Abstract
Objective
To evaluate the anatomical parameters that must be considered when performing thoracic transpedicular or extrapedicular screw fixation.
Methods
We selected 958 vertebrae (1,916 pedicles) from 98 patients for analysis. Eight parameters were measured from CT scans : the transverse outer pedicular diameter, transverse inner pedicular diameter, length, angle, chord length of the pedicles and the transverse width, angle, and chord length of the pedicle-rib units.
Results
The age of the patients ranged from 21 to 82 years (mean : 48.2 years) and there were 57 men and 41 women. The narrowest transverse outer pedicular diameter was at T5 (4.4 mm). The narrowest pedicle length was at T1 (15.9 mm). For pedicle angle, T1 was 31.6 degrees, which was the most convergent angle, and it showed the tendency of the lower the level, the lesser the convergent angle. The chord length showed a horizontal pattern with similar values at all levels. For the PRU width, T5 showed a similar pattern to the pedicle width at 13.4 mm. For the PRU angle, T1 was the largest angle at 46.2 degrees and the tendency was the lower the level, the narrower the angle. For chord length, T1 was the shortest at 46.9 mm and T8 was the longest at 60.1 mm.
Conclusion
When transpedicular screw fixations carried out at the mid-thoracic level, special care must be taken because there is a high chance of danger of medial wall violation. In these circumstances, extrapedicular screw fixation may be considered as an alternative treatment.
Keywords: Pedicle screws, Extrapedicular screws, Thoracic spine, Pedicle morphology, Spine fixation, Morphology
INTRODUCTION
Transpedicular screw fixation methods are increasingly being used worldwide and because transpedicular screws provide sufficient mechanical strength and pull-out strength, almost all spinal surgeons currently use transpedicular screw systems3,8). However, the mechanical properties of these systems vary with regard to individual pedicular anatomy, especially in pedicle width, length, angle, and chord length1). Especially in thoracic spine, the accuracy of pedicle screws fixation may be prone to be lower than that of the lumbar spine because of anatomical characteristics. Thus, the importance of the anatomical morphometric structures of the pedicle is emphasized8,21). For the purpose of overcoming this weakness and the avoidance the inherent risks of the conventional approach for pedicle screw placement, Dvorak et al.6) presented an assessment of an extrapedicular screw fixation technique in the thoracic spine. But hitherto, there have been only a few reports about clinical, radiological and biomechanical results of this techniques.
Thus, the authors measured the anatomical parameters relevance to pedicle and extrapedicle screw fixations of Korean populations and compared them with those of other populations to reveal ethnic characteristics. Also, we investigated the characteristics and usefulness of extrapedicular screw fixation in the point of anatomical aspects.
MATERIALS AND METHODS
CT scans of the entire thoracic spine using a Philips scanner (16 slice MX800IDT, Royal Philips Electronics Inc., Amsterdam, Netherlands) with 2-mm slices were reviewed. A gantry was applied in tune with the direction of the pedicle's sagittal plane at each level. We selected 958 vertebrae (1,916 pedicles) from 98 patients for analysis. The age of the patients ranged from 21 to 82 years (mean : 48.2 years) and there were 57 men and 41 women. The age of the men ranged from 21 to 78 years (mean : 42.8 years) and that of the women ranged from 24 to 82 years (mean : 52.6 years). Included diseases were trauma, tumor, infection, degenerative and strain. Pathologic spines which were not able to apply exact gantry were excluded. The regions for which accurate measurements were impossible due to severe anatomical distortions were excluded. For each body, five parameters related to pedicles (transverse outer pedicular diameter, transverse inner pedicular diameter, length, angle and chord length) and three parameters related to extrapedicular structures (transverse width, angle and chord length) were measured. Each sides of parameters, mean values of both sides and standard deviations were determined separately for males and females. Complete descriptions of the measured parameters are presented in Fig. 1, 2.
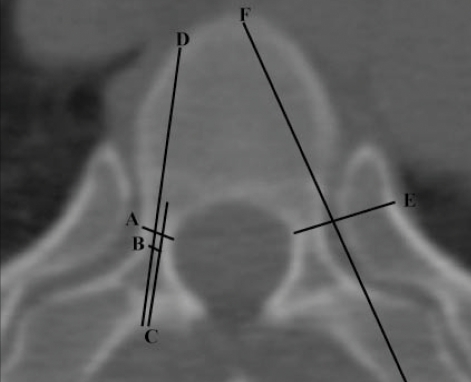
Fig. 1.
Measurements of parameters related to lengths, which were obtained from preoperative axial computed tomography scans. A : transverse outer pedicular width, B : transverse inner pedicular width, C : pedicular length, D : pedicular chord length, E : extrapedicular width, F : extrapedicular chord length.
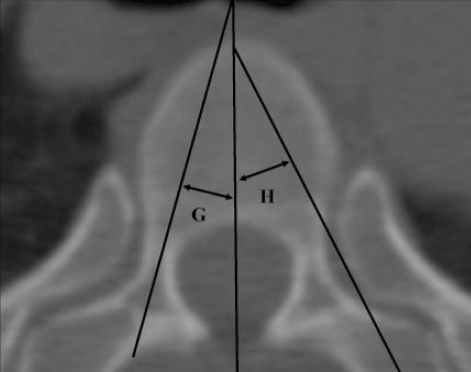
Fig. 2.
Measurements of parameters related to angles, which were obtained from preoperative axial computed tomography scans. A : pedicular angle, B : extrapedicular angle.
RESULTS
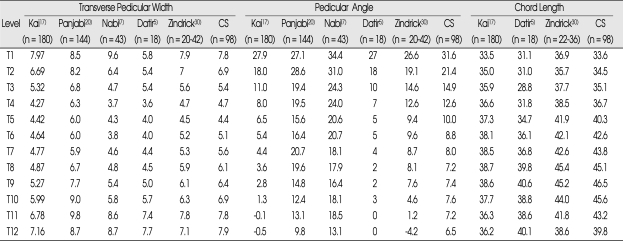
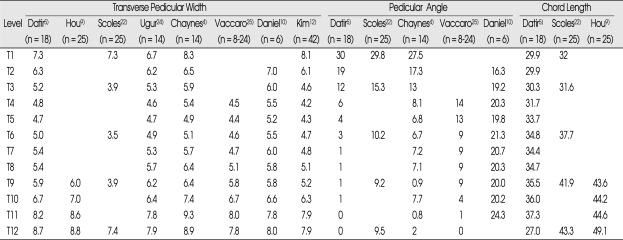
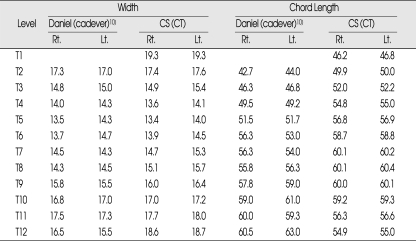
The list of the pedicular morphometric and statistical data of males and females based on CT measurements is shown in Table 1. For each level, the means and standard deviations of males and females went down the lists. The described values were mean values calculated from both sides of pedicles because right and left values showed no statistically no differences. Table 2 is the list of the transverse width, angle, and chord length of the pedicle-rib unit (PRU) in the extrapedicular anatomical structure, in the same manner as shown in Table 1. Table 3, 4, and 5 shows the lists of the comparison studies with the previous data and the current ones.
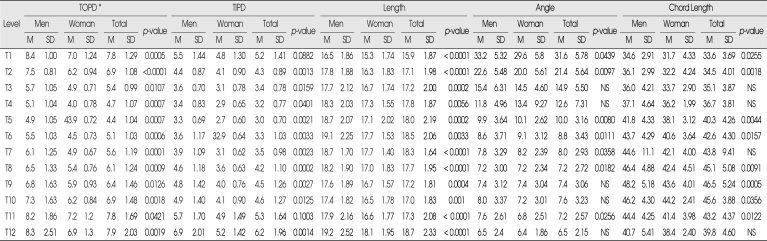
Table 1.
Measurements of thoracic pedicular anatomic parameters: transverse outer pedicular diameter (TOPD), transverse inner pedicular diameter (TIPD), length, angle, and chord length
TIPD : transverse inner pedicular diameter, TOPD : transverse outer pedicular diameter
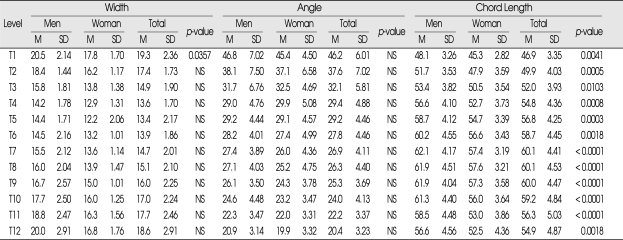
Table 2.
Measurements of extrapedicular anatomic parameters : extrapedicular (pedicle-rib unit, PRU) width, angle, and chord length
Table 3.
Comparison of computed tomography-measured pedicular width, angle, and chord length with previously reported data
CS : current study
Table 4.
Comparison of pedicle width, angle, and chord length with data from studies that were measured from cadavers
Table 5.
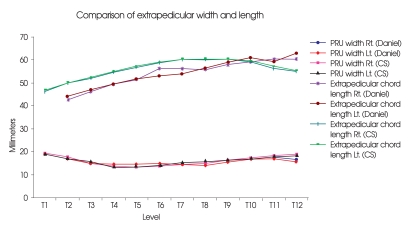
Comparison of extrapedicular width, angle, and chord length with data from studies that were measured from cadavers
We used two sample t-tests for statistical analysis and SAS version 9.1 as the statistical program. A p-value less than 0.05 was considered statistically significant.
Transverse outer pedicular diameter
For both males and females, T1 was the widest at 8.4 mm and 7.0 mm, respectively. The width gradually decreased from T1 to T4 until it was the narrowest at T4, and then gradually increased (Fig. 5). The narrowest region was T4 (males : 5.5 mm, females : 4.4 mm, total : 4.7 mm), and the widest region was T1 (males : 8.4 mm females 7.0 mm). In overall, the region with the greatest mean value was T12 (7.9 mm). Transverse outer pedicular diameter (TOPD) were larger at every level in males compared with females.
Fig. 5.
Comparison of extrapedicular (pedicle-rib unit) widths.
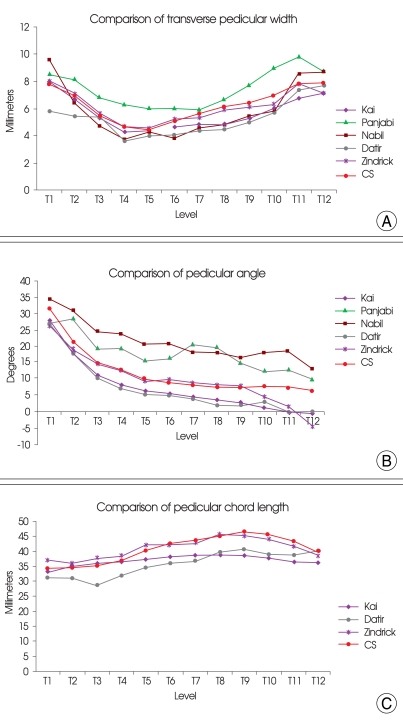
We compared our data with the data of previous studies (Fig. 3A). All of the data including the current data showed the similar trend except for the data of Panjabi, which showed generally large values in the upper levels. When the data from cadaveric studies were compared with the current study, all of the data showed similar patterns except for Daniel's data.
Fig. 3.
Comparison study (measurement from computed tomography scan). A : Transverse pedicular widths. B : Pedicular angles. C : Pedicular chord lengths.
Transverse inner pedicular diameter
In males, the TIPD decreased until T4; it was the smallest at T4 and T5, and increased again from T6. In females, the TIPD decreased until T5, and then steadily increased. The narrowest region was T5 (males : 3.3 mm, females : 2.7 mm, total : 3.0 mm), and the widest region was T12 (6.9 mm) for males and T1 (4.8 mm) for females. T12 was the widest in total with a mean of 6.2 mm and T5 was the narrowest in total with a mean of 3.0 mm. TIPDs were also larger in males compared with females at every level.
Previous studies measured outer pedicular width and very few measured inner pedicular width, so we could not compare previous data with the current data.
Pedicular length
The pedicular length tended to increase from T1 to T6, but it showed a pattern of relatively constant and similar values after that. The narrowest region was T1 (males : 16.5 mm, females : 15.3 mm) and the longest region was T6 (males : 19.1 mm, females : 17.7 mm). In overall, the region with the longest value was T12 (18.7 mm), and the region with the shortest value was T1 (15.9 mm). The pedicle lengths were longer in males compared with females at every level.
Pedicular angle
The region that showed the widest angle was T1 (33.2 degrees) for males and T1 (29.6 degrees) for females. It was also T1 with a value of 31.6 degrees. The pedicular angle gradually narrowed as the level progressed from T1 to T12, and it was the narrowest at T12 (males : 6.5 degrees, females : 6.4 degrees, total : 6.5 degrees). There was no significant difference between male and female patients at any level.
Comparing the data of other researchers, the data have nearly the same values and trends as those of the present data (Fig. 3B). When we examined the data of other researchers who used cadavers, they showed the same trend, except for the data of Daniel and Datir (Fig. 4B).
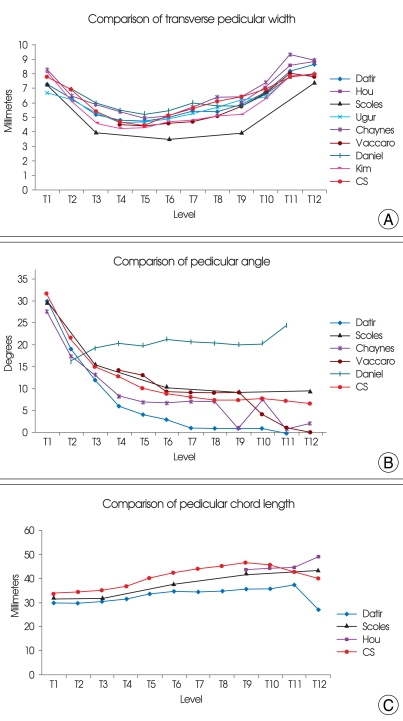
Fig. 4.
Comparison study (measurement from cadavers). A : Transverse pedicular widths. B : Pedicular angles. C : Pedicular chord lengths.
Pedicular chord length
Chord length of the pedicle is the maximum length of a screw that can be inserted into each pedicle. Therefore, the chord length is referred to as the "maximal pedicle screw pathway." This value increased from T1 to T9, and showed a decreasing trend from T10 to T12. The shortest region was T1 (males : 34.6 mm, females : 31.7 mm), and the longest region was T9 (48.2 mm) for males and T10 (44.2 mm) for females. The region with the longest mean value was T9 (46.5 mm). There was no significant difference between male and female patients at any level. The data of other studies showed nearly identical values and trends as the current data (Fig. 3C, 4C).
Extrapedicular width (pedicle rib unit width)
The PRUW is the distance from the pedicle's medial border to the rib's lateral border. Like the pedicle width, the PRUW decreased from T1 to T4 and T5, and then increased to T12. The narrowest region was T4 (14.2 mm) for males and T5 (12.2 mm) for females, and the widest region was T1 (males : 20.5 mm, females : 17.8 mm). PRUWs were larger in males compared with females at every level. There are no PRUW measurements using CT. Daniel's data, which was measured using cadavers, had similar patterns and trends as the present data (Fig. 5).
Extrapedicular angle
The angle was the largest at T1 (males : 46.8 degrees, females : 45.4 degrees, total : 46.2 degrees), and gradually decreased until T12, where the angle was the smallest (males : 20.9 degrees, females : 19.9 degrees, total : 20.4 degrees). There was no significant difference between male and female patients at any level.
Extrapedicular chord length
Extrapedicular chord length increased from T1 to T7, and then tended to decrease until T12. The shortest region was T1 (males : 48.1 mm, females : 45.3 mm), and the longest region was T7 (62.1 mm) for males and T8 (57.6 mm) for females. The regions with the longest mean value were T7 and T8 (60.1 mm). Extrapedicular chord length was greater in males compared with females at every level. The measurement data of Daniel and its trends were similar to those of the current data (Fig. 5).
DISCUSSION
For the western population, Zindrick et al. first reported the various parameters of thoracic pedicles by indirect measurements using CT and for the Korean population, Kim et al. reported direct measurements using cadavers12,30). Although the average height, weight, and BMI may differ by sex and race, most previous reports calculated the mean values of the total population without the division of males and females. Hence, the authors statistically analyzed the measurements of males and females and found that there were statistically significant differences2,23). As shown in Table 1, the transverse outer pedicular diameter, transverse inner pedicular diameter, and pedicular length were larger in males at almost every levels. However, the pedicle angle and chord length showed no differences between males and females, which leads to the conclusion that the parameters related to length, such as the gross measurements of the body and pedicle width and length, are proportional to sex, but the parameters related to angle are not related to sex. Furthermore, for pedicle width, which is the most important factor for pedicle screw fixation, this study showed that the width between the TOPD and TIPD was the narrowest at T5, and it was significantly narrower than other regions by around 5 mm from T3 to T6. As shown in Tables 3 and 4, this result was consistent with the results of other researchers, because the difference is not large, we can say that the region with the narrowest pedicle width is T4 or T5.
Nowadays, two insertional techniques which have been frequently performed in the thoracic spine include the straight-forward technique, in which the sagittal trajectory of the screw parallels the superior endplate of the vertebral body, and the anatomical trajectory, which is directed about 22 degrees in the cephalocaudal direction in the sagittal plane and parallels the anatomical axis of the pedicle. In both methods, the screws are ideally confined completely within the pedicle. In the coronal or transverse plane, pedicle axis varies slightly by level from near straight-forward at T12 to approximately 25 degrees convergence in the upper thoracic spine at T115,16). Contrary to lumbar pedicle, transverse width of thoracic pedicle is significantly less than its height and it has less medial inclination. There is scarcely located epidural space between the dural sac and the medial wall of the pedicle, but there are a few millimeters spaces between the spinal nerve roots and superior or inferior wall of the pedicle7,13,14,18). Thus, transverse pedicular width is more important than pedicular height. When choosing between two techniques, the posterior surface landmarks including transverse process, laminar, and facet joint should be considered15,16).
The transverse pedicular angle of lumbar vertebrae was the narrowest at L1 and increased toward L5. However, the angle was the largest at the upper thoracic (26.6-34.4 degrees) level and decreased toward the lower thoracic level; it was the narrowest at T11 or T1218,21,24). This angle is in reverse relation with the lumbar region.
Like the pedicle length, chord lengths are not greatly deviated and the relationships are horizontal, as shown in the graph, which is similar to the reports of other authors. The range is 28.8 mm to 46.5 mm. It is the shortest at T1 and the longest at T9 and T10. It becomes shorter toward T12, but it is still longer than in the upper thoracic level26).
In the case of extrapedicle parameters, it is not a single anatomical structure, but a virtual complex structure that consists of ribs and pedicles. This is referred to as the PRU11,27). In this study, we observed the interesting results that are different from the results of pedicles. Like the pedicle width, the PRU width was the narrowest at the T4 and T5 levels. As shown in the graph, the pattern is similar to that of pedicle width, but the gaps between the levels were smaller than those of pedicle width. This was very similar to the direct measurements of cadavers by Daniel, as was the difference between left and right. The transverse angle of the PRU was the largest at T1 and decreased as the thoracic level descended. The chord length of the PRU was the shortest at T1 and gradually became longer, reaching the maximum at T7 and T8, after which it gradually became shorter. The width and angle of the PRU were not different between males and females, but males appeared to have a greater chord length. This is the difference in the analysis results for various parameters between the pedicles and PRU.
There are a few requirements for screw placement to maintain better stability. The screw diameter must be larger, the screw length must be longer, or the screw insertional angle must be more convergent. When we compare the data of various investigators including current study, the probability of the medial wall violation is high during pedicle screw fixation because the pedicles between T3 and T7 are very narrow. To avoid violation, screws with smaller diameters and less convergent angles must be selected, and this is likely to lower the mechanical and pull-out strength.
To overcome this circumstance and avoid the violation by pedicle screws, extrapedicular screws fixation was introduced and has been performed in selected cases. Hitherto, extrapedicular screws fixation is unfamiliar to the spine surgeons. But, based on various anatomical and biomechanical studies, extrapedicular screws fixation maybe a helpful alternative technique in the very narrowed pedicles, especially mid thoracic spine. It provides a larger screw diameter, longer screw length and more convergent angle. Because of these reasons, this technique may be considered as another method of salvage of a failed/violated pedicle29).
Some studies revealed that the biomechanical strength of the extrapedicular screw fixation was not inferior to that of the intrapedicular screw fixation. Dvorak et al.6) reported rhat the biomechanical superiority of the extrapedicular screw fixation compared with intrapedicular screw fixation was ascertained. This insistence was due to additional sites of cortical bone purchase and the increased length of the screws. Also, this technique provided longer screw distance and reduction risks for violation of neurologic structures. However, they concluded that the posterior element anatomy was too variable to allow for a standardized insertion technique and that clinical application of this technique should be considered with cautious optimism in clinical circumstances in which conventional insertion techniques are not infeasible. On the other hand, Morgenstern et al.19) found no difference in range of motion in the thoracic spine constructs from T4-T8 when using either technique. Extrapedicular screw constructs averaged about 75% of the strength of transpedicular screws in this study and from a biomechanical standpoint, was second only to that of intrapedicular screw fixation when instrumenting the thoracic spine. White et al.28) came to a conclusion that transpedicular screws are biomechanically superior to the extrapedicular screws, but, this difference, however, was small. Extrapedicular screws offer a useful alternative when anatomy dictates their use with other screws in a segmental spinal construct when anatomy precludes safe, traditional placement. Previous investigations showed that biomechanical strengths of extrapedicular screws were not much behind those of transpedicular screws.
CONCLUSION
The anatomical parameters of the pedicles and extrapedicles of thoracic vertebrae appear to differ greatly by level, but exhibit a certain pattern or trend described as above. The parameters related to length are different between males and females with males having larger values. There is no difference in the angle-related values between males and females. In the mid-thoracic level, special care must be taken during pedicle screw fixation because the transverse pedicular width is very narrow. Particularly for females, more attention should be given. In this circumstances, extrapedicular screws fixation would be considered as an alternative.
References
- 1.Bernard TN, Jr, Seibert CE. Pedicle diameter determined by computed tomography. Its relevance to pedicle screw fixation in the lumbar spine. Spine (Phila Pa 1976) 1992;17(6) Suppl:S160–S163. doi: 10.1097/00007632-199206001-00017. [DOI] [PubMed] [Google Scholar]
- 2.Berry JL, Moran JM, Berg WS, Steffee AD. A morphometric study of human lumbar and selected thoracic vertebrae. Spine (Phila Pa 1976) 1987;12:362–367. doi: 10.1097/00007632-198705000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Chadha M, Balain B, Maini L, Dhaon BK. Pedicle morphology of the lower thoracic, lumbar, and S1 vertebrae : an Indian perspective. Spine (Phila Pa 1976) 2003;28:744–749. [PubMed] [Google Scholar]
- 4.Chaynes P, Sol JC, Vaysse P, Bécue J, Lagarrigue J. Vertebral pedicle anatomy in relation to pedicle screw fixation : a cadaver study. Surg Radiol Anat. 2001;23:85–90. doi: 10.1007/s00276-001-0085-z. [DOI] [PubMed] [Google Scholar]
- 5.Datir SP, Mitra SR. Morphometric study of the thoracic vertebral pedicle in an Indian population. Spine (Phila Pa 1976) 2004;29:1174–1181. doi: 10.1097/00007632-200406010-00004. [DOI] [PubMed] [Google Scholar]
- 6.Dvorak M, MacDonald S, Gurr KR, Bailey SI, Haddad RG. An anatomical, radiographic, and biomechanical assessment of extrapedicular screw fixation in the thoracic spine. Spine (Phila Pa 1976) 1993;18:1689–1694. doi: 10.1097/00007632-199309000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine. 1997;22:1553–1556. doi: 10.1097/00007632-199707150-00002. discussion 1557. [DOI] [PubMed] [Google Scholar]
- 8.Fisher CG, Sahajpal V, Keynan O, Boyd M, Graeb D, Bailey C, et al. Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine. 2006;5:520–526. doi: 10.3171/spi.2006.5.6.520. [DOI] [PubMed] [Google Scholar]
- 9.Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine (Phila Pa 1976) 1993;18:1850–1855. doi: 10.1097/00007632-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Husted DS, Haims AH, Fairchild TA, Kershaw TS, Yue JJ. Morphometric comparison of the pedicle rib unit to pedicles in the thoracic spine. Spine (Phila Pa 1976) 2004;29:139–146. doi: 10.1097/01.BRS.0000105537.49674.A3. [DOI] [PubMed] [Google Scholar]
- 11.Husted DS, Yue JJ, Fairchild TA, Haims AH. An extrapedicular approach to the placement of screws in the thoracic spine: an anatomic and radiographic assessment. Spine (Phila Pa 1976) 2003;28:2324–2330. doi: 10.1097/01.BRS.0000085361.32600.63. [DOI] [PubMed] [Google Scholar]
- 12.Kim NH, Lee HM, Chung IH, Kim HJ, Kim SJ. Morphometric study of the pedicle of thoracic and lumbar vertebrae in Koreans. Spine (Phila Pa 1976) 1994;19:1390–1394. doi: 10.1097/00007632-199406000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Kothe R, O'Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle. An anatomic study. Spine (Phila Pa 1976) 1996;21:264–270. doi: 10.1097/00007632-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 14.Krag MH, Weaver DL, Beynnon BD, Haugh LD. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine (Phila Pa 1976) 1988;13:27–32. doi: 10.1097/00007632-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Lehman RA, Jr, Kuklo TR. Use of the anatomic trajectory for thoracic pedicle screw salvage after failure/violation using the straight-forward technique: a biomechanical analysis. Spine (Phila Pa 1976) 2003;28:2072–2077. doi: 10.1097/01.BRS.0000084628.37133.BA. [DOI] [PubMed] [Google Scholar]
- 16.Lehman RA, Jr, Polly DW, Jr, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ., Jr Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine (Phila Pa 1976) 2003;28:2058–2065. doi: 10.1097/01.BRS.0000087743.57439.4F. [DOI] [PubMed] [Google Scholar]
- 17.Liau KM, Yusof MI, Abdullah MS, Abdullah S, Yusof AH. Computed tomographic morphometry of thoracic pedicles: safety margin of transpedicular screw fixation in malaysian malay population. Spine (Phila Pa 1976) 2006;31:E545–E550. doi: 10.1097/01.brs.0000225978.97652.e0. [DOI] [PubMed] [Google Scholar]
- 18.Lien SB, Liou NH, Wu SS. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16:1215–1222. doi: 10.1007/s00586-006-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgenstern W, Ferguson SJ, Berey S, Orr TE, Nolte LP. Posterior thoracic extrapedicular fixation : a biomechanical study. Spine (Phila Pa 1976) 2003;28:1829–1835. doi: 10.1097/01.BRS.0000083280.72978.D1. [DOI] [PubMed] [Google Scholar]
- 20.Panjabi MM, Takata K, Goel V, Federico D, Oxland T, Duranceau J, et al. Thoracic human vertebrae. Quantitative three-dimentional anatomy. Spine (Phila Pa 1976) 1991;16:881–901. doi: 10.1097/00007632-199108000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Park YK, Lee JK, Lim DJ, Chung HS, Lee HK. Pedicle screw fixation of the thoracic spine. J Korean Neurosurg Soc. 1999;28:190–195. [Google Scholar]
- 22.Scoles PV, Linton AE, Latimer B, Levy ME, Digiovanni BF. Vertebral body and posterior element morphology : the normal spine in middle life. Spine (Phila Pa 1976) 1988;13:1082–1086. doi: 10.1097/00007632-198810000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Tan SH, Teo EC, Chua HC. Quantitative three-dimensional anatomy of cervical, thoracic and lumbar vertebrae of Chinese Singaporeans. Eur Spine J. 2004;13:137–146. doi: 10.1007/s00586-003-0586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ugur HC, Attar A, Uz A, Tekdemir I, Egemen N, Genç Y. Thoracic pedicle : surgical anatomic evaluation and relations. J Spinal Disord. 2001;14:39–45. doi: 10.1097/00002517-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine. Part II An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Vougioukas VI, Weber J, Scheufler KM. Clinical and radiological results after parapedicular screw fixation of the thoracic spine. J Neurosurg Spine. 2005;3:283–287. doi: 10.3171/spi.2005.3.4.0283. [DOI] [PubMed] [Google Scholar]
- 28.White KK, Oka R, Mahar AT, Lowry A, Garfin SR. Pullout strength of thoracic pedicle screw instrumentation comparison of the transpedicular and extrapedicular techniques. Spine (Phila Pa 1976) 2006;31:E355–E358. doi: 10.1097/01.brs.0000219394.48091.d6. [DOI] [PubMed] [Google Scholar]
- 29.Yüksel KZ, Adams MS, Chamberlain RH, Potocnjak M, Park SC, Sonntag VK, et al. Pull out resistance of thoracic extrapedicular screws used as a salvage procedure. Spine J. 2007;7:286–291. doi: 10.1016/j.spinee.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 1987;12:160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]