Abstract
Although lateral retinacular releases are not uncommon, there is very little scientific knowledge about the properties of these tissues, on which to base a rationale for the surgery. We hypothesised that we could identify specific tissue bands and measure their structural properties. Eight fresh-frozen knees were dissected, and the lateral soft tissues prepared into three distinct structures: a broad tissue band linking the iliotibial band (ITB) to the patella, and two capsular ligaments: patellofemoral and patellomeniscal. These were individually tensile tested to failure by gripping the patella in a vice jaw and the soft tissues in a freezing clamp. Results: the ITB–patellar band was strongest, at a mean of 582 N, and stiffest, at 97 N/mm. The patellofemoral ligament failed at 172 N with 16 N/mm stiffness; the patellomeniscal ligament failed at 85 N, with 13 N/mm stiffness. These structural properties suggest that most of the load in-vivo is transmitted to the patella by the transverse fibres that originate from the ITB.
Keywords: Patella, Patellofemoral joint, Strength, Structural properties, Lateral retinaculum, Iliotibial band
1. Introduction
The lateral retinaculum remains incompletely understood and studies of its biomechanical properties are lacking. This contrasts with its medial counterpart, the medial patellofemoral ligament. The anatomy and biomechanics of the medial patellofemoral ligament have been described in the literature (Amis et al., 2003; Arendt et al., 2002; Nomura et al., 2005; Ostermeier et al., 2007a; Panagiotopoulos et al., 2006) and its structural properties have been reported (Mountney et al., 2005). The structural properties of the lateral retinaculum are unknown. There have been studies which characterise its tensile stress with knee flexion (Luo et al., 1997), the change in its tension during surgery (Ishibashi et al., 2002), its contribution to patellofemoral stability (Christoforakis et al., 2006; Marumoto et al., 1995) and the effects of its release in the prosthetic knee (Hsu et al., 1997; Wackerhagen et al., 1992); a knowledge of the structural properties of the retinacular tissues would aid the interpretation of these studies, for example showing whether tensile loads approach structural failure. Lateral retinacular release has been favoured over other procedures as it is a relatively simple procedure. However, an inappropriate lateral release can cause medial subluxation of the patella; this is a recognised complication that may be treated by reconstruction (Brinker et al., 2001; Hughston and Deese, 1988; Hughston et al., 1996; Nonweiler and Delee, 1994). Limiting the lateral release has been suggested to avoid this complication (Lattermann et al., 2007).
This study aimed to measure the stiffness and strength of the tissues that provide lateral restraint to the patella. This basic knowledge on the structural properties of a tissue that has often been released will provide information needed for rationalising repairs or reconstructions. In particular, it was hypothesised that discovery of the structural properties of specific bands of soft tissues lateral to the patella would provide a rationale for partial, or staged, lateral release procedures.
2. Materials and methods
Eight fresh-frozen cadaveric knees with no prior history of knee surgery or disease were used in this study (mean age 72 (S.D.8) years; range 54–79). These were obtained from the International Institute for the Advancement of Medicine (Jessup, PA, USA). The institute undertook screening and consent for the use of the knees for research. Ethical permission for the study was obtained from the Riverside Research Ethics Committee. The knees were stored at −20 °C and thawed a day prior to experimentation.
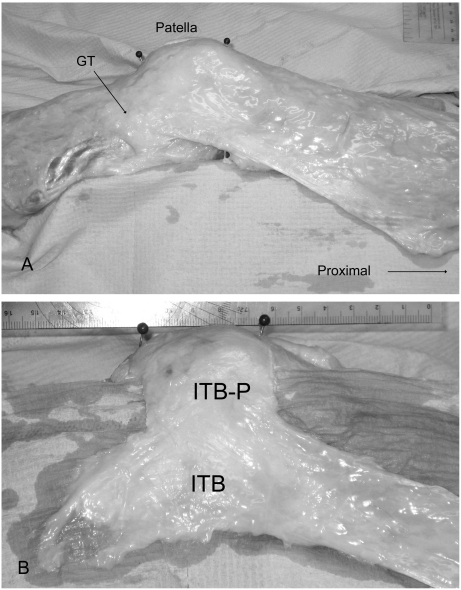
The skin and subcutaneous tissue were removed, revealing the deep fascial layer. It was adherent to the iliotibial band (ITB) posteriorly, but passed over the patella anteriorly (superficial) without attaching to it. This was removed, beginning anteriorly where it was most easily defined. The next layer was the lateral retinaculum, with extracapsular tissue interconnections that passed from the ITB to the patella. Depending on the depth, the predominant orientation of the tissue fibres differed and this detailed anatomy has been described (Merican and Amis, 2008). Anatomically, the most substantial part was the deepest part of this layer. Here the fibres criss-crossed in a predominantly transverse orientation and these have been termed the iliotibial band–patella (ITB-P) fibres (Merican and Amis, 2008). It was not distinctly separate superficially, but easily separated from the underlying joint capsule. Because of the interconnections with other structures and also the fact that it consisted of criss-crossing fibres, it was not possible to dissect this part of the lateral retinaculum into a series of distinct proximal, middle or distal tissue bands for separate tensile testing without damaging its integrity. Therefore, the lateral retinaculum was cut transversely at the levels of the proximal and distal limits of the patella, avoiding the criss-crossing fibre areas and including the entire width of the transverse iliotibial band–patellar fibres. This resulted in a band of tissue that connected the patella and the ITB, with width equal to the proximal–distal length of the patella, and without cutting the criss-crossing fibres (Fig. 1). The ITB was then cut from its tibial and femoral attachments and, beginning posteriorly, it was lifted off anteriorly, separating it from the underlying joint capsule.
Fig. 1.
The lateral retinaculum. Lateral aspect of a left knee. There are pins placed on the proximal and distal limits of the patella from anteriorly. The iliotibial band (ITB) is dissected and it is seen here attached to Gerdy's tubercle (GT). The lateral retinaculum and ITB are dissected as described in the text and this results in a band of tissue that connects ITB to patella (ITB–P) for material testing.
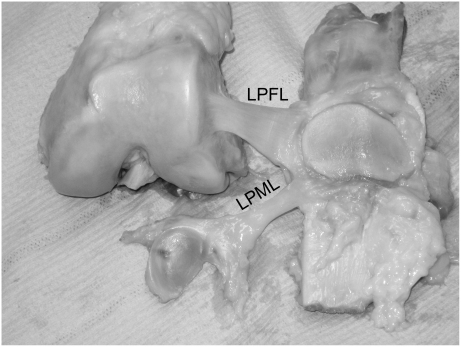
The joint was opened medially and the patellar and quadriceps tendons and both cruciate ligaments were transected. The tibia was separated from the femur and the lateral meniscus. The lateral patellofemoral ligament (LPFL) and the lateral patellomeniscal ligament (LPML) were thickened bands of the lateral joint capsule that connected the lateral border of the patella to the femur and to the anterior aspect of the lateral meniscus, respectively. They were identified by a combination of transillumination and palpation (Fig. 2). In its superficial aspect the LPFL passed over the lateral femoral epicondyle and was anchored in that proximity. However, because both the LPFL and the LPML were not always present as distinct fibre bands, it was decided not to try to isolate them from the rest of the capsule but to test the relevant part of the lateral capsule that connected the patella to the femur or to the anterior horn of the lateral meniscus. These capsulo-ligamentous bands included the LPFL and LPML, and will be referred-to as such in this paper.
Fig. 2.
Lateral capsular restraints. The lateral patellofemoral ligament (LPFL) and lateral patellomeniscal ligament (LPML) are isolated for structural testing.
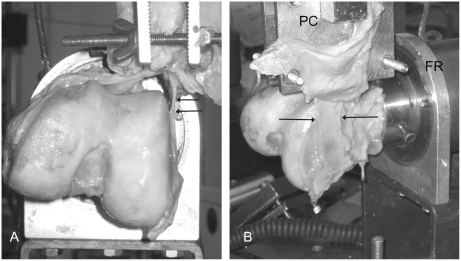
In this manner, the knee was prepared with three components of the lateral restraint of the patella available for sequential tensile testing; the lateral retinaculum, the lateral patellofemoral ligament and the lateral patellomeniscal ligament (Figs. 1 and 2). The lateral patellofemoral ligament was tested first (Fig. 3). The femur was secured in a steel pot using centralising grub screws and polymethylmethacrylate with its anatomical axis in line with the axis of the pot. This pot was placed in a rig that allowed for the femur to be rotated around its anatomical axis. The rig was placed on the base plate of an Instron 5565 materials testing machine (Instron Co., High Wycombe, Bucks, UK) such that the lateral femoral condyle was centred directly under the load cell with the femur horizontal. A drill bit was drilled through the anterior surface of the patella perpendicular to it and exited its articular surface in the proximal–distal centre of the median ridge. The patella was placed in a clamp attached to the load cell on the moving crosshead of the Instron. The drill bit was relocated into the patella through the jaws of the clamp. The lateral patellofemoral ligament was tensed by pulling it downwards and the patella was allowed to rotate to align itself to the load by virtue of the drill bit and then the clamp was tightened. The femur was rotated externally until the lateral capsule was tangential with the lateral surface of the lateral femoral condyle and then it was locked into that position (Fig. 3). The crosshead was moved down until the tissue was slack and the load measured by the cell was zeroed. The tissue was preconditioned with a series of ten cycles from 0 to 10 N and then extended to failure at a rate of 1000 mm/min, which was the maximum possible with this machine.
Fig. 3.
Testing of the lateral patellofemoral ligament. (A) Distal–proximal view of a left femur and (B) a side view. The femoral rig (FR) accepts the steel pot in which the femur is secured and allows for rotation of the femur so that the ligament (arrowed) is parallel to the surface of the lateral condyle. The patellar clamp (PC) holds the patella. The lateral retinaculum is reflected upwards and slung on the outer aspect of the clamp so it is out of the way and not damaged for later testing (B).
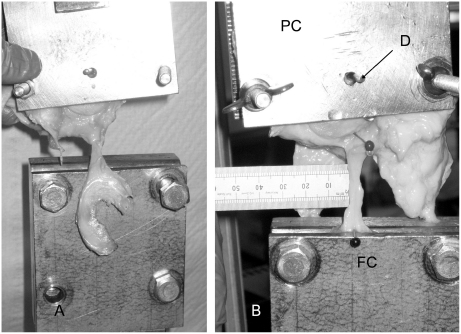
The patellomeniscal ligament was tested next (Fig. 4). The femur was removed from the base plate. The patella remained attached to the load cell. A soft tissue freeze clamp (Pring et al., 1985) was secured to the base plate centred directly under the patella. One of the jaws of the clamp was removed and the load cell with the patella lowered towards the clamp until the meniscus was resting on the inner side of the freeze clamp that remained. The patellar clamp was loosened and the patella was allowed to rotate around the drill and the meniscus was aligned so that the patellomeniscal ligament was on the loading axis. The patellar clamp was tightened and the meniscal clamp assembled. The meniscus was hardened by freezing with liquid carbon dioxide to prevent slippage, then the ligament was tensile tested as per the lateral capsule. Lastly, the ITB–patellar fibres of the lateral retinaculum was tested. The ITB was secured in the freeze clamp and the patella was realigned in its clamp so that the pull of the crosshead tensioned all the fibres of the tested tissue together (Fig. 5).
Fig. 4.
Testing of the lateral patellomeniscal ligament. The load cell and patellar clamp (PC) is lowered towards the freeze clamp (FC). The freeze clamp is disassembled and the meniscus placed inside the clamp (B). A drill bit has been replaced through both sides of the clamp and the centre of the median ridge of the patella. The patellar clamp is loosened and the patella rotated around the drill bit (D) to align the ligament.
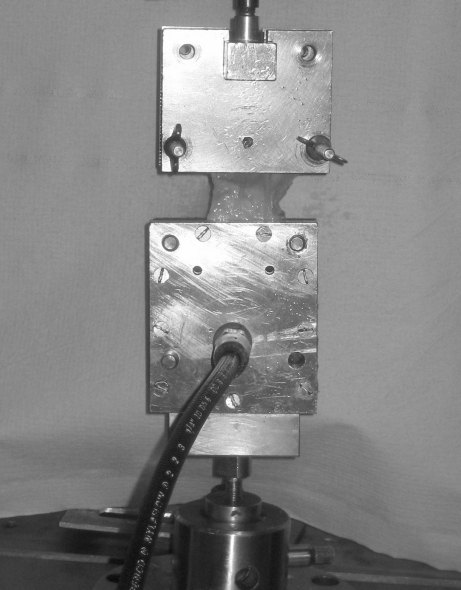
Fig. 5.
Testing of the lateral retinaculum. The iliotibial band is placed in the freeze clamp below and the patella is rotated in its clamp in order to apply an equal pull across all the fibres of the lateral retinaculum.
Data was collected with the manufacturer's software (Instron Bluehill materials testing software) and the raw data was imported into Microsoft Excel 2002 (Microsoft Corp, Seattle, WA, USA) for analysis. Load versus extension graphs were plotted for each tissue. The tensile strength was defined as the maximum load at failure and stiffness was measured by determining the slope of the linear portion of the graph. The high stiffness of the tensile test apparatus in comparison to the soft tissue specimens allowed the assumption that crosshead motion was the same as specimen elongation. In addition to calculating the descriptive statistics, data from the tests of the three structures were compared using repeated-measures one-way analyses of variance with Newman–Keuls multiple comparison post-hoc tests to examine the significance of individual differences; p<0.05 was taken to be significant.
3. Results
There was a significant difference (p<0.0001 by ANOVA) between the maximum loads of the three structures (Table 1), and the post-hoc tests showed that the ITB–P band was significantly stronger than both the LPFL and LPML (p<0.001 for each by post-testing). A significant difference was not demonstrated between the maximum strengths of the LPFL and LPML (p>0.05). In 6 out of the 8 specimens, the ITB–P band failed by an avulsion of bone from the lateral border of the patella (Table 1) and there were no specimens in the whole study where the soft tissue either slipped out of, or failed at, the freezing grip.
Table 1.
Site of failure and maximum load at failure for individual specimens.
| Knee | Age | Lateral retinaculum |
Lateral patellofemoral ligament |
Lateral patellomeniscal ligament |
|||
|---|---|---|---|---|---|---|---|
| Site of failure | Maximum load (N) | Site of failure | Maximum load (N) | Site of failure | Maximum load (N) | ||
| 1 | 74 | Patellar attachment | 550 | Mid-substance | 249 | Mid-substance | 137 |
| 2 | 76 | Patellar attachment | 412 | Femoral attachment | 137 | Mid-substance | 43 |
| 3 | 76 | Patellar attachment | 449 | Mid-substance | 242 | Patellar attachment | 62 |
| 4 | 75 | Patellar attachment | 865 | Patellar attachment | 210 | Mid-substance | 150 |
| 5 | 54 | Mid-substance | 761 | Femoral attachment | 153 | Mid-substance | 148 |
| 6 | 72 | Patellar attachment | 336 | Femoral attachment | 121 | Mid-substance | 75 |
| 7 | 70 | Mid-substance | 771 | Mid-substance | 104 | Mid-substance | 39 |
| 8 | 79 | Patellar attachment | 512 | Femoral attachment | 161 | Mid-substance | 25 |
The ITB–P band was significantly stiffer (p<0.001), as well as stronger, than the other two structures tested (LPFL and LPML). A significant difference of stiffness was not found (p>0.05) between the LPFL and the LPML (Fig. 6). The failure to demonstrate significant differences (p>0.05) between the strength, stiffness and extension to failure of the LPFL and LPML reflect the wide spread of results for the structural properties of the three structures tested (Table 2). In particular some specimens had a very weak capsular thickening to act as the LPML.
Fig. 6.
Mean load versus extension curves for 8 specimens. Error bars are standard deviations about mean point of maximum load.
Table 2.
Structural properties of the different tissues which provide for lateral restraint of the patella.
| Tissue tested | Strength (N) | Stiffness (N/mm) | Extension at failure (mm) |
|---|---|---|---|
| Lateral retinaculum | 582±193 (336–865) | 97±35 (54–156) | 11±4 (6–18) |
| Lateral patellofemoral ligament | 172±55 (104–249) | 16±7 (8–32) | 23±6 (15–32) |
| Lateral patellomeniscal ligament | 85±52 (25–150) | 13±8 (6–25) | 14±4 (9–21) |
Average values for 8 specimens are shown±standard deviation (min–max).
4. Discussion
This is the first study to report on the structural properties of the lateral retinacular and capsular tissues that attach to the patella. It shows that the ITB–patellar fibres of the lateral retinaculum were by far the strongest and stiffest structure, followed by the lateral patellofemoral and patellomeniscal ligaments. The mean strength of the ITB–patellar fibres was approximately three times that of the LPFL and six times as strong as the LPML. This is not unexpected since by gross inspection, the tissue between the ITB and the extensor mechanism is thickened at the level of the patella and reinforced on its deeper aspect by the criss-crossing iliotibial band–patella (ITB–P) fibres. These fibres, being more transverse in orientation and denser compared to the more superficial fibres, are well-suited to resist pulling the patella away from the ITB. Due to the criss-crossing nature of the ITB–P fibres, it was not possible to test the proximal part versus the distal part, for example, because cutting transversely across it at the mid patellar level would weaken its structural integrity. The lateral patellofemoral ligament (LPFL) and the lateral patellomeniscal ligament (LPML) were not always present as distinct fibre bands, and some authors (Blauth and Tillmann, 1983; Reider et al., 1981) have not found them in all knees, so it was difficult to separate them from the lateral capsule, as noted by Merican and Amis (2008). Because of this, the LPFL and LPML were tested integrally with a strip of the local capsule.
The structural properties of the ITB–P fibres of the lateral retinaculum are comparable in magnitude to the superficial medial collateral ligament (MCL). In this study the strength, stiffness and extension at failure were 582 N (S.D.193), 97 N/mm (S.D.35) and 11 mm (S.D.4), respectively. The values for the superficial MCL have been reported to be 534 N (S.D.84), 80 N/mm (S.D.8) and 10.2 mm (S.D1.1), respectively (Robinson et al., 2005). These properties and the transverse orientation of the tissue fibres imply that the lateral retinaculum resists large medial displacement forces acting on the patella. The medial patellofemoral ligament (MPFL), on the other hand, is anatomically much less substantial and may be vanishingly thin in some cases (Amis et al., 2003), yet it still has a tensile strength of 208 N (S.D.90) and an extension at failure of 26 mm (S.D. 7) (Mountney et al., 2005). In this respect, it is similar to the properties of the capsular lateral patellofemoral ligament reported in this study; their attachments close to the respective epicondyles are also similar.
In knee extension the patella is less constrained with respect to the femur due to the lack of engagement with the trochlea, and because the quadriceps muscle is not effectively pulling the patella against the femur, so the medial and lateral retinacula are expected to be important for patellar medial–lateral stability. In extension, the lateral trochlea is more prominent than the medial side and external rotation of the tibia in ‘screw-home’ (Ishii et al., 1997) increases the lateral force vector acting on the patella. One might, therefore, expect a stronger medial compared to a lateral soft tissue checkrein. Indeed, lateral patellar dislocation is not an uncommon clinical problem (Atkin et al., 2000) whereas medial patellar dislocation as a result of an injury has not been reported. Iatrogenic medial patellar instability is recognised after release of the lateral retinaculum (Hughston and Deese, 1988; Hughston et al., 1996; Miller et al., 1991; Nonweiler and Delee, 1994) and quite possibly due to differing interpretations of terminology, this may also include releasing the lateral capsule and its thickenings, the lateral patellofemoral and patellomeniscal ligaments. In the only published work documenting cases of frank medial dislocation demonstrated radiologically, all had lateral retinacular release (Miller et al., 1991). This is consistent with the finding in this study that the retinaculum is a strong and stiff structure, oriented to resist patellar medial displacement. It is, therefore, adapted to function as a static stabiliser of the patella. In addition, it would also be expected that to fulfil this role the lateral retinaculum would have to be stiffer than the medial side because it is only attached to bone indirectly through the femoral and tibial attachments of the ITB. However, it is unclear why the lateral side requires an additional stronger structure in addition to the lateral capsular structures, the patellofemoral and patellomeniscal ligaments, which are comparable to the MPFL and the medial patellomeniscal ligament. We do know that the lateral retinacular structures help to resist patellar lateral subluxation when the knee is near extension (Christoforakis et al., 2006), and it has been shown recently that the transverse ITB–patellar band is slack when the knee is extended and tightens significantly in flexion (Ghosh et al., 2009), so it could be speculated that the ITB–patellar band acts when the knee is flexed. This has recently been shown: releasing the capsular structures reduced patellar medial stability significantly from 0° to 20° knee flexion, releasing the ITB–patellar band reduced the stability significantly from 30° to 90° knee flexion (Merican et al., 2009). Similarly, Ostermeier et al. (2007b) found that a lateral retinacular release allowed the patella to translate and tilt medially, compared with the intact condition, despite having not loaded the vastus lateralis or iliotibial band in their experiment.
Several factors act to limit the conclusions which may be drawn from this study; these should be noted. The specimens tested were from elderly donors. Work on the anterior cruciate ligament suggests that ligaments weaken with advancing age (Noyes and Grood, 1976; Woo et al., 1991). Moreover, bony resorption in the elderly may cause premature avulsion failure leading to lower tensile strength: the level of activity of the donors was not known and this may also be important. Another cause of variability in the data is the difficulty of aligning the tissue so that all the fibres are tensioned equally. If this is not achieved then sequential localised failures of the tissue occur and the maximal possible load may not be reached. In the lateral retinaculum, the fibres were not neatly oriented and aligned as in a more classical ligament. There was also difficulty with preparation of the patellomeniscal ligament as it was a thickening of the capsule without well-defined borders, so variability was introduced by the dissector's interpretation of the limits of this ligament. Nonetheless, the variability as reflected by the standard deviation was comparable to other works using similar experimental protocols (Mountney et al., 2005; Robinson et al., 2005). Freezing jaws which used liquid carbon dioxide were used to clamp the irregular and slippery test specimens. The freeze clamp can go to −80 °C. We did not attempt to keep the clamp temperature constant, because tissue has very low conductivity, so it did not freeze in the tested tissue band, only within the metal jaws. We never had a failure of this system in this study, and have experience of tensile tests to failure of long tendons, which supported much higher stresses, without slipping (Pring et al., 1985). Finally, we were not sure how to orient the line of tension in relation to the patella, so chose to pull in the plane of the patella, because we estimated that to be the direction which would result when the patella has been displaced medially and the lateral retinaculum had to pass over the lateral edge of the trochlea.
This study has provided novel data on the strength and stiffness of the principal soft tissue structures attaching to the lateral aspect of the patella. The transverse fibres that link the ITB to the patella were much stronger and stiffer than the lateral capsular structures: the patellofemoral and patellomeniscal ligaments. This suggests that the ITB–patellar band will take more of the load than the lateral patellofemoral and patellomeniscal ligaments if the patella is displaced medially, particularly when the knee is flexed. However, it should be noted that the tests in this study had the ITB clamped rigidly, while it is relatively mobile in-vivo. The ITB moves anteriorly beside the extending knee, so the ITB–patellar band is then slack and it is tight when the knee is flexed (Ghosh et al., 2009). This might provide a rationale for selective cutting, if patellar maltracking relates to a particular arc of knee flexion. It had been hypothesised that the structural properties of lateral retinacular fibre bands would provide a rationale for staged, partial, releases. To test this hypothesis, different parts of the ITB–patellar band would have to be isolated for testing. However, it was discovered that criss-crossing of the fibres between the ITB and the patella meant that this structure could not be cut into discrete parallel fibre bands, since attempts to do that would have compromised the strength by destroying end-to-end fibre continuity.
The structural characteristics of the tissue bands tested in this study suggest that arthroscopic releases of the capsular ligaments will still leave most of the strength and stiffness of the lateral retinaculum, even if they have become pathologically tight or thickened, because of the much higher strength and stiffness of the fibres that link the ITB to the lateral edge of the patella. Conversely, a release performed from outside–in, that leaves the capsular structures intact, will leave only relatively weak, low stiffness, restraints to patellar medial displacement. However, this study has now shown that the LPFL has similar properties to the medial patellofemoral ligament. While this study has found the strength and stiffness of the lateral retinacular tissue bands attaching to the patella, the data should be used in conjunction with other studies, including the effects of cutting them on patellar stability or tracking, before any recommendations about clinical practise can be made.
Conflict of interest
The authors confirm that no benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. There are no potential conflicts of interest (employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding) or financial and personal relationships with other people or organisations that influences or introduces bias in the results and interpretation of this work.
Acknowledgements
Azhar M. Merican was supported by the University of Malaya Medical Centre, Kuala Lumpur and the Arthritis Research Campaign (ARC). The ARC provided the Instron machine and the knee specimens were funded by a grant from the ARC.
References
- Amis A.A., Firer P., Mountney J., Senavongse W., Thomas N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- Arendt E.A., Fithian D.C., Cohen E. Current concepts of lateral patella dislocation. Clin. Sports Med. 2002;21(3):499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- Atkin D.M., Fithian D.C., Marangi K.S., Stone M.L., Dobson B.E., Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am. J. Sports Med. 2000;28(4):472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- Blauth M., Tillmann B. Stressing on the human femoro-patellar joint. I. Components of a vertical and horizontal tensile bracing system. Anat. Embryol. (Berlin) 1983;168(1):117–123. doi: 10.1007/BF00305403. [DOI] [PubMed] [Google Scholar]
- Brinker M.R., O’Connor D.P., Flandry F., Hughston J.C. Diagnosis and surgical correction of medial patellar subluxation. Op. Tech. Sports Med. 2001;9(3):183–189. [Google Scholar]
- Christoforakis J., Bull A.M., Strachan R.K., Shymkiw R., Senavongse W., Amis A.A. Effects of lateral retinacular release on the lateral stability of the patella. Knee Surg. Sports Traumatol. Arthrosc. 2006;14(3):273–277. doi: 10.1007/s00167-005-0699-5. [DOI] [PubMed] [Google Scholar]
- Ghosh K.M., Merican A.M., Iranpour-Boroujeni F., Deehan D.J., Amis A.A. Length change patterns of the extensor retinaculum and the effect of total knee replacement. J. Orthop. Res. 2009;27:865–870. doi: 10.1002/jor.20827. [DOI] [PubMed] [Google Scholar]
- Hsu H.C., Luo Z.P., Rand J.A., An K.N. Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J. Arthroplasty. 1997;12(1):74–83. doi: 10.1016/s0883-5403(97)90051-6. [DOI] [PubMed] [Google Scholar]
- Hughston J.C., Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am. J. Sports Med. 1988;16(4):383–388. doi: 10.1177/036354658801600413. [DOI] [PubMed] [Google Scholar]
- Hughston J.C., Flandry F., Brinker M.R., Terry G.C., Mills J.C. Surgical correction of medial subluxation of the patella. Am. J. Sports Med. 1996;24(4):486–491. doi: 10.1177/036354659602400413. [DOI] [PubMed] [Google Scholar]
- Ishibashi Y., Okamura Y., Otsuka H., Tsuda E., Toh S. Lateral patellar retinaculum tension in patellar instability. Clin. Orthop. Relat. Res. 2002;(397):362–369. doi: 10.1097/00003086-200204000-00042. [DOI] [PubMed] [Google Scholar]
- Ishii Y., Terajima K., Terashima S., Koga Y. Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin. Orthop. Relat. Res. 1997;(343):144–150. [PubMed] [Google Scholar]
- Lattermann C., Toth J., Bach B.R., Jr. The role of lateral retinacular release in the treatment of patellar instability. Sports Med. Arthrosc. 2007;15(2):57–60. doi: 10.1097/JSA.0b013e318042af30. [DOI] [PubMed] [Google Scholar]
- Luo Z.P., Sakai N., Rand J.A., An K.N. Tensile stress of the lateral patellofemoral ligament during knee motion. Am. J. Knee Surg. 1997;10(3):139–144. [PubMed] [Google Scholar]
- Marumoto J.M., Jordan C., Akins R. A biomechanical comparison of lateral retinacular releases. Am. J. Sports Med. 1995;23(2):151–155. doi: 10.1177/036354659502300204. [DOI] [PubMed] [Google Scholar]
- Merican A.M., Amis A.A. Anatomy of the knee lateral retinaculum. J. Bone Joint Surg. Br. 2008;90B(4):527–534. doi: 10.1302/0301-620X.90B4.20085. [DOI] [PubMed] [Google Scholar]
- Merican A.M., Kondo K., Amis A.A. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J. Biomech. 2009;42:291–296. doi: 10.1016/j.jbiomech.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Miller P.R., Klein R.M., Teitge R.A. Medial dislocation of the patella. Skeletal Radiol. 1991;20(6):429–431. doi: 10.1007/BF00191085. [DOI] [PubMed] [Google Scholar]
- Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J. Bone Joint Surg. Br. 2005;87(1):36–40. [PubMed] [Google Scholar]
- Nomura E., Inoue M., Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg. Sports Traumatol. Arthrosc. 2005;13(7):510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- Nonweiler D.E., Delee J.C. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am. J. Sports Med. 1994;22(5):680–686. doi: 10.1177/036354659402200517. [DOI] [PubMed] [Google Scholar]
- Noyes F.R., Grood E.S. The strength of the anterior cruciate ligament in humans and Rhesus monkeys. J. Bone Joint Surg. Am. 1976;58(8):1074–1082. [PubMed] [Google Scholar]
- Ostermeier S., Holst M., Bohnsack M., Hurschler C., Stukenborg-Colsman C., Wirth C.J. In vitro measurement of patellar kinematics following reconstruction of the medial patellofemoral ligament. Knee Surg. Sports Traumatol. Arthrosc. 2007;15(3):276–285. doi: 10.1007/s00167-006-0200-0. [DOI] [PubMed] [Google Scholar]
- Ostermeier S., Holst M., Hurschler C., Windhagen H., Stukenborg-Colsman C. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg. Sports Traumatol. Arthrosc. 2007;15:547–554. doi: 10.1007/s00167-006-0261-0. [DOI] [PubMed] [Google Scholar]
- Panagiotopoulos E., Strzelczyk P., Herrmann M., Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg. Sports Traumatol. Arthrosc. 2006;14(1):7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- Pring D.J., Amis A.A., Coombs R.R.H. The mechanical properties of digital flexor tendons related to artificial tendons. J. Hand Surg. 1985;10B:331–336. doi: 10.1016/s0266-7681(85)80055-3. [DOI] [PubMed] [Google Scholar]
- Reider B., Marshall J.L., Koslin B., Ring B., Girgis F.G. The anterior aspect of the knee joint. J. Bone Joint Surg. Am. 1981;63(3):351–356. [PubMed] [Google Scholar]
- Robinson J.R., Bull A.M., Amis A.A. Structural properties of the medial collateral ligament complex of the human knee. J. Biomech. 2005;38(5):1067–1074. doi: 10.1016/j.jbiomech.2004.05.034. [DOI] [PubMed] [Google Scholar]
- Wackerhagen A., Bodem F., Hopf C., Palme E. The influence of lateral release on patello-femoral joint loading in knee arthroplasty. An experimental in vitro study. Int. Orthop. 1992;16(1):19–24. doi: 10.1007/BF00182978. [DOI] [PubMed] [Google Scholar]
- Woo S.L., Hollis J.M., Adams D.J., Lyon R.M., Takai S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am. J. Sports Med. 1991;19(3):217–225. doi: 10.1177/036354659101900303. [DOI] [PubMed] [Google Scholar]