug use prior to age 14. A strong, linear relationship exists between the total number of ACEs and various negative health outcomes (Anda et al., 2006; Chapman et al., 2004; Dube et al., 2003; Felitti et al., 1998; Springer, Sheridan, Kuo, & Carnes, 2007). For example, in a study of 17,337 adults, for each unit increase in the number of ACEs, there was a nearly 60% increased risk of attempted suicide (Dube et al., 2001).
Most studies relating ACEs to the subsequent development of psychopathology have been limited to the impact of physical or sexual abuse, without addressing many other possible ACEs. Parental alcohol and/or drug use is especially relevant, as it may increase a child’s risk of multiple adverse experiences (Anda et al., 2002; Galaif, Stein, Newcomb, & Bernstein, 2001). In a retrospective study of more than 9,000 adults, the increased risk of depression in adulthood associated with parental alcoholism was accounted for by a higher risk of ACEs in alcoholic families (Anda et al., 2002; Galaif, Stein, Newcomb, & Bernstein, 2001). A longitudinal community study showed that positive early family processes, such as parental support and bonding, predicted less problem alcohol use in adulthood (Galaif, Stein, Newcomb, & Bernstein, 2001). Thus, various family and household factors in childhood maltreatment warrant further study as potential moderators or mediators of adult psychopathology. A recent analysis of data from the National Epidemiologic Survey on Alcohol and Related Conditions, a population survey of more than 43,000 individuals, examined the impact on the risk of alcohol dependence of four childhood or adolescent adverse events: parental divorce, death of a biological parent, living with foster parents, and living in an institution (Pilowsky, Keyes, & Hasin, 2009). Controlling for potential confounders, this analysis showed that individuals who experienced two or more of these adverse events had a likelihood of developing alcohol dependence that was 1.37 times that of individuals who experienced no or one adverse event.
Because SD and other psychiatric disorders are highly comorbid in both clinical and non-clinical populations (Grant et al., 2004; Nunes & Rounsaville, 2006; Schuckit, 2006), the relationship between ACEs and these conditions continues to be of interest. A recent prospective study of 1,545 adolescent Finnish twins showed that an early onset of depressive disorders was predictive of frequent illicit drug and alcohol use, an association that was independent of shared familial influences (Sihvola et al., 2008). This finding provides initial support for the hypothesis that the relationship between negative experiences in childhood and subsequent SD may be partially mediated by mood and anxiety disorders.
We examined the role of a variety of ACEs on the risk of adult substance dependence (SD). We hypothesized that greater childhood trauma (i.e., violent crime, physical abuse, sexual abuse), the presence of substance use in the childhood household, and lower stability in the childhood home (as evidenced by a negative perception of family relationships, multiple caregivers, and multiple relocations) would be uniquely predictive of SD. Second, we predicted that multiple childhood traumas would increase SD risk in a cumulative fashion. Finally, because mood and anxiety disorders co-occur frequently among individuals with SD, we hypothesized that such disorders mediate the relations between ACEs and SD risk, findings that could inform efforts to identify and intervene with young adults to reduce the risk of SD.
2. METHODS
A subset of 2,510 subjects from the pooled data from family-based and case-control genetic studies of SD was selected for this secondary data analysis. These subjects were recruited at four sites: Yale University (New Haven, CT; n = 1,122); the University of Connecticut Health Center (Farmington, CT; n = 1,017), the Medical University of South Carolina (Charleston, SC; n = 305), and McLean Hospital (Belmont, MA; n = 66). The institutional review board at each of the participating locations approved the study protocol. After subjects received a complete description of the study, they provided written informed consent and were paid for their participation.
Subjects in the pooled dataset were recruited to participate in either family-based linkage studies or case-control association studies of the genetics of SD (Gelernter et al., 2005; Gelernter et al., 2007; Gelernter et al., 2006). The family-based sub-sample was ascertained through two or more siblings affected with a lifetime diagnosis of cocaine and/or opioid dependence. We recruited the case-control sub-sample as unrelated individuals with a lifetime diagnosis of alcohol, cocaine, or opioid dependence and healthy control subjects. Additional family members of probands from family-based studies and of cases from case-control studies were also recruited irrespective of their SD status. The control group was screened to exclude individuals with any psychiatric disorder, including a substance use disorder.
For this secondary data analysis, we selected only probands and their self-identified full- and half-siblings from either family or case-control studies. SD diagnoses were obtained using the Semi-Structured Assessment for Drug Dependence and Alcoholism (SSADDA, see details below), based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4thedition (DSM-IV: American Psychiatric Association, 1994). In the current regression-based analysis, cases and controls were defined based on the presence of a lifetime diagnosis of alcohol, cocaine or opioid dependence irrespective of ascertainment in the genetic studies. Data from 2,186 families were included, consisting of 420 families contributing control subjects only, 1,739 families contributing SD subjects only, and 27 families contributing both control and SD subjects. In total, there were 2,061 cases with lifetime dependence on alcohol, cocaine, or opioids, and 449 control subjects with no lifetime substance use disorder.
2.1. Assessment Procedures
All participants were evaluated using the SSADDA, which provides demographic information, assesses DSM-IV diagnostic criteria for lifetime substance dependence and a variety of co-morbid psychiatric disorders, including lifetime diagnoses of mood and anxiety disorders, and elicits information on the childhood home environment and other childhood experiences. A detailed description of this instrument, its administration methods, and its diagnostic reliability are provided elsewhere (Pierucci-Lagha et al., 2007; Pierucci-Lagha et al., 2005).
2.2 Measures
The primary outcome variable was a dichotomized lifetime SD diagnosis indicator. Subjects dependent on one or more of the following were considered positive for SD: alcohol, cocaine, and opioids. The control group consisted of subjects who were free of any lifetime diagnosis of abuse or dependence on alcohol, cocaine, opioids, nicotine, cannabis, sedatives, stimulants.
Eighteen variables derived from SSADDA items were evaluated as potential risk factors for membership in the SD group vs. the control group. These included 7 demographic control variables: sex, age, self-identified race/ethnicity [European-American (EA), African-American (AA), or Hispanic], 2-level marital status [never married vs. ever married or cohabiting (defined as having lived with someone for at least a year as though married)], years of education, 3-level employment status [employed full-time, employed part-time, or unemployed], and 3-level annual household gross income [≤$10,000, $10–29,999, ≥$30,000].
There was a high degree of psychiatric comorbidity in the sample, 33.3% (37.6% in the SD group and 13.8% in the control group) were diagnosed with at least one lifetime mood and/or anxiety disorder, and a summary measure of the number of lifetime mood or anxiety disorders was used as a potential mediator of SD risk. In this study, diagnoses for which information was incomplete due to non-response on relevant SSADDA items, which involved less than 4% of study participants, were treated as negative in computing the mood and anxiety disorder index. The index included major depressive disorder (MDD), bipolar disorder, PTSD, generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), social phobia, agoraphobia, and panic disorder. Because MDD and bipolar disorder are mutually exclusive, the score for this variable ranged from 0–7. The overall prevalence of the disorders was: 19.0% for any mood disorder (15.0% for MDD; 4.0% for bipolar disorder I or II), 13.9% for PTSD, 0.4% for GAD, 1.8% for OCD, 5.1% for social phobia, 5.6% for agoraphobia, and 5.5% for panic disorder. The test-retest and inter-rater reliability of the mood and anxiety disorder index was r=0.80 and r=0.73, respectively.
2.3 Adverse Childhood Events
The remaining 10 variables reflect subjects’ experiences in early life through adolescence. The test-retest and inter-rater reliability estimates for these items ranged from 0.62 to 0.99, and 0.41 to 0.82, respectively. Two of the variables reflected the perceived stability of the subjects’ home life: multiple main caregivers and number of relocations. Three predictors addressed the experience of childhood trauma: violent crime, sexual abuse, and physical abuse. The item “violent crime” was defined by subjects’ response to the question: “Did you witness or experience a violent crime, like a shooting or a rape, by age 13?” The predictor “sexual abuse” was defined by a response to the question: “By the time you were age 13, were you ever sexually abused?” and “physical abuse” was defined as being beaten by an adult so badly before age 13 that medical care was needed or marks on the body remained for more than 30 days. The remaining predictors were household substance use, regular household smoking, and three variables concerned with social interactions thought to be potentially protective against ACEs: frequency of religious participation [weekly or more frequent vs. less frequent], quality of relationship with the main caregiver, and frequency of contact with other relatives [monthly or more frequent vs. less frequent]. All of the questions elicited information on respondents’ experiences before the age of 13. All but two of the early childhood predictors were naturally dichotomous. The variable “number of relocations” was categorized into 4 levels: 0, 1, 2, and 3+, and “relationship with main caregiver” was categorized into 5 levels: excellent, very good, good, fair, and poor.
2.4. Analyses
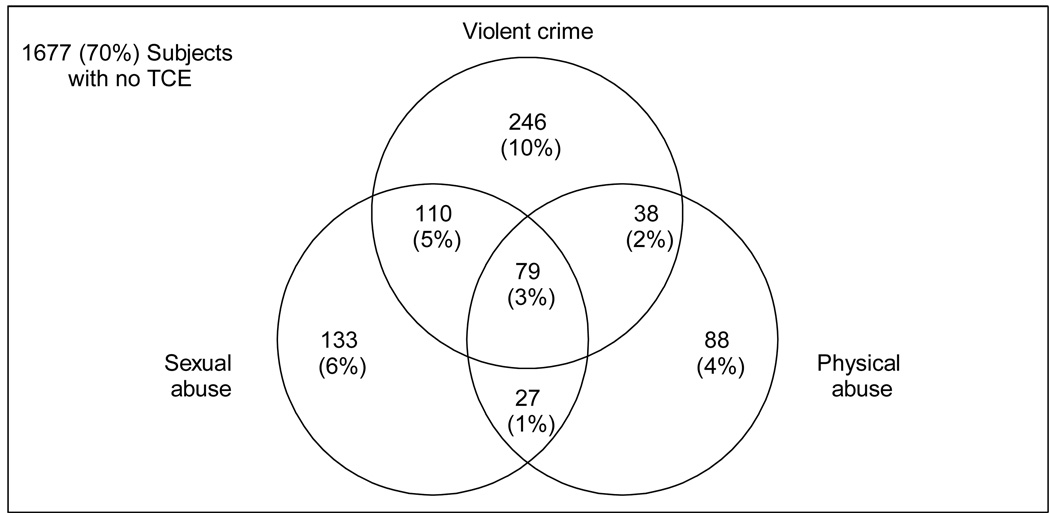
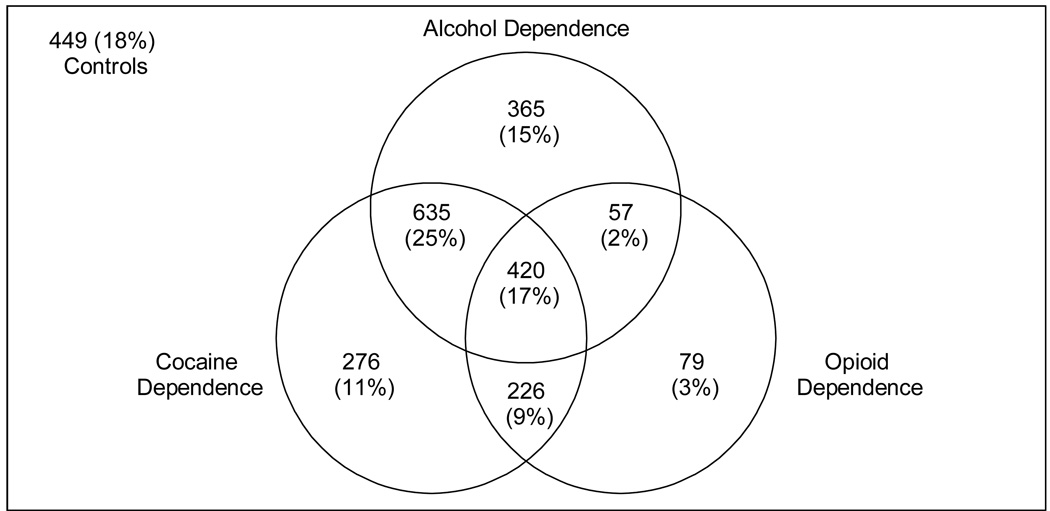
The 2,510 subjects represented 2,186 nuclear families, with 1–6 participants from each. Generalized estimating equation (GEE) analysis was used to model within-family correlation as exchangeable in all regression structures. Simple (unadjusted) logistic or normal regressions were used to examine pair wise association of the mood and anxiety index with all ACE predictors. To compare SD individuals with controls, logistic regression examined both unadjusted and adjusted relationships between the binary SD indicator and potential risk factors. Figure 1shows the cross-classifications of the three traumatic childhood experiences (i.e., witnessing violent crime or experiencing physical or sexual abuse). Given the primary focus on these factors, we also considered their two- and three-way interactions. Based on the findings of those analyses, we created a cumulative variable, “number of types of violent crime/abuse experiences,” which varies from 0–3, depending on whether the subject endorsed a history of violent crime experience, physical abuse, and/or sexual abuse (Cronbach’s α= 0.56). Many subjects met criteria for dependence on more than one substance. As can be seen in Figure 2, the largest proportion of individuals met lifetime criteria for cocaine dependence (n = 1,559), followed by alcohol dependence (n = 1,478) and opioid dependence (n = 783). Due to the high degree of overlap among the disorders, we examined the three SD diagnoses together to maximize statistical power.
Figure 1.
Cross-classification frequencies of three traumatic childhood experiences (TCEs): violent crime, sexual abuse, and physical abuse.
Figure 2.
Cross-classification frequencies of lifetime alcohol, cocaine, and opioid dependence. Note that the number of subjects with each disorder or combination of disorders includes only those with complete data on all three dependence diagnoses, so that the total is less than the total subject sample included in the analyses.
We used a stepwise selection procedure, a backward elimination procedure, and several fit statistics, taking the hierarchical nature of the interaction terms into consideration, to select a set of significant risk factors for the SD group classification. Pair wise deletion was used in all GEE logistic regressions.
We added the index of lifetime mood and anxiety disorders to the final model of the effects of the control and ACE variables, to examine the index’s impact on the relations between ACEs and risk of SD. First, we used a paired t-test to compare the age of onset of the first mood or anxiety disorder with the age of onset of the first SD disorder; an earlier age of onset of mood and anxiety disorders would be required to support the mediation model. We then applied a logistic Sobel Test (the Aroian version) (MacKinnon & Dwyer, 1993; Sobel, 1982) to test whether the mediator variable (i.e., the mood and anxiety disorder index) significantly carries the influence of an independent variable (i.e., ACEs) to a dependent variable (i.e., risk of SD).
3. RESULTS
3.1. Sample Characteristics and Unadjusted Relationships
The sample’s demographic characteristics are shown in Table 1. In the unadjusted simple logistic with GEE regression analysis, after Bonferroni correction, all but one control variable (race) were significantly associated with SD risk.
Table 1.
Demographic characteristics of the study sample and unadjusted tests in relation to substance dependence risk.
| Control Variables | Overall (n = 2510) |
SDa Group (n = 2061) |
Controls (n = 449) |
P-valueb |
|---|---|---|---|---|
| Sex | < 0.0001 | |||
| Male | 53.63% | 58.18% | 32.74% | |
| Age | < 0.0001 | |||
| Mean | 38.88 | 39.51 | 35.99 | |
| (s.d.) | (10.41) | (9.36) | (13.92) | |
| Race/Ethnicityc | 0.019 | |||
| EA | 38.62% | 37.82% | 42.32% | |
| AA | 52.81% | 52.91% | 52.34% | |
| Hispanic | 8.57% | 9.27% | 5.35% | |
| Marital Statusd | < 0.0001 | |||
| NM | 18.25% | 13.15% | 41.65% | |
| Education (yrs) | < 0.0001 | |||
| Mean | 12.18 | 11.72 | 14.26 | |
| (s.d.) | (2.24) | (2.01) | (2.07) | |
| Current Employment Status | < 0.0001 | |||
| Full-time | 23.12% | 17.56% | 48.87% | |
| Part-time | 15.12% | 13.81% | 21.17% | |
| Unemployed | 61.76% | 68.63% | 29.95% | |
| Current Household Income | < 0.0001 | |||
| ≤$10,000 | 47.65% | 53.60% | 20.36% | |
| $10,000 – $29, 999 | 29.19% | 29.34% | 28.51% | |
| ≥$30,000 | 23.16% | 17.06% | 51.13% |
Substance dependence
Wald Type III GEE χ2
EA: European-American; AA: African-American
NM: Never Married
Pair wise associations between the mood and anxiety disorder index and ACE predictors were positive and significant at the 5% level, except infrequent [less than weekly] religious participation and infrequent [less than monthly] contact with relatives. A similar pattern of pair wise associations existed among ACE predictor variables (again with the exception of infrequent religious participation and infrequent contact with relatives).
Table 2 provides values for the 12 study variables. In the unadjusted simple logistic with GEE regression analysis, after Bonferroni correction, 10 of the 12 study variables were significantly associated with risk of SD, including the mood and anxiety disorder index.
Table 2.
Characteristics of the study sample and unadjusted tests of study variables in relation to substance dependence risk.
| Study Variables | Overall (n = 2,510) |
SDaGroup (n = 2,061) |
Controls (n = 449) |
P-valueb |
|---|---|---|---|---|
| Multiple Caregivers | 0.004 | |||
| Yes | 7.50% | 8.25% | 4.24% | |
| Number of Relocations | < 0.0001 | |||
| 0 | 24.63% | 23.51% | 29.57% | |
| 1 | 21.96% | 20.50% | 28.44% | |
| 2 | 18.47% | 19.02% | 16.03% | |
| 3 + | 34.94% | 36.97% | 25.96% | |
| Violent Crime Exposure | < 0.0001 | |||
| Yes | 19.85% | 22.85% | 6.70% | |
| Sexual Abuse Exposure | < 0.0001 | |||
| Yes | 14.65% | 16.46% | 6.71% | |
| Physical Abuse Exposure | < 0.0001 | |||
| Yes | 9.72% | 11.49% | 2.01% | |
| Number of Types of Violent | < 0.0001 | |||
| Crime/Abuse Exposures Mean (s.d.) |
0.44 (0.77) | 0.50 (0.81) | 0.15 (0.42) | |
| Household Substance Use | < 0.0001 | |||
| Yes | 57.42% | 62.92% | 33.26% | |
| Regular Smokers in the | < 0.0001 | |||
| Household | ||||
| Yes | 73.74% | 78.28% | 53.79% | |
| Infrequent Religious | 0.71 | |||
| Involvement | 26.02% | 26.20% | 25.17% | |
| Yes | ||||
| Relationship with | < 0.0001 | |||
| Main Caregiver | ||||
| Excellent | 44.52% | 42.92% | 51.56% | |
| Very Good | 19.46% | 17.94% | 26.12% | |
| Good | 20.41% | 21.36% | 16.29% | |
| Fair | 9.79% | 11.01% | 4.46% | |
| Poor | 5.81% | 6.78% | 1.56% | |
| Infrequent Contact with | 0.18 | |||
| Relatives | 40.90% | 41.55% | 38.03% | |
| Index of Lifetime Mood and | < 0.0001 | |||
| Anxiety Disorders | ||||
| Mean (s.d.) | 0.51 (0.88) | 0.59 (0.93) | 0.18 (0.49) |
Substance dependence
Wald Type III GEE χ2
3.2. Adjusted Relations Between Outcome and Risk Factors
A set of 9 factors was jointly statistically significant (at the 5% level) as predictors of group membership (i.e., SD vs. control) in the final GEE logistic regression model. Table 3 displays the significant predictors, which included six demographic variables (sex, 3-level race/ethnicity, 2-level marital status, years of education, 3-level employment status, and 3-level household income) and three ACEs (number of types of violent crime/abuse experiences, household substance use, and regular household smoking).
Table 3.
Final GEE logistic model including significant predictor variables for SD riska
| Control or Risk Variable | Odds Ratio | P-valueb | |
|---|---|---|---|
| Estimate | 95% CIc | ||
| Sex | < 0.0001 | ||
| Female vs. Male | 0.24 | (0.17, 0.32) | |
| Race/Ethnicityd | 0.002 | ||
| AA vs. EA | 0.59 | (0.43, 0.80) | |
| Hispanic vs. EA | 0.54 | (0.27, 1.07) | |
| Marital Statuse | < 0.0001 | ||
| NM vs. M | 0.24 | (0.17, 0.32) | |
| Education | < 0.0001 | ||
| +1 | 0.62 | (0.57, 0.67) | |
| Employment Status | < 0.0001 | ||
| Full-time vs. Unemployed | 0.28 | (0.18, 0.37) | |
| Part-time vs. Unemployed | 0.54 | (0.36, 0.81) | |
| Current Household Incomef | < 0.0001 | ||
| Low vs. High | 2.77 | (1.87, 4.11) | |
| Medium vs. High | 2.30 | (1.64, 3.23) | |
| Number of Types of Violent | < 0.0001 | ||
| Crime/Abuse Experiences +1 |
1.76 | (1.35, 2.28) | |
| Household Substance Use | < 0.0001 | ||
| Yes vs. No | 1.97 | (1.46, 2.65) | |
| Household Regular Smoking | 0.001 | ||
| Yes vs. No | 1.67 | (1.23, 2.27) | |
Exclusive of the mood and anxiety disorder index
Wald Type III GEE χ2
Confidence interval
EA: European-American; AA: African-American
NM: Never Married; M: Ever Married or Cohabited
Low: ≤$10,000; Medium: $10,000–$29,999; High: ≥$ 30,000
Unemployed European-American males with a history of having been married or having cohabited and low household income and education levels were most likely to be diagnosed with alcohol, cocaine, or opioid dependence. After controlling for these characteristics, each additional violent crime or abuse experience resulted in a near doubling of the odds of being in the SD group. Growing up in a household in which there was substance use approximately doubled the odds, while living in a household with regular smokers increased the risk of SD by approximately two-thirds.
The mean age of onset of the first mood or anxiety disorder was 19.8 yrs (s.d. = 11.2), compared with a mean age of onset of the first SD diagnosis of 23.4 yrs (s.d. = 7.1); the mean paired difference was 3.0 yrs (s.d. = 11.9) (t772 = 7.0, p < 0.0001).
Inclusion in the model of the mood and anxiety disorder index attenuated the effects of these three childhood factors, though they all remained statistically significant predictors of SD risk (Table 4). Specifically, the odds ratio for the number of types of violent crime or abuse experiences declined from 1.76 (p < 0.0001) to 1.42 (p = 0.020), the odds ratio for household substance use declined from 1.97 (p < 0.0001) to 1.55 (p = 0.024), and the odds ratio for living in a household with regular smokers decreased from 1.67 (p = 0.001) to 1.51 (p = 0.029). After adjusting for significant control variables, examination of the relations between the mood and anxiety disorder index and the three childhood factors showed that the index was significantly related to the number of types of violent crime or abuse experiences (p < 0.0001) and household substance use (p < 0.0001), but not to regular household regular smoking (p = 0.21). Consequently, we did not test the effect of the mood and anxiety disorder index as a mediator of regular household regular smoking and SD risk.
Table 4.
Mood and anxiety disorder index as a mediator of the effects of ACEsa on SD risk
| Impact on main model | P-value of the adjusted relationship between mediator and ACE |
Logistic Sobel Test | |||
|---|---|---|---|---|---|
| ACEsa | Odds ratio |
p-value | Z-Test statistic |
P-value | |
| Violent | 1.76b | < 0.0001b | < 0.0001 | 3.89 | < 0.0001 |
| Crime/Abuse | ↓ | ↓ | |||
| Experiences | 1.42c | 0.020c | |||
| Household | 1.97b | < 0.0001b | < 0.0001 | 3.21 | 0.001 |
| Substance | ↓ | ↓ | |||
| Use | 1.55c | 0.024c | |||
| Household | 1.67b | 0.001b | 0.21 | Not Applicable | |
| Regular | ↓ | ↓ | |||
| Smoking | 1.51c | 0.029c | |||
Adverse childhood experiences
Prior to inclusion in the model of the mediator variable
After inclusion in the model of the mediator variable
Application of the Sobel Test for binary outcome variables (MacKinnon & Dwyer, 1993; Sobel, 1982) indicated that the mood and anxiety disorder index mediated the effect of the number of types of violent crimes or abuse experiences (Z-Test Statistic = 3.89, p < 0.0001). Similarly, there was evidence for mediation by mood and anxiety disorders on the relations between household substance use and SD risk (Z-Test Statistic = 3.21, p = 0.001).
In this sample, 264 (10.52%) subjects reported an age of onset of mood or anxiety disorder after the onset of SD, inconsistent with the temporal order inherent in a mediation model (Baron & Kenny, 1986). When the logistic Sobel test for mediation was repeated excluding these 264 subjects, the results were nearly identical.
4. DISCUSSION
Our initial hypotheses regarding SD were supported by the finding that individuals who had experienced sexual abuse or physical abuse, or who witnessed violent crime were significantly more likely to be diagnosed with SD, consistent with prior studies showing that ACEs increase the likelihood of SD later in life. We extended prior findings by demonstrating that subjects who grew up in a home where substance use and regular smoking were present were significantly also more likely to be dependent on alcohol, cocaine, and/or opioids. Household substance use nearly doubled the risk of SD, while household smoking increased the risk by approximately two-thirds. Because substance use and dependence have a substantial genetic contribution (Gelernter & Kranzler, 2008), family members’ use of substances may, in part, reflect the heritability of these traits and their interaction with the environment. As anticipated, the SD group also reported less household stability, reporting a significantly greater number of relocations, multiple main caregivers, and a lower perceived quality of relationship with the primary caregiver during childhood than for control group.
In addition, consistent with our hypothesis and previous research, we found a cumulative effect of childhood traumas on the risk of SD (Anda et al., 2006; Dube et al., 2003; Felitti et al., 1998). Specifically, for every unit increase in the number of types of violent crime/abuse experiences, a person’s odds of developing dependence on alcohol, cocaine, and/or opioids were nearly doubled (Table 3). Thus, repeated or co-occurring childhood traumas may potentiate the harmful consequences of these events to a greater extent than any one type of childhood trauma alone.
Our findings are also consistent with evidence that relations between ACEs and SD are mediated by psychiatric disorders (Kessler, Davis, & Kendler, 1997; Sihvola et al., 2008; Simpson & Miller, 2002). Using data from the National Comorbidity Survey, the associations between ACEs and addictive disorders were mediated by psychiatric disorders; however, in that study, ACEs had no direct relationship with SD (Kessler, Davis, & Kendler, 1997). Further, a review of studies involving adults who had experienced childhood physical or sexual abuse concluded that, although abuse is a significant risk factor for substance use problems, the relationship is apparently mediated by psychiatric illness, including depression and anxiety disorders (Simpson & Miller, 2002).
We found that the development of mood and anxiety disorders usually preceded the onset of SD and a summary measure of lifetime mood and anxiety disorders mediated the effects of two ACEs on subsequent SD. Specifically, the inclusion of this measure attenuated the effects of childhood trauma and household substance use, though these remained significant predictors (consistent with a modest direct effect of ACEs on SD risk). These findings provide support for a causal chain in which ACEs lead to an increased risk of mood and anxiety disorders, which in turn lead to an increased risk of substance dependence. It should be acknowledged that, although the mediation effects are statistically significant, they do not fully explain the relations between ACEs and risk of SD. There is a robust effect of ACEs on risk of SD that is independent of the development of mood and anxiety disorders.
Limitations of this study include the fact that the sample was not from the general population, with a preponderance of SD subjects, including those dependent on cocaine and opioids. In addition, the relatively small control group increases the chance of Type II error in our analyses, so that we may have missed or underestimated some important risk factors for SD. Although there were demographic differences between SD subjects and controls, we controlled for these differences in the analyses. Further, ACEs were quantified using the SSADDA, rather than a more widely used assessment in childhood abuse research, such as the Childhood Trauma Questionnaire (Bernstein et al., 1994) or the Early Trauma Inventory (Bremner, Vermetten, & Mazure, 2000). In particular, the SSADDA’s strict definition of physical abuse may have increased the likelihood of a correlation between such severe trauma and future psychopathology. Nonetheless, our findings are consistent with other studies of ACEs and substance use that utilized these well-established instruments (Dube et al., 2003; Galaif, Stein, Newcomb, & Bernstein, 2001), supporting the validity of the inventory of childhood events in the SSADDA. Finally, we obtained the data through retrospective recall by subjects, potentially introducing errors and biases in reporting. A study of the validity of retrospective reporting for childhood sexual abuse, which used existing medical records as a criterion measure, showed that the occurrence of abuse was underestimated by self-report (Edwards et al., 2001). Despite these limitations, our findings dovetail with the existing literature and address a wider spectrum of family factors. In particular, the finding that the lifetime mood and anxiety disorder index was a mediator of SD risk has broad implications for clinical interventions and future research on causal chains in the development of SD.
A 25-year prospective study of 1,265 New Zealand children examined developmental precursors to illicit drug use in adulthood (Fergusson, Boden, & Horwood, 2008). Consistent with our findings, the authors reported that childhood abuse and parental substance use were significant predictors of future illicit drug use. They also evaluated the pathway from drug use to drug dependence and found that cannabis use, early onset alcohol use, and affiliation with substance using peers were significant mediators. Another recent study found that childhood maltreatment increased the risk of developing an Axis II disorder (Tyrka, Wyche, Kelly, Price, & Carpenter, 2009), suggesting that personality disorders, as well as mood and anxiety disorders, may warrant research as mediators of the effect of ACEs on SD risk.
SD treatment outcomes for adults abused as children are of particular clinical interest (Pirard, Sharon, Kang, Angarita, & Gastfriend, 2005; Rosen, Ouimette, Sheikh, Gregg, & Moos, 2002). In a sample of 700 substance-abusing patients, half had experienced physical or sexual abuse. These individuals were more impaired at baseline, required more outpatient treatment, and had a worse psychiatric status at one-year follow-up (Pirard, Sharon, Kang, Angarita, & Gastfriend, 2005). A study of 26,000 veterans also showed that individuals who were abused as children had poorer SD treatment outcomes at one-year follow up (Rosen, Ouimette, Sheikh, Gregg, & Moos, 2002).
Continued study of the environmental, genetic, and psychiatric factors that increase the risk for SD can guide our understanding of the detrimental long-term consequences of ACEs, including the gene by environment interactions that contribute to these negative outcomes. By addressing a more complete spectrum of ACEs and examining psychiatric disorders as mediators of SD, this research may help to identify novel approaches to early intervention among at-risk children and young adults, thereby helping to prevent the severe adverse consequences of childhood maltreatment.
ACKNOWLEDGEMENTS
This study was supported by NIH grants, DA12690, DA12849, DA15105, DA022288, AA11330, AA13736, and GM08607. The authors thank the interviewers and other research personnel who conducted the study, and the study participants at all of the research sites.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- American Psychiatric Association. 4th Edition. American Psychiatric Press Inc: Washington, DC; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Vermetten E, Mazure CM. Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: the Early Trauma Inventory. Depression and Anxiety. 2000;12(1):1–12. doi: 10.1002/1520-6394(2000)12:1<1::AID-DA1>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PA, Slutske WS, et al. Early sexual abuse and lifetime psychopathology: a co-twin-control study. Psychological Medicine. 2000;30(1):41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Journal of American Medical Association. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Anda RF, Nordenberg DF, Felitti VJ, Williamson DF, Wright JA. Bias assessment for child abuse survey: factors affecting probability of response to a survey about childhood abuse. Child Abuse and Neglect. 2001;25(2):307–312. doi: 10.1016/s0145-2134(00)00238-6. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: evidence from a 25-year longitudinal study. Drug and Alcohol Dependence. 2008;96(1–2):165–177. doi: 10.1016/j.drugalcdep.2008.03.003. [DOI] [PubMed] [Google Scholar]
- Galaif ER, Stein JA, Newcomb MD, Bernstein DP. Gender differences in the prediction of problem alcohol use in adulthood: exploring the influence of family factors and childhood maltreatment. Journal of Studies on Alcohol and Drugs. 2001;62(4):486–493. doi: 10.15288/jsa.2001.62.486. [DOI] [PubMed] [Google Scholar]
- Gelernter J, Kranzler HR. Genetics of addiction. In: Galanter M, Kleber HD, editors. Textbook of Substance Abuse Treatment. 4th ed. Washington, DC: American Psychiatric Press Inc; 2008. pp. 17–27. [Google Scholar]
- Gelernter J, Panhuysen C, Weiss R, Brady K, Hesselbrock V, Rounsaville B, et al. Genomewide linkage scan for cocaine dependence and related traits: significant linkages for a cocaine-related trait and cocaine-induced paranoia. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2005;136B(1):45–52. doi: 10.1002/ajmg.b.30189. [DOI] [PubMed] [Google Scholar]
- Gelernter J, Panhuysen C, Weiss R, Brady K, Poling J, Krauthammer M, et al. Genomewide linkage scan for nicotine dependence: identification of a chromosome 5 risk locus. Biological Psychiatry. 2007;61(1):119–126. doi: 10.1016/j.biopsych.2006.08.023. [DOI] [PubMed] [Google Scholar]
- Gelernter J, Panhuysen C, Wilcox M, Hesselbrock V, Rounsaville B, Poling J, et al. Genomewide linkage scan for opioid dependence and related traits. American Journal of Human Genetics. 2006;78(5):759–769. doi: 10.1086/503631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Jasinski JL, Williams LM, Siegel J. Childhood physical and sexual abuse as risk factors for heavy drinking among African-American women: a prospective study. Child Abuse and Neglect. 2000;24(8):1061–1071. doi: 10.1016/s0145-2134(00)00158-7. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57(10):953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27(5):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Langeland W, Draijer N, van den Brink W. Psychiatric comorbidity in treatment-seeking alcoholics: the role of childhood trauma and perceived parental dysfunction. Alcohol: Clinical and Experimental Research. 2004;28(3):441–447. doi: 10.1097/01.alc.0000117831.17383.72. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. American Journal of Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, et al. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Archives of General Psychiatry. 2002;59(2):139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Nunes EV, Rounsaville BJ. Comorbidity of substance use with depression and other mental disorders: from Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) to DSM-V. Addiction. 2006;101(S1):89–96. doi: 10.1111/j.1360-0443.2006.01585.x. [DOI] [PubMed] [Google Scholar]
- Penza KM, Heim C, Nemeroff CB. Neurobiological effects of childhood abuse: implications for the pathophysiology of depression and anxiety. Archives of Women's Mental Health. 2003;6(1):15–22. doi: 10.1007/s00737-002-0159-x. [DOI] [PubMed] [Google Scholar]
- Pierucci-Lagha A, Gelernter J, Chan G, Arias A, Cubells JF, Farrer L, et al. Reliability of DSM-IV diagnostic criteria using the semi-structured assessment for drug dependence and alcoholism (SSADDA) Drug and Alcohol Dependence. 2007;91(1):85–90. doi: 10.1016/j.drugalcdep.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierucci-Lagha A, Gelernter J, Feinn R, Cubells JF, Pearson D, Pollastri A, et al. Diagnostic reliability of the Semi-structured Assessment for Drug Dependence and Alcoholism (SSADDA) Drug and Alcohol Dependence. 2005;80(3):303–312. doi: 10.1016/j.drugalcdep.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Keyes KM, Hasin DS. American Journal of Public Health. 2. Vol. 99. Washington DC: American Psychiatric Press Inc.; 2009. Adverse childhood events and lifetime alcohol dependence; pp. 258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirard S, Sharon E, Kang SK, Angarita GA, Gastfriend DR. Prevalence of physical and sexual abuse among substance abuse patients and impact on treatment outcomes. Drug and Alcohol Dependence. 2005;78(1):57–64. doi: 10.1016/j.drugalcdep.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Ouimette PC, Sheikh JI, Gregg JA, Moos RH. Physical and sexual abuse history and addiction treatment outcomes. Journal of Studies on Alcohol and Drugs. 2002;63(6):683–687. doi: 10.15288/jsa.2002.63.683. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006;101(S1):76–88. doi: 10.1111/j.1360-0443.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- Sihvola E, Rose RJ, Dick DM, Pulkkinen L, Marttunen M, Kaprio J. Early-onset depressive disorders predict the use of addictive substances in adolescence: a prospective study of adolescent Finnish twins. Addiction. 2008;103(12):2045–2053. doi: 10.1111/j.1360-0443.2008.02363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clinical Psychology Review. 2002;22(1):27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Social Methodology. Washington D.C: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- Spak L, Spak F, Allebeck P. Factors in childhood and youth predicting alcohol dependence and abuse in Swedish women: findings from a general population study. Alcohol and Alcoholism. 1997;32(3):267–274. doi: 10.1093/oxfordjournals.alcalc.a008266. [DOI] [PubMed] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse and Neglect. 2007;31(5):517–530. doi: 10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrka AR, Wyche MC, Kelly MM, Price LH, Carpenter LL. Childhood maltreatment and adult personality disorder symptoms: influence of maltreatment type. Psychiatry Research. 2009;165(3):281–287. doi: 10.1016/j.psychres.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64(1):49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]