Abstract
In a randomized controlled trial, behavioral day treatment, including contingency management (CM+), was compared to contingency management components alone (CM). All 206 cocaine dependent, homeless participants received a furnished apartment with food and work training/employment contingent on drug-negative urine tests. CM+ also received cognitive behavioral therapy, therapeutic goal management, and other intervention components. Results revealed that CM+ treatment attendance and abstinence were not significantly different from CM during 24 weeks of treatment. After treatment and contingencies ended, however, CM+ showed more abstinence than CM, indicating a delayed effect of treatment from 6 to 18 months. CM+ had more consecutive weeks abstinent across 52 weeks, but not during active treatment. We conclude that CM alone may be viable as initial care for cocaine dependent homeless persons. That CM+ yields more durable abstinence indicates it may be appropriate as stepped up care for clients not responding to CM. Clinical Trials.gov #NCT00368524
1. Introduction
The estimated number of U. S. homeless persons during any week in 1996 ranged from 440,000 to 840,000 (Burt & Aron, 2000). In the first nationwide study completed in a decade, 744,000 homeless persons were found at a single point in time in 2005, and far more persons experience homelessness over the course of a year (Research Reports on Homelessness: Homelessness Counts, 2007). In addition to systemic factors (e.g. low-cost housing availability) and individual factors (e.g. severe mental illness), substance abuse augments the risk for both homelessness (Corrigan & Anderson, 1984; Koegel, Burnam, & Farr, 1988; Rosenheck et al., 1989) and major health problems (Martens, 2001; Plumb, 1997; Smereck & Hockman, 1998). A recent large study of risk factors for homelessness in a cohort of 10,340 persons being treated for schizophrenia, bipolar disorder, or major depression, found that 15% were homeless (Folsom et al., 2005). In a recent study of 185,870 tuberculosis cases reported in the National TB Surveillance System, 1994–2003, 11,369 were homeless. Compared to non-homeless, homeless persons with TB had a higher prevalence of substance abuse, and TB in the homeless was more likely to be infectious. Additionally, 34% had co-infection with HIV (Haddad, Wilson, Ijaz, Marks, & Moore, 2005). Currently homeless were almost twice as likely to have a lifetime diagnosis of substance use disorder than the never homeless (Toro et al., 1995). The estimated 437,000 crack users among the 1.7 million current users of cocaine (SAMHSA, 2000) likely shows that crack use may trigger episodes of homelessness and contribute to their health problems. Cocaine abuse and its treatment represent a special treatment concern, in part because of the absence of any viable pharmacotherapy like those available for alcohol and opiate dependence. Among homeless persons who sought addiction treatment in 2004 (175,000 admissions), 17% reported cocaine as the primary substance of abuse (SAMSHA, 2006). Effective treatment for cocaine dependence among homeless persons has potential to improve health, social functioning, and may assist in the return to housed status (Kertesz et al., 2006).
Our previous treatment trials with a homeless, non-psychotic, dually diagnosed, crack cocaine dependent population, yielded substantial retention and good psychiatric diagnostic and abstinence outcomes. The treatment model, developed iteratively over three trials, has included contingency managed housing, employment, and work training, with as many as 6-½ hours of behavioral day treatment per day (Milby et al., 1996; 2000; 2003; Schumacher, 2003). Trial data show that the inclusion of housing as part of the overall treatment program improves both retention and abstinence (Milby et al., 2000; Milby, Schumacher, Wallace, Freedman, & Vuchinich, 2005b). Moreover, analyses that controlled for attendance suggested that requiring abstinence in exchange for continued housing further enhanced abstinence outcomes, compared to the provision of housing without such a requirement (Milby et al., 2005b).
The rationale for this study involved two core concepts. First, though we have developed and replicated an effective treatment for cocaine dependence in homeless persons, its cost and complexity are barriers to widespread implementation. To address these barriers, we extracted contingency managed components of this effective intervention, shown in a previous study to be efficacious when added to behavioral day treatment (Milby et al., 2000), and utilized them as an “abbreviated” – that is, a less complicated and less expensive – intervention which could potentially serve as a “first step” treatment, reserving more complex interventions for persons not improving with abbreviated care. The extracted components offered as abbreviated treatment were: contingency managed housing, job training and work with transportation services, which together were called Contingency Management (CM). This CM abbreviated treatment was compared, in a randomized controlled clinical trial, to what we called CM+ which consisted of these same CM components plus our behavioral day treatment.
Second, the appeal of an abbreviated contingency managed intervention is likely to be influenced by the durability of therapeutic response. The treatment literature reflects concerns over the persistence of behavior change resulting from CM approaches, especially after contingencies for reinforcement cease or contingent reinforcement is greatly diminished. Relatively few studies have measured outcomes 12 months or more after termination of active treatments and fewer studies have found evidence of persistent benefit (Higgins, Wong, Badger, Ogden, & Dantona, 2000). This trial attempted to address this gap in the literature by observing participants for a full year after treatment. We judged that if the abbreviated CM treatment proved similarly effective to, or even slightly less effective than the “full” intervention in a comparative trial, then providers and policy makers could consider this for an initial treatment in a stepped care program. The more intensive behavioral day treatment (CM+), requiring approximately double the labor and cost, would be reserved for clients with refractory problems.
The purpose of this randomized trial was to examine both the relative effectiveness of the two interventions and their respective cost effectiveness. This paper addresses the question of relative effectiveness in terms of treatment exposure, retention, and proximal and distal measured abstinence. Ongoing work will address the results in the context of a detailed enumeration of costs, cost effectiveness, and cost benefit analyses, with attention to long term outcomes. Thus, the cost-effectiveness and cost benefits aspects of the trial will be the subject of a separate paper and are not reported here.
Though we hypothesized that CM+ would show better abstinence and retention outcomes, we expected considerable abstinence improvement to be observed in CM participants. Accordingly, we analyzed results from the two treatment phases, and across six months of follow-up, to test whether an abbreviated CM treatment could produce clinically meaningful drug abstinence that was no more than 25% inferior to the full treatment (CM+). To test for effectiveness of CM relative to CM+, we hypothesized that abstinence achieved by CM that was 75% or greater than outcomes obtained for CM+ would be considered clinically substantial and non-inferior to CM+ as an abbreviated care outcome. The rationale for this clinical judgment was based on the fact that CM was a much less complex intervention that involved about half the treatment time and costs. Additionally, previous trials with CM+ yielded abstinence levels above 70%, so that a stepped care outcome of 75% of these outcomes would be clinically substantial and render it more likely to be adopted as an initial intervention for this population.
2. Material and Methods
2.1 Participants and Recruitment
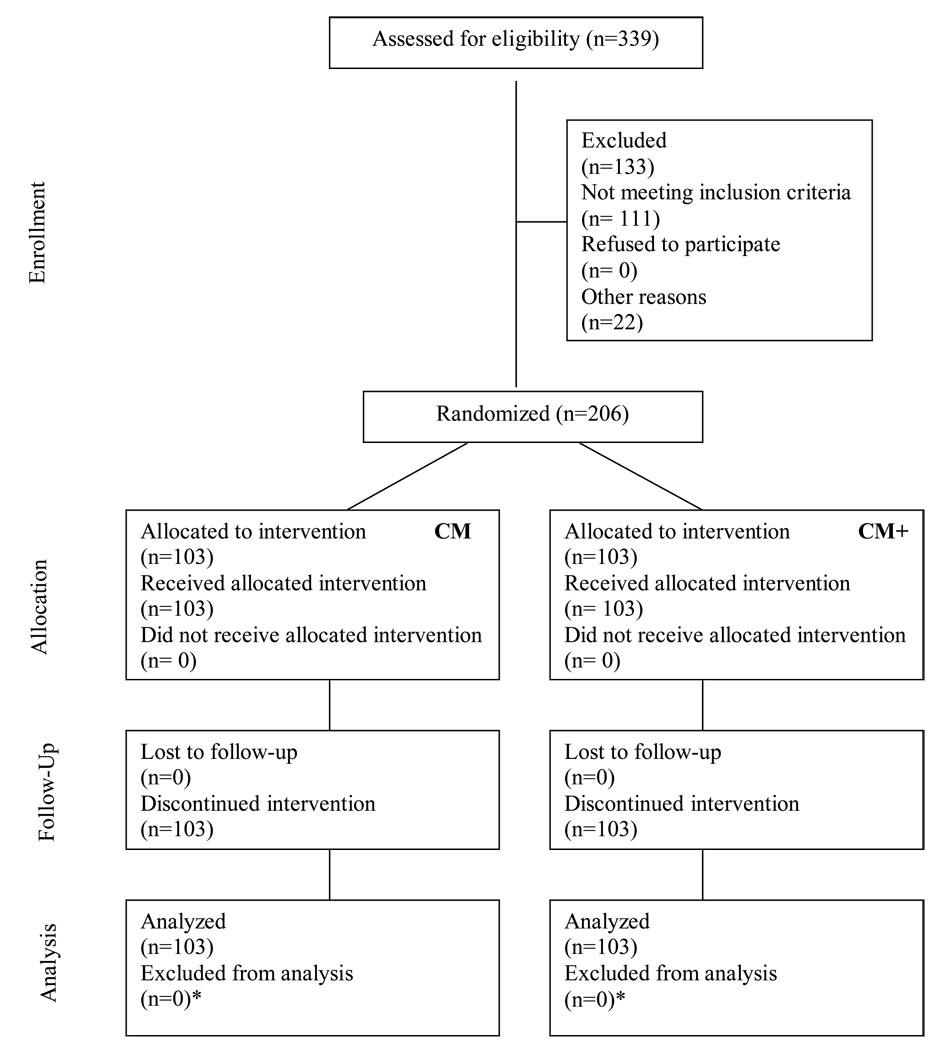
A CONSORT format flow chart of participants’ movement through the study is found in Figure 1. Applicants were recruited from Birmingham Healthcare (BHC), the largest agency serving homeless persons in Alabama. Applicants were interviewed by BHC staff regarding the homelessness criteria and the likely presence of a cocaine use disorder. Eligible applicants were then formally assessed for inclusion and exclusion criteria by research staff and were either processed for study entry or referred back to BHC for other services. Of 339 applicants initially screened and referred for possible study participation, 206 met study criteria, which included: McKinney Act criteria for homelessness (McKinney, 1987); a diagnosis of cocaine dependence according to the Diagnostic and Statistical Manual, version IV (DSM-IV), with self reported cocaine use within the last two weeks; significant psychological distress, as indicated by a score of 70 (two SD’s above the mean) on one or more Brief Symptom Inventory (BSI) scales (Derogatis, 1977; Derogatis & Cleary, 1977); willingness to participate in the study, and no plans to move from the Birmingham area for 18 months. Exclusion criteria were: cognitive impairment precluding informed consent or if persons required immediate inpatient medical treatment. All procedures were approved by the UAB Institutional Review Board. There were 103 assigned to CM and 103 to CM+. Subject demographics are reported in Table 1.
Figure 1.
Flow chart of participant movement through the study from initial screening, follow-up, and data analysis employing the CONSORT format.
*No participant data were excluded from the analysis because missing urine tests were included as drug positive. Methods for coping with missing data are described in the outcomes section. Data are summarized in Table 2.
Table 1.
Characteristics of the participant sample compared by group CM vs. CM+
| Characteristic | CM | CM+ | p* | ||
|---|---|---|---|---|---|
| M (SD) | n (%) | M (SD) | n (%) | ||
| Male | 77 (74.8) | 73 (70.9) | .64 | ||
| Female | 26 (25.2) | 30 (29.1) | |||
| Age, years | 39.5 (7.2) | 40.6 (7.1) | .27 | ||
| African American | 95 (92.2) | 99 (96.1) | .37 | ||
| Caucasian | 8 (7.8) | 4 (3.9) | |||
| Drug of Abuse, years | |||||
| Alcohol | 17.7 (10.4) | 18.5 (10.2) | .59 | ||
| Cannabis | 11.0 (9.4) | 10.2 (9.7) | .59 | ||
| Cocaine | 12.4 (7.0) | 11.4 (6.0) | .29 | ||
| Education, years | 11.7(1.7) | 12.2 (1.5) | .04* | ||
| Homeless, months | 32.8 (47.9) | 27.2 (46.4) | .40 | ||
| Longest Full-time Job, months | 52.5 (41.2) | 58.5 (57.2) | .39 | ||
2.2 Phases of Treatment and Assessment Procedure
There were four study phases. Phases I-II included active treatment during weeks 1–24. Phase III involved aftercare and post treatment follow-up during weeks 25–52 and Phase IV involved aftercare and less frequent follow-up in weeks 53–78.
Retention in treatment and substance use were assessed by obtaining observed urine specimens and testing with the OnTrak TestStik™ Radioimmunoassay (Varian Inc.). Retention in the study was measured as the time to the last urine supplied during the first 24 weeks. At study entry participants were tested for cocaine, marijuana, alcohol, benzodiazepines, opiates and amphetamine. They were given a $25 backpack containing personal hygiene items for the baseline assessment. Subsequent assessments consisted of observed urine tests for cocaine, marijuana, and alcohol obtained Monday, Wednesday, and Friday each week from weeks 1–24 to assess drug use and impose contingencies for housing and work incentives. For those participants who tested positive for benzodiazepines, opiates or amphetamine at baseline, tests for these drugs were added during weekly tests and monthly during follow-up. From weeks 25–52, participants were tested randomly once a week and paid $10 for urine specimens. In weeks 53–78, participants were tested randomly once every two months and paid $50 for each specimen. A follow-up tracker made continuous efforts to locate and re-engage those who dropped from treatment or were lost to follow-up. Attendance, i.e. exposure to treatment, was assessed by a counselor-verified daily service log recorded in 15 minute epochs.
2.3 Design
The study was a two-arm randomized controlled trial, comparing the abbreviated treatment model (offering contingency-managed housing, vocational training and work therapy, i.e. CM) to the full treatment model (CM+), which included the same interventions plus extensive behavioral day treatment (detailed below). Random draw procedures equalized the distribution of women to the groups and assured that the trial arms were of similar size. Because of the intervention design, trial arm assignment was not concealed from participants. Upon establishing study eligibility and obtaining informed consent, participants were immediately given study entry urine tests, and then randomized. Participants were recruited, randomized, and treated from 2001 to 2004. Continuous follow-ups via urine tests were conducted during the two study phases after treatment, 6–12, and 13–18 months. Weekly follow-up for Phase III occurred during weeks 24–52, and bi-monthly follow-up occurred for Phase IV across months 13–18.
2.4 Intervention Components Common to Both Groups
Participants in both trial arms were transported daily to and from study-provided housing (or shelters or other domiciles) to their intervention each day. Transportation was also provided to training, work, job interviews and paid employment sites. Noon meals were served to clients daily except Wednesday, which was not a full intervention day. Both groups attended AIDS/HIV information and risk reduction group sessions.
The contingency-managed housing intervention consisted of providing a furnished apartment with food and flatware to each new client during the first week of intervention. During treatment weeks 2–8, housing was provided free but contingent on evidence of continued drug abstinence, demonstrated by urine tests administered Monday, Wednesday, and Friday. Participants were moved to a shelter or other housing within six hours of a drug-positive urine test. Return to the housing unit was conditional on three sequential negative urines. Abstinent contingent housing was provided for a modest rent paid from program stipends during weeks 9–24. During this period, members of both groups who sustained abstinence were referred to Shelter Plus Care, a locally administered transitional housing program funded by the United States Department of Housing and Urban Development and common in major cities. In Birmingham, the locally-set requirements for entry to Shelter Plus Care included four months of continuous abstinence. A missed or drug-positive urine placed participants at the end of the local Shelter Plus Care waiting list. From weeks 25 to 78 (18 months), a period considered to be “aftercare,” abstinent contingent housing was only provided on a space available basis for a modest rent. During this period a missed or drug-positive urine test caused permanent removal from this housing.
The vocational training intervention began in week one and was scheduled for 3.5 hrs. Monday, Tuesday, Thursday, and Friday, in the morning for CM and in the afternoon for CM+. It consisted of educational and vocational assessment, and options for earning stipends for computer and office machine training or for work renovating offices and housing for homeless persons. Computer/office training was conducted at an 11-station computer training lab with internet and State employment listing access, telephone, fax machine and copier. Phones were set up for clients to make job related calls and receive messages. More work preparation occurred in months 3–4 with an increased emphasis on Job Club(Azrin & Besalel, 1983; Azrin, Flores, & Kaplan, 1975), an intervention for obtaining employment, promoting job search, interviewing practice, and job retention skills in months 5–6. Hourly pay of $1.25 started the first day. Every workday thereafter, the hourly rate could increase by $1.00 up to a maximum of $5.25 per hour if urine tests were negative for drugs and alcohol, and behavior was 100% in compliance with worksite guidelines (i.e., arrived to worksite on time, completed shift, and exhibited non-confrontational behavior). If a participant provided a drug or alcohol positive urine, failed to provide a mandatory urine, or did not comply with work guidelines, the stipend rate was reset to $1.25 per hour, with subsequent opportunity to increase by $1.00 per hour for each day they met the abstinence contingency and was in 100% compliance with work guidelines. Actual earnings varied between $4.28 up to a maximum of $18.38 per day depending on participants’ hourly rates. Partial earnings up to $20 were distributed weekly via a Wal-Mart debit card. Any excess earnings were saved and held on account by the program for later use as apartment rent deposits or other uses. Once per week, both groups used their Wal-Mart debit cards on a supervised shopping trip. Once per month both groups attended a monthly transition ceremony with lunch. At the ceremony, transitions and achievements during each phase were recognized with certificates and a person who was successful in recovery addressed the group.
To summarize, both groups experienced the same contingency consequences of housing loss and training program loss with stipend reset for any missed or drug positive urine test or inappropriate work behaviors. They also received the same contingency benefit for sustained abstinence and work appropriate behaviors with continued access to housing and continued access to work stipends at the maximum rate. For both groups, formal treatment ended with Phase II, i.e. after 24 weeks. Participants were encouraged to continue in aftercare provided by the program or in more convenient community locations closer to their new employment or housing, but this was not required. During study Phases III and IV there were no contingencies in effect and housing and work experiences were not provided, but participants were followed and tested for abstinence outcomes.
2.5 Intervention Unique to CM
After completion of the 6 month intervention, CM participants were referred to BHC for once per week group aftercare counseling. Aftercare participation with negative urines was required for referral to federal Shelter Plus Care housing.
2.6 Intervention Unique to CM+ in Phase I, (weeks 1–8)
The CM+ group received all vocational procedures received by CM, except they were scheduled in the afternoon. Unique to CM+ was participation in the manualized behavioral day treatment with incentives utilized in previous studies. This day treatment was scheduled in the mornings daily except Wednesday. It started with behavioral assessment and objective treatment goal setting for five common problem domains: addiction, homelessness, unemployment, lack of non-drug-related social and recreational activities, and mental/health and emotional problems. These goals were reviewed and revised each week in goal review and goal development sessions. Goal attainment was reinforced with a $7.50 Wal-Mart debit card deposit for 80% goal attainment and $15.00 for 100% goal attainment. Clients spent their funds in the once weekly supervised group shopping trip to Wal-Mart. Other group treatment sessions were: a daily patient-conducted morning meeting; emotional processing group; drug and alcohol education; relapse prevention; anger management and assertiveness training; role playing; rational evaluation of mood and emotions, relaxation and stress management training, healthy decision making, healthy communication, healthy self-esteem, weekend planning, recreational outings organized within the treatment context, and recreation/art therapy. In addition clients met with their individual counselor for .75 –1.0 hr or more each week.
2.7 Intervention Unique to CM+ in Phase II (weeks 9–24)
During Phase II, CM+ clients attended behavioral day treatment aftercare group meetings once per week which supported continued goal development and attainment but without tangible reinforcement for goal attainment. Clients continued individual counseling as needed.
2.8 Outcomes
Outcomes were retention in treatment, attendance during treatment, and three measures of abstinence based on the urine tests scheduled three times weekly during active treatment weeks 1–24, and randomly once per week throughout aftercare and follow-ups during weeks 25–52, and at three random times during months 13–18. Retention in treatment was measured as the time from treatment entry to the last urine supplied during the first 24 weeks during active treatment. Attendance during treatment outcomes, i.e. exposure to treatment, was average quarter-hour units of treatment per day.
The three abstinence outcomes each measure a slightly different construct. First, the individual urine measures provide an indication of the point prevalence of abstinence for the group at a point in time. Second, the proportion of clean urines exhibited by an individual over a period of time (typically one or more of the treatment phases), provides a measure of overall abstinence over that time period. Third, the longest string of consecutive weeks abstinent for an individual provides a measure of that individual’s ability to initiate and sustain abstinence.
For all three abstinence measures, missing drug tests were coded as: assumed drug-positive; excused and assumed drug-negative, (for example, on occasions where patients were hospitalized or attended a family funeral out of town); or administratively missing. Administratively missing was coded when tests were scheduled but untested by staff due to computer or scheduling problems, or tests scheduled for clinic holidays. Because CM+ spent twice as much time in Phase I treatment, from 7:30 am to 4 pm except for a half day on Wednesdays, this group had much less time to meet important appointments for benefits, health care, court and probation appointments etc. which were important for treatment goal attainment and recovery progress. The CM group had each afternoon to schedule and meet these appointments, thus needing fewer excused absences.
Both excused and assumed drug-negative and administratively missing urines were treated as randomly missing; they were not counted as disruptive to a series of consecutive clean urines, nor were they included in analyses of point prevalence or proportion clean urines. For the individual urine measurements, weekly prevalence of abstinence was generated by calculating the proportion of clean urines obtained during each week among the total number of urines not considered to be missing at random during the week.
2.9 Statistical Analysis Procedures
An intention-to-treat analysis was used for all outcomes. A Kaplan Meier model survival analysis with an associated log rank test was used to compare retention in the two groups. A two-sample t-test, with Sattherwaite correction to account for unequal variances, was used to compare the amount of treatment activity to which participants were exposed in the two groups. A generalized estimating equation (GEE) extension of generalized linear models was used to assess differences between groups and whether abstinence was modified by attendance as reported in our previous work (Milby et al., 2005b). The first models estimated abstinence as a function of treatment group and study phase, (I, II, III, IV), while the second examined abstinence as a function of treatment group and study phase while controlling for attendance. Wald tests, based on the Liang and Zeger’s (1986) procedure, were used to test for effects of group, study phase, and attendance. For the outcomes of consecutive weeks abstinent in subject-level proportion abstinence over a fixed time period, ANOVA models tested for differences between groups, with and without control for attendance.
We tested the notion of non-inferiority of CM to CM+ abstinence with two outcomes. The first, more sensitive to harm reduction, was percent urine tests abstinent by treatment phase for each group using a GEE model. The other, more sensitive to sustained abstinence effects, was average longest consecutive weeks abstinent obtained for each group using ANOVA models. ANOVA models tested the non-inferiority of CM compared to CM+ by examining the one-sided t-test for the difference between the CM mean and 75% of the CM+ mean, with a significant test that this difference is 0 or greater supporting the hypothesis, while the GEE models utilized a similar procedure with a one sided z-test.
3. Results
Demographic data partitioned by trial arm and examined for significant differences are presented in Table 1. As can be seen there were no significant differences between groups after random assignment except for years of education. The CM+ trial arm had .5 years more education. Race was classified by participants themselves and assessed to assure minority representation.
3.1 Retention and Attendance Outcomes
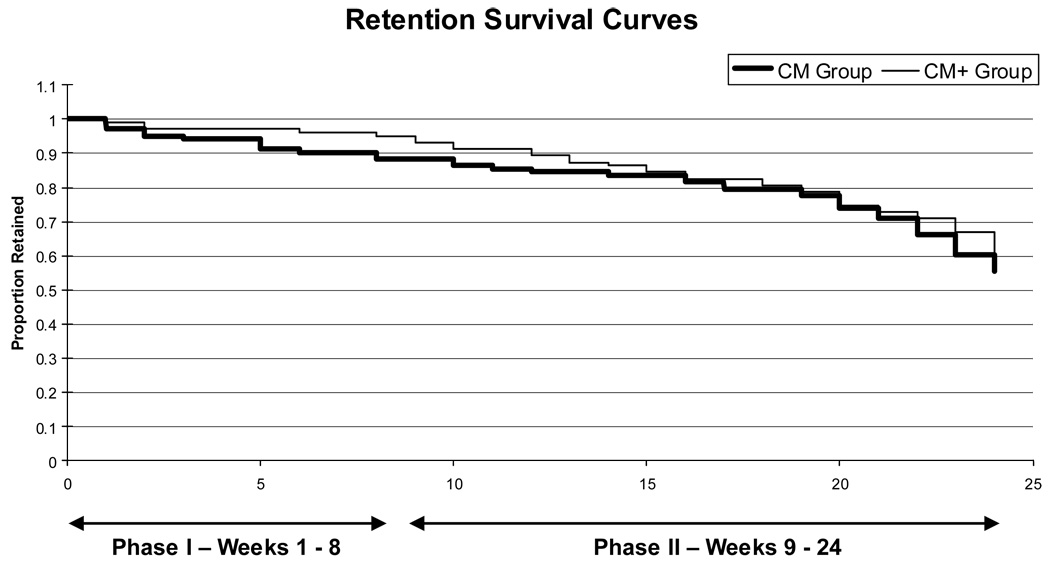
Treatment retention results from a Kaplan Meier model survival analysis are presented in Figure 2. Mean 24-week retention for CM was 19.7 weeks (s.e.=0.72 weeks) and for CM+ was 20.4 weeks (s.e.=0.62 weeks), (p=.45). Median survival times for both groups were the full 24 week treatment period.
Figure 2.
Treatment retention by week from 0 –24 weeks compared across the two groups, CM vs. CM+, graphed as Kaplan Meier model retention survival curves.
There were large and significant attendance differences (measured in 15 minute units of treatment) in the two arms, during both study Phases I and II, an expected result since CM+ attended both CM and CM+ treatment components mornings and afternoons. A second analysis was conducted based on only CM components common to both groups. During Phase I, CM was exposed on average to 273 (SD=148) quarter-hour units of CM treatment, while the CM+ was exposed to an average of 315 (SD=166) units, a difference favoring CM+ (t=2.11, df=204, p=0.036). During Phase II, the CM group was exposed on average to 709 (SD=448) quarter-hour units of treatment, while the CM+ group was exposed to an average of 835 (SD=503) units, a weak difference favoring CM+ (t=1.90, df=204, p=0.059).
3.2 Abstinence Prevalence Across Treatment Phases
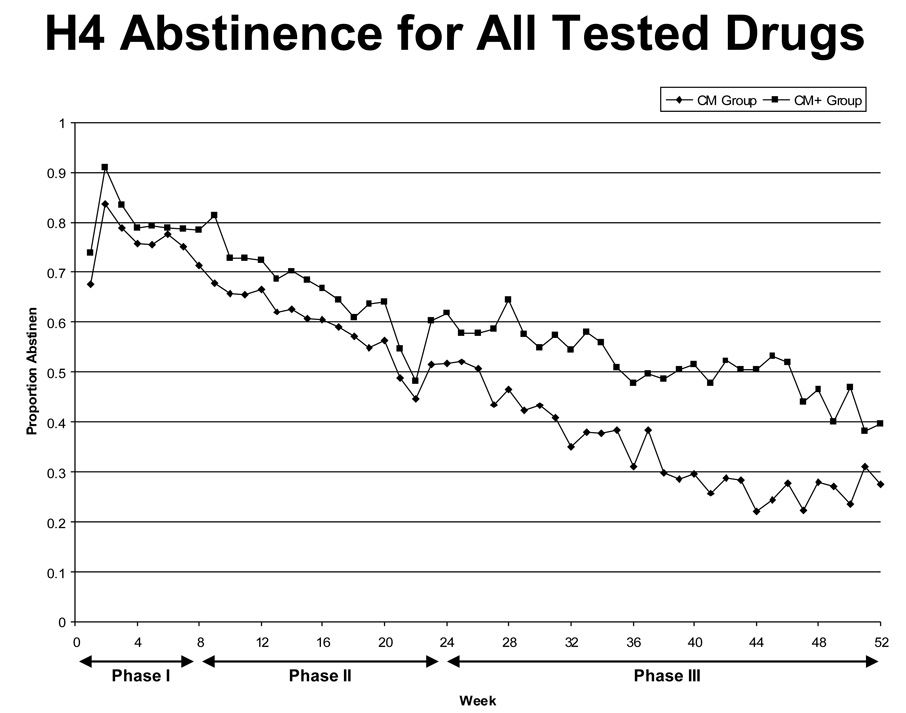
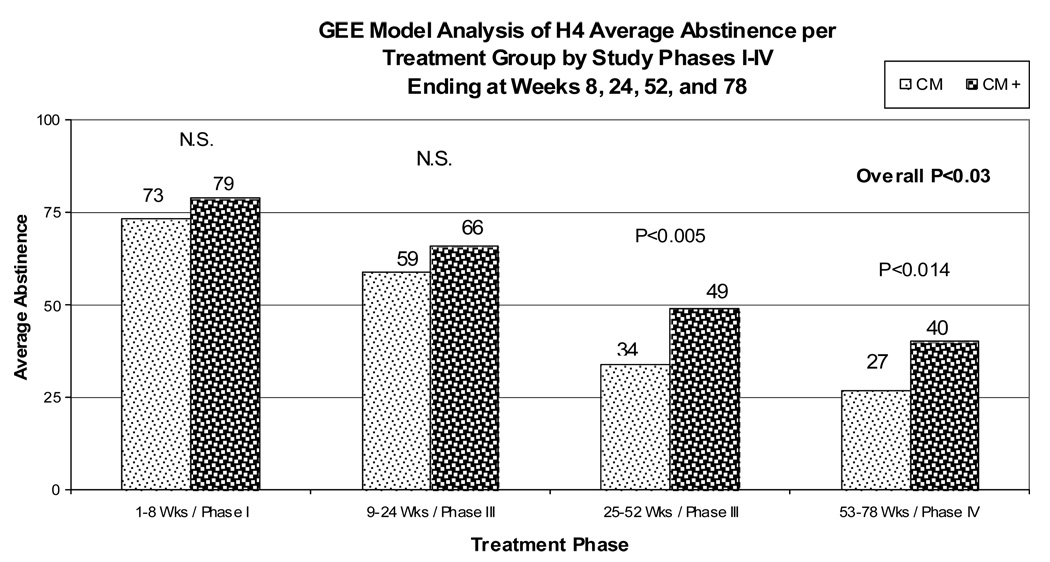
Figure 3 shows proportion group abstinence for weeks 1–52 based on individual urine-test data. Though there is a clear separation between CM+, which always has slightly higher abstinence than CM for each of the phases of active treatment (Phase I weeks 1–8, Phase II weeks 9–24), both groups show high abstinence, generally over 50% on a week-to-week basis during both phases, and mostly remaining in excess of 30–40% subsequently. Because we did not have weekly urinalysis results from Phase IV in weeks 53–78, but did have monthly tests, once per week, or random urine data for each month, we also partitioned all the urine data into four week month-equivalents, prepared a graph of results by month, and analyzed results by study phase. Comparison of monthly abstinence data across the four study Phases are shown in Figure 4. Abstinence comparisons show little difference by trial arm, until after six months (24 weeks) when formal treatment ended and contingencies ceased, at which time some trial arm differences emerged. Abstinence prevalence (average proportion of participants abstinent at a particular time point) were obtained for each study phase using the GEE model. These estimates confirm the graphical results. The comparisons across phases (proportion of group abstinent) for CM vs. CM+ were: .734 (SE=0.032) vs. .791(SE=0.031) for Phase I (p=0.21); .590 (SE=0.041) vs. .655 (SE=0.040) for Phase II (p=0.25); .341 (SE=0.034) vs. .486 (SE=0.0396), for Phase III (p=.0.006); and .266 (SE=0.038) vs. .398 (SE=0.038) for Phase IV (p=0.015). These GEE models were also used to test the non-inferiority of CM compared to CM+ by examining the one-sided Z-test for the difference between the CM abstinence prevalence and 75% of the CM+ abstinence prevalence, with a significant test that this difference is 0 or greater supporting the hypothesis. Based on tests using the model-based abstinence estimates shown above, results for Phases I and II support the non-inferiority hypothesis with an estimated difference for Phase 1 of 0.14 (z=3.56, p<0.001) and for Phase II of 0.099 (z=1.96, p=0.025) [where .14=.734 – .75 ×.791] and .099=.590 - .75 × .655]. However, the results for Phase III and Phase IV do not support that hypothesis with differences of −0.024 (z=-0.52 p=0.70) for Phase III and −0.032 (z=−0.66 p=0.75) for Phase IV, respectively.
Figure 3.
Weekly proportion abstinence across three study phases: 24 weeks of active treatment; 26 weeks of aftercare and follow-up in two groups, CM vs. CM+. Observed urine specimens were tested for cocaine, marijuana and alcohol, with other drug tests added where baseline urine tests indicated other drugs were being used.
Figure 4.
Average abstinence per group across four study phases of active treatment (Phases I – II) and aftercare and follow-up (Phases III – IV), as measured by observed urine collection and testing multiple times per week up to 24 weeks and randomly thereafter through week 78 (18 months follow-up).
3.3 Percentage Urine Tests Abstinent
Each participant’s percentage of urine tests abstinent is an outcome sensitive to harm reduction. ANOVA models were generated to compare the mean percentage urine tests negative between groups for Phases I, II, and III separately. The percentage was slightly greater for CM+ compared to CM during each phase of treatment, but non-significant for Phases I and II. During Phase III the percentage for CM was .335%, SD=.346, and for CM+ was .484%, SD=.402, with the difference between them significant (p=0.0052). There were an insufficient number of urine tests to test for differences in Phase IV. The ANOVA models used to test the non-inferiority of CM compared to CM+ results for Phases I and II support the non-inferiority hypothesis with a estimated difference for Phase 1 of 0.13 (t=3.42, df=204, p<0.001) and for Phase II of 0.093 (t=1.85, df=201, p=0.033). However, the results for Phase III do not support that hypothesis with a difference of −0.028 (t=−0.60, df=201, p=0.73). Thus, in Phase III CM was inferior to CM+ for this outcome.
3.4 Average Consecutive Weeks Abstinent
ANOVA models were also used to examine differences in consecutive weeks abstinent for all tested drugs, (counting the longest period for each participant) in Phases I and II combined. Means for consecutive weeks abstinent were CM= 11.07, SD=8.35, and CM+= 13.32, SD= 9.17 (P= 0.067). Consistent with earlier analyses, these results show CM+ having slightly greater sustained abstinence than CM, but the difference is not statistically significant. The ANOVA model was also used to evaluate the non-inferiority hypothesis described earlier. The difference between CM and 75% of CM+ of 1.08 (t=1.00, df=204, p=0.32) does not support the non-inferiority hypothesis. Though sustained abstinence for CM+ was not significantly higher than that for CM, the magnitude of the difference between groups was large enough that the non-inferiority of CM to CM+ could not be demonstrated.
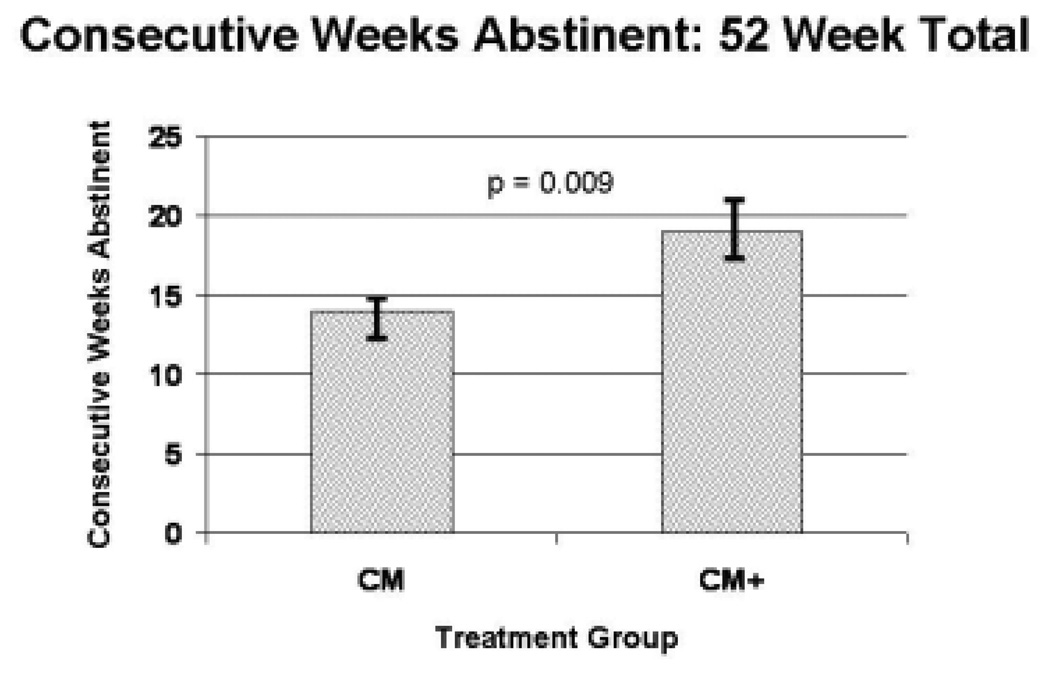
We examined consecutive weeks abstinent across Phases I-III from 0–52 weeks, where treatment ended at week 24. These results are displayed in Figure 5. Note that during weeks 25–52, instead of urine tests three times per week, urine was tested randomly once per week and may have allowed occasional undetected drug use. However, once weekly random testing seemed likely to detect regular or sustained occasional use and provided important data on sustained abstinence. For this longer period CM+ had significantly more consecutive weeks abstinent (19.18, SD=16.0) than did CM (13.89, SD=12.6), p=0.009. As noted in Table 1, years of education did differ significantly across the treatment arms. An added ANCOVA model controlling for age was fit to evaluate whether this difference might be confounding the treatment effect. The magnitude of the treatment effect was slightly smaller in the adjusted model (5.2 versus 5.3 weeks, p=0.013), but the difference was not clinically important. Consequently, education was ignored in the other analyses.
Figure 5.
Longest average consecutive weeks abstinent (sustained abstinence) in each of two treatment groups, CM vs. CM+, across 52 weeks, where formal treatment and all contingencies ceased at week 24. Bars indicate + or − 1 standard error.
3.5 The Role of Attendance in Abstinence Outcomes
Level of attendance was highly correlated with abstinence outcomes for both groups. When attendance was analyzed as a continuous cumulative variable, CM attendance was correlated r=.77 with consecutive weeks abstinent in Phase I, and r=.88 in Phase II. For CM, percentage weeks abstinent and attendance was correlated r=.54 in Phase I, and .74 in Phase II. Similarly, for CM+, consecutive weeks abstinent correlations with attendance were r=.76 and r=.88 for Phases I and II, and percentage weeks abstinent and attendance were correlated r=. 61 and r=.77 for Phase I and II. All these correlations were significant at p <.0001. Given that attendance was highly correlated with abstinence in both groups and that CM+ had somewhat greater attendance across treatment phases, it is not surprising that CM+ participants had more excused absences to attend important community recovery tasks. Also, we examined the abstinence rates between the two groups when the contribution of attendance to abstinence across study Phases I-II was controlled. It revealed estimated consecutive weeks abstinent for CM at 11.96, vs. CM+ at 12.43 with the difference not significant (p=0.41).
We also looked at a series of models that included treatment and days attendance during shared CM components in Phase I and II separately, as well as higher order interactions of treatment and the attendance variables. Because the model results showed no evidence of an interaction between attendance and treatment, results are presented for the model that included terms for treatment, days attendance during Phase I, and days attendance during Phase II. The estimates from the model indicate that every day of increased attendance in Phase I resulted in an estimated increase in mean consecutive weeks abstinent of 0.078 weeks [95% CI = (−0.035, 0.19) weeks] an effect that obviously was not significant (p=0.18). In contrast, every day of increased attendance in Phase II resulted in an estimated increase in mean consecutive weeks abstinent of 0.244 weeks [95% CI = (0.209, 0.279) weeks], a highly significant effect (p<0.000l). This model generated treatment-specific estimates of adjusted consecutive weeks abstinent (adjusted to the mean attendance level) for CM of 11.96, vs. CM+ of 12.43 with the difference not significant (p=0.41).
3.6 Possible Role of Missing Urines Assumed Drug Positive
Since we assumed missing data were drug-positive, it is possible that more missing data among CM participants could have contributed to their lower abstinence. To assess this possibility, we examined missing tests distributed among the two groups across all phases of treatment and confirmed more missing data in CM. A summary of percent missing urine data for each group across all four phases of treatment is found in Table 2. Obviously, the CM group had a somewhat greater level of missing urine tests at all phases than did the CM+ group, while the fraction of missing urine tests that were excused was somewhat higher in the CM+ group, suggesting that differences in missing data could have contributed to the observed differences in the two treatment arms.
Table 2.
Percent missing urine tests and excused urine tests (as a percentage of missing urine tests) during each of the four phases of treatment for CM vs. CM+.
| Phase I | Phase II | Phase III | Phase IV | |||||
|---|---|---|---|---|---|---|---|---|
| Miss. | Exc. | Miss. | Exc. | Miss. | Exc. | Miss. | Exc. | |
| CM | 18.13 | 6.89 | 38.35 | 4.51 | 56.06 | 3.75 | 48.53 | 1.66 |
| CM+ | 15.67 | 11.37 | 33.04 | 9.91 | 41.52 | 8.86 | 38.14 | 7.05 |
To assess whether using unexcused missing urine tests as indicating drug use may have yielded a result that would change derived conclusions regarding treatment effectiveness, we conducted a similar analyses but one which assumed missing urine tests were missing at random. Because all abstinence outcomes yielded the same general conclusions about the impact of treatment on abstinence, the sensitivity analyses were only conducted for the abstinence prevalence outcome measure. Results for the comparisons across phases for CM vs. CM+ were: .843 (SE=0.019) vs. .890 (SE=0.017) for Phase I (p=0.072); .850 (SE=0.020) vs. .889 (SE=0.017) for Phase II (p=0.19); .708 (SE=0.034) vs. .767 (SE=0.030), for Phase III (p=0.16); and .514 (SE=0.053) vs. .623 (SE=0.045) for Phase IV (p=0.11). Note that CM+ consistently has slightly greater abstinence than CM across all phases but that the differences are no longer statistically significant. Also, as expected the estimates of abstinence, which are likely biased high as a consequence of treating all missing data as randomly missing, are substantially greater than those shown in the primary analyses.
4. Discussion
The purpose of this study was to compare the effectiveness of an established but complex and expensive behavioral day treatment intervention with only its abstinence contingency managed components, the latter of which could possibly serve as a first step care for homeless persons with cocaine and other drug dependence. Three important results were obtained. First, high retention and abstinence levels were achieved by participants in both the abbreviated (CM) and full (CM+) interventions. Abstinence levels were higher than those of our three previous studies with this population (Milby et al., 2000; 2005b). Second, as hypothesized, the CM group achieved high and sustained abstinence throughout active treatment, which was not significantly different from, nor inferior to that of the more intense and expensive CM+ treatment. Third, distal outcomes of greater sustained abstinence, 6 and 12 months after treatment, emerged in the CM+ group. Similar delayed effects of substance abuse treatments have occasionally been reported by others. For example, a delayed effect was observed for relapse preventionbased behavioral psychotherapy in cocaine dependent patients treated with pharmacotherapy (Carroll et al., 1994). Also, Rawson and colleagues (2002) found delayed effects of cognitive behavioral therapy for cocaine dependent patients treated for opioid dependence with methadone maintenance.
These results may have policy implications for the utilization of the CM components as the first step in a stepped care model for homeless substance abusers, in which only those who fail to respond to initial stepped care would be referred for the intensive and more costly behavioral day treatment utilized in CM+. However, further study is needed before we could know if the response to CM+, given its sequential exposure to CM, is the same as response to CM+ only. The relative success of the CM intervention suggests that further reductions in its complexity as an initial step of care should be studied. For example, abstinent contingent housing alone may be a sufficient intervention for homeless substance abusers to initiate and sustain abstinence without further substance abuse treatment, especially for those with non-complicating mental disorders.
In our earlier clinical trials (Milby et al., 2000; 2005b), enhanced behavioral interventions maintained their significant effects on abstinence after statistically controlling for attendance. In the present study, controlling for attendance neutralized the effect of treatment. This suggests that CM+ gained its treatment superiority by retaining participants. By extension, we infer that if CM were to be modified to be more attractive and retain more participants, it could be more effective and potentially more cost effective, depending on the cost of such enhancements. Clearly, more research is needed here to determine whether these important implications can be verified in future research. The complete results suggest an ironic demurrer with an opposite policy implication. It may be that the long term outcomes achieved here may not be possible if we continue to insist that treatment be less expensive and less complicated.
The small advantage of behavioral day treatment over the contingency managed housing and work during active treatment, may indicate that CM outcomes approach a ceiling of reasonably expected levels of abstinence for this population beyond which it is difficult to yield further gains. Thus, CM alone may be a relatively inexpensive but nevertheless viable intervention, perhaps capable of helping a substantial proportion of homeless substance abusers initiate and sustain abstinence while concentrating on improving their housing and employment conditions. That abstinence for CM+ was significantly higher than CM during the post-treatment period (months 7–18), may indicate that gains in recovery resulting from behavioral day treatment are best reflected in long term reduced drug use and perhaps better life functioning, like long term housing stability, employment, psychiatric status improvement, and health care service utilization. Thus, CM+ may be a more viable alternative for a homeless cohort with more psychological problems in addition to chronic addiction. This possibility is suggested by other studies with this population.
Lester et al. (2006) studied PTSD symptoms in a subset of the present sample, and found more improvement in these symptoms among participants in the CM+ condition. Also, our research group (2001) examined the relative treatment response of participants with substance use disorders only compared to those with one or more additional DSM III-R Axis I disorders. All received behavioral day treatment like the current CM+ condition. Those with dual diagnoses showed greater positive changes than the substance use only group from baseline to six months, in alcohol, drug, employment/support, and psychiatric status areas. Although this pattern may reflect a regression to the mean, those results also are consistent with the notion that behavioral day treatment has important impacts on life functioning in addition to abstinence effects. Another example of more persistent treatment effects other than improved abstinence, was found by Higgins et al. (2003) . They studied the effect of contingency management alone compared to CM plus an intensive behavioral community reinforcement approach, similar to CM+ in the current study. Two years after treatment entry only the added behavioral intervention showed improvement in drinking to intoxication, more days of paid employment, fewer hospitalizations and legal problems.
Results from the current study, together with the PTSD subpopulation, and the earlier study from a similar cohort treated with the behavioral day treatment, suggest some functioning domains where behavioral day treatment may exert delayed treatment effects. Future research needs to replicate those effects to identify what additional participant characteristics change, other than improved long term abstinence. Research identifying such associated changed characteristics in the delayed treatment effect would seem to have implications for matching patients to either of these interventions in the most cost effective manner.
In addition to the question of what patient characteristics or behaviors change most during and after treatment, there also is the possibility of identifiable pre-treatment characteristics that predict favorable outcomes for the CM and CM+ conditions. Future analyses of these data and from other long term outcome studies may provide such predictors. Perhaps a more useful predictor of treatment outcome may be early treatment response. We and others have found that those participants who initiate and sustain abstinence early in treatment, to a great extent irrespective of the treatment to which they are assigned, show more sustained abstinence at distal follow-up after formal treatment has ended (Carroll et al., 1994; Higgins, Badger, & Budney, 2000; Kosten et al., 1992; Milby et al., 2004).
The current study results and our previous work using abstinent contingent housing, (Milby et al., 2000; 2005b) may appear to have very different implications than current and highly-publicized initiatives in what is termed a Housing First approach (Editorial, 2002, 2003; Ekholm, 2006; HUD, 2002; Tsemberis, Gulcur, & Nakae, 2004), where housing is offered directly to homeless persons, without preconditions other than provision of payment and/or agreement for a case manager to visit. Patients in the Tsemberis et al. continuum of care control group received access to housing based on substance abuse and psychiatric treatment participation and established abstinence. However, their abstinence outcomes, that were not different from the housing first group, may be a function of the different populations served. A harm reduction, housing first intervention may be more appropriate for homeless persons with severe mental illness studied by Tsemberis, and colleagues. For populations with non-psychotic mental illness and cocaine dependence, behavioral intervention, which offers housing for treatment participation in the first week, then imposes an abstinence contingency for continued housing, may be the most viable approach. These important treatment access and policy concerns should be addressed in future research designed to compare these options.
These results seem consistent with the Rawson, Huber, McCann, et al. (2002) results comparing Cognitive Behavioral Therapy (CBT) with Contingency Management (CM) alone, and both of these treatments alone with combined CM+CBT. At six and 12 month follow-ups, the superiority of CM over CBT observed during treatment disappeared, while performance of the CBT group appeared to improve over time. The Higgins group (2003) also found benefits two years after treatment entry from their behavioral intervention added to contingency management. These gains were observed 1.5 years after contingencies ended. Thus, findings are accumulating to suggest that intensive contingency management approaches when combined with cognitive behavioral therapy may be able to sustain treatment gains long after contingencies are discontinued.
Though cost and complexity are obvious barriers to implementation of this effective intervention, there are others that are less apparent. Thus, this study is only an initial step toward determining how this intervention can be disseminated. Effective implementation of CM is more complicated and requires more skill than people generally believe. It probably requires faithful adherence to manualized procedures and progressive steps of measured training like that utilized by Milby and colleagues in the Houston, Texas replication study (Milby et al., 2007). It may be that the most important barrier to acceptance and dissemination of CM (and CM+ for that matter) may be its conceptual acceptability to treatment providers and other stake holders.
Some limitations of the study should inform the interpretation of findings. Though missing data was reduced to lower levels than ever obtained by our research group studying this difficult population, it still requires interpretation, particularly when urine tests were more frequently missing for CM than for CM+. It could be that missing data contributed to differences in observed abstinence, because missing data points were coded drug-positive. First it should be noted that a finding of greater long-term abstinence in the trial arm with the least missing data (or conversely, the strictest scrutiny, as was the case for CM+ here) is generally likely to be a valid one. Second, since both groups had the same housing and work training incentives to lose from missing a urine test, and the same benefits from giving urine specimens testing free of abused drugs, it is likely a valid assumption that missing a urine test unexcused indicates drug use. If participants in either group were clean and missed a drug test they would lose these incentives in spite of being abstinent. The disparity in excused missing urine tests where CM+ had more excused missing tests may have contributed to abstinence outcomes. We attribute this finding to the fact that the CM+ group spent twice as much time in Phase I treatment, from 7:30 to 4 pm, and needed more excused absences to complete important community recovery tasks. Lastly, it is important to note that our participants were all treatment seekers and thus generalization to a population of homeless substance abusers, many of whom do not seek treatment, may be limited.
Acknowledgments
This research was supported by NIDA grant 3R01 DAD 11788-0451. Authors acknowledge the contributions of Sharon Waltz, PsyD, Marilyn Furman, PsyD, and Dan Lowery Ph.D., post-doctoral fellows who helped with screening, assessment, and intervention, and to Michelle Gould, M.A., Project Director, who coordinated clinical and scientific activities at project termination.
The CM and CM+ manuals and brief consultation on stepped training are available from the first author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jesse B. Milby, University of Alabama at Birmingham.
Joseph E. Schumacher, University of Alabama at Birmingham.
Rudy E. Vuchinich, University of Alabama at Birmingham.
Michelle J. Freedman, University of Alabama at Birmingham.
Stefan Kertesz, University of Alabama at Birmingham.
Dennis Wallace, Rho Inc. Federal Systems Division, Chapel Hill, North Carolina.
References
- Azrin NH, Besalel VA. Job Club Counselors Manual. Baltimore, MD: University Park Press; 1983. [Google Scholar]
- Azrin NH, Flores T, Kaplan SJ. Job-finding Club: A group assisted program for obtaining employment. Behavioral Research Therapy. 1975;13:17–27. [Google Scholar]
- Burt MR, Aron LY. Urban. 2000 from http://www.urban.org.luf.cfm?ID=90034.
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Corrigan EM, Anderson SC. Homeless alcoholic women on skid row. American Journal of Drug and Alcohol Abuse. 1984;10:535–549. doi: 10.3109/00952998409001491. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The SC-R-90 Manual I: Scoring, Administration and Procedures for the SCL-90. Baltimore, MD: Clinical Psychometric Research; 1977. [Google Scholar]
- Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90-R: A study in construct validation. J Clin Psychol. 1977;33:981–989. [Google Scholar]
- Editorial. Ending Chronic Homeless. New York Times. 2002:A-24. [Google Scholar]
- Editorial. Up and Off the Streets. New York Times. 2003:A-30. [Google Scholar]
- Ekholm E. New campaign shows progress for homeless. New York Times. 2006:18. [Google Scholar]
- Folsom DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. American Journal of Psychiatry. 2005;162(2):370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- Haddad MB, Wilson TW, Ijaz K, Marks SM, Moore M. Tuberculosis and homelessness in the United States, 1994–2003. Journal of the American MedicalAssociation. 2005;293(22):2762–2766. doi: 10.1001/jama.293.22.2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Experimental and Clinical Psychopharmacology. 2000;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, Heil SH, GJ B, Donham R, et al. Community reinforcement therapy for cocaine-dependent outpatients. Arch Gen Psychiatry. 2003;60:1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RT. Contingent reinforcement increase cocaine abstinence during outpatient treatment and 1 year of follow-up. Journal of Clinical and Consulting Psychology. 2000;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- HUD. U. S. Office of Housing and Urban Development Notice of Funding Availability (NOFA) for the Collaborative Initiative to Help End Chronic Homelessness. 2002 from http://www.hud.gov/offices/cpdhomeless/apply/2002nofa/index.cfm.
- Kertesz SG, Mullins AN, Schumacher JE, Wallace D, Kirk K, Milby JB. Long-term Housing and Work Outcomes Among Trated Cocaine-Using Homeless Persons. 2006 (under submission). [Google Scholar]
- Koegel P, Burnam MA, Farr RK. Alcoholism among homeless adults in the inner city of Los Angeles. Archives of General Psychiatry. 1988;51:1011–1018. doi: 10.1001/archpsyc.1988.01800350045007. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Gawin FH, Kosten TA, Morgan C, Rounsaville BJ, Shottenfeld R, et al. Six month follow-up of short-term pharmacotherapy for cocaine dependence. American Journal of the Addictions. 1992;1:40–49. [Google Scholar]
- Lester KM, Milby J, Schumacher J, Vuchinich R, Persons S, Clay OJ. Impact of behavioral contingency management intervention on coping behaviors and PTSD symptom reduction in cocaine addicted homeless. Birmingham: 2006. Unpublished manuscript. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Martens W. A review of physical and mental health in homeless persons. Public Health Review. 2001;29(1):13–33. [PubMed] [Google Scholar]
- McKinney SB. McKinney Homelessness Assistance Act. Public Law. 1987:100–177. [Google Scholar]
- McNamara C, Schumacher JE, Milby JB, Wallace D, Usdan S. Prevalence of nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent sample. American Journal of Drug and Alcohol Abuse. 2001;27(1):91–106. doi: 10.1081/ada-100103120. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Freedman M, Lester K, Netson KL, Norwood W, et al. A Progressive Process for Technology Transfer of a Complex, Effective Psychosocial Intervention: Methods and Preliminary Results. Addictive Disorders and Their Treatment. 2007 In Press. [Google Scholar]
- Milby JB, Schumacher JE, McNamara C, Wallace D, Usdan S, McGill T, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug and Alcohol Dependence. 2000;60(1):55–67. doi: 10.1016/s0376-8716(99)00139-8. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug and Alcohol Dependence. 1996;43(1–2):39–47. doi: 10.1016/s0376-8716(96)01286-0. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Vuchinich RE, Wallace D, Plant MA, Freedman MJ, et al. Transitions during effective treatment for cocaine-abusing homeless persons: establishing abstinence, lapse, and relapse, and reestablishing abstinence. Psychology of Addictive Behavior. 2004;18(3):250–256. doi: 10.1037/0893-164X.18.3.250. [DOI] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Wallace D, Freedman MJ, Vuchinich RE. To house or not to house: The effects of providing housing to homeless substance abusers in treatment. American Journal of Public Health. 2005b;95(7):1259–1265. doi: 10.2105/AJPH.2004.039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milby JB, Schumacher JE, Wallace D, Frison S, McNamara C, Usdan S, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. Journal of Consulting and Clinical Psychology. 2003;71(3):619–621. doi: 10.1037/0022-006x.71.3.619. [DOI] [PubMed] [Google Scholar]
- Plumb JD. Homelessness: care, prevention and public policy. Annual International Medicine. 1997;126(12):973–975. doi: 10.7326/0003-4819-126-12-199706150-00007. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Ling W. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Archives of General Psychiatry. 2002;59:593–600. doi: 10.1001/archpsyc.59.9.817. [DOI] [PubMed] [Google Scholar]
- Research Reports on Homelessness: Homelessness Counts. National Alliance to End Homelessness; 2007. pp. 1–41. [Google Scholar]
- Rosenheck R, Leda C, Astrachan B, Milstein R, Leaf Pl, Thompson D, et al. Initial assessment data from a 43-site program for homeless chronic mentally ill veterans. Hospital and Community Psychiatry. 1989;40:937–942. doi: 10.1176/ps.40.9.937. [DOI] [PubMed] [Google Scholar]
- SAMHSA. National Household Survey on Drug Abuse: Main Findings. National Clearinghouse for Alcohol and Drug Information; 2000. [Google Scholar]
- SAMSHA. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; The DASIS report: Characteristics of homeless admissions to substance abuse treatment. 2006
- Schumacher JE, Milby JB, Wallace D, Simpson C, Frison S, McNamara S, Usdan S. Diagnostic compared with abstinence outcomes of day treatment and contingency management among cocaine-dependent homeless persons. Experimental and Clinical Psychopharmacology. 2003;11(2):146–157. doi: 10.1037/1064-1297.11.2.146. [DOI] [PubMed] [Google Scholar]
- Smereck GA, Hockman EM. Prevalence of HIV infection and HIV risk behaviors associated with living place: on-the-street homeless drug users as a special target population for public health intervention. American Journal of Drug and Alcohol Abuse. 1998;24(2):299–319. doi: 10.3109/00952999809001714. [DOI] [PubMed] [Google Scholar]
- Toro PA, Bellavia CW, Daeschler CV, Ownes BJ, Wall DD, Passero JM, et al. Distinguishing homelessness from poverty: A comparative study. Journal of Consulting and Clinical Psychology. 1995;63:280–289. doi: 10.1037//0022-006x.63.2.280. [DOI] [PubMed] [Google Scholar]
- Tsemberis S, Gulcur L, Nakae M. Housing First, Consumer Choice, and Harm Reduction for Homeless Individuals With a Dual Diagnosis. American Journal of Public Health. 2004;94(4):651–656. doi: 10.2105/ajph.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]