Abstract
BACKGROUND
The burden of hypertension and related health care needs among Mexican Americans will likely increase substantially in the near future.
OBJECTIVES
In a nationally representative sample of U.S. Mexican American adults we examined: 1) the full range of blood pressure categories, from normal to severe; 2) predictors of hypertension awareness, treatment and control and; 3) prevalence of comorbidities among those with hypertension.
DESIGN
Cross-sectional analysis of pooled data from the National Health and Nutrition Examination Surveys (NHANES), 1999–2004.
PARTICIPANTS
The group of participants encompassed 1,359 Mexican American women and 1,421 Mexican American men, aged 25–84 years, who underwent a standardized physical examination.
MEASUREMENTS
Physiologic measures of blood pressure, body mass index, and diabetes. Questionnaire assessment of blood pressure awareness and treatment.
RESULTS
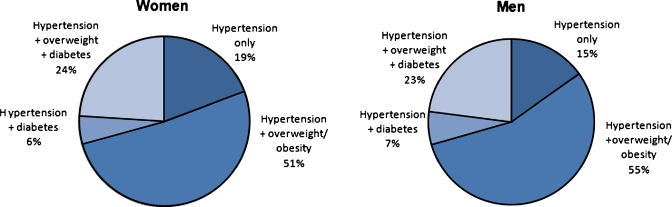
Prevalence of Stage 1 hypertension was low and similar between women and men (∼10%). Among hypertensives, awareness and treatment were suboptimal, particularly among younger adults (65% unaware, 71% untreated) and those without health insurance (51% unaware, 62% untreated). Among treated hypertensives, control was suboptimal for 56%; of these, 23% had stage ≥2 hypertension. Clustering of CVD risk factors was common; among hypertensive adults, 51% of women and 55% of men were also overweight or obese; 24% of women and 23% of men had all three chronic conditions-hypertension, overweight/obesity and diabetes.
CONCLUSION
Management of hypertension in Mexican American adults fails at multiple critical points along an optimal treatment pathway. Tailored strategies to improve hypertension awareness, treatment and control rates must be a public health priority.
KEY WORDS: Mexican American, hypertension, health care, practice patterns, secondary prevention
INTRODUCTION
Hypertension is the most prevalent modifiable risk factor for cardiovascular disease (CVD) among U.S. adults (29%)1, surpassing the prevalence of smoking, obesity and diabetes.2 Although the benefits of blood pressure treatment and control on cardiac and cerebrovascular outcomes are well-established,3,4 more than one-third of U.S. adults who have been diagnosed with hypertension are untreated1 and two-thirds have inadequate blood pressure control.5 Racial/ethnic differences in hypertension prevalence, awareness, treatment and control are well documented 1,5–7. Of particular concern are the lower rates of blood pressure treatment and control that have consistently been observed among Mexican Americans than among non-Hispanic whites and African Americans.
The burden of hypertension and related health care needs among Mexican Americans are likely to increase in the near future for several reasons. First, the Hispanic population, the large majority of whom is Mexican American, is the fastest growing ethnic minority population in the United States and is expected to grow 188% between 2000 and 20508. The numbers of older Mexican Americans are growing particularly fast9; it is this age group that has the highest burden of hypertension10 and is most likely to need health care for hypertension-related complications. Second, Mexican Americans are disproportionately uninsured (49% of foreign-born Mexican Americans and 21% of U.S. born Mexican Americans are uninsured)11 so they are less likely to receive preventive treatment. Finally, Mexican Americans are more likely to be overweight12–14 and have diabetes15 than non-Hispanic whites. Patients with such comorbidities constitute a large percentage of patients treated for cardiovascular and other chronic diseases.16
Most epidemiological studies of hypertension among Mexican Americans have been descriptive, estimating hypertension prevalence, awareness, treatment and control.6 Few studies have examined correlates of hypertension awareness, treatment and control7,17,18, knowledge that is critical to identifying and appropriately treating higher risk subgroups. Furthermore, almost all previous studies have focused on only two categories of blood pressure status- normotensives and hypertensives, without further examining a range of hypertension categories that includes prehypertensives as well as stage 1 and stage 2 hypertensives. This further examination can provide important and more refined indicators of hypertension control and indicators of the effectiveness of clinical and public health efforts. Lastly, to our knowledge, few or no national studies have examined the prevalence of comorbidities among hypertensive Mexican Americans that can contribute an additional dimension to their cardiovascular disease risk profile.
The following are therefore the objectives of this paper: 1) to examine the full range of blood pressure categories, from normal to severe among Mexican American women and men using pooled data from a national U.S. sample of NHANES, 1999–2004; 2) to examine correlates of hypertension awareness, treatment and control and; 3) to estimate the prevalence of comorbidities among those with hypertension. Our objective is to better define the processes that contribute to poor blood pressure control among Mexican American patients; Mexican American subgroups most in need of clinical and public health interventions; and, the level of cardiovascular disease risk among Mexican Americans.
METHODS
Sample
Data are from the 1999–2004 National Health and Nutrition Examination Surveys (NHANES), a nationally representative sample of the civilian, non-institutionalized U.S. population that uses a stratified multistage probability design and oversamples Mexican Americans. Our study sample included non-pregnant Mexican American adults (aged 25–84 years) who underwent a standardized physical examination. The overall response rates for the physical examination was 77% (rates are unavailable for specific ethnic groups).19
Ethnicity
NHANES respondents were asked to classify their race/ethnicity as black; Mexican or Mexican American; white; Asian or Pacific Islander; Aleut, Eskimo or American Indian; or other Latin-American or other Spanish. Adults who selected Mexican or Mexican-American were included in our analyses.
Primary Outcome
Hypertension status, awareness, treatment, and control were the primary outcomes and were defined in accordance with the Joint National Committee on Prevention, Evaluation, and Treatment of High Blood Pressure.20 Prehypertension was defined as systolic blood pressure (SBP) 120–139 mm Hg or diastolic blood pressure (DBP) 80–89 mm Hg. Hypertension was defined as SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg or on antihypertensive medications. Individuals with hypertension were further classified as having Stage 1 hypertension (SBP 140–159 or DBP 90–99) or Stage ≥2 hypertension (SBP ≥ 160 or DBP ≥ 100). We report the mean of the second and third of three blood pressure readings, measured on the right arm by a physician while the participant was seated during the medical examination.
Hypertensive individuals who responded positively to the question, “Have you ever been told you had hypertension?” were classified as aware. Hypertensive individuals who responded positively to the question, “Because of your high blood pressure are you now taking prescribed medication?” were classified as being treated for hypertension. Treated individuals whose SBP was <140 mm Hg and DBP was <90 mm Hg were classified as having controlled blood pressure. Hypertension control for diabetic individuals was defined as SBP < 130 mm Hg and DBP < 80 mm Hg. Given the high prevalence of uncontrolled blood pressure among treated Mexican American adults, we also were interested in classifying control using a more liberal cutpoint (SBP <160 mmHg and DBP <100 mmHg); this allowed us also to estimate percent of treated individuals with stage ≥2 hypertension.
Sociodemographic Variables
Age in years, sex, country of birth (Mexico or United States), primary language spoken at home (English or Spanish), education (<high school, a high school degree, >high school), and health insurance status (none, private, government Medicaid) were used to predict hypertension awareness, treatment and control.
Comorbidities
Individuals were classified as normal weight (BMI of 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), obese (BMI ≥ 30 kg/m2) or morbidly obese (≥40 kg/m2). Individuals using insulin or diabetes medications or with a fasting plasma glucose ≥126 mg/dL were classified as diabetic.21 Fasting plasma glucose levels were determined using a microadaptation of the national glucose oxidase reference method.22
Statistical Analysis
Separate logistic regression equations were conducted to assess the independent association of hypertension awareness, treatment, and control and severely uncontrolled hypertension with sociodemographic factors, including sex, country of birth, primary language spoken, education and health insurance. BMI was added as a further independent variable to allow for the examination of the influence of sociodemographic factors above and beyond BMI. When poverty income ratio was added as an additional independent variable in an ancillary analysis, the results were very similar and did not account for variability in a meaningful way. The analyses used SAS Survey Procedures (version 9.1.3, SAS Institute Inc, Cary, North Carolina) that account for the complex, stratified multistage probability cluster sampling design used in NHANES. All analyses incorporated sampling weights that adjusted for unequal probabilities of selection.
RESULTS
The pooled sample sizes for Mexican Americans in NHANES 1999–2004 were 1359 for women and 1421 for men (Table 1). The sample was evenly distributed among the age groups, and the majority of the sample was born in Mexico and reported speaking primarily Spanish. Overall, educational attainment was low; 63% of women and 65% of men had not completed high school. Approximately 30% had no health insurance, 40% reported having private insurance and 10% reported that they received Medicaid.
Table 1.
Sample Sizes by Sociodemographic Characteristics and Health Insurance Status: Mexican-American Women and Men, Ages 25–84, NHANES 1999–2004, Unweighted Data
| Women ( = 1359) | Men ( = 1421) | |||
|---|---|---|---|---|
| % | % | |||
| Age | ||||
| 25–34 y | 246 | 18.1 | 318 | 22.4 |
| 35–44 y | 290 | 21.3 | 296 | 20.8 |
| 45–54 y | 232 | 17.1 | 215 | 15.1 |
| 55–64 y | 232 | 17.1 | 243 | 17.1 |
| 65–74 y | 259 | 19.0 | 244 | 17.2 |
| 75–84 y | 100 | 7.4 | 105 | 7.4 |
| Country of birth | ||||
| Mexico (%) | 746 | 54.9 | 843 | 59.3 |
| US (%) | 613 | 45.1 | 578 | 40.7 |
| Primary language spoken | ||||
| Spanish (%) | 951 | 70.1 | 1039 | 73.1 |
| English (%) | 406 | 29.9 | 382 | 26.9 |
| Education | ||||
| < High school (%) | 848 | 62.5 | 923 | 65.1 |
| High school degree (%) | 206 | 15.2 | 220 | 15.5 |
| > High school (%) | 303 | 22.3 | 276 | 19.4 |
| Health insurance | ||||
| None (%) | 423 | 31.1 | 498 | 35.1 |
| Private (%) | 545 | 40.1 | 605 | 42.6 |
| Medicaid (%) | 139 | 10.2 | 88 | 6.2 |
| Other (%) | 252 | 18.6 | 230 | 16.1 |
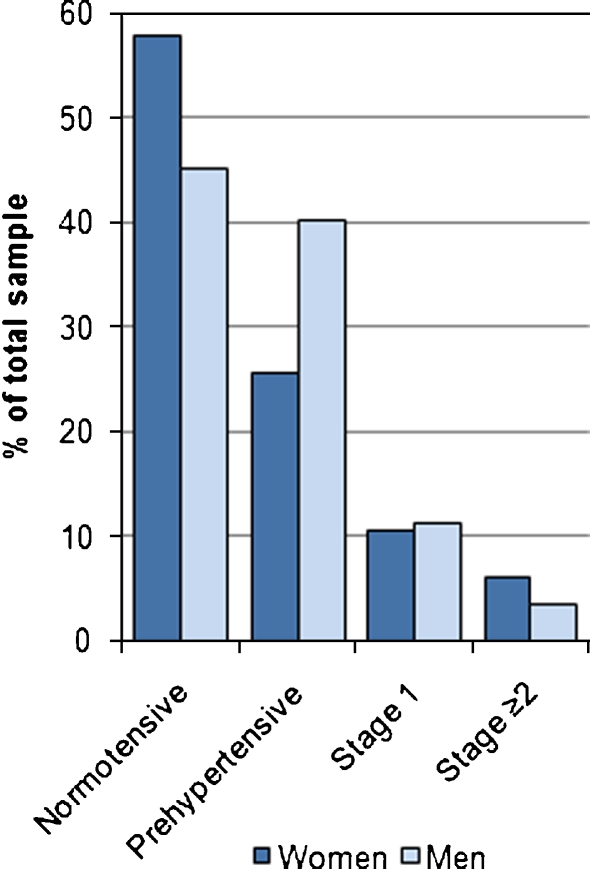
Figure 1 presents the distribution of blood pressure categories among the sample. Although more women than men were normotensive (58% of women compared with 45% of men), fewer women than men were prehypertensive (26% of women compared with 40% of men). The large numbers of both women and men who were prehypertensive, and therefore at risk of becoming hypertensive, illustrate the importance of distinguishing prehypertensives from normotensives. While the prevalence of Stage 1 hypertension was similar between women and men (approximately 10%), more women (6%) than men (4%) were classified as having Stage ≥2 hypertension.
Figure 1.
Distribution of blood pressure categories by sex: NHANES 1999–2004. Normotensive: <120 mmHg and <80 mmHg, Prehypertensive: 120–139 mmHg or 80–89 mmHg, Stage 1 Hypertension 140–159 mmHg or 90–99 mmHg, Stage ≥2 Hypertension ≥160 or ≥100 mmHg.
Overall, 59% of women and men were aware that they were hypertensive; the prevalence of awareness, however, differed significantly by age, country of birth, and health insurance status (Table 2). Younger Mexican Americans (25–34 year olds) were significantly less likely to be aware of their hypertension than older Mexican Americans (75–84 year olds) (35% vs. 72%, respectively, OR = 5.5, p < 0.001). Those born in U.S. were significantly less likely to be aware of their hypertension than those born in Mexico (54% vs. 65%, respectively; OR = 1.7, p < 0.05). Mexican Americans with no health insurance were significantly less likely to be aware of their hypertension than Medicaid recipients (49% vs. 70%, respectively; OR = 3.0, p < 0.005).
Table 2.
Predictors of Hypertension Awareness and Treatment among Mexican-American Adults, Ages 25–84, NHANES 1999–2004, Weighted Data
| Aware of hypertension among hypertensives 59% aware | Treated for hypertension among hypertensives 50% treated | |||||
|---|---|---|---|---|---|---|
| Odds ratio | (95% CI) | Predicted prevalence (%) | Odds ratio | (95% CI) | Predicted prevalence (%) | |
| Gender | ||||||
| Women | 1 | 60 | 1 | 53 | ||
| Men | 0.9 | (0.6–1.4) | 59 | 0.8 | (0.5–1.0) | 47 |
| Age | ||||||
| 25–34 y | 1 | 35 | 1 | 29 | ||
| 35–44 y | 1.7 | (0.7–3.9) | 47 | 0.9 | (0.3–2.9) | 26 |
| 45–54 y | 4.3 | (1.4–13.1) | 66* | 3.9 | (1.1–13.5) | 57* |
| 55–64 y | 5.7 | (2.3– 14.6) | 72** | 5.2 | (1.6–16.8) | 64** |
| 65–74 y | 4.4 | (1.7–11.4) | 67** | 5.4 | (1.7–16.7) | 65** |
| 75–84 y | 5.5 | (1.7– 17.5) | 72** | 4.4 | (1.2–16.1) | 60** |
| Country of birth | ||||||
| Mexico | 1 | 54 | 1 | 48 | ||
| US | 1.7 | (1.1–2.8) | 65* | 1.2 | (0.9–1.7) | 52 |
| Primary language spoken | ||||||
| Spanish | 1 | 63 | 1 | 53 | ||
| English | 0.7 | (0.4–1.3) | 57 | 0.8 | (0.5–1.3) | 48 |
| Education | ||||||
| < High school | 1 | 60 | 1 | 47 | ||
| High school degree | 0.8 | (0.5–1.3) | 55 | 1.2 | (0.8–1.7) | 51 |
| > High school | 1.3 | (0.7–2.3) | 64 | 1.4 | (0.9–2.2) | 54 |
| Health insurance | ||||||
| None | 1 | 49 | 1 | 38 | ||
| Private | 1.7 | (1.1–2.6) | 60* | 1.6 | (1.1–2.5) | 49* |
| Medicaid | 3 | (1.6–5.3) | 70** | 3.1 | (1.7–5.8) | 63** |
* P < 0.05
** P < 0.01
Of Mexican Americans who were aware of their hypertension, 50% reported that they were being treated with anti-hypertensive medications. Again, age and health insurance status distinguished higher risk groups. Fewer than 30% of younger Mexican Americans (25–34, and 35–44 years old) and fewer than 40% of those with no health insurance were treated for hypertension compared with their respective counterparts.
Control also was suboptimal among 56% of treated hypertensives; moreover, 23% of treated hypertensives continued to have Stage ≥2 hypertension (≥160 SBP mmHg and/or ≥100 DBP mmHg) (Table 3). Women had significantly lower control rates than men (38% vs. 49%, respectively; OR = 1.7, p < 0.001). Uncontrolled Stage ≥2 hypertension was observed among 23% of individuals treated for hypertension. Women were significantly more likely to have uncontrolled Stage ≥2 hypertension than men (27% vs. 18%, respectively; OR = 1.7, p < 0.05). Mexican Americans with no health insurance also were significantly more likely to have uncontrolled severe hypertension than Medicaid recipients (26% vs. 15%, respectively; OR = 2.0, p < 0.05).
Table 3.
Predictors of Hypertension Control among Mexican-American Adults, Ages 25–84, NHANES 1999–2004, Weighted Data
| Controlled hypertension (stage 1) among treated hypertensives† 44% controlled | Controlled hypertension (stage 2) among treated hypertensives‡ 77% controlled | |||||
|---|---|---|---|---|---|---|
| Odds ratio | (95% CI) | Predicted prevalence (%) | Odds ratio | (95% CI) | Predicted prevalence (%) | |
| Gender | ||||||
| Women | 1 | 38 | 1 | 73 | ||
| Men | 1.7 | (1.2–2.4) | 49** | 1.7 | (1.2–2.4) | 82* |
| Age | ||||||
| 25–34 y | 1 | 53 | 1 | 72 | ||
| 35–44 y | 1 | (0.1–7.3) | 53 | 1.7 | (0.1–8.4) | 80 |
| 45–54 y | 1.4 | (0.2–12.3) | 61 | 4.8 | (0.5–9.4) | 92 |
| 55–64 y | 0.4 | (0.1–3.2) | 33 | 1.3 | (0.2–6.4) | 75 |
| 65–74 y | 0.4 | (0.1–3.8) | 32 | 1.4 | (0.1–6.9) | 77 |
| 75–84 y | 0.3 | (0.1–3.3) | 28 | 1.1 | (0.1–5.3) | 72 |
| Country of birth | ||||||
| Mexico | 1 | 42 | 1 | 81 | ||
| US | 1.1 | (0.8–1.5) | 45 | 0.7 | (0.5–1.0) | 75 |
| Primary language spoken | ||||||
| Spanish | 1 | 46 | 1 | 74 | ||
| English | 0.8 | (0.5–1.2) | 41 | 1.5 | (0.9–2.5) | 81 |
| Education | ||||||
| < High school | 1 | 44 | 1 | 76 | ||
| High school degree | 0.9 | (0.5–1.5) | 41 | 1.9 | (0.9–3.9) | 84 |
| > High school | 1.1 | (0.6–2.0) | 46 | 0.9 | (0.4–1.7) | 74 |
| Health insurance | ||||||
| None | 1 | 40 | 1 | 74 | ||
| Private | 1.3 | (1.0–1.7) | 47* | 1.6 | (0.9–2.7) | 81 |
| Medicaid | 1.2 | (0.6–2.4) | 45 | 2 | (1.0–3.9) | 85* |
* P < 0.05
** P < 0.01
† Stage 1 control = SBP < 140 mmHg and DBP < 90 mmHg
‡ Stage 2 control = SBP < 160 mmHg and DBP < 100 mmHg
Because clustering of risk factors increases an individual’s overall risk of cardiovascular disease morbidity and mortality, we estimated the prevalence of comorbidities among those with hypertension to show the current burden of disease (Fig. 2). Only 19% of women and 15% of men had hypertension without being overweight/obese and/or diabetic. Fifty-one percent of women and 55% of men who were hypertensive were also overweight or obese but not diabetic. Most striking, 24% of women and 23% of men had all three chronic conditions-hypertension, overweight/obesity and diabetes
Figure 2.
Percent of hypertensive Mexican-American women and men, ages 25–84, with comorbidities: NHANES 1999–2004.
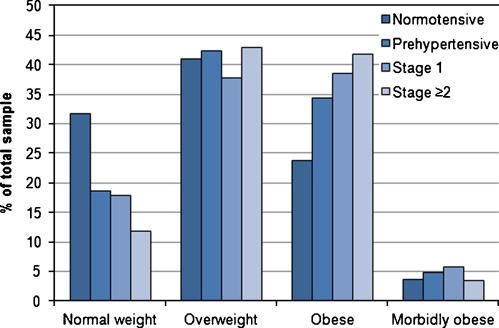
The distributions of body mass index categories by the four blood pressure categories are shown in Figure 3. The proportion of individuals classified as obese increased with each progressive stage of hypertension; 24% of normotensives were classified as obese compared with 42% among Stage ≥2 hypertensives.
Figure 3.
Distribution of body mass index categories by blood pressure categories. Normal weight: BMI <25 kg/m2; Overweight: BMI 25–29.9 kg/m2; Obese: BMI ≥30 kg/m2; Morbidly obese: BMI ≥40 kg/m2.
DISCUSSION
These findings from a nationally representative sample of 2,780 Mexican American adults offer insight into hypertension detection, management and control needs for Mexican American women and men. Previous studies have shown that blood pressure control among treated Mexican Americans is suboptimal.5–7,23 Our results build on this finding by presenting the severity of uncontrolled blood pressure and its correlates. Only 44% of treated hypertensives achieved control (BP < 140/90 mmHg); the remaining 56% had uncontrolled hypertension. Perhaps more striking, 23% of treated adults had Stage ≥2 hypertension (BP ≥ 160/100 mmHg), indicative of more severe blood pressure dysregulation. This finding highlights a substantial problem with the quality and intensity of treatment provided to Mexican Americans that negatively affects the health status of Mexican Americans by increasing their risk of cardiac and cerebrovascular adverse outcomes.
Poor blood pressure control among Mexican Americans is of particular concern given the high prevalence of comorbidities. Among hypertensives, 51% of women and 55% of men were overweight or obese but not diabetic; and 24% of women and 23% of men were overweight/obese and also had diabetes. This clustering of chronic disease risk factors likely compromises efforts to control hypertension.12–14,24,25 In addition, this clustering suggests the clinical need to coordinate efforts to manage those patients with multiple risk factors, particularly in facilitating a comprehensive clinical approach. Given the potential role of dietary and physical activity in managing hypertension, diabetes and obesity/overweight, these lifestyle strategies may be especially important adjuncts to pharmacotherapy.26–29 This clustering also emphasizes the need for long-term preventive strategies to prevent these conditions. Improved control is also important among Mexican Americans as both obesity and diabetes are projected to increase at a faster rate among Mexican Americans than non-Hispanic whites.30,31 The effect of obesity and diabetes may be compounded by a decline in positive health behaviors among Latinos,32,33 and Mexican American men may be at elevated risk.34
Although control rates were similar between younger and older Mexican Americans (a surprising finding given the difficulty of achieving control among older individuals), younger Mexican Americans had significantly lower rates of hypertension awareness and treatment than older Mexican Americans. This is likely to translate into lower control rates and a higher burden of cardiovascular disease as younger Mexican Americans enter higher risk ages. Since a worse prognosis, in terms of both morbidity and mortality, is associated with an earlier onset of hypertension35,36, age-specific approaches that are both public health and clinician-driven should be considered to minimize the burden of hypertension among younger Mexican Americans.
Consistent with earlier findings37, the prevalence of prehypertension among Mexican American adults was high (40.1% among men and 25.5% among women). Substantial evidence demonstrates that prehypertension is associated with an elevated risk for cardiovascular disease.38,39 Furthermore, the probability of progressing from prehypertension to hypertension is several fold higher than the probability of progressing from normal blood pressure to hypertension.40,41 These statistics underscore the importance of reporting the distribution of blood pressure categories given that the more common practice of reporting normotensive vs. hypertensives may underestimate cardiovascular disease risk.
Medicaid recipients had significantly higher rates of hypertension awareness, treatment and control than those with no health insurance, suggesting that insurance status plays an important role in hypertension management. Previous studies have shown that Medicaid patients are 126% more likely to be prescribed anti-hypertension medication than uninsured participants.42 Insurance status also may partially explain the particularly low rates of hypertension awareness observed among Mexican Americans born in Mexico. Data indicate this group was more than twice as likely to be uninsured than those born in the U.S.11 Although Mexican Americans born in Mexico had similar rates of hypertension treatment and control, it is possible that their level of cardiovascular disease risk was underestimated in this study since they did not contribute to the population analyzed for rates of treatment or control.
An important strength of this study is its use of a large nationally representative sample of Mexican American women and men that allowed us to examine a specific ethnic group and its subgroups rather than a broader, mixed group of Latinos. Previous studies have shown that health characteristics, including rates of hypertension, differ substantially between Mexican Americans and other Latino groups, including Cubans and Puerto Ricans.43,44 An additional strength of this study is that the NHANES medical examination is conducted by a physician, and health data (blood pressure, BMI and blood glucose levels) are based on physiologic measures. The specificity of a Mexican American sample and the in-person survey and medical assessment contrasts to the data collected by the BRFSS where Mexican Americans are not distinguished from other Latino populations and where information is obtained via telephone survey.45
Some limitations warrant discussion. First, the NHANES measure of hypertension awareness and use of current antihypertensive medications is based on self-report (as are most health surveys). As a result, estimates of awareness and treatment, and therefore control, may be biased. However, there is no evidence to suggest that the bias would be differential across subgroups. Second, differential non-response to the physical examination could have biased estimates of hypertension prevalence, awareness, treatment and control. Although it is possible that sicker individuals were less likely to undergo the physical exam, a recent analysis showed that NHANES participants who initially refused the physical examination were not significantly different from those who participated in their rates of hypertension or obesity, two primary health outcomes assessed in our study46.
IMPLICATIONS AND CONCLUSIONS
Our finding that Stage 1 and Stage ≥2 hypertension is prevalent among treated hypertensives shows that the management of hypertension in Mexican Americans fails at multiple critical points along an optimal treatment pathway. The proportion of hypertensive individuals who were aware of their hypertension exceeded the proportion of those being treated by more than 10%. This discrepancy may result when patients do not accept or continue therapy because of misconceptions about the use and/or value of medicines; adverse effects of medications; or health care access, language or economic barriers. In addition, physicians may not reinitiate discontinued therapy or may not communicate the usual lifelong need for pharmacotherapy. Even among those individuals whose hypertension is treated, the likelihood of adequate treatment is suboptimal. Contributors to this may include the failure to escalate medication dosage, failure to prescribe multiple medications, and incomplete patient adherence to medication taking. Results from this study suggest that to prevent cardiovascular complications among Mexican Americans, strategies to improve control rates must be a public health priority.
Acknowledgments
The authors thank Dr. David Ahn for his statistical and analytical expertise and Alana Koehler for her technical assistance in preparing the tables and figures. This research was supported by Public Health Service Training Grants T32 HL 07034 (AB) and K24 HL 086703 (RSS), both from the National Heart, Lung, and Blood Institute. This project was also supported by the Network for Multicultural Research on Health and Healthcare, Dept. of Family Medicine - UCLA David Geffen School of Medicine, funded by the Robert Wood Johnson Foundation.
References
- 1.Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007;49(1):69–75. [DOI] [PubMed]
- 2.Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 2003;290(7):891–7. [DOI] [PubMed]
- 3.Neal B, MacMahon S, Chapman N; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. The Lancet 2000;356(9246):1955–64. [DOI] [PubMed]
- 4.Wong ND, Thakral G, Franklin SS, L'Italien GJ, Jacobs MJ, Whyte JL, et al. Prevention and rehabilitation: preventing heart disease by controlling hypertension: impact of hypertensive subtype, stage, age, and sex. American Heart Journal 2003;145(5):888–95. [DOI] [PubMed]
- 5.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 2003;290(2):199–206. [DOI] [PubMed]
- 6.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension 2008;52(5):818–27. [DOI] [PubMed]
- 7.He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162(9):1051–8. [DOI] [PubMed]
- 8.US Census Bureau. 2008 National Population Projections. 2008 [cited 2008 November 18]; Available from: http://www.census.gov/population/www/projections/tablesandcharts.html
- 9.Angel J, Angel R. Aging trends - Mexican Americans in the Southwestern USA. Journal of Cross-Cultural Gerontology 1998;13(3):281–90. [DOI] [PubMed]
- 10.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D'Agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: the Framingham heart study. JAMA 2002;287(8):1003–10. [DOI] [PubMed]
- 11.DeNavas-Walt C, Proctor B, Smith J. Income, poverty, and health insurance coverage in the United States: 2007. Washington DC: US Government Printing Office; 2008.
- 12.Ogden LG, He J, Lydick E, Whelton PK. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC VI risk stratification. Hypertension 2000;35(2):539–43. [DOI] [PubMed]
- 13.Hubert HB, Snider J, Winkleby MA. Health status, health behaviors, and acculturation factors associated with overweight and obesity in Latinos from a community and agricultural labor camp survey. Prev Med. 2005;40(6):642–51. [DOI] [PubMed]
- 14.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29(3):470–477. [DOI] [PubMed]
- 15.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006. Diabetes Care 2009;32(2):287–94. [DOI] [PMC free article] [PubMed]
- 16.Farquhar I JJ, Weir E. Costs of concomitant illnesses among patients with hypertension and diabetes. Abstr Acad Health Serv Res Health Policy Meet 2000.
- 17.Hertz RP, Unger AN, Ferrario CM. Diabetes, hypertension, and dyslipidemia in Mexican Americans and non-Hispanic whites. Am J Prev Med. 2006;30(2):103–10. [DOI] [PubMed]
- 18.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55(7):1056–65. [DOI] [PubMed]
- 19.National Center for Health Statstics. Response Rates & CPS Population Totals. 2009 [cited 2009 July 23]; Available from: http://www.cdc.gov/nchs/nhanes/nhanes_cps_totals.htm
- 20.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the joint national committee on the prevention, detection, evaluation, and treatment of high blood pressure (JNC 7): resetting the hypertension sails. Hypertension 2003;41(6):1178–9. [DOI] [PubMed]
- 21.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003;26 Suppl 1:S5–20. [DOI] [PubMed]
- 22.Neese JW, Duncan P, Bayse DD, et al. Development and evaluation of a hexokinase/glucose-6-phosphate dehydrogenase procedure for use as a national glucose reference method. HEW Publication No. (CDC) 77–8330. HEW. USPHS, Centers for Disease Control and Prevention, 1976.
- 23.Natarajan S, Santa Ana EJ, Liao Y, Lipsitz SR, McGee DL. Effect of treatment and adherence on ethnic differences in blood pressure control among adults with hypertension. Ann Epidemiol. 2009;19(3):172–9. [DOI] [PubMed]
- 24.Molenaar EA, Hwang SJ, Vasan RS, Grobbee DE, Meigs JB, D'Agostino RB, Sr., et al. Burden and rates of treatment and control of cardiovascular disease risk factors in obesity: the Framingham Heart Study. Diabetes Care 2008;31(7):1367–72. [DOI] [PMC free article] [PubMed]
- 25.Wong ND, Lopez V, L'Italien G, Chen R, Kline SE, Franklin SS. Inadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003–2004. Arch Intern Med. 2007;167(22):2431–6. [DOI] [PubMed]
- 26.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension 2006;47(2):296–308. [DOI] [PubMed]
- 27.Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens 2006;24(2):215–33. [DOI] [PubMed]
- 28.Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144(7):485–95. [DOI] [PubMed]
- 29.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. [DOI] [PubMed]
- 30.Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care 2003;26(3):917–32. [DOI] [PubMed]
- 31.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008;16(10):2323–30. [DOI] [PubMed]
- 32.Winkleby MA, Kim S, Urizar GG, Ahn D, Jennings MG, Snider J. Ten-year changes in cancer-related health behaviors and screening practices among Latino women and men in California. Ethnicity & Health 2006;11(1):1–17. [DOI] [PubMed]
- 33.Winkleby MA, Cubbin C. Changing patterns in health behaviors and risk factors related to chronic diseases, 1990–2000. Am J Health Promot. 2004;19(1):19–27. [DOI] [PubMed]
- 34.Bersamin A, Hanni KD, Winkleby MA. Predictors of trying to lose weight among overweight and obese Mexican-Americans: a signal detection analysis. Public Health Nutr. 2008:1–10. [DOI] [PMC free article] [PubMed]
- 35.Prognosis in hypertension. Br Med J. 1970;4(5737):697–8. [PMC free article] [PubMed]
- 36.Buck C, Baker P, Bass M, Donner A. The prognosis of hypertension according to age at onset. Hypertension 1987;9(2):204–8. [DOI] [PubMed]
- 37.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164(19):2126–34. [DOI] [PubMed]
- 38.Qureshi AI, Suri MF, Kirmani JF, Divani AA. Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monit. 2005;11(9):CR403–9. [PubMed]
- 39.Kshirsagar AV, Carpenter M, Bang H, Wyatt SB, Colindres RE. Blood pressure usually considered normal is associated with an elevated risk of cardiovascular disease. Am J Med. 2006;119(2):133–41. [DOI] [PubMed]
- 40.Jimenez-Corona A, Lopez-Ridaura R, Stern MP, Gonzalez-Villalpando C. Risk of progression to hypertension in a low-income mexican population with pre-hypertension and normal blood pressure. Am J Hypertens 2007;20(9):929–36. [DOI] [PMC free article] [PubMed]
- 41.Leitschuh M, Cupples LA, Kannel W, Gagnon D, Chobanian A. High-normal blood pressure progression to hypertension in the Framingham Heart Study. Hypertension 1991;12(1):22–27. [DOI] [PubMed]
- 42.Huttin C, Moeller J, Stafford R. Patterns and costs for hypertension treatment in the United States: clinical, lifestyle and socioeconomic predictors from the 1987 national medical expenditures survey clinical drug investigation 2000;20(3):181–95.
- 43.Borrell LN, Crawford ND. Disparities in self-reported hypertension in Hispanic subgroups, non-Hispanic black and non-Hispanic white adults: the national health interview survey. Ann Epidemiol. 2008;18(10):803–12. [DOI] [PMC free article] [PubMed]
- 44.Loria CM, Bush TL, Carroll MD, Looker AC, McDowell MA, Johnson CL, et al. Macronutrient intakes among adult Hispanics: a comparison of Mexican Americans, Cuban Americans, and mainland Puerto Ricans. Am J Public Health 1995;85(5):684–9. [DOI] [PMC free article] [PubMed]
- 45.National Center for Chronic Disease Prevetion and Health Promotion. Behavioral Risk Factor Surveillance System. 2008; Available from: http://www.cdc.gov/brfss//
- 46.Chong Y, Carroll M, Burt V, Montalvan P. NHANES converted refusals: are they different from willing respondents in cardiovascular risk factors? In: American Association For Public Opinion Association; 2009; Miami Beach, FL; 2009.