Abstract
Objective
The authors sought to evaluate the association of self-efficacy with objective measures of cardiac function, subsequent hospitalization for heart failure (HF), and all-cause mortality.
Design
Observational cohort of ambulatory patients with stable CHD. The authors measured self-efficacy using a published, validated, 5-item summative scale, the Sullivan Self-Efficacy to Maintain Function Scale. The authors also performed a cardiac assessment, including an exercise treadmill test with stress echocardiography.
Main Outcome Measures
Hospitalizations for HF, as determined by blinded review of medical records, and all-cause mortality, with adjustment for demographics, medical history, medication use, depressive symptoms, and social support.
Results
Of the 1,024 predominately male, older CHD patients, 1013 (99%) were available for follow-up, 124 (12%) were hospitalized for HF, and 235 (23%) died during 4.3 years of follow-up. Mean cardiac self-efficacy score was 9.7 (SD 4.5, range 0–20), corresponding to responses between “not at all confident” and “somewhat confident” for ability to maintain function. Lower self-efficacy predicted subsequent HF hospitalization (OR per SD decrease = 1.4, p = 0006), and all-cause mortality (OR per SD decrease = 1.4, p < .0001). After adjustment, the association of cardiac self-efficacy with both HF hospitalization and mortality was explained by worse baseline cardiac function.
Conclusion
Among patients with CHD, self-efficacy was a reasonable proxy for predicting HF hospitalizations. The increased risk of HF associated with lower baseline self-efficacy was explained by worse cardiac function. These findings indicate that measuring cardiac self-efficacy provides a rapid and potentially useful assessment of cardiac function among outpatients with CHD.
Keywords: self-efficacy, heart failure, epidemiology
As mortality from coronary heart disease (CHD) improves in the acute setting, improving care and outcomes for those with stable CHD assumes greater importance for public health. Avoiding hospitalization for heart failure (HF) is an important goal for this population, and understanding predictors of HF is the first step toward targeted prevention measures. In addition to cardiac physiology, psychosocial factors may contribute to HF hospitalizations (Howie-Esquivel & Dracup, 2007; Jiang et al., 2007; Sherwood et al., 2007), through both increased physiologic stress and through patient behaviors such as inadequate medication adherence (Murray et al., 2007; Tu et al., 2005).
Self-efficacy is a psychological construct based on social–cognitive theory, which describes the interaction between behavioral, personal, and environmental factors in health and chronic disease (Bandura, 1977, 1997; Lorig & Holman, 2003). The theory of self-efficacy proposes that patients’ confidence in their ability to perform certain health behaviors influences their engagement in and actual performance of those behaviors (e.g., diet and exercise adherence), which in turn influence health outcomes. Indeed, the construct of self-efficacy has extended far beyond the psychological arena, and has been demonstrated to affect health behaviors and chronic disease management in many chronic diseases settings (Aljasem, Peyrot, Wissow, & Rubin, 2001; Arnold et al., 2005; Bernal, Woolley, Schenaul, & Dickinson, 2000; Clark & Dodge, 1999; Holden, 1991; Kavanagh, Gooley, & Wilson, 1993; McCaul, Glasgow, & Schafer, 1987). Importantly, self-efficacy is a modifiable characteristic; many health behavior interventions have been shown to improve patients’ self-efficacy (Lorig & Holman, 2003; Lorig et al., 2001; Maddigan et al., 2004; Oka, DeMarco, & Haskell, 2005).
In patients with cardiovascular disease, studies of self-efficacy have largely focused on its role in successful cardiac rehabilitation (Berkhuysen, Nieuwland, Buunk, Sanderman, & Rispens, 1999; Carlson et al., 2001; Ewart, Taylor, Reese, & DeBusk, 1983; Foster et al., 1995; Gardner et al., 2003; Izawa et al., 2005). In addition, one previous study found that self-efficacy predicted health status in 198 patients undergoing cardiac angiography (Sullivan, LaCroix, Russo, & Katon, 1998). In our previous work, we found that greater cardiac self-efficacy was associated with better health status in a cross-sectional study of patients with CHD (Sarkar, Ali, & Whooley, 2007).
We chose to examine HF for two reasons. First, HF requires complex self-management activities including not only medication adherence but also frequent weighing, and, for some patients, self-titration of diuretic medications. Because higher self-efficacy has been associated with better self-management across multiple chronic disease settings, we hypothesized that self-efficacy would be especially relevant to avoiding hospitalization for HF (Curtin et al., 2008; Sarkar, Fisher, & Schillinger, 2006; Subramanian, Hopp, Mitchinson, & Lowery, 2008; Wolf et al., 2007). Second, the symptoms of HF often vary substantially from day to day. Thus, day-to-day management of HF and its symptoms is much more challenging (and more likely to be influenced by self-efficacy) than management of CHD, in which day-to-day symptom levels do not usually fluctuate and hospitalizations are much more sudden/episodic.
Therefore, we sought to determine whether baseline cardiac self-efficacy would predict subsequent hospitalizations for HF within a population of 1024 outpatients with established CHD (CHD), and to assess whether this relationship would be independent of known demographic factors, psychosocial characteristics, and baseline cardiac function. In addition, because mortality is the ultimate endpoint for patients with CHD, we report the association between baseline self-efficacy and all-cause mortality in this cohort, with adjustment for other factors as above.
Method
Participants
The Heart and Soul Study is a prospective cohort study of psychosocial factors and health outcomes in patients with coronary disease. Data collection methods have been described in detail elsewhere (Bibbins-Domingo et al., 2007; Ruo et al., 2003; Ruo, Rumsfeld, Pipkin, & Whooley, 2004). Briefly, administrative databases were used to identify patients with one of the following eligibility criteria: a history of myocardial infarction, angiographic evidence of at least 50% stenosis of one or more coronary vessels, evidence of ischemia by treadmill or nuclear stress testing, or a history of coronary revascularization. The exclusion criteria were an intention to move out of the area within three years, a history of myocardial infarction within the last six months, or exercise tolerance less than 1 block, all of which precluded safe completion of the study.
Between September 2000 and December 2002, we recruited 1,024 participants with CHD from 2 Department of Veterans’ Affairs Medical Centers, 1 university hospital, and 9 public health clinics in the San Francisco Bay Area. These are the subjects of the current analysis. The baseline appointment included a medical history interview, a physical examination, an exercise treadmill test with a stress echocardiogram, and a comprehensive health status questionnaire. The protocol was approved by the institutional review boards at all participating facilities.
Outcomes: HF Hospitalization
We conducted annual telephone follow-up interviews with participants (or their proxy) to ask about death or hospitalizations. If any participant or proxy reported a hospitalization, we retrieved and reviewed the medical records for that hospitalization. Two independent and blinded adjudicators retrieved and reviewed medical records, electrocardiograms, death certificates, and coroner’s reports. If both adjudicators agreed on the outcome classification, it was binding. If there was disagreement, they conferred, reconsidered their classification, and requested consultation from a third, blinded adjudicator as necessary.
The outcome of interest, HF hospitalization, was defined as hospitalization for a clinical syndrome with ≥2 of paroxysmal nocturnal dyspnea, orthopnea, increased jugular venous pressure, pulmonary rales, third heart sound, cardiomegaly on chest X-ray, or pulmonary edema on chest X-ray, as determined by the adjudicators from reviewing medical records. These clinical signs and symptoms must have represented a clear change from the normal clinical state of the patient and been accompanied by either failing cardiac output, determined as peripheral hypoperfusion (hypotension in the absence of other causes, such as sepsis or dehydration) or peripheral or pulmonary edema. In addition to all the hospital records, supportive documentation of decreased cardiac index, increasing pulmonary capillary wedge pressure, decreasing oxygen saturation, and end-organ hypoperfusion, if available, were included in adjudication.
Outcome: All-Cause Mortality
For any reported death, medical records, coroner’s reports, and death certificates were reviewed. For this analysis, we include all causes of death.
Predictor: Cardiac Self-Efficacy
The main predictor of interest was cardiac self-efficacy, defined as participants’ confidence in their ability to take care of their health (Bandura, 1977, 1997). We measured cardiac self-efficacy using Sullivan’s validated 5-item summative “Maintain function” scale (Arnold et al., 2005; Berkhuysen et al., 1999; Salamah, Wahl, & Abriam-Yago, 2003; Sullivan et al., 1998). We elected to use a disease-specific measure because we hypothesized patients’ cardiac disease would be a strong driver of their self-efficacy, and that would be best captured by the well-validated, widely used Sullivan scale. Each item begins with the stem, “How confidant are you that you know or can,” and assesses an aspect of daily life-function, such as work and social activities (See Appendix). The responses are a 5-level Likert scale from 0 = “not at all confident” to 4 = “completely confident.” We did not include a “not applicable” response option. The self-efficacy scores range between 0 and 20, with a higher score indicating better self-efficacy to maintain function.
Cardiac Function
To evaluate whether differences in baseline cardiac function accounted for the relation between self-efficacy and HF, we performed three baseline measures of cardiac function: echocardiographic assessment of resting left ventricular ejection fraction (LVEF), exercise treadmill test for exercise capacity, and a stress echocardiogram for assessment of fixed and inducible ischemia (wall motion abnormalities). All of these variables are well-established measures of cardiac function (Braunwald et al., 2002).
A complete resting two-dimensional echocardiogram was performed on each participant. To determine the LVEF, standard two-dimensional parasternal short-axis and apical two-chamber and four-chamber views were used. Before and after exercise, we obtained apical two-chamber, four-chamber, and precordial long-and short-axis views to detect changes in wall motion or ventricular dilatation with exercise. To account for fixed and exertional wall motion defects (our measure of ischemia), we calculated the wall motion score at peak exercise. Each of 16 wall segments was evaluated for contractility at peak exercise, as follows 1 = normal, 2 = hypokinetic, 3 = akinetic, 4 = dyskinetic, 5 = aneurysm. The scores for each segment are averaged to create an index from 1–165 16, with a higher score indicating worse contractility.
Other Participant Characteristics
Participants reported demographic characteristics, including age, ethnicity, education, and marital status. Patients reported their annual household income, and because we were interested in low income as a risk factor, we dichotomized responses into less that $20,000 versus ≥$20,000 annual household income. Self-reported history of myocardial infarction, stroke, diabetes mellitus, or hypertension, as well as alcohol and tobacco use, were assessed by questionnaire. To account for other clinical characteristics that could affect HF hospitalization, we recorded use of medications such as beta-blockers, statins, renin-angiotensin system inhibitors, and antidepressants. Body-mass index (weight in kilograms divided by height in meters squared) was calculated for each participant.
Because we wanted to assess the independent contribution of self-efficacy, we chose to measure and adjust for several potentially related psychosocial variables (Cossette, Frasure-Smith, & Lesperance, 2001; Golden-Kreutz & Andersen, 2004; Ruo et al., 2003; Shyu, Tang, Tsai, Liang, & Chen, 2005; Spertus, McDonell, Woodman, & Fihn, 2000; Sullivan, LaCroix, Spertus, & Hecht, 2000). We measured depressive symptoms using the Patient Health Questionnaire-9 (Spitzer, Kroenke, & Williams, 1999), a validated measure in which a higher score indicates more depressive symptoms. We considered a score of 10 or higher as consistent with depressive symptoms (McManus, Pipkin, & Whooley, 2005). To assess perceived stress, we used the 16-point, 4-item Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983), in which experiencing at least one stressful symptom “fairly often,” or a score of 9 or higher, indicates stress. We asked participants “do you have as much contact as you like with someone you feel close to, someone in whom you can trust and confide (yes/no)?” to assess social support (Williams et al., 1992).
Statistical Analysis
We aimed to evaluate the associations between cardiac self-efficacy and baseline cardiac function, between cardiac self-efficacy and future HF hospitalization, and between cardiac self-efficacy and all-cause mortality. First, we examined the association of decreasing self-efficacy quartile with three measures of cardiac function at baseline. Next, we created Kaplan-Meier curves to depict heart-failure free survival, and overall survival, by quartile of cardiac self-efficacy.
To further evaluate the independent association of self-efficacy with HF hospitalization, we performed a sequential multivariate linear regression, per standard deviation (4.5-point decrease) in self-efficacy. Potential predictors were grouped a priori into five conceptually based blocks, and each block of variables was added sequentially into the model as follows: (a) demographic variables: age, gender, race, income, education, marital status; (b) medical history: hypertension, diabetes mellitus, prior myocardial infarction, prior coronary revascularization, prior stroke, body mass index; (c) medication use: beta-blocker, statin, renin-angiotensin system inhibitor, aspirin, antidepressant; (d) psychosocial characteristics: depressive symptoms, current tobacco use, poor social support, regular alcohol use, and perceived stress; (e) cardiac function variables: LVEF, wall motion index, and exercise capacity. We employed an identical procedure to elucidate the relationship between self-efficacy and all-cause mortality.
In all models, we tested for interactions between self-efficacy score and other psychosocial characteristics (depressive symptoms, social support, and perceived stress); and between self-efficacy and gender and nonwhite ethnicity and age. Results are reported as odds ratios with 95% confidence intervals. Analyses were performed using SAS version 9 (SAS Institute, Inc., Cary, NC).
Results
Patient Characteristics
Patients were older and predominantly male, with relatively low socioeconomic status (see Table 1). The cohort has significant disease burden, with a majority of patients reporting history of myocardial infarction (54%) and coronary revascularization (59%). The mean self-efficacy score was 9.7 (standard deviation 4.5, range 0–20, skewness 0.18) corresponding to responses between “not at all confident” and “somewhat confident” for all of the scale items. The Cronbach’s alpha for the scale was 0.80.
Table 1.
Characteristics of 1,024 Participants With Coronary Heart Disease
| N(%) or Mean (SD) | |
|---|---|
| Demographics | |
| Age | 67 ± 11 |
| Male | 839 (82) |
| White | 616 (60) |
| High school graduate | 891 (87) |
| Income < 20,000/year | 499 (49) |
| Married | 434 (43) |
| Medical history | |
| Hypertension | 723 (71) |
| Myocardial infarction | 548 (54) |
| Coronary revascularization | 604 (59) |
| Stroke | 147 (14) |
| Diabetes mellitus | 266 (26) |
| Body mass index | 28.4 ± 5.3 |
| Medication use | |
| Beta-blocker | 594 (58) |
| Statin | 656 (64) |
| Renin-angiotensin system inhibitor | 524 (51) |
| Aspirin | 793 (77) |
| Antidepressant | 188 (18) |
| Psychosocial factors | |
| Depressive symptoms ≥ 10 (PHQ ≥ 10) | 199 (19) |
| Current smoking | 202 (20) |
| Poor social support | 330 (32) |
| Regular alcohol use | 294 (29) |
| Perceived stress | 5.3 ± 3.2 |
| Cardiac function | |
| LV ejection fraction | .62 ± .10 |
| Wall motion score index | 1.2 ± .35 |
| Exercise capacity (METS) | 7.3 ± 3.3 |
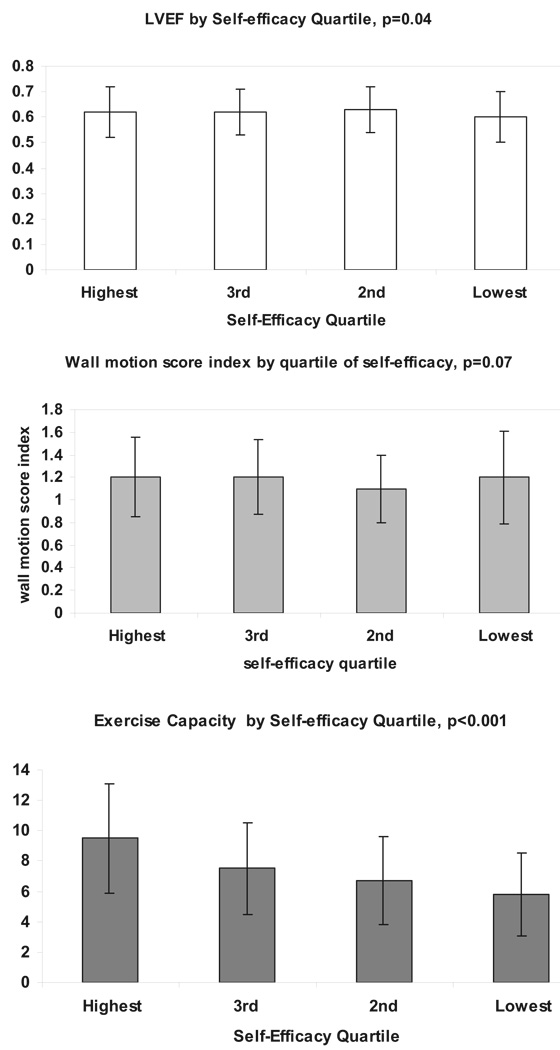
Self-Efficacy and Cardiac Function
We observed an association between lower self-efficacy score and worse baseline cardiac function. With each decreasing quartile of self-efficacy, the mean LVEF ( p for trend = 0.048), mean wall motion score index ( p = .07) and mean exercise capacity ( p for trend <0.001) decreased (see Figure 1).
Figure 1.
Baseline cardiac function by quartile of self-efficacy. With each decreasing quartile of self-efficacy, mean LVEF, wall motion index, and exercise capacity are lower.
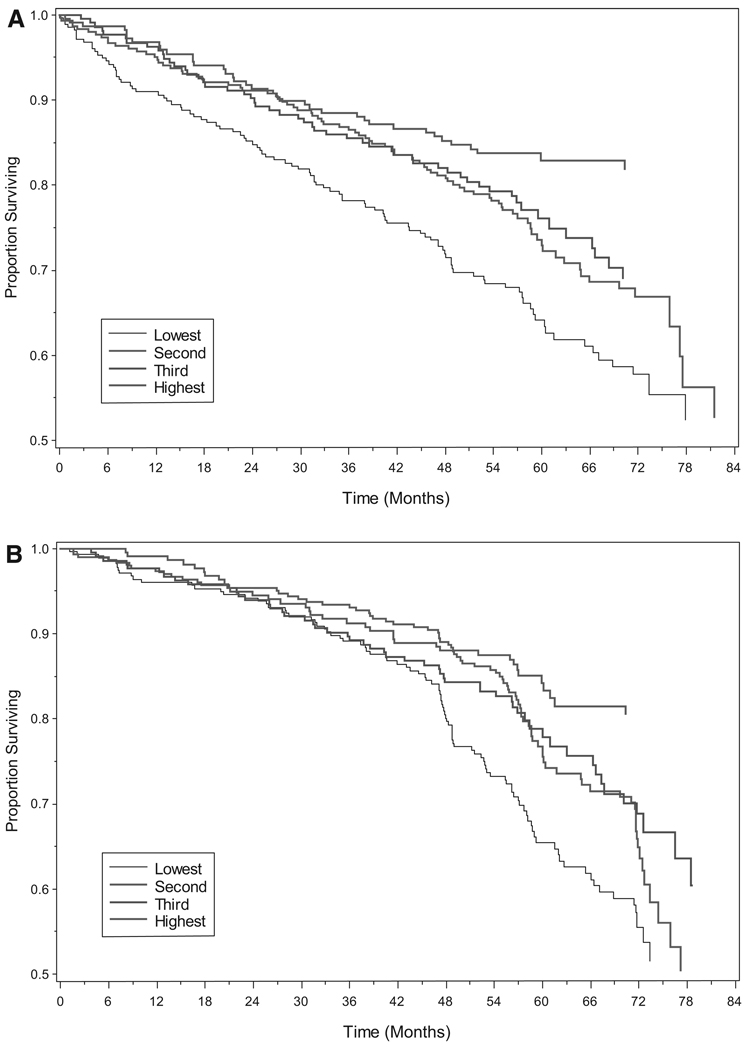
HF Hospitalizations and Mortality
During an average of 4.3 years of follow-up, 124 patients were hospitalized for HF, 235 died, and 9 were lost to follow-up. Figure 2 depicts the HF-free survival for each quartile of self-efficacy. Those with lower baseline self-efficacy were more likely to be hospitalized for HF. In fact, with each standard-deviation (22%) decrease in self-efficacy participants were 40% more like to be hospitalized for HF, and 30% more likely to die (Table 2)
Figure 2.
(A) HF hospitalization by quartile of self-efficacy. (B) All-cause mortality by quartile of self-efficacy.
Table 2.
Association. Between Self-Efficacy, Entered per Standard Deviation (4.5-Point) Decrease and Heart Failure Hospitalization, and All-Cause Mortality, in Participants With Coronary Disease, Adjusted for All Variables in Table 1*
| Heart failure hospitalization | All-cause mortality | |||
|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | |
| Unadjusted | 1.4 (1.1–1.7) | 0.0006 | 1.4 (1.2–1.6) | < 0.0001 |
| Adjusted for demographic characteristics | 1.3 (1.1–1.6) | 0.004 | 1.3 (1.1–1.6) | 0.0005 |
| Adjusted for above plus medical history | 1.3 (1.1–1.6) | 0.007 | 1.4 (1.1–1.6) | 0.0004 |
| Adjusted for above plus medication use | 1.3 (1.1–1.6) | 0.01 | 1.3 (1.1–1.6) | 0.002 |
| Adjusted for above plus psychosocial factors | 1.4 (1.1–1.7) | 0.01 | 1.4 (1.2–1.7) | 0.0003 |
| Adjusted for above plus cardiac function (LVEF, exercise capacity and wall motion score index) |
1.0 (0.8–1.4) | 0.91 | 1.2 (0.9–1.5) | 0.16 |
Other variables associated with heart failure (at p < .05) were older age, less education, history of diabetes mellitus, regular alcohol use, lower LV ejection fraction and lower exercise capacity. Other variables associated with mortality (at p < .05) were older age, male gender, lower body-mass-index, diabetes mellitus, antidepressant use, higher perceived stress, worse wall motion score index, and lower exercise capacity.
Self-Efficacy and HF Hospitalization
With stepwise adjustment for demographics, medical history, medication use, and psychosocial factors, self-efficacy remained independently predictive of heart failure hospitalization and death. However, after adjustment for baseline cardiac function, self-efficacy was no longer associated with future heart failure hospitalizations or all–case mortality (see Table 2).
There were no interactions between self-efficacy and the other psychosocial measures (depressive symptoms, social support, and perceived stress). We also did not find interactions of self-efficacy score with gender, race/ethnicity, age or cardiac function (all p values for interaction >0.10).
Discussion
Low self-efficacy was associated with worse baseline cardiac function and with increased risk of HF hospitalizations in 1024 ambulatory patients with CHD. Self-efficacy is thus a reasonable proxy for predicting future hospitalizations, but this observed association appears to be related to differences in baseline cardiac function. This suggests that self-reported cardiac self-efficacy provides a rapid, potentially useful assessment of cardiac function for ambulatory CHD patients. Thus, a patient’ own reported self-efficacy may add additional insight beyond the standard data in the ambulatory setting about their risk for hospitalization, and even mortality. This lends support to a more patient-centered view of ambulatory cardiac care.
These findings build on the growing body of evidence linking self-efficacy with physical health (Clark & Dodge, 1999; Lorig & Holman, 2003; Lorig et al., 2001). In prior studies, self-efficacy has been correlated with self-management behaviors for chronic conditions (Aljasem et al., 2001; Bernal et al., 2000; Kavanagh et al., 1993; McCaul et al., 1987). In small studies of selected groups, including patients undergoing cardiac rehabilitation (Berkhuysen et al., 1999; Carlson et al., 2001; Ewart et al., 1983; Foster et al., 1995; Gardner et al., 2003; Izawa et al., 2005) and cardiac catheterization (Sullivan et al., 1998), patients with chronic obstructive pulmonary disease (Arnold et al., 2005), and older women with congestive HF (Clark & Dodge, 1999), investigators have found an association between self-efficacy and health status. Our prior work found significant consistent associations between baseline self-efficacy and health status (Sarkar et al., 2007).
Our study further elucidates the self-efficacy—health outcome relationship in several ways. First, we measured self-efficacy at baseline and followed patients prospectively, avoiding the potential problem of reverse causation. Another strength of our study was our ability to adjust for psychosocial characteristics such as depressive symptoms, perceived stress, and social support, which could certainly play a role in HF hospitalization. Finally, because all participants underwent a detailed cardiac evaluation, we were able to include several objective measures of cardiac function in our analysis.
We recognize that the cross-sectional association between self-efficacy and baseline cardiac function can be interpreted in several ways. First, it may be that for patients with CHD, their cardiac function determines their self-efficacy, or their confidence in their ability to manage their health. Given that objective measures of cardiac function are not strongly associated with patient-reported health status, this seems less likely. Another possibility is that this particular self-efficacy measure, because it was developed and validated for cardiac patients, focuses on cardiac function more than overall function. However, the individual items in the self-efficacy scale do not allude to specific CHD symptoms or problems. Finally, it may be that this measure of self-efficacy provides a patient-reported measure or estimate of cardiac function, such that patients’ confidence accurately reflects their own functional abilities. This suggests that the Sullivan Self-efficacy to Maintain Function scale shows potential as a research instrument not only to estimate self-efficacy but also as a marker for baseline cardiac function among patients with stable CHD.
Despite its strengths, our study also has several limitations. First, most participants were older, lower-income males, and therefore the results may not be generalizable to other patient populations. Second, although a debate exists as to the utility of disease-specific versus global self-efficacy instruments (Clark & Dodge, 1999; Lorig et al., 2001), we elected to use a disease-specific measure. Third, we measured self-efficacy only at baseline. Self-efficacy may have worsened between study initiation and hospitalization, leading to an underestimate of the true effect of self-efficacy on hospitalization. Finally, because of the variety of self-efficacy measures in the literature (ranging from single item to in-depth cognitive interviews) we cannot accurately compare the effect sizes for the self-efficacy—health status associations we found to those in other studies.
In summary, understanding risks for HF hospitalization, and for mortality, is an important goal for chronic management of cardiovascular disease. We found that patient self-efficacy is predictive of HF hospitalization and all-cause mortality, and that this relationship is entirely explained by worse baseline cardiac function among participants with low self-efficacy. These results suggest that self-efficacy is a marker for patients’ cardiac function, and this may contribute to its role in CHD outcomes.
Acknowledgments
Urmimala Sarkar is supported by National Research Service Awards Grant No. 1 T32 HP19025. This work was supported by grants from the Department of Veterans Affairs (Epidemiology Merit Review Program), the Robert Wood Johnson Foundation (Generalist Physician Faculty Scholars Program), the American Federation for Aging Research (Paul Beeson Faculty Scholars in Aging Research Program), the Ischemia Research and Education Foundation, and the Nancy Kirwan Heart Research Fund. None of these funding sources had any role in the collection of data, interpretation of results, or preparation of this article.
Appendix
Cardiac Self-Efficacy Scale
How confident are you that you can
…Maintain your usual social activities?
…Maintain your usual activities at home?
…Maintain your usual activities outside of your home?
…Engage in sexual activity?
…Get aerobic exercise (work up a sweat and increase your heart rate)?
Note: Responses scale is Not at all confident (0), Somewhat confident (1), Moderately confident (2), Very confident (3), or Completely confident (4).
Contributor Information
Urmimala Sarkar, Department of Medicine, Division of General Internal Medicine, University of California, San Francisco.
Sadia Ali, Section of General Internal Medicine, San Francisco Veterans’ Affairs Medical Center, San Francisco.
Mary A. Whooley, Department of Medicine, Division of General Internal Medicine, University of California, San Francisco and Section of General Internal Medicine, San Francisco Veterans’ Affairs Medical Center, San Francisco.
References
- Aljasem L, Peyrot M, Wissow L, Rubin R. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educator. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- Arnold R, Ranchor AV, DeJongste MJ, Koeter GH, Ten Hacken NH, Aalbers R, et al. The relationship between self-efficacy and self-reported physical functioning in chronic obstructive pulmonary disease and chronic heart failure. Behavioral Medicine. 2005;31:107–115. doi: 10.3200/BMED.31.3.107-115. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freedman and Co; 1997. [Google Scholar]
- Berkhuysen MA, Nieuwland W, Buunk BP, Sanderman R, Rispens P. Change in self-efficacy during cardiac rehabilitation and the role of perceived overprotectiveness. Patient Education and Counseling. 1999;38:21–32. doi: 10.1016/s0738-3991(98)00115-3. [DOI] [PubMed] [Google Scholar]
- Bernal H, Woolley S, Schenaul J, Dickinson J. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educator. 2000;26:673–680. doi: 10.1177/014572170002600415. [DOI] [PubMed] [Google Scholar]
- Bibbins-Domingo K, Gupta R, Na B, Wu AH, Schiller NB, Whooley MA. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. Journal of the American Medical Association. 2007;297:169–176. doi: 10.1001/jama.297.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction-summary article: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina) Journal of the American College of Cardiology. 2002;40:1366–1374. doi: 10.1016/s0735-1097(02)02336-7. [DOI] [PubMed] [Google Scholar]
- Carlson JJ, Norman GJ, Feltz DL, Franklin BA, Johnson JA, Locke SK. Self-efficacy, psychosocial factors, and exercise behavior in traditional versus modified cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2001;21:363–373. doi: 10.1097/00008483-200111000-00004. [DOI] [PubMed] [Google Scholar]
- Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Education and Behavior. 1999;26:72–89. doi: 10.1177/109019819902600107. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cossette S, Frasure-Smith N, Lesperance F. Clinical implications of a reduction in psychological distress on cardiac prognosis in patients participating in a psychosocial intervention program. Psychosomatic Medicine. 2001;63:257–266. doi: 10.1097/00006842-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Curtin RB, Walters BA, Schatell D, Pennell P, Wise M, Klicko K. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Advances in Chronic Kidney Disease. 2008;15:191–205. doi: 10.1053/j.ackd.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Taylor CB, Reese LB, DeBusk RF. Effects of early postmyocardial infarction exercise testing on self-perception and subsequent physical activity. American Journal of Cardiology. 1983;51:1076–1080. doi: 10.1016/0002-9149(83)90348-x. [DOI] [PubMed] [Google Scholar]
- Foster C, Oldridge NB, Dion W, Forsyth G, Grevenow P, Hansen M, et al. Time course of recovery during cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 1995;15:209–215. doi: 10.1097/00008483-199505000-00007. [DOI] [PubMed] [Google Scholar]
- Gardner JK, McConnell TR, Klinger TA, Herman CP, Hauck CA, Laubach CA., Jr Quality of life and self-efficacy: Gender and diagnoses considerations for management during cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2003;23:299–306. doi: 10.1097/00008483-200307000-00007. [DOI] [PubMed] [Google Scholar]
- Golden-Kreutz DM, Andersen BL. Depressive symptoms after breast cancer surgery: Relationships with global, cancer-related, and life event stress. Psychooncology. 2004;13:211–220. doi: 10.1002/pon.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden G. The relationship of self-efficacy appraisals to subsequent health related outcomes: A meta-analysis. Social Work Health Care. 1991;16:53–93. doi: 10.1300/j010v16n01_05. [DOI] [PubMed] [Google Scholar]
- Howie-Esquivel J, Dracup K. Effect of gender, ethnicity, pulmonary disease, and symptom stability on rehospitalization in patients with heart failure. American Journal of Cardiology. 2007;100:1139–1144. doi: 10.1016/j.amjcard.2007.04.061. [DOI] [PubMed] [Google Scholar]
- Izawa KP, Watanabe S, Omiya K, Hirano Y, Oka K, Osada N, et al. Effect of the self-monitoring approach on exercise maintenance during cardiac rehabilitation: A randomized, controlled trial. American Journal of Physical Medicine and Rehabilitation. 2005;84:313–321. doi: 10.1097/01.phm.0000156901.95289.09. [DOI] [PubMed] [Google Scholar]
- Jiang W, Kuchibhatla M, Clary GL, Cuffe MS, Christopher EJ, Alexander JD, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. American Heart Journal. 2007;154:102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- Kavanagh D, Gooley S, Wilson P. Prediction of adherence and control in diabetes. Journal of Behavioral Medicine. 1993;16:509–523. doi: 10.1007/BF00844820. [DOI] [PubMed] [Google Scholar]
- Lorig K, Holman H. Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter P, Stewart A, Sobel D, Brown B, Jr, Bandura A, et al. Chronic Disease Self-Management Program: 2-year health status and health utilization outcomes. Medical Care. 2001;39:1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Maddigan S, Majumdar S, Guirguis L, Lewanczuk R, Lee T, Toth E, et al. Improvements in patient-reported outcomes associated with an intervention to enhance quality of care for rural patients with type 2 diabetes. Diabetes Care. 2004;27:1306–1312. doi: 10.2337/diacare.27.6.1306. [DOI] [PubMed] [Google Scholar]
- McCaul K, Glasgow R, Schafer L. Diabetes Regimen Behaviors: Predicting Adherence. Medical Care. 1987;25:868–881. [PubMed] [Google Scholar]
- McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study) American Journal of Cardiology. 2005;96:1076–1081. doi: 10.1016/j.amjcard.2005.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, et al. Pharmacist intervention to improve medication adherence in heart failure: A randomized trial. Annals of Internal Medicine. 2007;146:714–725. doi: 10.7326/0003-4819-146-10-200705150-00005. [DOI] [PubMed] [Google Scholar]
- Oka RK, DeMarco T, Haskell WL. Effect of treadmill testing and exercise training on self-efficacy in patients with heart failure. European Journal Of Cardiovascular Nursing. 2005;4:215–219. doi: 10.1016/j.ejcnurse.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: The Heart and Soul Study. Journal of the American Medical Association. 2003;290:215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruo B, Rumsfeld JS, Pipkin S, Whooley MA. Relation between depressive symptoms and treadmill exercise capacity in the Heart and Soul Study. American Journal of Cardiology. 2004;94:96–99. doi: 10.1016/j.amjcard.2004.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salamah M, Wahl S, Abriam-Yago K. Life Situations Of Elderly People With Heart Disease: The Impact Of Self-Efficacy On Self-Care. The Internet Journal of Advanced Nursing Practice. 2003:5. [Google Scholar]
- Sarkar U, Ali S, Whooley MA. Self-efficacy and health status in patients with coronary heart disease: Findings from the heart and soul study. Psychosomatic Medicine. 2007;69:306–312. doi: 10.1097/PSY.0b013e3180514d57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- Sherwood A, Blumenthal JA, Trivedi R, Johnson KS, O’Connor CM, Adams KF, Jr, et al. Relationship of depression to death or hospitalization in patients with heart failure. Archives of Internal Medicine. 2007;167:367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- Shyu YI, Tang WR, Tsai WC, Liang J, Chen MC. Emotional support levels can predict physical functioning and health related quality of life among elderly Taiwanese with hip fractures. Osteoporosis International. 2005;17(4):501–506. doi: 10.1007/s00198-005-0020-y. [DOI] [PubMed] [Google Scholar]
- Spertus JA, McDonell M, Woodman CL, Fihn SD. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. American Heart Journal. 2000;140:105–110. doi: 10.1067/mhj.2000.106600. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Subramanian U, Hopp F, Mitchinson A, Lowery J. Impact of provider self-management education, patient self-efficacy, and health status on patient adherence in heart failure in a Veterans Administration population. Congest Heart Fail. 2008;14:6–11. doi: 10.1111/j.1751-7133.2008.07174.x. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, LaCroix AZ, Russo J, Katon WJ. Self-efficacy and self-reported functional status in coronary heart disease: A six-month prospective study. Psychosomatic Medicine. 1998;60:473–478. doi: 10.1097/00006842-199807000-00014. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, LaCroix AZ, Spertus JA, Hecht J. Five-year prospective study of the effects of anxiety and depression in patients with coronary artery disease. American Journal of Cardiology. 2000;86:1135–1138. A1136–A1139. doi: 10.1016/s0002-9149(00)01174-7. [DOI] [PubMed] [Google Scholar]
- Tu W, Morris AB, Li J, Wu J, Young J, Brater DC, et al. Association between adherence measurements of metoprolol and health care utilization in older patients with heart failure. Clinical Pharmacology and Therapeutics. 2005;77:189–201. doi: 10.1016/j.clpt.2004.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease [published erratum appears in JAMA 1992 Nov 18;268(19):2652] Journal of the American Medical Association. 1992;267:520–524. [PubMed] [Google Scholar]
- Wolf MS, Davis TC, Osborn CY, Skripkauskas S, Bennett CL, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Education and Counseling. 2007;65:253–260. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]