Abstract
Objective
This study was done to evaluate the correlation between carpal tunnel pressure (CTP), electrodiagnostic and ultrasonographic findings in patients with carpal tunnel syndrome (CTS).
Methods
CTP was measured during endoscopic carpal tunnel release (ECTR) for CTS using Spiegelberg ICP monitoring device with parenchymal type catheter. Neurophysiologic severity and nerve cross sectional area were evaluated using nerve conductive study and ultrasonography (USG) before ECTR in all patients.
Results
Tests were performed in a total of 48 wrists in 39 patients (9 cases bilateral). Maximum CTP was 56.7 ± 19.3 mmHg (Mean ± SD) and 7.4 ± 3.3 mmHg before and after ECTR, respectively. No correlation was found between maximum CTP and either neurophysiologic severity or nerve cross sectional area, whereas we found a significant correlation between the latter two parameters.
Conclusion
CTP was not correlated with neurophysiologic severity and nerve cross sectional area. Dynamic, rather than static, pressure in carpal tunnel might account for the basic pathophysiology of CTS better.
Keywords: Carpal tunnel syndrome, Pressure, Ultrasonography, Electrodiagnosis
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy. Combination of clinical findings with electrodiagnostic study is the most valid way of diagnosing CTS1,24). Since CTS is a compression neuropathy, the most direct evaluation tool would be the measurement of carpal tunnel pressure (CTP)21). Since the first report of CTP measurement using water-filled bulb, there have been many studies about CTP in patients having CTS, using various devices3,4,9,15,20,26,30). CTP was reported to be elevated in patients with CTS, ranging from 12 to 43 mmHg, while it was 5-14 mmHg in healthy subjects4,15,20,26,31,32). Elevated CTP in CTS has been reported to decrease to the normal range immediately after surgical release of the transverse carpal ligament19,27,28).
The nerve compression at carpal tunnel lead to functional change of the median nerve, which can be evaluated by nerve conductive study, i.e., focal slowing of nerve conduction velocity across the carpal tunnel1,5). Structural change has also known to occur in the median nerve, which can be assessed by ultrasonography (USG), i.e., swollen nerve in patients with CTS2,7,23). However, little is known about the relationship between CTP and functional/structural changes caused by elevated pressure. Therefore, this study was performed to investigate the relationship between CTP and the findings of electrodiagnostic and ultrasonographic studies.
MATERIALS AND METHODS
Patients and operative procedure
From November 2005 to May 2007, CTP was measured during operation for CTS. The patients were diagnosed by clinical symptoms and signs and confirmed by electrophysiological study. Patients with idiopathic CTS were included in study.
Endoscopic carpal tunnel release (ECTR) was done for patients who did not respond to conservative treatment or presented with thenar atrophy. All of the patients were operated on using Endocarp™ (Linvatec, Largo, FL, USA) under local anesthesia and with application of pneumatic tourniquet. The nature of the study was explained to all patients and informed consent for the pressure measurement was obtained from the patients. This study was approved by the institutional review board of our hospital.
Electorphysiologic study and ultrasonography
Nerve conductive studies (NCS) were performed before operation using standard techniques of surface stimulation and recording (Nicolet Viking IV, Madison, WI, USA), by one neurologist (YHH). Skin temperatures were maintained above 31.0℃. Median sensory nerve conduction velocity (SNCV) was orthodromically measured in the index finger-wrist segment, and the median distal motor latency from the wrist 5 cm proximal to the recording electrode at the abductor pollicis brevis. When these conventional tests yielded normal results, segmental (mixed nerve conduction with stimulation of mildpalm and recording at the wrist) or comparative studies (median/ulnar or median/radial comparisons) were performed. The severity of CTS was assessed based on the results of NCS using a previously reported neurophysiologic classification22).
USG of the carpal tunnel was performed before operation by one radiologist (YHK), unware of the clinical finding. The USG device was HDI 3000 (Philips, Nederland), Sequoia 512 (Acuson, Mountain View, CA, USA). A 2-6 MHz linear array transducer was used. Cross sectional area (CSA) of median nerve was measured using elliptical method at two points : one at mid-forearm, the other at just proximal to carpal tunnel, where the nerve swelling is most prominent. The absolute value of nerve area at just proximal to carpal tunnel and ratio of nerve swelling to mid-forearm was used for analysis.
Pressure measurement
Pressures were measured with Spiegelberg intracranial pressure (ICP) monitoring device connected to a parenchymal type catheter (B Braun Medical Inc, Germany). After dissection of subcutaneous fat, the ligament layer was identified and incised in transverse direction. The Endocarp cannula was inserted so that the distal end of cannula was located just distal to distal end of ligament using surface landmark. This position of cannula was confirmed by endoscope. The catheter was inserted through cannula into the carpal canal. The depth of insertion was usually 1 cm passed last marker of the catheter (D4). In some cases, initial depth of insertion was at the level of last marker of the catheter (D3), due to the difference in length of carpal tunnel. Then, the cannula was removed and pressure was measured. The pressure measured repeatedly with each 1 cm distraction of catheter until the proximal end of balloon was just visible (D2 and D1) (Fig. 1). Three or four point measurements were done. After division of transverse carpal ligament, the pressure was measured again as done before division of ligament. Pressure proximal to the initial incision of ligament was done with same method. P3 corresponds to D3, P2 to D2, and P1 to D1, respectively. Usually the measurement was done in two to three points.
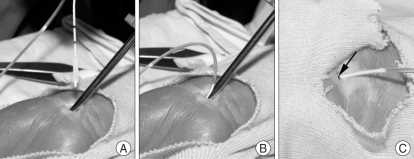
Fig. 1.
Steps of pressure measurement. After the cannula tip has been inserted to distal end of transverse carpal ligament, catheter is then inserted A : There are two marks, spaced 1 cm, each other, on the catheter. Then the catheter is inserted so that 1 cm passed after the second mark on the catheter B : Pressure is measured after the removal of cannula. Pressure at D3 is measured C : Note the second mark of the catheter (arrow).
Statistical analysis
Data were analyzed using a commercially available statistical soft ware package (SPSS for Windows, version 11.0, SPSS, Inc., Chicago, IL, USA). Correlation between NCS grade, USG finding and maximum pressure was analyzed with analysis of variance (ANOVA). Posthoc analyses were done using Tukey's HSD. Correlation between USG finding and maximum pressure was analyzed with linear regression. p value less than 0.05 was considered significant.
RESULTS
We measured preoperative and postoperative carpal tunnel pressure in 48 wrists from thirty-nine patients (18 Left hands, 30 Right hands). There were 35 females (7 cases bilateral) and four males (2 cases bilateral) aged 25 to 80 years (mean 55.5).
NCS and USG were done in all cases. NCS results were as follows : mild in 1 hand (2.1%), moderate in 14 (29.2%), severe in 18 (37.5%) and extreme in 15 (31.3%).
Mean of median nerve CSA was 0.062cm2 (range 0.04-0.09) at forearm, 0.16 (range 0.08-0.3) at just proximal to carpal tunnel. Mean of ratio of CSA was 2.63 (range 1.29-4.93).
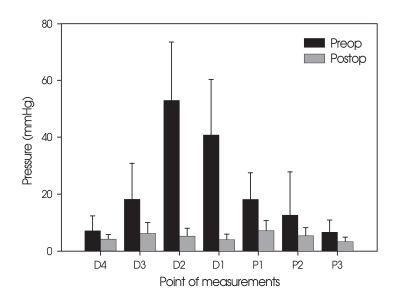
Before carpal tunnel release, mean of maximum pressure at distal to incision site was 56.7 mmHg (22.3 to 105) and mean of maximum pressure at proximal to incision site was 18.2 mmHg (5.5 to 34.1). There was a significance of difference in pressure between points of measurements before operation (Table 1).
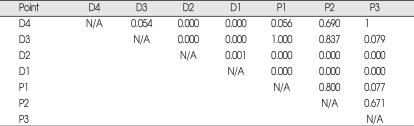
Table 1.
Significance of difference in pressure between points of measurements before operation (ANOVA)
After carpal tunnel release, mean of maximum pressure at distal to incision site was 7.4 mmHg (0.7 to 13.6) and mean of maximum pressure at proximal to incision site was 7.5 mmHg (1.9 to 13.4) (Fig. 2, Table 2).
Fig. 2.
Results of pressure measurements.
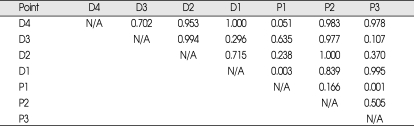
Table 2.
Significance of pressure change after operation
When the postoperative pressure was compared with the preoperative value, all of the measurement points except for proximal point 2 showed significant decrease (Table 2). The difference in pressure between measurement points, existed before operation, disappeared after operation (Table 3).
Table 3.
Significance of difference in pressure between points of measurements after operation (ANOVA)
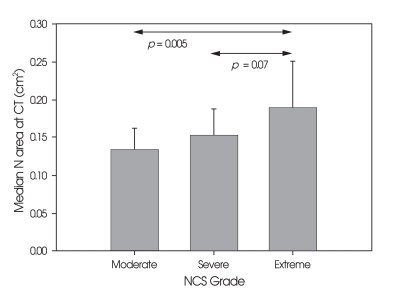
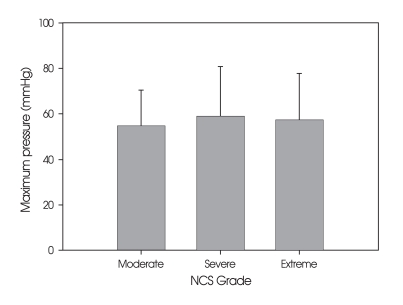
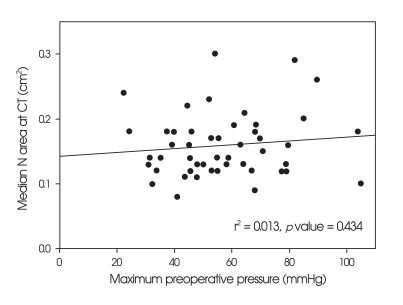
Relation between NCS grade, maximum preoperavtive pressure and median nerve swelling was investigated. One case with mild grade was excluded to make statistical analysis feasible. There was a statistically significant correlation between NCS and cross sectional median nerve area (p = 0.006, ANOVA) (Fig. 3). Nerve swelling ratio showed relationship of borderline significance with NCS grade (p = 0.061, ANOVA). There was no a statistical difference between NCS grade and maximum pressure (p = 0.795, ANOVA) (Fig. 4). Neither Cross sectional median nerve area at carpal tunnel nor the ratio of nerve swelling showed statistically significant correlation with maximum preoperative pressure (Fig. 5).
Fig. 3.
Difference in median nerve area at carpal tunnel according to nerve conductive studies grade.
Fig. 4.
Difference of pressure according to nerve conductive studies grade.
Fig. 5.
Scatterplot showing the correlation between maximum preoperative pressure and median nerve swelling at carpal tunnel.
DISCUSSION
As expected, the present study showed high CTPs in patients with CTS, which dropped significantly after carpal tunnel release. The measured pressure values before and after carpal tunnel release in this study were also comparable to those of previous studies18,21,28). Neurophysiologic severity was also highly correlated with nerve swelling assessed by USG, which is also in line with previous studies13,23). This suggests functional change correlates with anatomical change. However, we could not find any significant correlation between the CTP and either neurophysiologic severity nor USG findings.
Regarding the relationship between CTP and neurophysiologic severity, previous studies reported a significant correlation between them, suggesting that the increased pressure underlie the functional alteration of nerve conduction8,14). Our results, however, failed to show such a significant correlation, and the discrepancy is to be addressed in detail. First of all, there are several differences between the present study and previous ones in neurophysiologic study method and patient population included. The median nerve conduction was studied intraoperatively, but only the sensory nerve conduction was evaluated in 19 patients14). In another study, they compared the carpal canal pressure with the latency of sensory nerve potential8). Unlike previous studies, in the present investigation, the neurophysiologic severity was graded according to both motor and sensory nerve conductive studies. Furthermore, about two thirds of our patients did not show any sensory nerve potential in NCS (severe and extreme grade), indicating a vast majority of our patients had severe nerve dysfunction.
The real pathologic factor might be median nerve intraneural pressure, rather than CTP. There has been one report on direct measurement of intraneural pressure, which showed that there was strong correlation between intraneural pressure and CTP21). Therefore, if intraneural pressure would have had significant correlation, carpal tunnel pressure would have shown significant correlation, too. Various methods have been reported for CTP measurements, including ICP monitoring device, as in our series9). It is known that application of tourniquet do not affect the CTP29).
One possible explanation for the lack of correlation is the static versus dynamic pressure. We measured the static pressure in resting state with neutral wrist position. Pressure changes on wrist position, finger action, or repetitive hand activity suggest dynamic nerve compression might be a real causative factor in CTS, rather than static compression4,11,25,33).
The duration of nerve compression would be another factor in CTS pathogenesis. Duration, in addition to certain pressure level, might influence the functional and structural changes in the median nerve10). In chronic nerve compression disorder, such as CTS, the pressure might increase gradually over time according to structural change in carpal tunnel. Therefore, the pressure level would parallel with symptom duration. Besides, the exact assessment of duration is not easy in chronic nerve compression disorder.
It is known that USG reveals swelling of median nerve in CTS, helpful in diagnosis and severity evaluation12,13,17,23). There has been no report about the correlation between CTP and USG finding. Our data showed no significant correlation between the two, contrary to our expectation. Since it is known that CTP is related to neurophysiologic severity, we think that there might be a causal relationship between CTP and median nerve swelling, although not disclosed yet in this study.
It is known that the maximum point of compression is located in the central portion of carpal tunnel, where the pressure shows highest value6,14,16,29). It is suggested that nonuniform dimension of carpal tunnel may be the cause of this pressure profile15). It is notable that the pressure differences between measurements were disappeared after carpal tunnel release (Table 1, 3, Fig. 2), which meant reversal of abnormal anatomy of CTS back to normal condition. To our knowledge, the difference in pressure profile is evaluated statistically for the first time in this study.
One of the limitations of our study is the population of patients. The majority of our patients were in severe/extreme in NCS grade. This allowed us to evaluate the impact of NCS grade in only one side of spectrum, rather than all grades of neurophysiological severity.
Although our study doesn't show significant correlation between basic pathologic factor of CTS and resulting changes of median nerve, it is well known that the carpal tunnel pressure is elevated in CTS patients. Refining of pressure measurement technique might elucidate the correlation and clinical implications of carpal tunnel pressure in CTS.
CONCLUSION
Electrodiagnostic and anatomical changes showed a significant correlation, although the basic pathologic factor for these changes showed no significant correlation. The dynamic pressure measurements, rather than static, might be a better evaluation of basic pathology of CTS.
Acknowledgments
This work was supported by research grants from the Seoul National University Boramae Hospital.
References
- 1.Aroori S, Spence RA. Carpal Tunnel Syndrome. Ulster Med J. 2008;77:6–17. [PMC free article] [PubMed] [Google Scholar]
- 2.Bayrak IK, Bayrak AO, Tilki HE, Nural MS, Sunter T. Ultrasonography in carpal tunnel syndrome : comparison with electrophysiological stage and motor unit number estimate. Muscle Nerve. 2007;35:344–348. doi: 10.1002/mus.20698. [DOI] [PubMed] [Google Scholar]
- 3.Brain WR, Wright AD, Wilkinson M. Spontaneous compression of both median nerves in the carpal tunnel : six cases treated surgically. Lancet. 1947;1:277. doi: 10.1016/s0140-6736(47)90093-7. [DOI] [PubMed] [Google Scholar]
- 4.Gelberman RH, Hergenroeder PT, Hargens AR, Lundborg GN, Akeson WH. The carpal tunnel syndrome. A study of carpal canal pressures. J Bone Joint Surg Am. 1981;63:380–383. [PubMed] [Google Scholar]
- 5.Gelberman RH, Szabo RM, Williamson RV, Hargens AR, Yaru NC, Minteer-Convery MA. Tissue pressure threshold for peripheral nerve viability. Clin Orthop Relat Res. 1983:285–291. [PubMed] [Google Scholar]
- 6.Hashizume H, Nanba Y, Shigeyama Y, Hirooka T, Yokoi T, Inoue H. Endoscopic carpal tunnel pressure measurement : a reliable technique for complete release. Acta Med Okayama. 1997;51:105–110. doi: 10.18926/AMO/30783. [DOI] [PubMed] [Google Scholar]
- 7.Hobson-Webb LD, Massey JM, Juel VC, Sanders DB. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin Neurophysiol. 2008;119:1353–1357. doi: 10.1016/j.clinph.2008.01.101. [DOI] [PubMed] [Google Scholar]
- 8.Ikeda K, Osamura N, Tomita K. Segmental carpal canal pressure in patients with carpal tunnel syndrome. J Hand Surg Am. 2006;31:925–929. doi: 10.1016/j.jhsa.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Kanta M, Ehler E, Hosszú T, Danková C, Lastovicka D, Adamkov J, et al. [Measurement of carpal tunnel pressure during surgery of carpal tunnel syndrome.] Rozhl Chir. 2005;84:253–257. [PubMed] [Google Scholar]
- 10.Kaymak B, Ozçakar L, Cetin A, Candan Cetin M, Akinci A, Hascelik Z. A comparison of the benefits of sonography and electrophysiologic measurements as predictors of symptom severity and functional status in patients with carpal tunnel syndrome. Arch Phys Med Rehabil. 2008;89:743–748. doi: 10.1016/j.apmr.2007.09.041. [DOI] [PubMed] [Google Scholar]
- 11.Keir PJ, Bach JM, Rempel D. Effects of computer mouse design and task on carpal tunnel pressure. Ergonomics. 1999;42:1350–1360. doi: 10.1080/001401399184992. [DOI] [PubMed] [Google Scholar]
- 12.Koyuncuoglu HR, Kutluhan S, Yesildag A, Oyar O, Guler K, Ozden A. The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electrodiagnostic tests. Eur J Radiol. 2005;56:365–369. doi: 10.1016/j.ejrad.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Lee CH, Kim TK, Yoon ES, Dhong ES. Correlation of high-resolution ultrasonographic findings with the clinical symptoms and electrodiagnostic data in carpal tunnel syndrome. Ann Plast Surg. 2005;54:20–23. doi: 10.1097/01.sap.0000141942.27182.55. [DOI] [PubMed] [Google Scholar]
- 14.Luchetti R, Schoenhuber R, Alfarano M, Deluca S, De Cicco G, Landi A. Carpal tunnel syndrome : correlations between pressure measurement and intraoperative electrophysiological nerve study. Muscle Nerve. 1990;13:1164–1168. doi: 10.1002/mus.880131211. [DOI] [PubMed] [Google Scholar]
- 15.Luchetti R, Schoenhuber R, De Cicco G, Alfarano M, Deluca S, Landi A. Carpal-tunnel pressure. Acta Orthop Scand. 1989;60:397–399. doi: 10.3109/17453678909149305. [DOI] [PubMed] [Google Scholar]
- 16.Luchetti R, Schoenhuber R, Nathan P. Correlation of segmental carpal tunnel pressures with changes in hand and wrist positions in patients with carpal tunnel syndrome and controls. J Hand Surg Br. 1998;23:598–602. doi: 10.1016/s0266-7681(98)80009-0. [DOI] [PubMed] [Google Scholar]
- 17.Nakamichi K, Tachibana S. Ultrasonographic measurement of median nerve cross-sectional area in idiopathic carpal tunnel syndrome : Diagnostic accuracy. Muscle Nerve. 2002;26:798–803. doi: 10.1002/mus.10276. [DOI] [PubMed] [Google Scholar]
- 18.Nakao E, Short WH, Werner FW, Fortino MD, Palmer AK. Changes in carpal tunnel pressures following endoscopic carpal tunnel release : a cadaveric study. J Hand Surg Am. 1998;23:43–47. doi: 10.1016/S0363-5023(98)80087-7. [DOI] [PubMed] [Google Scholar]
- 19.Okutsu I, Hamanaka I, Chiyokura Y, Miyauchi Y, Sugiyama K. Intraneural median nerve pressure in carpal tunnel syndrome. J Hand Surg Br. 2001;26:155–156. doi: 10.1054/jhsb.2000.0534. [DOI] [PubMed] [Google Scholar]
- 20.Okutsu I, Ninomiya S, Hamanaka I, Kuroshima N, Inanami H. Measurement of pressure in the carpal canal before and after endoscopic management of carpal tunnel syndrome. J Bone Joint Surg Am. 1989;71:679–683. [PubMed] [Google Scholar]
- 21.Okutsu I, Ninomiya S, Yoshida A, Hamanaka I, Kitajima I. Measurement of carpal canal and median nerve pressure in patients with carpal tunnel syndrome. Tech Hand Up Extrem Surg. 2004;8:124–128. doi: 10.1097/01.bth.0000127362.60294.92. [DOI] [PubMed] [Google Scholar]
- 22.Padua L, LoMonaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997;96:211–217. doi: 10.1111/j.1600-0404.1997.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 23.Padua L, Pazzaglia C, Caliandro P, Granata G, Foschini M, Briani C, et al. Carpal tunnel syndrome : ultrasound, neurophysiology, clinical and patient-oriented assessment. Clin Neurophysiol. 2008;119:2064–2069. doi: 10.1016/j.clinph.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Park SK, Lee JH, Lee HG, Ryu KY, Kang DG, Kim SC. Predictive value of sensory nerve conduction in carpal tunnel syndrome. J Korean Neurosurg Soc. 2006;40:401–405. [Google Scholar]
- 25.Rempel D, Bach JM, Gordon L, So Y. Effects of forearm pronation/supination on carpal tunnel pressure. J Hand Surg Am. 1998;23:38–42. doi: 10.1016/S0363-5023(98)80086-5. [DOI] [PubMed] [Google Scholar]
- 26.Rojviroj S, Sirichativapee W, Kowsuwon W, Wongwiwattananon J, Tamnanthong N, Jeeravipoolvarn P. Pressures in the carpal tunnel. A comparison between patients with carpal tunnel syndrome and normal subjects. J Bone Joint Surg Br. 1990;72:516–518. doi: 10.1302/0301-620X.72B3.2187880. [DOI] [PubMed] [Google Scholar]
- 27.Sanz J, Lizaur A, Sánchez Del Campo F. Postoperative changes of carpal canal pressure in carpal tunnel syndrome : a prospective study with follow-up of 1 year. J Hand Surg Br. 2005;30:611–614. doi: 10.1016/j.jhsb.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 28.Schuind F. Canal pressures before, during, and after endoscopic release for idiopathic carpal tunnel syndrome. J Hand Surg Am. 2002;27:1019–1025. doi: 10.1053/jhsu.2002.36541. [DOI] [PubMed] [Google Scholar]
- 29.Sekiya H, Sugimoto N, Kariya Y, Hoshino Y. Carpal tunnel pressure in patients with carpal tunnel syndrome due to long-term hemodialysis. Int Orthop. 2002;26:274–277. doi: 10.1007/s00264-002-0366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Szabo RM, Chidgey LK. Stress carpal tunnel pressures in patients with carpal tunnel syndrome and normal patients. J Hand Surg Am. 1989;14:624–627. doi: 10.1016/0363-5023(89)90178-0. [DOI] [PubMed] [Google Scholar]
- 31.Szabo RM, Gelberman RH, Williamson RV, Hargens AR. Effects of increased systemic blood pressure on the tissue fluid pressure threshold of peripheral nerve. J Orthop Res. 1983;1:172–178. doi: 10.1002/jor.1100010208. [DOI] [PubMed] [Google Scholar]
- 32.Werner CO, Elmqvist D, Ohlin P. Pressure and nerve lesion in the carpal tunnel. Acta Orthop Scand. 1983;54:312–316. doi: 10.3109/17453678308996576. [DOI] [PubMed] [Google Scholar]
- 33.Werner R, Armstrong TJ, Bir C, Aylard MK. Intracarpal canal pressures : the role of finger, hand, wrist and forearm position. Clin Biomech (Bristol, Avon) 1997;12:44–51. doi: 10.1016/s0268-0033(96)00044-7. [DOI] [PubMed] [Google Scholar]