Abstract
Purpose
To compare visual acuity results obtained using the Lea Symbols chart with results obtained using Early Treatment Diabetic Retinopathy Study (ETDRS) charts in young children who are members of a population with a high prevalence of astigmatism.
Methods
Subjects were 438 children aged 5 through 7 years who were enrolled in kindergarten or 1st grade on the Tohono O’odham Reservation: 241 (55%) had astigmatism ≥1.00 D in one or both eyes (range, 0.00 to 6.75 D). While wearing best correction, each child had right eye visual acuity tested with the 62 cm by 65 cm Lea Symbols chart at 3 m and with the 62 cm by 65 cm ETDRS chart at 4 m. Visual acuity was scored as the smallest optotype size at which the child correctly identified 3 out of a maximum of 5 optotypes. ETDRS visual acuity was also scored based on the total number of letters that the child correctly identified.
Results
Correlation between Lea Symbols visual acuity and ETDRS visual acuity was 0.78 (p < 0.001). Mean Lea Symbols visual acuity was one-half line (0.04 to 0.06 logMAR) better than mean ETDRS visual acuity (p < 0.001). Difference between Lea Symbols and ETDRS visual acuity was not correlated with the mean of the Lea Symbols and ETDRS visual acuity scores, which ranged from −0.3 logMAR (20/10) to 0.74 logMAR (20/110).
Conclusions
In this population of young children, in whom the primary source of reduced visual acuity is astigmatism-related amblyopia, the Lea Symbols chart produced visual acuity scores that were about 0.5 line better than visual acuity scores obtained with ETDRS charts.
The Early Treatment Diabetic Retinopathy Study (ETDRS) charts1 are considered to be a gold standard for assessment of visual acuity because the charts meet the Committee on Vision standards for assessment of visual acuity2 through the use of optotypes (Sloan letters) equivalent in difficulty to the Landolt ring, through a spacing of 0.1 log unit in optotype size between lines, and through proportional spacing between optotypes on each line. However, ETDRS charts may not be usable with preschool-aged children because of the difficulty young children have in identifying the ten letters on the chart. The Lea Symbols chart3 was developed to provide a chart that conforms to the Committee on Vision standards2 and that can be used with children too young to be tested with Sloan letters or Landolt rings. It uses optotypes (square, circle, house, heart) that are sized to provide acuity scores equivalent to scores based on an adult eye chart,3 lines that progress in 0.1 log unit steps, and optotypes that are spaced proportionally.
Previous studies have found that in older children and adults Lea Symbols visual acuity is 0.5 to 2 lines better than visual acuity measured with non-logMAR Landolt C charts4 or with Bailey-Lovie logMAR letter charts,5 and the difference is greater for poorer acuity scores than for better scores.4,5 In addition, preliminary results from 1st grade children found Lea Symbols visual acuity to be approximately 0.5 line better than ETDRS visual acuity.6 However, there have been no large-scale comparisons of visual acuity results obtained with Lea Symbols and ETDRS charts in the same individuals.
The present report aims to compare best-corrected visual acuity results obtained using the Lea Symbols chart with results obtained with an ETDRS chart in a large sample of young children. These children are members of a Native American tribe (Tohono O’odham) known to have a high prevalence of astigmatism and astigmatism-related amblyopia.7–9
Methods
Subjects
Subjects were 482 children who were enrolled in kindergarten or 1st grade in a school on the Tohono O’odham Reservation in southern Arizona during the 2005/2006, 2006/2007, or 2007/2008 academic years. All were participants in a longitudinal study of the development and treatment of astigmatism-related amblyopia, in children age 6 months through 1st grade. All study participants who are at least three years of age undergo an eye examination with cycloplegic refraction, followed by assessment of visual acuity and other aspects of visual function while wearing spectacles containing best correction. Although some children completed exams during more than one academic year, only data from the first eye examination were used in the analyses.
The study was approved by the Tohono O’odham Nation and by the Institutional Review Board of the University of Arizona and conformed to the requirements of the United States Health Insurance Portability and Privacy Act. Parents provided written informed consent prior to the child’s participation.
Procedures
Each subject was scheduled to participate in two testing sessions. The first session, which was conducted by a pediatric ophthalmologist (JMM) or optometrist (KG), included cycloplegic refraction 40 to 60 minutes after instillation of 1 drop of proparacaine (0.5%) followed by 2 drops of cyclopentolate (1%) 5 minutes apart. Children were prescribed spectacles if they had astigmatism ≥2.00 D in either eye or if they had uncorrected letter visual acuity (measured during the first session) worse than 20/20 in either eye and met one or more of the following criteria in either eye: myopia ≥0.75 D in either meridian, hyperopia ≥4.00 D in either meridian, astigmatism ≥1.00 D, or anisometropia >1.50 D spherical equivalent.10 Correction of hyperopic refractive error was reduced by one-third or by 1.00 D, whichever was greater.11
The second session, conducted several weeks after the eye examination, included assessment of best-corrected visual acuity of the right eye, using Lea Symbols charts (Precision Vision, Inc., La Salle, IL),3 and assessment of best-corrected logMAR letter visual acuity of both the right eye and left eye, using ETDRS charts.1 During visual acuity testing, all subjects wore spectacles containing best correction in order to minimize variability of accommodative demand across subjects and to mask testers to which children had refractive error high enough that they were prescribed spectacles. Children who did not meet the prescribing criteria for spectacles wore a pair of “stock” spectacles that contained right and left lenses with no more than 0.50 vector dioptric difference12–14 from the child’s cycloplegic refraction with reduction of hyperopia correction, as noted above. Children for whom spectacles had been prescribed wore their new spectacles for the first time during vision testing; these spectacles were dispensed to the children at the end of the vision testing session.
Following fitting of the spectacles to be worn during vision testing, the child’s left eye was occluded with 5 cm wide adhesive paper tape (3M Micropore, Minneapolis, MN) and the spectacles were placed on the child’s face. Then, a study-trained vision tester measured the Lea Symbols visual acuity of the right eye of each child at a distance of 3 m, using a 62 cm by 65 cm logMAR chart with five symbols per line, mounted in an illuminator cabinet (Precision Vision, Inc., LaSalle, IL). Immediately thereafter, the trained vision tester measured the ETDRS visual acuity of the right eye and the left eye at a distance of 4 m, using a 62 cm by 65 cm logMAR chart (Precision Vision Inc., LaSalle, IL; Chart 1 for the right eye, Chart 2 for the left eye) with five letters per line, mounted in the illuminator cabinet. The protocol of the longitudinal study in which the children were enrolled required testing of Lea Symbols acuity prior to testing of ETDRS acuity.
Vision testing began with the top line on the chart (20/200). The child was asked to name, or to match to symbols on a lap card, the symbols on each line on the Lea Symbols chart. As soon as the child correctly identified 3 of the 5 symbols on a line, the tester was permitted to ask the child to begin identifying symbols on the next smaller line. Acuity was scored as the smallest symbol size on which the child identified at least 3 of the 5 symbols on the line.
For the ETDRS charts, the child was asked to name, or to match to letters on a lap card, all 5 of the symbols on each line on the chart. Acuity was scored as the smallest letter size on which the child identified at least 3 letters correctly, a line-by-line scoring method that is identical to that used for the Lea Symbols chart and has been used in studies of children.15,16 ETDRS acuity was also scored based on the total number of letters identified correctly, ie, a letter-by-letter scoring method that is traditionally used with the ETDRS charts and that provides better reliability of scores than do other methods of scoring.17
Data Analysis
Acuity scores were transformed to log values for data analysis. For scoring of ETDRS results based on the child’s reading of all letters, the following formula, which assigns a value of 0.02 log unit to each letter identified, was used to transform scores to logMAR values:
where Tc = the total number of letters identified correctly.
Results
Study Sample
A total of 482 kindergarten and 1st grade children were enrolled in the study and completed the eye examination between September 2005 and August 2008. Data were excluded from three children who refused cycloplegic drops at the eye examination, 16 children who were older than eight years of age at the eye vision testing session, and 25 children who did not complete the vision testing session. The mean age of the final sample of 438 children was 6.2 years (SD 0.6; range, 5.2 to 7.8 years) at the eye exam, and 6.4 years (SD 0.6; range, 5.3 to 7.9 years) on the day of vision testing. All 438 children completed both Lea Symbols and ETDRS acuity testing.
Based on the results of the eye examination, conducted 5 to 235 days (mean 43.0 days, SD 31.3) prior to assessment of visual acuity, 248 children (56.6%) met one or more refractive error criteria for eyeglass prescription: 241(55.0%) had astigmatism ≥1.00 D in one or both eyes (range, 0.00 to 6.75 D), 97 (22.1%) had myopia ≥0.75 D in either meridian, 61 (13.9%) had hyperopia ≥4.00 D in either meridian, and 9 (2.1%) had anisometropia >1.50 D spherical equivalent.
Visual Acuity Results: Comparison of Lea Symbols and ETDRS Scores
Best-corrected logMAR acuity ranged from −0.30 to 0.70 (20/10 to 20/100) for both the Lea Symbols and the ETDRS charts using the line-by-line scoring method, and from −0.18 to 0.74 (20/13 to 20/110) for letter-by-letter scoring of ETDRS data.
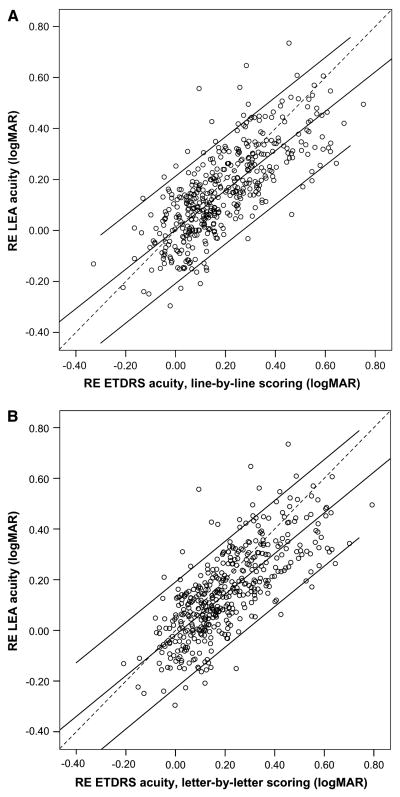
Figure 1 provides comparisons of (A) Lea Symbols and (B) ETDRS visual acuity results for the 438 study participants. Correlation between Lea Symbols and ETDRS line-by-line visual acuity, and between Lea Symbols and ETDRS letter-by-letter scoring, was 0.78 (p < 0.001). The correlation between ETDRS line-by-line and letter-by-letter visual acuity was 0.96 (p < 0.001).
FIG 1.
Lea Symbols versus Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity results for the 438 5- to 7-year-old study participants, with ETDRS visual acuity determined using line-by-line (A) and letter-by-letter (B) scoring. Correlation between Lea Symbols and ETDRS visual acuity was 0.78 (p < 0.001). Dashed line represents perfect agreement between Lea Symbols and ETDRS visual acuity, solid lines represent regression line and 95% confidence interval.
Overall, mean Lea Symbols visual acuity (0.15 logMAR [20/28], SD 0.17) was approximately one-half line (2 to 3 letters) better than mean ETDRS line-by-line visual acuity (0.19 logMAR [20/31], SD 0.17, t437 = 7.41, p < 0.001) and ETDRS letter-by-letter visual acuity (0.21 logMAR [20/32], SD 0.17, t437 = 11.22, p < 0.001). The difference between Lea Symbols and ETDRS visual acuity (for both line-by-line and letter-by-letter scoring) did not differ significantly across age groups (5- vs 6- vs 7-year-olds).
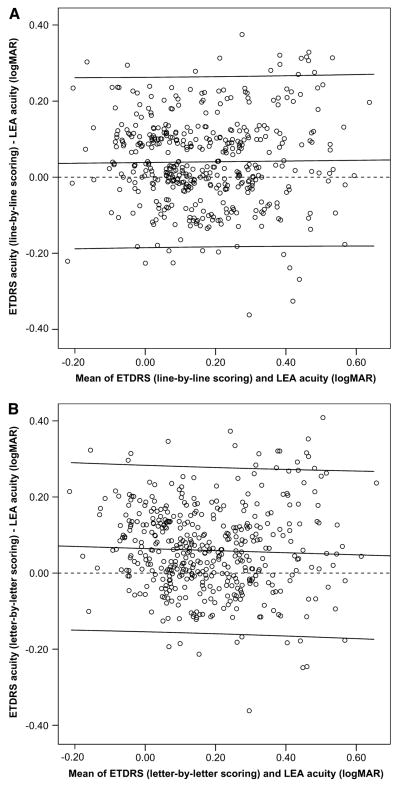
Figures 2 presents Bland-Altmann18 plots showing the difference between Lea Symbols and ETDRS visual acuity versus the mean of the visual acuity scores obtained with the Lea Symbols and ETDRS charts. There were no significant correlations between the difference between Lea Symbols and ETDRS acuity scores (for both line-by-line and letter-by-letter scoring) and the mean visual acuity.
FIG 2.
Difference between Lea Symbols and Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity plotted as a function of the mean of the visual acuity scores obtained with the Lea Symbols and ETDRS charts, with ETDRS visual acuity determined using line-by-line (A) and letter-by-letter (B) scoring. There was no significant correlation between the difference between Lea Symbols and ETDRS visual acuity scores and the mean of the scores. Dashed line represents perfect agreement between Lea Symbols and ETDRS visual acuity, solid lines represent regression line and 95% confidence interval.
Discussion
The present study provides the first large-scale comparison of Lea Symbols and ETDRS visual acuity in young children. The results indicate that while visual acuity results obtained with the Lea Symbols chart are significantly correlated with visual acuity results obtained with ETDRS charts, Lea Symbols visual acuity scores are, on average, 0.5 line (0.04 to 0.06 log unit) better than visual acuity scores obtained with ETDRS charts. There was no significant relation between the difference in scores on the two charts and acuity level (Figure 2). The finding that children show better visual acuity when tested with Lea Symbols than with ETDRS charts is in agreement with preliminary data from a similar population.6 In addition, the results are in agreement with previous studies that have found better visual acuity when patients were tested with Lea Symbols than when they were tested with either a non-logMAR Landolt C test4 or with the logMAR Bailey-Lovie chart.5 In contrast to the present results, however, both previous studies showed that the difference between Lea Symbols visual acuity and visual acuity obtained with standard adult logMAR acuity tests is greater at low acuity levels than for acuity scores within the normal range.4,5 The failure to find a relation between visual acuity level and the difference between Lea Symbols and ETDRS visual acuity in the present study may be related to the relatively narrow range of visual acuity scores (worst acuity was 0.74 logMAR [20/110]), compared to the much greater range of visual acuity scores of subjects in the two previous studies.4,5 That is, the finding of a relatively large difference between Lea Symbols and ETDRS visual acuity may be evident only at lower acuity levels than were obtained in the present study.
A possible explanation for the better acuity scores obtained with the Lea Symbols chart than with the ETDRS and Bailey-Lovie charts is that the Lea Symbols test includes only four optotypes, whereas ten optotypes are used in the ETDRS and Bailey-Lovie charts. This means that as acuity threshold is approached, the individual has a 25% chance of guessing the correct symbol in the Lea Symbols chart, but only a 10% chance of guessing the correct letter in the Bailey-Lovie and ETDRS charts, which could result in a better acuity score due to correct guessing with the Lea Symbols chart.
Another factor that may contribute to differences in visual acuity obtained with Lea Symbols versus ETDRS, Landolt C, and Bailey-Lovie charts is the difference in optotypes used in the different tests (symbols vs letters). Although the designer of the Lea Symbols chart empirically determined that in normal adults tested with optotypes presented at various distances, the Lea Symbols optotype sizes produced visual acuity scores that were equivalent to those produced by optotypes of the same acuity level on the Snellen E chart,3 and to optotypes of the same acuity level on the Landolt C chart (Hyvärinen, personal communication, 1999), it is possible that in children, and in patients with ocular abnormalities, the visual acuity results from the two types of optotypes are not equivalent. In addition, it is possible that the young children’s interest in the testing was better maintained by a chart containing familiar shapes than by a chart composed of less familiar letters.
The present study has both strengths and limitations. An important strength is the large sample size: data were obtained from 438 children who were tested with both the Lea Symbols and ETDRS charts in the same session. In addition, ETDRS acuity was scored using a method identical to the method used for LEA acuity scoring (ie, the line-by-line method) as well as the scoring method traditionally used for the ETDRS charts (ie, the letter-by-letter method). The fact that the pattern of results was the same with both scoring methods suggests that the difference between ETDRS and LEA acuity was not related to the scoring method used to determine visual acuity.
A limitation is the possibility that the poorer scores obtained with ETDRS charts vis-à-vis the Lea Symbols chart may have been related to fatigue or boredom. The following may have been causes of fatigue or boredom: (1) protocol requirements of the larger study in which these children were participants—Lea Symbols acuity was always tested before ETDRS acuity; (2) the ETDRS task, which requires the child to identify 10 letter optotypes, is more difficult than the Lea Symbols task, which requires the child to identify 4 symbol optotypes; (3) for ETDRS testing, children were required to identify all letters on each line, whereas in the Lea Symbols chart, children were permitted to skip the last 2 symbols on a line if they identified the first 3 correctly. However, in at least one of the previous studies that reported better visual acuity with Lea Symbols than with an adult visual acuity chart,5 order of testing was varied, suggesting that the unvaried order of testing may not have been an important factor in the present study.
Another limitation of the present study is the relatively restricted range of acuity scores that were generated by the subjects. The worst Lea Symbols visual acuity obtained was 20/100, and the worst ETDRS visual acuity was 20/110. Thus the results do not provide information about agreement between Lea Symbols and ETDRS visual acuity at acuity levels worse than about 20/100.
In conclusion, the results of the present study suggest that although there is a significant correlation between visual acuity scores obtained with Lea Symbols and ETDRS charts, the Lea Symbols chart may overestimate the acuity score measured by the ETDRS letter chart in young children. Alternatively, it could be argued that ETDRS charts underestimate visual acuity in the young child, as a result of the difficulty of the task involved and the unfamiliarity of letter optotypes to young children.
Acknowledgments
Supported by grant U10 EY13153 (EMH) from the National Eye Institute of the National Institutes of Health, Department of Health and Human Services, by unrestricted funds to the Department of Ophthalmology and Vision Science from Research to Prevent Blindness (JMM), and by a Career Development Award from Research to Prevent Blindness (EMH). The authors thank the Tohono O’odham Nation, the Indian Oasis/Baboquivari School District, the Bureau of Indian Affairs Office of Indian Education Programs (BIA OIEP, Papago/Pima Agency), the San Xavier Mission School, and our NIH/NEI Data Monitoring and Oversight Committee (Maureen Maguire, PhD [former chair], Robert Hardy, PhD [current chair], Morgan Ashley, Donald Everett, MA, Jonathan Holmes, MD, Cynthia Norris, and Karla Zadnik, OD, PhD).
Footnotes
Study conducted at: University of Arizona
Presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, May 6–10, 2007.
The authors have no financial interest in any of the tests used in this study.
References
- 1.Ferris FL, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–6. [PubMed] [Google Scholar]
- 2.Committee on Vision. Recommended standard procedures for the clinical measurement and specification of visual acuity. Adv Ophthalmol. 1980;41:103–48. [PubMed] [Google Scholar]
- 3.Hyvärinen L, Näsänen R, Laurinen P. New visual acuity test for pre-school children. Acta Ophthalmol (Copenh) 1980;58:507–11. doi: 10.1111/j.1755-3768.1980.tb08291.x. [DOI] [PubMed] [Google Scholar]
- 4.Gräf MH, Becker R, Kaufmann H. Lea Symbols: Visual acuity assessment and detection of amblyopia. Graefe’s Arch Cliin Exp Ophthalmol. 2000;238:53–8. doi: 10.1007/s004170050009. [DOI] [PubMed] [Google Scholar]
- 5.Vision In Preschoolers (VIP) Study Group. Visual acuity results in school-aged children and adults: Lea Symbols chart versus Bailey-Lovie Chart. Optom Vis Sci. 2003;80:650–54. doi: 10.1097/00006324-200309000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Harvey EM, Miller JM, Dobson V, Lopez CA, Lopez FM. A comparison of ETDRS (letter) acuity and Lea (symbol) acuity in a first grade population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 1998;39:S947. [Google Scholar]
- 7.Dobson V, Miller JM, Harvey EM. Corneal and refractive astigmatism in a sample of 3- to 5-year-olds with a high prevalence of astigmatism. Optom Vis Sci. 1999;76:855–60. doi: 10.1097/00006324-199912000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Dobson V, Miller JM, Harvey EM, Sherrill DL. Vision Science and Its Applications: February 19–22, 1999, Santa Fe, New Mexico. Washington: Optical Society of America; 1999. Prevalence of astigmatism, astigmatic anisometropia, and glasses wearing among preschool- and school-age Native American children; pp. 177–80. OSA Technical Digest Series. [Google Scholar]
- 9.Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism, eyeglass wear, and poor visual acuity among Native American grade-school children. Optom Vis Sci. 2006;83:206–12. doi: 10.1097/01.opx.0000214333.84822.71. [DOI] [PubMed] [Google Scholar]
- 10.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Amblyopia in astigmatic children: Patterns of deficits. Vision Res. 2007;47:315–26. doi: 10.1016/j.visres.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guyton DL, Miller JM, West CE. Optical pearls and pitfalls: Tricks and traps in strabismus. In: Wright KW, Speigel PH, editors. Pediatric Ophthalmology and Strabismus. 2. New York: Springer; 2003. pp. 292–6. [Google Scholar]
- 12.Long WF. A matrix formalism for decentration problems. Am J Optom Physiol Opt. 1976;53:27–33. doi: 10.1097/00006324-197601000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Harris WF. The mean and variance of samples of dioptric powers: the basic calculations. Clin Exp Optom. 1990;73:89–92. [Google Scholar]
- 14.Harvey EM, Miller JM, Dobson V, Tyszko R, Davis AL. Measurement of refractive error in Native American preschoolers: Validity and reproducibility of autorefraction. Optom Vis Sci. 2000;77:140–9. doi: 10.1097/00006324-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: Snellen visual acuity and structural outcome at 5½ years after randomization. Arch Ophthalmol. 1996;114:417–424. doi: 10.1001/archopht.1996.01100130413008. [DOI] [PubMed] [Google Scholar]
- 16.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. Ophthalmological outcomes at 10 years. Arch Ophthalmol. 2001;119:1110–18. doi: 10.1001/archopht.119.8.1110. [DOI] [PubMed] [Google Scholar]
- 17.Arditi A, Cagenello R. On the statistical reliability of letter-chart visual acuity measurements. Invest Ophthalmol Vis Sci. 1993;34:120–29. [PubMed] [Google Scholar]
- 18.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]