Abstract
Objective
Medpor porous polyethylene was used to reconstruct small bone defects (gaps and burr holes) along a craniotomy bone flap. The feasibility and cosmetic results were evaluated.
Methods
Medpor Craniotomy Gap Wedges, V and T, were designed. The V implant is a 10 cm-long wedge strip, the cross section of which is an isosceles triangle with a 4 mm-long base, making it suitable for gaps less than 4 mm after trimming. Meanwhile, the Medpor T wedge includes a 10 mm-wide thin plate on the top surface of the Medpor V Wedge, making it suitable for gaps wider than 4 mm and burr holes. Sixty-eight pterional craniotomies and 39 superciliary approaches were performed using the implants, and the operative results were evaluated with respect to the cosmetic results and pain or tenderness related to the cranial flap.
Results
The small bone defects were eliminated with less than 10 minutes additional operative time. In a physical examination, there were no considerable cosmetic problems regarding to the cranial bone defects, such as a linear depression or dimple in the forehead, anterior temporal hollow, preauricular depression, and parietal burr hole defect. Plus, no patient suffered from any infectious complications.
Conclusion
The Medpor Craniotomy Gap Wedge is technically easy to work with for reconstructing small bone defects, such as the bone gaps and burr holes created by a craniotomy, and produces excellent cosmetic results.
Keywords: Cosmetic appearance, Craniotomy, Medpor, Operative technique
INTRODUCTION
A current standard craniotomy requires burr holes to introduce the craniotome and leaves bone gaps along the bone flap. The adult craniotome makes a narrow bone gap, approximately 2 mm wide, and usually does not cause a cosmetic problem. However, if the bone flap is repositioned flush to one side of the craniotomy to avoid the defect above the orbital ridge, as in a pterional craniotomy and supraorbital mini-craniotomy in the superciliary approach, the bone gap on the other side is doubled in width. As a result, these widened craniotomy gaps along with the burr holes can produce undesirable and disfiguring furrows and dimples in the forehead.
Accordingly, the author (J.P.) designed two types of Medpor implants to fill such gaps and burr holes, and reports on a surgical technique to use them.
MATERIALS AND METHODS
Medpor Craniotomy Gap Wedge
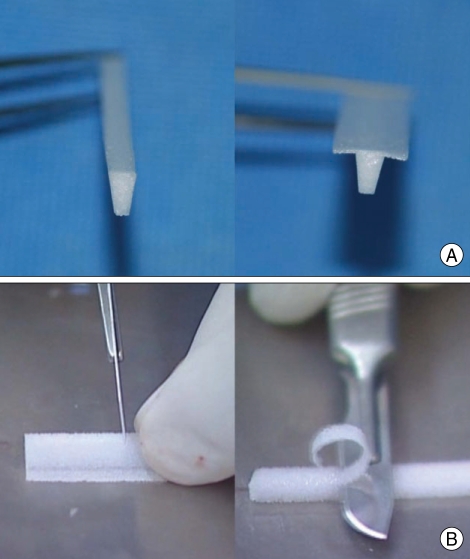
Two types of Medpor Craniotomy Gap Wedge, V and T, were designed to fill the small bone defects invariably left after a craniotomy (Fig. 1A). These porous polyethylene implants are manufactured and sterilized by Porex Surgical, Inc (Newman, Georgia).
Fig. 1.
Photographs of Medpor Craniotomy Gap Wedge. A : V Type (left) and T type (right) implants. B : For a gap of less than 4 mm, the Medpor V Wedge is trimmed appropriately with a scalpel (left), while The Medpor T Wedge is cut to fit various larger bone defects (right).
The Medpor V Wedge is a 10 cm-long wedge strip, a cross section of which is an isosceles triangle. The base of the triangle is 4 mm, making it suitable for bone gaps up to 4 mm wide. For gaps less than 4 mm, the implant is trimmed appropriately with a scalpel (Fig. 1B). Meanwhile, the Medpor T Wedge includes a 10 mm-wide thin plate on the top surface of the Medpor V Wedge, making it suitable for gaps wider than 4 mm and burr holes.
Operative technique
Pterional craniotomies, one of the most widely used approaches in neurosurgery, have been modified by many neurosurgeons to improve the cosmetic problems. Major cosmetic concerns are related to the frontotemporal branch of the facial nerve, the temporalis muscle, and small bone defects along the cranial bone flap, including the keyhole defect.
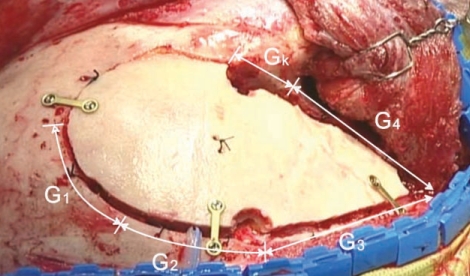
In a pterional craniotomy, the bone flap is fixed frontally and medially without bony distance to avoid the defect above the orbital ridge. Thus, the bone gap around the cranial flap can be arbitrarily divided into five segments : a vertical bone gap in the upper forehead (G1), an upper posterior gap without temporalis coverage (G2), a lower posterior gap with temporalis coverage (G3), a gap at the temporal base (G4), and defects including the keyhole and drilled out sphenoid ridge (GK) (Fig. 2). G1 and G2 gaps are prominent and disfiguring in patients with a high forehead (Fig. 3), and reconstructed with the implant if 3 mm or wider. G3 and G4 gaps are not problematic from a cosmetic perspective, yet large defects or burr holes can cause local pain or tenderness due to muscle adherence to the underlying dura. GK gaps are also cosmetically important as they can cause an anterior temporal hollow.
Fig. 2.
Intraoperative photograph showing bone gaps along the cranial flap after a pterional craniotomy. G1 = vertical bone gap in the upper forehead; G2 = upper posterior gap with no temporalis coverage; G3 = lower part gap with temporalis coverage; G4 = gap at the temporal base; GK = defect comprised of keyhole and drilled out sphenoid ridge.
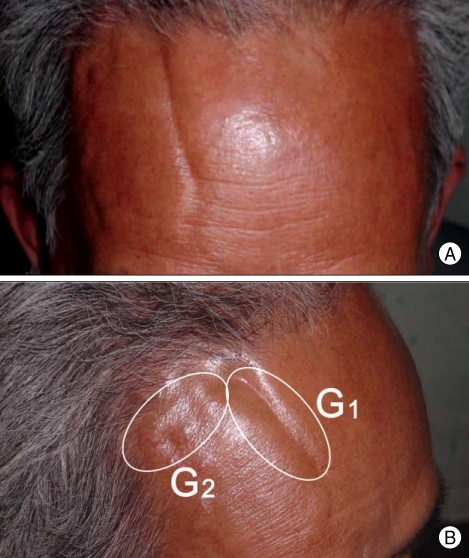
Fig. 3.
Photographs showing undesirable linear depressions in the forehead after a pterional craniotomy. A : Noticeable vertical groove (G1) in the upper forehead remarkable. B : Vertical groove (G1) and upper posterior gap (G2) without temporalis coverage in a patient with a high forehead.
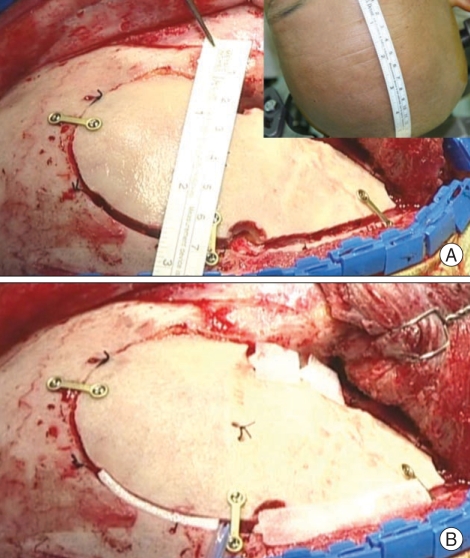
Measuring the height of the forehead can be used to predict the cosmetic effect of burr holes and bone gaps (Fig. 4A). For a GK gap, a short segment of a Medpor T Wedge is suitable. For G1 and G2 gaps of less than 4 mm, a Medpor V Wedge can be trimmed with a scalpel to fill the gap. For a gap wider than 4 mm and associated burr holes, a Medpor T Wedge can be cut to a suitable length and bent slightly to fit. In most cases, the Craniotomy Gap Wedges do not require any additional fixation procedures, such as screws or sutures (Fig. 4B).
Fig. 4.
Intraoperative photographs showing a pterional craniotomy. A : Cosmetic effect of bone defects along the cranial flap predicted based on measuring (inlet) the forehead before skin incision. B : Gaps 3 mm or greater and associated burr holes reconstructed using the Medpor Craniotomy Gap Wedge.
An eyebrow keyhole approach requires a small craniotomy above the orbital ridge, but the defect along the bone flap can make a more remarkable facial disfigurement than larger craniotomy. A keyhole and bone gaps around the small cranial flap are filled with small pieces of the Medpor T and V Wedges.
Assessment of cosmetic results
Between July 2007 and December 2008, the authors used the Medpor Craniotomy Gap Wedge in 68 pterional craniotomies and 39 superciliary approaches. The Medpor implants were used for all patients with the superciliary approach and selected patients with the pterional approach who are younger than 60 years old. More than 3 months after the surgery, the operative results were examined in several cosmetic points, as follows : a linear depression in the forehead, anterior temporal hollow, preauricular depression, and parietal burr hole defect in the patients who underwent the pterional craniotomy; linear depressions in the forehead and a dimple at the keyhole site in the patients with the superciliary approach.
RESULTS
In 68 pterional craniotomies and 39 superciliary approaches, bone gaps 3 mm or greater and burr holes were easily filled with the implants in each case. Additional operative time required for the implantation of the preformed Medpor Cranial Gap Wedge was less than ten minutes. Postoperatively, the implantation was not related to any infection or any other complications.
In the physical examinations, no considerable cosmetic problems were found. No linear depressions and dimples were visible on the forehead. No focal hollow in the anterior temporal area due to a keyhole defect was noticed, whereas nine patients showed a slight, diffuse hollow in the temporal area due to atrophy of the temporalis in cases of a pterional craniotomy. Three patients developed mild preauricular tenderness, yet in those cases a temporal bone defect was not covered with the implant. There was no palpable bone defect found at the site of a parietal burr hole on the scalp.
DISCUSSION
Although surgical techniques using an oscillating saw and chisel for a craniotomy have been developed to avoid leaving burr holes and gaps, such techniques are more difficult than standard craniotomies using a craniotome3,5). The drill bits for adult craniotomes are either fluted or spiral. The fluted routers of the Midas Rex system (Medtronic Inc., Fort Worth, TX, USA) and Anspach eMax system (Anspach Effort Inc., Palm Beach Gardens, FL, USA) are 16 mm long, with a 1.85 mm diameter at the tip that increases to 2 mm over a length of 10 mm, reaching 2.3 mm at the base. Meanwhile, the spiral router for the Anspach eMax system is 22 mm long, with a 1.75 mm diameter at the tip that also increases to approximately 2 mm over a length of 10 mm, reaching 3.15 mm at the base. Therefore, the width of the bone gap produced by such craniotomes depends on the types of the routers and the thickness of the skull due to the increasing diameter of the routers from the tip. Thus, a skull with a 10 mm thickness results in bone gaps greater than 2 mm. Furthermore, when the bone flap is repositioned flush to one side, as in a pterional craniotomy, the width of the bone gap on the other side is doubled, i.e., greater than 4 mm. Such wide bone gaps and burr holes create cosmetic problems on the forehead and can also cause local pain due to the adherence of the scalp and muscle to the underlying dura through the bone defect14).
The Medpor implants are composed of high-density polyethylene with a continuous porosity. Fibrovascular and bony ingrowth into the pores makes the implant stable, biocompatible, and resistant to infection. In the case of a pterional craniotomy revised six months after implanting a Medpor Wedge, bony ingrowth was demonstrated in the implant (Fig. 5). Medpor porous polyethylene also has other advantages, including easy usage due to its plasticity and carvability, radiolucency on plain X-rays and CT scans, and MR compatibility without artifacts. Thus, it has been widely used to reconstruct various locations in craniofacial surgeries since its approval by the U.S. Food and Drug Administration in 19841,2,4,6,10,12).
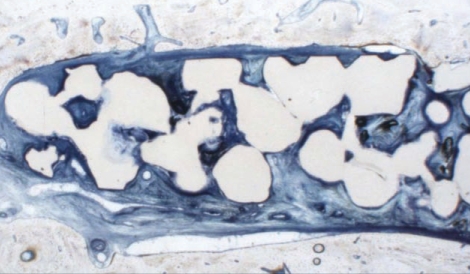
Fig. 5.
Medpor Craniotomy Gap Wedge implanted into the bone gap along the craniotomy flap; note the bony ingrowth into the implant (Vilanueva staining, original magnification ×10).
Several other materials can also be used to fill small bone defects. A methylmethacrylate can be easily applied, but produces a highly exothermic reaction and tissue injury during the curing process. Plus, it becomes encased in a fibrous capsule that demonstrates an inflammatory reaction with a foreign-body giant cell response. It does not allow for tissue incorporation and has been related to a significant infection rate. Meanwhile, hydroxyapatite and carbonated apatite cements are widely used due to their biocompatibility as a result of their osteoconductive property and easy usage. However, despite being easy to mix and contour to small bone defects, they also have important drawbacks, including a long setting time of up to 15 minutes (Bone-Source; Stryker Leibinger, Flint, MI, USA) and a tendency to be washed out in a wet field. Thus, meticulous hemostasis is essential to ensure a dry surgical field. Plus, there is a potential for postoperative resorption when a CSF leak is present9,11).
Although various preformed implants have already been devised for covering burr holes4,7,8,13), the Medpor Craniotomy Gap Wedge is devised to reconstruct bone gaps as well as burr holes. A major disadvantage of the implants is the high cost. Meanwhile, the design of the Medpor Craniotomy Gap Wedge needs to be further developed to optimize surgical handling.
CONCLUSION
The Medpor Craniotomy Gap Wedge is technically easy to work with for reconstructing small bone defects such as bone gaps and burr holes created by a craniotomy, and provides excellent cosmetic results.
References
- 1.Couldwell WT, Chen TC, Weiss MH, Fukushima T, Dougherty W. Cranioplasty with the Medpor porous polyethylene Flexblock implant. Technical note. J Neurosurg. 1994;81:483–486. doi: 10.3171/jns.1994.81.3.0483. [DOI] [PubMed] [Google Scholar]
- 2.Couldwell WT, Stillerman CB, Dougherty W. Reconstruction of the skull base and cranium adjacent to sinuses with porous polyethylene implant : preliminary report. Skull Base Surg. 1997;7:57–63. doi: 10.1055/s-2008-1058609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiMeco F, Li KW, Mendola C, Cantú G, Solero CL. Craniotomies without burr holes using an oscillating saw. Acta Neurochir (Wien) 2004;146:995–1001. doi: 10.1007/s00701-004-0322-4. discussion 1001. [DOI] [PubMed] [Google Scholar]
- 4.Dujovny M, Aviles A, Cuevas P. Bone-like polyethylene burr-hole cover. Neurol Res. 2005;27:333–334. doi: 10.1179/016164105X22138. [DOI] [PubMed] [Google Scholar]
- 5.Ferroli P, Franzini A, Marchetti M, Maccagnano E, Broggi G. Craniotomy using image-guided oscillating saw : technical note. Neurol Res. 2006;28:145–148. doi: 10.1179/016164106X98017. [DOI] [PubMed] [Google Scholar]
- 6.Frodel JL, Lee S. The use of high-density polyethylene implants in facial deformities. Arch Otolaryngol Head Neck Surg. 1998;124:1219–1223. doi: 10.1001/archotol.124.11.1219. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi S, Hara H, Okudera H, Takemae T, Sugita K. Usefulness of ceramic implants in neurosurgery. Neurosurgery. 1987;21:751–755. doi: 10.1227/00006123-198711000-00032. [DOI] [PubMed] [Google Scholar]
- 8.Koyama J, Hongo K, Iwashita T, Kobayashi S. A newly designed key-hole button. J Neurosurg. 2000;93:506–508. doi: 10.3171/jns.2000.93.3.0506. [DOI] [PubMed] [Google Scholar]
- 9.Mathur KK, Tatum SA, Kellman RM. Carbonated apatite and hydroxyapatite in craniofacial reconstruction. Arch Facial Plast Surg. 2003;5:379–383. doi: 10.1001/archfaci.5.5.379. [DOI] [PubMed] [Google Scholar]
- 10.Park J, Guthikonda M. The Medpor sheet as a sellar buttress after endonasal transsphenoidal surgery : technical note. Surg Neurol. 2004;61:488–492. doi: 10.1016/S0090-3019(03)00581-0. discussion 493. [DOI] [PubMed] [Google Scholar]
- 11.Poetker DM, Pytynia KB, Meyer GA, Wackym PA. Complication rate of transtemporal hydroxyapatite cement cranioplasties : a case series review of 76 cranioplasties. Otol Neurotol. 2004;25:604–609. doi: 10.1097/00129492-200407000-00031. [DOI] [PubMed] [Google Scholar]
- 12.Romano JJ, Iliff NT, Manson PN. Use of medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993;4:142–147. doi: 10.1097/00001665-199307000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Schantz JT, Lim TC, Ning C, Teoh SH, Tan KC, Wang SC, et al. Cranioplasty after trephination using a novel biodegradable burr hole cover : technical case report. Neurosurgery. 2006;58(1) Suppl:ONS-E176. doi: 10.1227/01.NEU.0000193533.54580.3F. discussion ONS-E176. [DOI] [PubMed] [Google Scholar]
- 14.Schessel DA, Rowed DW, Nedzelski JM, Feghali JG. Postoperative pain following excision of acoustic neuroma by the suboccipital approach : observations on possible cause and potential amelioration. Am J Otol. 1993;14:491–494. doi: 10.1097/00129492-199309000-00014. [DOI] [PubMed] [Google Scholar]