Abstract
Many clinicians are trying unique strategies, including vancomycin and linezolid in combination, for treatment of patients who do not respond to conventional therapy against methicillin (meticillin)-resistant Staphylococcus aureus. In our study, which illustrated in vitro activity only, no synergistic activity was seen when the two agents were combined. Conversely, antagonistic activity occurred in three of five strains when linezolid was added to vancomycin. Our results indicate that vancomycin and linezolid in combination should be avoided.
Methicillin (meticillin)-resistant Staphylococcus aureus (MRSA) is a well-known nosocomial pathogen. There is considerable evidence showing that the incidence and possibly the virulence are rising (5, 8, 9, 10). Deep-seated infections are not responding as well to conventional vancomycin therapy (11, 15, 16). There have been case reports of not only vancomycin tolerance but also vancomycin resistance (3). This has an impact on the healthy population, with the growing incidence of community-acquired MRSA, and is of even more concern for the ever-growing number of elderly patients with numerous comorbid conditions, including hospitalized and nursing home patients (4, 6, 7, 17). Numerous alternative regimens are being tested in this era of multidrug-resistant organisms. These regimens include various lengths of treatment as well as combinations of antimicrobial agents. We have observed an increase in the use of linezolid and vancomycin together, with little evidence to support this practice. There is also the potential for overlap when one agent is switched to the other. Vancomycin is a bactericidal agent which inhibits bacterial cell wall synthesis, resulting in cell lysis. Linezolid is a bacteriostatic agent which binds the 50S ribosomal unit and inhibits protein synthesis. Few previous studies show the activity of these two antibiotics in combination. There have been approximately 20 strains of MRSA tested, and of these strains, several have shown no difference in activity while others suggest that linezolid and vancomycin may actually be antagonistic (2, 12, 14, 18). Our investigation was designed to consider additional MRSA isolates in a different geographic region and help provide more evidence about the interaction that vancomycin and linezolid have when used together.
In order to start this study, we first obtained five strains of MRSA isolates from blood cultures at Christiana Hospital and tested them to be sure they were different ribotypes. Next, the MICs for each strain were determined using the microdilution technique. The MICs were defined as the lowest concentration of an antimicrobial agent that prevented turbidity when assessed after 24 h of inoculation. MIC determination was repeated twice for consistency, and the average value for all three determinations was used as the final MIC. The MICs were 0.06 μg/ml for vancomycin in all isolates; 0.125 μg/ml for linezolid in isolates 1, 2, 4, and 5; and 0.25 μg/ml for isolate 3.
The time-kill study was performed with four concurrent tubes that were run over 24 h. All stock solutions were prepared in accordance with guidelines provided by the Clinical and Laboratory Standards Institute, formerly known as NCCLS (1). Each tube contained Mueller-Hinton broth, with an inoculum of 5 × 106 to 1 × 107 CFU/ml. Tube 1 was antibiotic free and served as the control. Tubes 2 and 3 had linezolid and vancomycin, respectively. Tube 4 contained both linezolid and vancomycin. All tubes were run with all five strains of MRSA separately. Surviving bacteria were counted at 0, 4, 8, and 24 h by subculturing 50-μl serial dilutions (10−1, 10−2, and 10−4) of samples in normal saline solution on Mueller-Hinton plates. The above was done at one-fourth, one-half, and two times the MIC for each agent. Bactericidal effect was defined as ≥3 log10 CFU/ml decrease in comparison with the level for the initial inoculum after 24 h of incubation. Synergy was defined as a decrease of ≥2 log10 CFU/ml between the combination and the most active single agent. Antagonism was defined as an increase in the colony count of ≥2 log10 CFU/ml with the combination in comparison with the count obtained with the most active single agent (13). This entire process was repeated for all five strains at one-fourth, one-half, and two times the MIC for each agent alone and in combination.
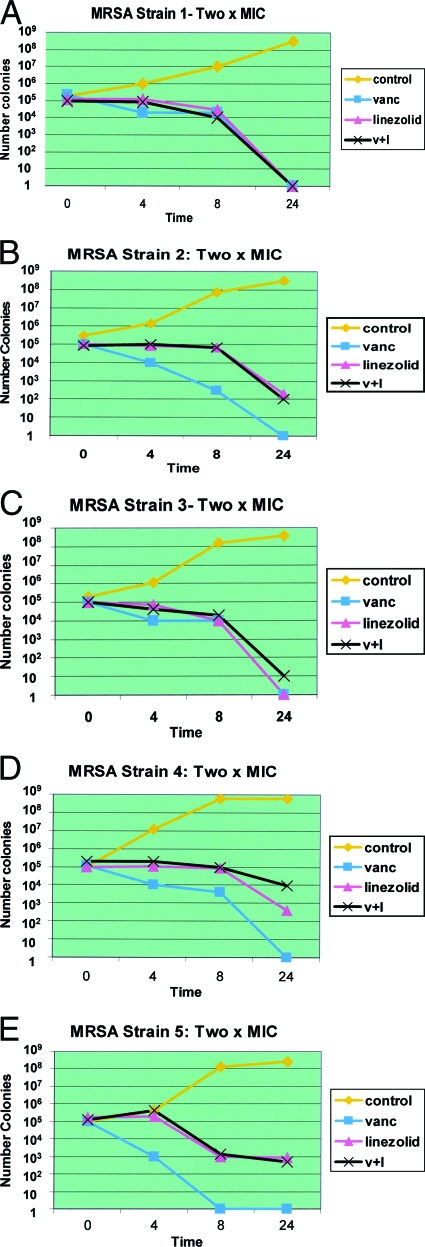
The final data were best delineated at two times the MIC. Figure 1A through E show the macrodilution time-kill curves for all five strains at two times the MIC. These show that for MRSA strains 2, 4, and 5, vancomycin was more effective when used alone than when linezolid was added. In strain number 1, there was no significant difference between each agent alone and combined. In strain number 3, vancomycin alone and linezolid alone were similar in activity. When the two agents were combined, they were less active than either agent alone, although this result was not significant enough to indicate antagonism. No synergistic activity was seen in any of the five strains of MRSA. Three of the five strains exhibited antagonistic activity when linezolid was added to vancomycin. Two of the strains were equivocal. This data set indicates that combination therapy is of no benefit and that vancomycin and linezolid should not be used together for MRSA infections. These results suggest that special attention may need to be given to patients with illnesses such as chronic renal disease when one agent is switched to another since these antibiotics may have altered kinetics or a prolonged half-life. We hypothesize that this antagonism may be due to a reduced ability on the part of vancomycin to bind to cells exposed to linezolid, which is bacteriostatic and decreases protein synthesis.
FIG. 1.
Panels A through E graphically illustrate the results at two times the MIC for each bacterial strain, comparing the activity of vancomycin and linezolid together against that of each antibiotic alone as well as the results for the control group, which did not contain any antibiotics.
These results do not account for tissue penetration and metabolism which alter the in vivo activity of these agents when used in combination. There needs to be more data both in vivo and in vitro to demonstrate the interaction between these two agents. These types of combinations as well as new agents will need to be studied as MRSA becomes more resistant and infections become more severe and harder to eradicate.
Acknowledgments
The linezolid powder used in this study was provided by Pfizer Global Pharmaceuticals, Highland Park, NJ.
We thank Cynthia J. T. Clendenin, Medical Editor for Academic Affairs at Christiana Care Health System, for her assistance with our manuscript, and Douglas Bugel, Medical Photographer, for his assistance with the preparation of the figure.
Footnotes
Published ahead of print on 27 July 2009.
REFERENCES
- 1.Barry, A. L., W. C. Craig, H. Nadler, L. B. Reller, C. C. Sanders, and J. M. Swenson. 1999. Methods for determining bactericidal activity of antimicrobial agents; approved guideline. NCCLS document M26-A. National Committee for Clinical Laboratory Standards, Wayne, PA.
- 2.Chiang, F. Y., and M. Climo. 2003. Efficacy of linezolid alone or in combination with vancomycin for treatment of experimental endocarditis due to methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 47:3002-3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deville, J. G., S. Adler, P. H. Azimi, B. A. Jantausch, M. R. Morfin, S. Beltran, B. Edge-Padbury, S. Naberhuis-Stehouwer, and J. B. Bruss. 2003. Linezolid versus vancomycin in the treatment of known or suspected resistant gram-positive infections in neonates. Pediatr. Infect. Dis. J. 22(Suppl.):S158-S163. [DOI] [PubMed] [Google Scholar]
- 4.Drinka, P. J., M. E. Stemper, C. D. Gauerke, J. E. Miller, B. M. Goodman, and K. D. Reed. 2005. Clustering of multiple endemic strains of methicillin-resistant Staphylococcus aureus in a nursing home: an 8-year study. Infect. Control Hosp. Epidemiol. 26:215-218. [DOI] [PubMed] [Google Scholar]
- 5.Jacqueline, C., J. Callion, V. Le Mabecque, A. F. Miegeville, P. Y. Donnio, D. Bugnon, and G. Potel. 2003. In vitro activity of linezolid alone and in combination with gentamicin, vancomycin or rifampicin against methicillin-resistant Staphylococcus aureus by time-kill curve methods. J. Antimicrob. Chemother. 51:857-864. [DOI] [PubMed] [Google Scholar]
- 6.Jones, R. N., T. R. Anderegg, and L. M. Deshpande. 2002. AZD2563, a new oxazolidinone: bactericidal activity and synergy studies combined with gentamicin or vancomycin against staphylococci and streptococcal strains. Diagn. Microbiol. Infect. Dis. 43:87-90. [DOI] [PubMed] [Google Scholar]
- 7.Kallen, A., T. Driscoll, S. Thorton, P. Olson, and M. Wallace. 2000. Increase in community-acquired methicillin-resistant Staphylococcus aureus at a Naval Medical Center. Infect. Control Hosp. Epidemiol. 21:223-226. [DOI] [PubMed] [Google Scholar]
- 8.Kowalski, T. J., E. F. Berbari, and D. R. Osmon. 2005. Epidemiology, treatment, and prevention of community-acquired methicillin-resistant Staphylococcus aureus infections. Mayo Clin. Proc. 80:1201-1207. [DOI] [PubMed] [Google Scholar]
- 9.Kreman, T., J. Hu, J. Pottinger, and L. A. Herwaldt. 2005. Survey of long-term-care facilities in Iowa for policies and practices regarding residents with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci. Infect. Control Hosp. Epidemiol. 26:811-815. [DOI] [PubMed] [Google Scholar]
- 10.National Nosocomial Infections Surveillance System. 2004. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am. J. Infect. Control 32:470-485. [DOI] [PubMed] [Google Scholar]
- 11.Samra, Z., O. Ofer, and H. Shmuely. 2005. Susceptibility of methicillin-resistant Staphylococcus aureus to vancomycin, teicoplanin, linezolid, pristinamycin and other antibiotics. Isr. Med. Assoc. J. 7:148-150. [PubMed] [Google Scholar]
- 12.Sweeney, M. T., and G. E. Zurenko. 2003. In vitro activity of linezolid combined with other antimicrobial agents against staphylococci, enterococci, pneumococci, and selected gram-negative organisms. Antimicrob. Agents Chemother. 47:1902-1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swenson, J. M., J. B. Patel, and J. H. Jorgensen. 2007. Special phenotypic methods for detecting antibacterial resistance, p. 1173-1192. In P. R. Murray, E. J. Baron, J. H. Jorgensen, M. L. Landry, and M. A. Pfaller (ed.), Manual of clinical microbiology, 9th ed. ASM Press, Washington, DC.
- 14.Tenover, F. C., L. M. Weigel, P. C. Appelbaum, L. K. McDougal, J. Chaitram, S. McAllister, N. Clark, G. Killgore, C. M. O'Hara, L. Jevitt, J. B. Patel, and B. Bozdogan. 2004. Vancomycin-resistant Staphylococcus aureus isolate from a patient in Pennsylvania. Antimicrob. Agents Chemother. 48:275-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weigelt, J., K. Itani, D. Stevens, W. Lau, M. Dryden, C. Knirsch, et al. 2005. Linezolid versus vancomycin in treatment of complicated skin and soft tissue infections. Antimicrob. Agents Chemother. 49:2260-2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weigelt, J., H. M. Kaafarani, K. M. Itani, and R. N. Swanson. 2004. Linezolid eradicates MRSA better than vancomycin from surgical-site infections. Am. J. Surg. 188:760-766. [DOI] [PubMed] [Google Scholar]
- 17.Wunderink, R. G., J. Rello, S. K. Cammarata, R. V. Croos-Dabrera, and M. H. Kollef. 2003. Linezolid vs vancomycin: analysis of two double-blind studies of patients with methicillin-resistant Staphylococcus aureus nosocomial pneumonia. Chest 124:1789-1797. [PubMed] [Google Scholar]
- 18.Zetola, N., J. S. Francis, E. L. Nuermberger, and W. R. Bishai. 2005. Community-acquired meticillin-resistant Staphylococcus aureus: an emerging threat. Lancet Infect. Dis. 5:275-286. [DOI] [PubMed] [Google Scholar]