Abstract
To identify mutations that can arise in highly pathogenic A(H5N1) viruses under neuraminidase inhibitor selective pressure, two antigenically different strains were serially passaged with increasing levels of either oseltamivir or zanamivir. Under oseltamivir pressure, both A(H5N1) viruses developed a H274Y neuraminidase mutation, although in one strain the mutation occurred in combination with an I222M neuraminidase mutation. The H274Y neuraminidase mutation reduced oseltamivir susceptibility significantly (900- to 2,500-fold compared to the wild type). However the dual H274Y/I222M neuraminidase mutation had an even greater impact on resistance, with oseltamivir susceptibility reduced significantly further (8,000-fold compared to the wild type). A similar affect on oseltamivir susceptibility was observed when the dual H274Y/I222M mutations were introduced, by reverse genetics, into a recombinant seasonal human A(H1N1) virus and also when an alternative I222 substitution (I222V) was generated in combination with H274Y in A(H5N1) and A(H1N1) viruses. These viruses remained fully susceptible to zanamivir but demonstrated reduced susceptibility to peramivir. Following passage of the A(H5N1) viruses in the presence of zanamivir, the strains developed a D198G neuraminidase mutation, which reduced susceptibility to both zanamivir and oseltamivir, and also an E119G neuraminidase mutation, which demonstrated significantly reduced zanamivir susceptibility (1,400-fold compared to the wild type). Mutations in hemagglutinin residues implicated in receptor binding were also detected in many of the resistant strains. This study identified the mutations that can arise in A(H5N1) under either oseltamivir or zanamivir selective pressure and the potential for dual neuraminidase mutations to result in dramatically reduced drug susceptibility.
Large-scale outbreaks of highly pathogenic A(H5N1) avian influenza affecting poultry have occurred throughout many parts of Asia, North Africa, and the Middle East since 2003 (1). The virus, which now appears to be enzootic in many regions, has on occasion caused zoonotic infections in humans (1). Humans who acquire the infection develop severe pneumonia that can progress to acute respiratory distress syndrome with high risk of mortality. For the 6-year period 2003 to 2008, 395 confirmed A(H5N1) virus human infections were reported, and 250 were fatal (a case fatality rate of 63%) (http://www.who.int/csr/disease/avian_influenza/en/index.html). Human-to-human transmission of A(H5N1) virus appears to be rare and has been associated only with very close unprotected contact with severely ill patients (30). Of concern is the potential for the A(H5N1) virus to become easily transmissible between humans, which, because of the lack of prior immunity to this strain in humans, might result in a global influenza pandemic. Based on these theoretical concerns and the experiences of large-scale morbidity and mortality from previous influenza pandemics, many countries have prepared plans to address or mitigate such an occurrence, including the stockpiling of inactivated A(H5N1) influenza vaccines, as well as anti-influenza drugs. Because multiple vaccine doses may be necessary to achieve protection and some time would be required to generate a vaccine with an antigenically matched strain (1), antiviral drugs could play a critical role in the treatment or prophylaxis of influenza, particularly during the early stages of a pandemic. The oral neuraminidase (NA) inhibitor oseltamivir (Tamiflu) has been the most widely used anti-influenza drug for the treatment of A(H5N1) virus -infected patients and has been stockpiled for potential broad use. Results from uncontrolled clinical trials suggest that the use of oseltamivir may increase the survival rate of patients with A(H5N1) virus infection, particularly if administered early in the course of illness (1). However, oseltamivir-resistant A(H5N1) virus variants with an H274Y NA mutation have been isolated from treated patients and may be associated with clinical deterioration and fatal outcomes (9). Viruses with the H274Y NA mutations are susceptible to the NA inhibitor zanamivir, which has led to the inclusion of inhaled zanamivir, together with oseltamivir, in pandemic drug stockpiles. The volume of drug that might be used in the event of a pandemic would be significantly greater than has ever been used previously for treatment of seasonal influenza. There is concern that this may lead to a high frequency of drug resistance. While previous studies have identified a number of NA inhibitor resistance mutations that have arisen in seasonal influenza viruses under drug pressure, little is known about which NA inhibitor resistance mutations might arise in highly pathogenic A(H5N1) viruses. To investigate this question, two A(H5N1) strains from different phylogenetic clades were subjected to serial passage in Madin-Darby canine kidney (MDCK) cells in the presence of increasing levels of either oseltamivir or zanamivir, and the resultant viruses were analyzed functionally and genetically.
MATERIALS AND METHODS
Virus culture.
Two A(H5N1) influenza viruses known to be highly pathogenic in chickens, A/Vietnam/1203/2004 (Vn/1203) (phylogenetic clade 1) and A/Chicken/Laos/26/2006 (Laos/26) (phylogenetic clade 2.3) (1) (kindly supplied by Paul Selleck, Australian Animal Health Laboratory, Australia), were allowed to adsorb to confluent MDCK cells (American Type Culture Collection [CCL-34]) at a low multiplicity of infection (0.01 PFU per cell) for 30 min at 35°C prior to removal of the inoculum and the addition of media (19) containing various concentrations of either oseltamivir or zanamivir. Viruses were cultured and handled under enhanced biosafety level 3 conditions at the Australian Animal Health Laboratory, Australia. Oseltamivir carboxylate, the active form of the ethyl ester prodrug oseltamivir phosphate, was kindly provided by Hoffmann-La Roche Ltd., Switzerland, and zanamivir was kindly provided by GSK Australia.
The first passage of the virus under NA inhibitor selective pressure was at a concentration of 1 nM, after which the cultured virus was repassaged in medium containing two times and five times the drug concentration used in the previous passage (i.e., after the first passage at 1 nM of NA inhibitor, second passages of the virus were conducted at both 2 nM and 5 nM of NA inhibitor). The viruses were harvested after 48 h, and the hemagglutination titer was determined using turkey erythrocytes. Viruses that had grown to a titer of at least 2 hemagglutinin (HA) units at the highest drug concentration were diluted and used to reinfect MDCK cells at a further increased drug concentration (2× and 5×). Both viruses, Vn/1203 and Laos/26, were cultured a total of 10 times at increasing concentrations (2× or 5×) of NA inhibitor (drug concentrations ranged from 1 nM to 1,950 μM) and were then cultured once in the absence of drug to remove residual NA inhibitor from the medium prior to testing.
NA activity.
To determine the relative NA activity, recombinant viruses were standardized to an equivalent infectious dose (105.8 50% tissue culture infective doses [TCID50]/ml), serially diluted (twofold) in assay buffer (32.5 mM MES [morpholineethanesulfonic acid] [pH 6.5], 4 mM CaCl2 with 0.1% NP-40 and 0.3 mg/ml bovine serum albumin), and then mixed with an equal volume (50 μl) of the substrate 2-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA) (0.3 mM) before incubation at 37°C for 60 min. The reaction was terminated by the addition of 100 μl of stop solution (0.14 M NaOH in 83% ethanol). Quantification of the fluorescent product 4-methylumbelliferone was determined using a Fluoroscan Ascent FL (Thermo) with an excitation wavelength of 360 nm and an emission wavelength of 448 nm. The viruses were tested in duplicate in three separate assays. The NA activities of the mutant viruses were calculated as relative percentages of the NA activity of the wild-type virus.
NA inhibition assay.
The viruses were tested for susceptibility to oseltamivir, zanamivir, and peramivir, an NA inhibitor currently undergoing clinical development in parenteral formulations (kindly provided by BioCryst, Birmingham, AL). To determine the drug concentration required to inhibit 50% of the NA activity (IC50), 50 μl of virus, diluted according to the NA activity assay, was mixed with various concentrations of inhibitor in microtiter plates (FluoroNunc plates; Nunc). The final reaction mixture concentrations of the NA inhibitors ranged from 0.01 nM to 10,000 nM. The virus-inhibitor mixture was incubated at room temperature for 45 min prior to the addition of 50 μl of MUNANA substrate (0.3 mM) and then incubated at 37°C for 60 min. The reaction was terminated by the addition of 100 μl of the stop solution. The data were plotted as the percentage of fluorescence activity inhibited against the log NA inhibitor concentration. IC50s were calculated using the logistic curve fit program Robosage, kindly provided by GSK, United Kingdom. Control susceptible and resistant strains were included in each assay and demonstrated an IC50 variability of 8% over six separate assays.
RT-PCR and sequencing.
Viral RNA was extracted from 200 μl of MDCK cell culture supernatants using the MagnaPure extraction system according to the manufacturer's recommendations (Roche, Australia) with an elution volume of 90 μl. A 5-μl aliquot of RNA was used to amplify the selected influenza virus gene using specific primers (sequences are available by request) and the SuperScriptIII Platinum One-Step reverse transcription (RT)-PCR system (Invitrogen) reagents. The amplicons were visualized on a 2% agarose gel. The PCR products were purified for use in a sequencing reaction using the QIAquick PCR Purification Kit (Qiagen). DNA sequencing was carried out using the ABI Prism Dye Terminator III cycle-sequencing kit (Applied Biosystems), followed by the removal of excess dye terminators using a DyeEx Spin Kit (Qiagen). The sequence was determined using an automated capillary DNA sequencer (an ABI Prism 377 located at the Institute of Medical and Veterinary Science, Adelaide, Australia). Sequences were assembled and aligned using the DNAStar Lasergene 8 package.
Pyrosequencing analysis.
RT-PCR of the NA genes was conducted as described previously, except that one of the PCR primers was biotinylated. Biotinylated PCR products (40 μl) were immobilized on streptavidin-coated Sepharose beads (Streptavidin Sepharose HP; Amersham Biosciences) in binding buffer (40 μl) by shaking them at 1,000 rpm for 5 min at room temperature according to the Pyromark ID System guidelines (Biotage, Sweden). The resultant single-stranded biotinylated DNAs were then transferred using the Pyromark Vacuum Prep Workstation (Biotage, Sweden) into 40 μl annealing buffer containing pyrosequencing primers and annealed at 80°C for 2 min. The mixture was cooled to room temperature and then subjected to pyrosequencing reactions using Pyro Gold Reagents on a Pyromark ID System (Biotage AB, Sweden) following the protocol provided by the manufacturer. The relative proportions of wild-type and mutant genes were determined with the Pyromark ID v1.0 software following allele quantitation analysis.
Generation of recombinant viruses and site-directed mutagenesis.
Recombinant viruses were generated using the eight-plasmid reverse-genetics system with pHW2000 plasmids that contained the cDNA of the influenza virus gene segments (17). The NA gene from the cultured viruses was amplified by RT-PCR as previously described (17) and incorporated into the pHW2000 plasmid. The NA plasmid was then combined with other plasmids containing the seven remaining gene segments from A/Puerto Rico/8/1934 (H1N1) influenza virus (kindly supplied by Robert Webster, St. Jude Children's Research Hospital, Memphis, TN). All eight plasmids were transfected into a coculture of 293T and MDCK cells as previously described (17) and then further expanded in MDCK cells. To investigate mutations at key residues, site-directed mutagenesis was conducted on the NA gene plasmid using the QuikChange Site-Directed Mutagenesis Kit (Stratagene, CA). Introduced mutations were confirmed by sequencing.
Replication kinetics.
MDCK cells were infected with viruses at a multiplicity of infection of 0.01 TCID50/cell and incubated at 35°C for 1 h. The cells were then washed and overlaid with maintenance medium before being incubated at 35°C. Three hundred microliters of supernatant from each virus was collected at 12, 24, 36, 48, and 60 h postinfection and stored at −70°C prior to determination of the viral infectivity titer.
Viral infectivity assay.
MDCK cells were seeded into 96-well plates (Cellstar; Greiner Bio-one) (1.5 × 104 cells per well) and grown to confluence overnight at 37°C in a 5% CO2 incubator. The monolayers were washed twice with Ca2+/Mg2+-free phosphate-buffered saline before inoculation with triplicate 10-fold dilutions of virus. After incubation for 4 days at 35°C in 5% CO2, each well was scored for virus growth by cytopathic effect, and the dose required to infect 50% of the wells (TCID50) was determined.
RESULTS
Analysis of the Vn/1203 virus following culture in the presence of oseltamivir revealed an increase in the oseltamivir IC50 at passage 6 (P6) (1,250 nM) (Table 1), which was associated with a histidine (H)-to-tyrosine (Y) NA mutation at residue 274 (N2 numbering, equivalent to residue 275 in N1). The IC50s increased as the proportion of H274Y mutants in the viral population increased (estimated by pyrosequencing to be 64% to 100%) (Table 1). The H274Y NA mutation was also detected following passage of the Laos/26 strain with oseltamivir, although not until the virus was grown in the presence of a much higher oseltamivir concentration (78 μM; P8) (Table 1). Interestingly, the Laos/26 virus had an additional NA mutation, I222M (N2 numbering, equivalent to residue 223 in N1), which was detected at an earlier passage level (P6; 3,125 nM) than the H274Y mutation, and this I222M mutation was then maintained together with the H274Y mutation from P8 until the end of the experiment (P10) (Table 1).
TABLE 1.
Serial passage of A(H5N1) viruses in the presence of increasing concentrations of oseltamivira
| Virus strain | Passage no. | Oseltamivir concn | Zanamivir IC50 | Oseltamivir IC50 | HA mutationb | NA mutation (%)c |
|---|---|---|---|---|---|---|
| A/Vietnam/1203/2004 | 0 nM | 0.5 | 0.2 | |||
| 1 | 1 nM | 0.7 | 0.3 | |||
| 2 | 5 nM | 0.5 | 0.3 | |||
| 3 | 25 nM | 0.3 | 0.2 | |||
| 4 | 50 nM | 0.3 | 0.2 | |||
| 5 | 250 nM | 0.5 | 0.2 | |||
| 6 | 1,250 nM | 0.5 | 25.3 | H274Y (64) | ||
| 7 | 6,250 nM | 0.5 | 145.2 | H274Y (92) | ||
| 8 | 31 μM | 0.5 | 177.0 | H274Y (100) | ||
| 9 | 156 μM | 0.5 | 180.3 | A45S; K156E; P210Q; L313F | H274Y (100) | |
| 10 | 781 μM | 0.5 | 152.8 | A45S; K156E; P210Q; L313F | H274Y (100) | |
| A/Chicken/Laos/26/2006 | 0 nM | 0.3 | 0.3 | |||
| 1 | 1 nM | 0.3 | 0.2 | |||
| 2 | 5 nM | 0.3 | 0.3 | |||
| 3 | 25 nM | 0.3 | 0.3 | |||
| 4 | 125 nM | 0.3 | 0.3 | |||
| 5 | 625 nM | 0.3 | 0.4 | |||
| 6 | 3,125 nM | 0.3 | 0.4 | I222M (68) | ||
| 7 | 16 μM | 0.3 | 18.2 | K234Q | I222M (65) | |
| 8 | 78 μM | 0.4 | 89.2 | K234Q | I222M (31); H274Y (45) | |
| 9 | 390 μM | 0.5 | 191.6 | K234Q | I222M (21%); H274Y (100) | |
| 10 | 1,950 μM | 0.7 | 1,390.0 | K234Q | I222M (70); H274Y (100) |
A(H5N1) influenza viruses A/Vietnam/1203/2004 and A/Chicken/Laos/26/2006 were cultured in MDCK cells in the presence of increasing concentrations of oseltamivir. Each passage level was tested for susceptibility to zanamivir and oseltamivir and sequenced to investigate the generation of any HA or NA mutations. IC50 values are based on assays completed in duplicate.
Based on H5 residue numbering.
Based on N2 residue numbering. The percentages in parentheses indicate the proportion of each individual mutant in the total viral population based on pyrosequencing analysis. Mutations that were present at <20% of the total viral population are not shown.
Passage of the Vn/1203 virus in the presence of zanamivir (1,250 nM) at P6 resulted in the detection of a D198G NA mutation (N2 numbering, equivalent to residue 199 in N1) (Table 2). This mutation was present in only 28% of the viral population (estimated by pyrosequencing analysis) at P6 (1,250 nM) but increased to a peak of 93% by P8 (31 μM). Although the D198G mutation was still present at P9 (156 μM), viruses with an E119G NA mutation were also detected in the viral population, and following a further passage (P10; 781 μM), only the E119G mutation was detected (Table 2). Passage of the Laos/26 strain in the presence of zanamivir generated the same E119G mutation detected in the Vn/1203 virus under zanamivir pressure (Table 2). By the end of the passaging protocol, the E119G mutation was present in approximately 88% of the Laos/26 viral population, similar to the proportion of the mutant in the Vn/1203 P10 viral population (76%). Mutations in the HA gene of the drug-passaged viruses were also detected (Tables 1 and 2), with some zanamivir-selected Vn/1203 viruses and oseltamivir-selected Laos/26 virus, both containing a K234 mutation (K234N in Vn/1203 virus and K234Q in Laos/26 virus).
TABLE 2.
Serial passage of A(H5N1) viruses in the presence of increasing concentrations of zanamivira
| Virus strain | Passage no. | Zanamivir concn | Zanamivir IC50 | Oseltamivir IC50 | HA mutationb | NA mutation (%)c |
|---|---|---|---|---|---|---|
| A/Vietnam/1203/2004 | 0 nM | 0.7 | 0.2 | |||
| 1 | 1 nM | 1.1 | 0.3 | |||
| 2 | 5 nM | 0.6 | 0.2 | |||
| 3 | 25 nM | 0.6 | 0.2 | |||
| 4 | 50 nM | 0.8 | 0.2 | |||
| 5 | 250 nM | 0.6 | 0.2 | |||
| 6 | 1,250 nM | 0.6 | 0.2 | K234N | D198G (28) | |
| 7 | 6,250 nM | 1.2 | 0.4 | K234N | D198G (86) | |
| 8 | 31 μM | 7.0 | 2.1 | K234N | D198G (93) | |
| 9 | 156 μM | 7.8 | 2.3 | K234N | D198G (64); E119G (35) | |
| 10 | 781 μM | 40.3 | 3.0 | K234N | E119G (76) | |
| A/Chicken/Laos/26/2006 | 0 nM | 0.2 | 0.2 | |||
| 1 | 1 nM | 0.2 | 0.2 | |||
| 2 | 5 nM | 0.2 | 0.2 | |||
| 3 | 25 nM | 0.2 | 0.2 | |||
| 4 | 125 nM | 0.3 | 0.3 | |||
| 5 | 625 nM | 0.2 | 0.2 | |||
| 6 | 3,125 nM | 0.2 | 0.3 | |||
| 7 | 16 μM | 0.2 | 0.3 | E119G (50) | ||
| 8 | 78 μM | 4.0 | 0.9 | E119G (82) | ||
| 9 | 390 μM | 19.1 | 6.2 | K205E | E119G (87) | |
| 10 | 1,950 μM | 16.7 | 5.7 | K205E | E119G (88) |
A(H5N1) influenza viruses A/Vietnam/1203/2004 and A/Chicken/Laos/26/2006 were cultured in MDCK cells in the presence of increasing concentrations of oseltamivir. Each passage level was tested for susceptibility to zanamivir and oseltamivir and sequenced to investigate the generation of any HA or NA mutations. IC50 values are based on assays completed in duplicate.
Based on H5 residue numbering.
Based on N2 residue numbering. The percentages in parentheses indicate the proportion of each individual mutant in the total viral population based on pyrosequencing analysis. Mutations that were present at <20% of the total viral population are not shown.
Although NA mutations were detected in the isolates following serial MDCK passage in the presence of drug, these isolates contained mixed viral populations and, as such, could not be used to distinguish the effect of each mutation on NA inhibitor susceptibility. Therefore, the NA segments from the Vn/1203 and Laos/26 viruses containing each of the NA mutations detected following serial MDCK passage were used to generate viruses by reverse genetics. Single I222M and H274Y mutations in the Laos/26 NA resulted in 36- and 911-fold increases in the oseltamivir IC50, respectively, but together caused a >8,000-fold increase (Table 3). The double mutant, although remaining fully susceptible to zanamivir, had a >3,000-fold increase in the peramivir IC50, even though the peramivir susceptibility of the virus with the I222M mutation alone was not different from that of the wild type (Table 3). The NA activity of the double mutant was reduced by approximately 50% compared to the wild type (Table 3).
TABLE 3.
NA inhibitor susceptibilities of recombinant viruses
| Recombinant virus and NA mutationa | Relative NA activity (%)e | Oseltamivir
|
Zanamivir
|
Peramivir
|
|||
|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM)f | Fold change | Mean IC50 ± SD (nM)f | Fold change | Mean IC50 ± SD (nM)f | Fold change | ||
| Laos/26 H5N1 NAb | |||||||
| Wild type | 100 | 0.8 ± 0.2 | 1 | 0.5 ± 0.1 | 1 | 0.3 ± 0.02 | 1 |
| I222M | 76 ± 12 | 27.8 ± 4.2 | 36 | 0.5 ± 0.1 | 1 | 0.3 ± 0.02 | 1 |
| H274Y | 43 ± 16 | 695.6 ± 178.0 | 911 | 0.6 ± 0.1 | 1 | 142.4 ± 31.4 | 533 |
| I222M + H274Y | 52 ± 4 | 6,126.2 ± 1,319.0 | 8,024 | 1.4 ± 0.1 | 3 | 891.4 ± 119.9 | 3,340 |
| I222V | 71 ± 9 | 5.3 ± 1.5 | 7 | 0.7 ± 0.1 | 1 | 0.3 ± 0.04 | 1 |
| I222V + H274Y | 29 ± 6 | 1,469.7 ± 291.3 | 1,925 | 1.1 ± 0.1 | 2 | 562.1 ± 66.2 | 2,106 |
| E119G | 1 ± 1 | 3.1 ± 0.6 | 4 | 677.3 ± 187.8 | 1,345 | 43.6 ± 2.0 | 164 |
| Vn/1203 H5N1 NAc | |||||||
| Wild type | 100 | 0.2 ± 0.02 | 1 | 0.6 ± 0.1 | 1 | 0.3 ± 0.02 | 1 |
| H274Y | 74 ± 15 | 498.9 ± 81.9 | 2,502 | 1.0 ± 0.2 | 2 | 27.0 ± 3.8 | 108 |
| D198G | 50 ± 7 | 6.4 ± 0.6 | 32 | 25.5 ± 3.9 | 44 | 1.0 ± 0.1 | 4 |
| E119G | 2 ± 1 | 0.7 ± 0.1 | 3 | 868.1 ± 365.2 | 1,485 | 3.0 ± 0.5 | 12 |
| NC/20 H1N1 NAd | |||||||
| Wild type | 100 | 1.5 ± 0.2 | 1 | 0.7 ± 0.1 | 1 | 0.2 ± 0.1 | 1 |
| I222M | 67 ± 12 | 11.9 ± 1.7 | 8 | 0.4 ± 0.1 | 1 | 0.2 ± 0.1 | 1 |
| H274Y | 56 ± 1 | 1,178.3 ± 164.1 | 761 | 0.8 ± 0.2 | 1 | 82.8 ± 19.7 | 347 |
| I222M + H274Y | 50 ± 2 | 3,009.1 ± 395.2 | 1,943 | 0.5 ± 0.1 | 1 | 95.5 ± 25.7 | 400 |
| I222V | 141 ± 25 | 4.5 ± 0.9 | 3 | 1.3 ± 0.3 | 2 | 0.3 ± 0.02 | 1 |
| I222V + H274Y | 123 ± 10 | 1,502.8 ± 216.0 | 971 | 1.5 ± 0.3 | 2 | 213.0 ± 46.1 | 893 |
Recombinant viruses were generated using reverse genetics in which the NA gene was derived as indicated and the remaining seven genes were derived from A/PR/8/34. Mutations were generated in the NA gene by site-directed mutagenesis.
The NA gene was derived from A(H5N1) virus A/Chicken/Laos/26/2006.
The NA gene was derived from A/Vietnam/1203/2004.
The NA gene was derived from the A(H1N1) virus A/New Caledonia/20/99.
The mean ± standard deviation for the relative NA activity compared with that of the respective wild-type virus, which was considered 100%.
The mean IC50 values and standard deviations were based on the analysis of reverse genetics-rescued viruses with oseltamivir, zanamivir, and peramivir in three separate assays.
The D198G mutation identified in the Vn/1203 strain following zanamivir passage resulted in 44-fold, 32-fold, and 4-fold increases in the IC50s for zanamivir, oseltamivir, and peramivir, respectively, in the recombinant strains (Table 3), while the E119G mutation, which was identified following passage of both H5 strains in high concentrations of zanamivir, conferred a >1,300-fold increase in the zanamivir IC50 but had no effect on the oseltamivir sensitivities of the viruses and relatively little effect on the peramivir IC50 (Table 3). The NA activities of the E119G mutants were severely reduced in both H5 strains, demonstrating only 1 to 2% of the activity of the wild-type virus (Table 3).
Analysis of the NA sequences of A(H5N1) viruses in GenBank identified a strain isolated from a 15-year-old patient from Egypt (A/Egypt/2751-NAMRU3/2007; GenBank accession no. ACJ53861) with an I222V mutation. Using site-directed mutagenesis and reverse genetics, viruses with the NA from Laos/26 were generated with the I222V mutation alone and with the dual I222V and H274Y mutations. The I222V mutation alone conferred a minor change in oseltamivir susceptibility (a 7-fold increase in the IC50), but when introduced as a dual mutation with H274Y, it resulted in a >1,900-fold increase in the IC50, more than double the IC50 of viruses with the H274Y mutation alone (Table 3). The oseltamivir IC50 for the I222V virus (5.3 nM) was lower than that observed for the I222M mutant virus (27.8 nM), and similarly, the IC50 for the I222V/H274Y dual mutation was lower (1469 nM) than that for the I222M/H274Y dual mutation (6,126 nM) (Table 3).
Because of the effect of the I222M or I222V mutation in combination with the H274Y mutation in increasing the oseltamivir and peramivir IC50s in the N1 from the Laos/26 A(H5N1) virus, the same combinations of mutations were investigated in the N1 from the human A(H1N1) virus A/New Caledonia/20/99 (NC/20) using reverse genetics. The I222M and I222V mutations alone conferred minor increases in the oseltamivir IC50 (eightfold and threefold, respectively) and no increase in the peramivir IC50. The dual I222M/H274Y and I222V/H274Y mutations resulted in 1,943-fold and 971-fold increases in the oseltamivir IC50 compared to a 761-fold increase with the H274Y mutation alone. These data demonstrate a trend similar to that of the impact of the NA mutations in the Laos/26 recombinant viruses (Table 3).
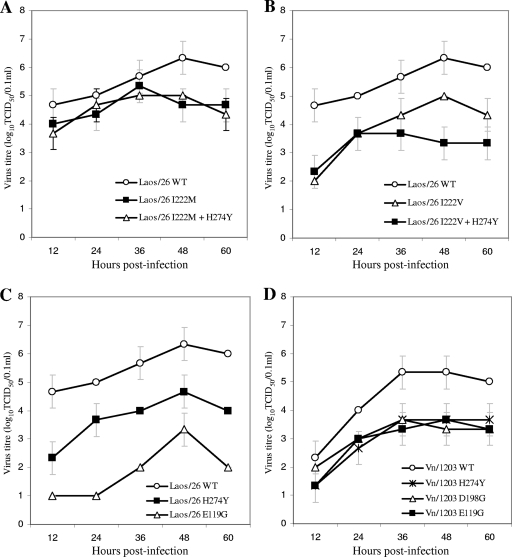
The replication kinetics of the A(H5N1) recombinant viruses were compared following analysis of virus yields at 12-hour intervals postinfection. The Laos/26 I222M and the dual I222M/H274Y mutant viruses had yields similar to those of the Laos/26 wild type until 36 h postinfection, after which the titers for the mutants were at least 1 log unit lower than those of the wild type (Fig. 1A). The Laos/26 I222V and H274Y single mutants and the dual mutant I222V/H274Y all had yields that were 1 to 2 log units lower than those of the wild type for all time points postinfection (Fig. 1B and C), while the Laos/26 E119G mutant appeared to be the most compromised of all, with yields approximately 3 log units lower than those of the wild type (Fig. 1C). No significant difference was observed between the growth rates of the Vn/1203 H274Y, D198G, and E119G recombinant mutants; however, all of these strains grew to lower virus yields than the wild type (Fig. 1D).
FIG. 1.
In vitro replication kinetics of recombinant viruses. Shown are growth curves for recombinant viruses Laos/26 wild type (WT), I222M, and I222M plus H274Y (A); Laos/26 WT, I222V, and I222V plus H274Y (B); Laos/26 WT, H274Y, and E119G (C); and Vn/1203 WT, Vn/1203 H274Y, Vn/1203 D198G, and Vn/1203 E119G (D). Virus yields were determined from the TCID50s in MDCK cells at 12, 24, 26, 48, and 60 h. Each data point represents the yield of a virus tested in triplicate (mean ± standard deviation of TCID50/0.1 ml).
DISCUSSION
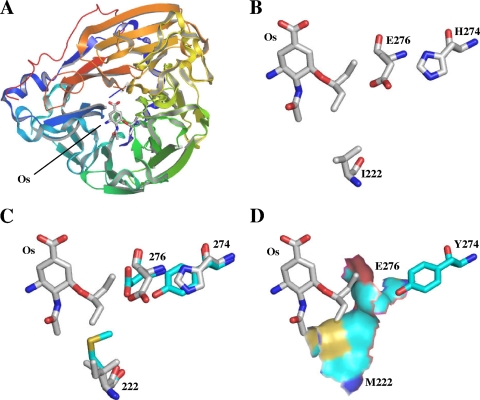
To investigate which amino acids in the NA may be susceptible to mutation under either zanamivir or oseltamivir selective pressure, two influenza A(H5N1) viruses from different genetic clades were grown in the presence of the drugs. Under oseltamivir pressure, both of the strains used in this study developed an H274Y NA mutation, which was the same substitution that has been detected in influenza A(H5N1) viruses isolated from two Vietnamese patients during oseltamivir treatment (9). The H274Y mutation has also been the most commonly observed NA inhibitor resistance mutation in human seasonal A(H1N1) viruses following oseltamivir treatment (21) and has now been identified in a high proportion of circulating A(H1N1) viruses isolated since late 2007 in Europe, the United States, and regions of Asia and Oceania (16, 20, 28) in the absence of oseltamivir treatment. The H274Y mutation has no impact on zanamivir susceptibility but causes high-level oseltamivir resistance, as it produces considerable movement of the neighboring side chain of E276 so that it significantly disturbs one of the ethyl moieties of oseltamivir, causing the diethyl moiety to reposition in the active site (Fig. 2C) (7). The additional mutations in the I222 framework residue of the Laos/26 virus (I222M or I222V) involve the other ethyl moiety of the oseltamivir diethyl extension and result in the loss of hydrophobic interaction between the side chain of I222 and oseltamivir. In the case of the I222M mutation, the longer amino acid side chain of methionine partially projects into the binding site (Fig. 2C). However, combined with the H274Y mutation, this results in an extensive occlusion of the active site, so that it can no longer accommodate the bulky diethyl extension of oseltamivir (Fig. 2D).
FIG. 2.
Modeling of resistance mutations. (A) Ribbon representation of a single monomer of the A/Vietnam/1203/2004 A(H5N1) NA-oseltamivir (Os) complex (Protein Data Bank [PDB] ID, 2HT8). (B) Stick representation of wild-type A/Vietnam/1203/2004 A(H5N1) NA, shown in standard atomic coloring, displaying the important interacting residues with the diethyl moiety of oseltamivir (PDB ID, 2HT8). (C) Stick representation of wild-type A/Vietnam/1203/2004 A(H5N1) NA (white sticks) superimposed on mutants H274Y and I222M (cyan sticks). (D) The crystal structure of the H274Y mutation (PDB ID, 3Cl0) was utilized, and an I222M mutation was introduced using modeling software. The addition of the protein surface shows that the dual H274Y/I222M mutation occludes the active site, explaining the large increase in the oseltamivir IC50 observed experimentally. The images were produced with the modeling software package PYMOL (10) using PDB codes 2HT8 (27) and 3Cl0 (7) downloaded from the RCS Protein Data Bank.
The I222 residue is highly conserved across all influenza A and B viruses and, together with R224, S246, and E276, forms the hydrophobic pocket of the active NA site (18). Of the 782 NA sequences from A(H5N1) viruses available on GenBank (accessed 15 January 2009), 24 (3%) had mutations at the I222 residue (I222T (15 strains), I222V (4 strains), I222L (2 strains), I222K (1 strain), I222F (1 strain), and I222M (1 strain)). Unlike the A(H5N1) strains, none of the 613 NAs from A(H1N1) viruses available on GenBank had any mutations at the I222 residue, although one A(H1N1) community isolate with an I222V mutation had been detected previously (24). In an unpublished study (31) reported by Baz et al. (5), an I222V mutation was identified both as a single mutation and in combination with the H274Y mutation following the in vitro passage of an A(H1N1) virus in the presence of oseltamivir. The I222V mutation conferred a 2-fold increase in the oseltamivir IC50, while the dual mutation resulted in a >1,000-fold increase (5), effects that were similar to the 3-fold (I222V) and 971-fold (I222V and H274Y) increases in the oseltamivir IC50 when the same mutations were introduced into the NC/20 A(H1N1) NA of viruses generated by reverse genetics in this study. The I222V mutation has also been detected in combination with a E119V NA mutation in an influenza A(H3N2) virus isolated from an immunocompromised patient undergoing oseltamivir treatment (5). As was observed with the I222V/M and H274Y mutations in the current study, the dual I222V and E119V mutations in the N2 NA also caused a greater reduction in oseltamivir susceptibility in combination than when present as single mutations (5). Interestingly, in the study by Baz et al., the I222V mutation caused an increase in NA activity in the N2 virus (123%) similar to that observed in the NC/20 N1 NA from the current study (141%). Further study is necessary to determine why the I222V mutation increased the NA activities in these human N1 and N2 strains but decreased the activity in the avian Laos/26 H5N1 virus. Nevertheless, any NA inhibitor resistance mutation that does not reduce the NA activity of a virus could be considered more likely to occur in circulating strains than mutations that cause severely reduced NA activity and therefore result in reduced viral fitness (such as the E119G mutation).
Under zanamivir selective pressure, both the Vn/1203 and Laos/26 viruses developed an E119G NA mutation. Earlier in vitro studies detected zanamivir resistance due to an E119G mutation following passage of influenza A N2 (14) and N9 viruses (6) and influenza B virus (4) in the presence of zanamivir, but this had not been previously detected in an influenza A N1 virus. The mutation had previously been introduced into an N1 NA using site-directed mutagenesis, although viruses could not be easily grown (2, 35), supporting the data from this study that showed the E119G recombinant mutants had significantly compromised growth compared to the wild type. The D198G NA mutation detected in the Vn/1203 strain following passage in zanamivir had not been previously identified in an N1 NA. N1 sequences on GenBank included two A(H1N1) and two A(H5N1) strains with D198N and D198H NA mutations. A D198N NA mutation had been detected previously in influenza B viruses from an oseltamivir-treated immunocompromised patient (12) and from three patients prior to and following oseltamivir treatment (15). A D198E mutation had also been detected in an influenza B virus from an untreated infant patient (22). Both of the zanamivir-selected viruses also contained HA mutations in residues that had previously been implicated in receptor binding in A(H5N1) strains (K234Q and K205E; H5 numbering) (29). The HA mutation in the oseltamivir-selected Laos/26 was at the same receptor-binding residue observed in the zanamivir-selected Vn/1203 strain, although with a different substitution (K234N).
The degree to which a given increase in the IC50 of an influenza virus strain predicts clinical failure of NA inhibitor treatment is uncertain, and this may be further complicated in the case of influenza A(H5N1) virus infections, where the virus may spread systemically (8). Previous studies indicated that higher than normal doses of oseltamivir (e.g., 150 mg twice daily compared with the normal adult dose of 75 mg twice daily) may be necessary for effective treatment of A(H5N1) virus infections (11). While the viruses with the single H274Y mutation had oseltamivir IC50s that were similar to the expected maximum concentration in plasma following normal oseltamivir dosing (348 ng/ml; 1,224 nM) (26), the IC50s of viruses with the dual H274Y/I222V or H274Y/I222M mutations far exceed expected oseltamivir plasma concentrations. However, the dual H274Y/I222V/M mutant viruses had peramivir IC50s that were well below the expected peramivir plasma concentrations, reported to exceed 10,000 ng/ml (30,488 nM) following a 300-mg parenteral dose (3). The E119G mutation (zanamivir IC50s, 677.3 and 868.1 nM for Laos/26 and Vn/1203, respectively) would be expected to result in a reduction of the clinical efficacy of zanamivir, although median concentrations of this drug in sputum between 6 and 24 h postdose are reported to be from 1,336 to 47 ng/ml (4,020 to 142 nM) (25).
Previous in vitro studies involving the serial MDCK passage of seasonal influenza virus strains in the presence of an NA inhibitor (12, 32) have generated mutations that have also been recovered from drug-treated individuals (13, 23, 33, 34), suggesting that such methods can be used to predict mutants that occur in vivo. However, further studies are necessary to evaluate the in vivo fitness of the A(H5N1) NA inhibitor-resistant viruses derived in this study. The recent detection of large numbers of A(H1N1) viruses with an H274Y mutation circulating in the community in the absence of drug pressure (20) has demonstrated that viruses can carry this mutation while maintaining a high level of fitness. It would be particularly interesting to investigate the fitness of the dual H274Y/I222M A(H5N1) mutant virus in a ferret model, as well as assessing the impact on viral fitness of introducing a range of I222 mutations into the existing H274Y A(H1N1) mutant virus currently circulating in the human population. The in vitro data from this study found no difference in growth between the dual H274Y/I222M mutant and the single H274Y mutant, although both had reduced growth compared to the wild-type virus. This study has highlighted the I222 N1 residue as a key amino acid to monitor, given its ability, in combination with other NA inhibitor resistance mutations, to increase drug resistance. Oseltamivir prophylaxis and treatment dosing regimens have previously been assessed in ferrets for two different A(H5N1) viruses, but NA inhibitor-susceptible viruses were used. It will be informative to conduct similar studies with NA inhibitor-resistant A(H5N1) viruses, such as those generated in this study, to determine the effectiveness of treatment and prophylaxis, not only for oseltamivir, but also for zanamivir and peramivir. Such information will be important in the event of a resistance mutation occurring in a circulating A(H5N1) pandemic strain. The NA inhibitors remain essential drugs for the prophylaxis and treatment of influenza infection, but further work is necessary to understand how effective these agents might be against a novel NA inhibitor-resistant influenza A(H5N1) virus in a pandemic scenario.
Acknowledgments
This study was supported by Australian National Health and Medical Research Council award 400595. The Melbourne WHO Collaborating Centre for Reference and Research on Influenza is supported by the Australian Government Department of Health and Ageing.
We thank Robert Shaw, WHO Collaborating Centre for Reference and Research on Influenza, Melbourne, Australia, for experimental assistance; Deborah Middleton and Sue Lowther, Australian Animal Health Laboratory, for provision of laboratory space during the virus growth experiments; and Michael Parker, St. Vincent's Institute of Medical Research, for assistance with structural modeling.
Footnotes
Published ahead of print on 3 August 2009.
REFERENCES
- 1.Abdel-Ghafar, A. N., T. Chotpitayasunondh, Z. Gao, F. G. Hayden, D. H. Nguyen, M. D. de Jong, A. Naghdaliyev, J. S. Peiris, N. Shindo, S. Soeroso, and T. M. Uyeki. 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261-273. [DOI] [PubMed] [Google Scholar]
- 2.Abed, Y., M. Baz, and G. Boivin. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antivir. Ther. 11:971-976. [PubMed] [Google Scholar]
- 3.Alexander, W. J., L. A. Harman, P. J. Collis, J. Elder, J. M. Kilpatrick, G. Atiee, and E. Mead. 2007. Nasal and pharyngeal concentrations of peramivir following intramuscular and intravenous administration in health volunteers. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., poster A-1410.
- 4.Barnett, J. M., A. Cadman, F. M. Burrell, S. H. Madar, A. P. Lewis, M. Tisdale, and R. Bethell. 1999. In vitro selection and characterisation of influenza B/Beijing/1/87 isolates with altered susceptibility to zanamivir. Virology 265:286-295. [DOI] [PubMed] [Google Scholar]
- 5.Baz, M., Y. Abed, J. McDonald, and G. Boivin. 2006. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin. Infect. Dis. 43:1555-1561. [DOI] [PubMed] [Google Scholar]
- 6.Blick, T. J., T. Tiong, A. Sahasrabudhe, J. N. Varghese, P. M. Colman, G. J. Hart, R. C. Bethell, and J. L. McKimm-Breschkin. 1995. Generation and characterization of an influenza virus neuraminidase variant with decreased sensitivity to the neuraminidase-specific inhibitor 4-guanidino-Neu5Ac2en. Virology 214:475-484. [DOI] [PubMed] [Google Scholar]
- 7.Collins, P. J., L. F. Haire, Y. P. Lin, J. Liu, R. J. Russell, P. A. Walker, J. J. Skehel, S. R. Martin, A. J. Hay, and S. J. Gamblin. 2008. Crystal structures of oseltamivir-resistant influenza virus neuraminidase mutants. Nature 453:1258-1261. [DOI] [PubMed] [Google Scholar]
- 8.de Jong, M. D., C. P. Simmons, T. T. Thanh, V. M. Hien, G. J. Smith, T. N. Chau, D. M. Hoang, C. N. Van Vinh, T. H. Khanh, V. C. Dong, P. T. Qui, B. Van Cam, D. Q. Ha, Y. Guan, J. S. Peiris, N. T. Chinh, T. T. Hien, and J. Farrar. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Jong, M. D., T. T. Tran, H. K. Truong, M. H. Vo, G. J. Smith, V. C. Nguyen, V. C. Bach, T. Q. Phan, Q. H. Do, Y. Guan, J. S. Peiris, T. H. Tran, and J. Farrar. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667-2672. [DOI] [PubMed] [Google Scholar]
- 10.DeLano, W. L. 2009. PYMOL. DeLano Scientific, Palo Alto, CA.
- 11.Govorkova, E. A., N. A. Ilyushina, D. A. Boltz, A. Douglas, N. Yilmaz, and R. G. Webster. 2007. Efficacy of oseltamivir therapy in ferrets inoculated with different clades of H5N1 influenza virus. Antimicrob. Agents Chemother. 51:1414-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gubareva, L. V. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199-203. [DOI] [PubMed] [Google Scholar]
- 13.Gubareva, L. V., L. Kaiser, M. N. Matrosovich, Y. Soo-Hoo, and F. G. Hayden. 2001. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J. Infect. Dis. 183:523-531. [DOI] [PubMed] [Google Scholar]
- 14.Gubareva, L. V., M. J. Robinson, R. C. Bethell, and R. G. Webster. 1997. Catalytic and framework mutations in the neuraminidase active site of influenza viruses that are resistant to 4-guanidino-Neu5Ac2en. J. Virol. 71:3385-3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatakeyama, S., N. Sugaya, M. Ito, M. Yamazaki, M. Ichikawa, K. Kimura, M. Kiso, H. Shimizu, C. Kawakami, K. Koike, K. Mitamura, and Y. Kawaoka. 2007. Emergence of influenza B viruses with reduced sensitivity to neuraminidase inhibitors. JAMA 297:1435-1442. [DOI] [PubMed] [Google Scholar]
- 16.Hauge, S. H., S. Dudman, K. Borgen, A. Lackenby, and O. Hungnes. 2009. Oseltamivir-resistant influenza viruses A (H1N1), Norway, 2007-08. Emerg. Infect. Dis. 15:155-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffmann, E., S. Krauss, D. Perez, R. Webby, and R. Webster. 2002. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 20:3165. [DOI] [PubMed] [Google Scholar]
- 18.Hung, H. C., C. P. Tseng, J. M. Yang, Y. W. Ju, S. N. Tseng, Y. F. Chen, Y. S. Chao, H. P. Hsieh, S. R. Shih, and J. T. Hsu. 2009. Aurintricarboxylic acid inhibits influenza virus neuraminidase. Antivir. Res. 81:123-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurt, A. C., and I. G. Barr. 2008. Influenza viruses with reduced sensitivity to the NA inhibitor drugs in untreated young children. Commun. Dis. Intell. 32:57-62. [DOI] [PubMed] [Google Scholar]
- 20.Hurt, A. C., J. Ernest, Y. Deng, P. Iannello, T. G. Besselaar, C. Birch, P. Buchy, M. Chittaganpitch, S. C. Chiu, D. E. Dwyer, A. Guigon, B. Harrower, I. P. Kei, T. Kok, C. Lin, K. McPhie, A. Mohd, R. Olveda, T. Panayotou, W. Rawlinson, L. Scott, D. Smith, H. D'Souza, N. Komadina, R. Shaw, A. Kelso, and I. G. Barr. 2009. Emergence and spread of oseltamivir-resistant A(H1N1) influenza viruses in Oceania, South East Asia and South Africa. Antivir. Res. 83:90-93. [DOI] [PubMed] [Google Scholar]
- 21.Hurt, A. C., H. T. Ho, and I. Barr. 2006. Resistance to anti-influenza drugs: adamantanes and neuraminidase inhibitors. Expert Rev. Anti. Infect. Ther. 4:795-805. [DOI] [PubMed] [Google Scholar]
- 22.Hurt, A. C., P. Iannello, K. Jachno, N. Komadina, A. W. Hampson, I. G. Barr, and J. L. McKimm-Breschkin. 2006. Neuraminidase inhibitor-resistant and -sensitive influenza B viruses isolated from an untreated human patient. Antimicrob. Agents Chemother. 50:1872-1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ison, M. G., L. V. Gubareva, R. L. Atmar, J. Treanor, and F. G. Hayden. 2006. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J. Infect. Dis. 193:760-764. [DOI] [PubMed] [Google Scholar]
- 24.Monto, A. S., J. L. McKimm-Breschkin, C. Macken, A. W. Hampson, A. Hay, A. Klimov, M. Tashiro, R. G. Webster, M. Aymard, F. G. Hayden, and M. Zambon. 2006. Detection of influenza viruses resistant to neuraminidase inhibitors in global surveillance during the first 3 years of their use. Antimicrob. Agents Chemother. 50:2395-2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng, A. W., S. Milleri, and D. S. Stein. 2000. Direct measurement of the anti-influenza agent zanamivir in the respiratory tract following inhalation. Antimicrob. Agents Chemother. 44:1974-1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roche Pharmaceuticals. 2006. Tamiflu (oseltamivir carboxylate) capsules and for oral suspension. Package insert. Hoffmann-La Roche Inc., Nutley, NJ. http://www.tamiflu.com.
- 27.Russell, R. J., L. F. Haire, D. J. Stevens, P. J. Collins, Y. P. Lin, G. M. Blackburn, A. J. Hay, S. J. Gamblin, and J. J. Skehel. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443:45-49. [DOI] [PubMed] [Google Scholar]
- 28.Sheu, T. G., V. M. Deyde, M. Okomo-Adhiambo, R. J. Garten, X. Xu, R. A. Bright, E. N. Butler, T. R. Wallis, A. I. Klimov, and L. V. Gubareva. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob. Agents Chemother. 52:3284-3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stevens, J., O. Blixt, T. M. Tumpey, J. K. Taubenberger, J. C. Paulson, and I. A. Wilson. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404-410. [DOI] [PubMed] [Google Scholar]
- 30.Ungchusak, K., P. Auewarakul, S. F. Dowell, R. Kitphati, W. Auwanit, P. Puthavathana, M. Uiprasertkul, K. Boonnak, C. Pittayawonganon, N. J. Cox, S. R. Zaki, P. Thawatsupha, M. Chittaganapitch, R. Khontong, J. M. Simmerman, and S. Chunsutthiwat. 2005. Probable person to person transmission of avian influenza A (H5N1). N. Engl. J. Med. 352:333-340. [DOI] [PubMed] [Google Scholar]
- 31.Wang, M. Z., C. Y. Tai, and D. B. Mendel. 2000. Characterisation of an influenza A virus variant selected in vitro in the presence of the neuraminidase inhibitor, GS4071. Antivir. Res. A 60:46. [Google Scholar]
- 32.Wang, M. Z., C. Y. Tai, and D. B. Mendel. 2002. Mechanism by which mutations at His274 alter sensitivity of influenza A virus N1 neuraminidase to oseltamivir carboxylate and zanamivir. Antimicrob. Agents Chemother. 46:3809-3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weinstock, D. M., L. V. Gubareva, and G. Zuccotti. 2003. Prolonged shedding of multidrug-resistant influenza A virus in an immunocompromised patient. N. Engl. J. Med. 348:867-868. [DOI] [PubMed] [Google Scholar]
- 34.Whitley, R. J., F. G. Hayden, K. S. Reisinger, N. Young, R. Dutkowski, D. Ipe, R. G. Mills, and P. Ward. 2001. Oral oseltamivir treatment of influenza in children. Pediatr. Infect. Dis. J. 20:127-133. [DOI] [PubMed] [Google Scholar]
- 35.Yen, H. L., N. A. Ilyushina, R. Salomon, E. Hoffmann, R. G. Webster, and E. A. Govorkova. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418-12426. [DOI] [PMC free article] [PubMed] [Google Scholar]