Abstract
Arboviruses are capable of causing encephalitis in animals and human population when transmitted by the vector or potentially via infectious aerosol. Recent re-emergence of Venezuelan equine encephalitis virus (VEEV) in South America emphasizes the importance of this pathogen to public health and veterinary medicine. Despite its importance no antivirals or vaccines against VEEV are currently available in the USA. Here we review some of the older and newer approaches aimed at generating a safe and immunogenic vaccine as well as most recent data about the mechanistic of protection in animal models of infection.
Venezuelan equine encephalitis virus and its replication
Venezuelan equine encephalitis virus (VEEV, Alphavirus in the Togaviridae family) is an enveloped virus with a non-segmented, positive-sense RNA genome of approximately 11.4 kb (Fig. 1). The 5' two-thirds of the genome encodes four nonstructural proteins (nsP1 to nsP4) that form an enzyme complex required for viral replication [1–3]. The full-length RNA then serves as a template for the synthesis of positive-sense genomic RNA and for transcription of a subgenomic 26S RNA [1]. The approximately 4-kb-long, subgenomic RNA corresponds to the 3’ one-third of the viral genome and is translated into a structural polyprotein that is proteolytically cleaved into the capsid and the envelope glycoproteins E2 and E1 [4].
Figure 1.
Genomic organization of Venezuelan equine encephalitis virus.
Epidemiology of encephalitic alphaviruses
Most of the encephalitic viruses in the Family Togaviridae, genus Alphavirus are zoonotic pathogens that are transmitted via hematophagous arthropods. These pathogens have a widespread distribution in North, Central and South America (reviewed in [5]). Some of them are highly infectious via the aerosol route, thus have been responsible for numerous laboratory accidents (>150 documented cases without an associated perforating injury) and/or have been developed as a biological weapon in the U.S and in the former Soviet Union. First virus isolations were reported in the 1930s from diseased horses in California, in Virginia and New Jersey, and from an infected child in Caracas, Venezuela, and were subsequently named based on their region of isolation as Western equine encephalomyelitis virus (WEEV), Eastern equine encephalomyelitis virus (EEEV) and Venezuelan equine encephalomyelitis virus (VEEV), respectively.
Disease in humans
VEEV infection has an incubation period of 2–10 days, which results typically in non-specific flu-like symptoms. Severe encephalitis is a less common outcome of VEEV infection in comparison to EEEV and WEEV infection, although VEEV-associated encephalitis is a more common outcome in children. Neurological disease, including disorientation, ataxia, mental depression, and convulsions can be detected in up to 14% of infected individuals, especially children, although the human case-fatality rate is low (<1%).
Mouse model for VEEV infection
The murine model for VEEV-induced disease is established and typically utilizes subcutaneous inoculation [6–9]. Previous studies have demonstrated that the murine model is characterized by biphasic disease, which starts with the productive infection of lymphoid tissue and culminates in the destruction of the CNS by viral replication and a “toxic” neuroinflammatory response that is uniformly lethal [10–16]. By the time the acute encephalitis has developed in an infected mouse, the virus is usually absent from the peripheral organs and blood [10–16]. The mouse model is useful for testing of vaccine and drug efficacy.
Humoral immunity
Protection from peripheral inoculation or natural alphavirus infection depends mostly on the production of neutralizing antibodies [17, 18]. While virus neutralizing antibody is important for the protection against natural (peripheral) challenge mediated by mosquito-borne transmission, more recent studies demonstrate that even relatively high serum titers of polyclonal neutralizing antibody achieved via passive transfer (not achievable with any vaccination known to authors) do not protect mice from intranasal (i.n.) challenge in the mouse model of infection [19, 20]. These data supports the conclusion that virus neutralizing antibody plays a significant role in preventing the penetration of the CNS after peripheral challenge with VEEV, while it is relatively ineffective in controlling the rapid onset of CNS disease following i.n. infection [20, 21].
Alpha Beta (αβ)T cell response
The αβ T cells represent the major proportion of T cells that respond to various pathogens and are subdivided into CD4+ helper and CD8+ cytotoxic cells. These “conventional” T cells have been well characterized functionally. Prior studies in mice vaccinated with TC83 suggest that Th1-type responses predominate [22]. However, in mice vaccinated parenterally with TC83, cytotoxic T cell activity could not be detected in the spleen or draining lymph node [23]. It was previously demonstrated that host factors contribute to mortality in neurovirulent Sindbis virus (NSV)-induced encephalitis model in mice [24]. Animals deficient in αβ-, but not γδ-T cells had lower mortality rates when infected with neuroadapted Sindbis virus (NSV), indicating their different contribution to the outcome of the brain infection [25]. CD4+ T cell effector functions in encephalitis may include a combination of Th1, Th2 and regulatory T cells (CD25+, forkhead family transcription factor, Foxp3+) activities [26–28]. In other models of acute encephalitis, such as experimental autoimmune encephalomyelitis (EAE) as well as in more chronic encephalitis described for toxoplasmic encephalitis (TE), the myelin basic protein specific CD4+ T cells are crucial for the development of the encephalitis. CD8+ T cells contribute to both pathogenesis of and recovery from encephalitic flavivirus infections [29, 30] but their role in VEEV-induced encephalitis, immunopathology and protection is less clear. In general, it has been hypothesized that cell-mediated cytotoxicity is less critical for control of cytopathic viruses such as VEEV in comparison to noncytopathic viruses [31, 32]. This can be extended to the CNS where elimination of virus from neurons is thought to be via non-lytic mechanisms due to the poor regenerative capacity of this cell type [24, 32–37].
Gamma delta (γδ) T cell response
Recent studies suggest an important role for another well studied T cell subpopulation, γδ T cells, in disease development and lethal outcomes of VEEV infection [19]. Specifically, qualitative and quantitative changes in the inflammatory cellular infiltrates in vaccinated and challenged mice suggest a regulatory role in the secondary response to virus. However, direct evaluation of their role in pathology vs. protection is limited by the lack of feasible methods for isolating sufficient quantities for adoptive transfer. This cell population constitutes a relatively minor subset of T cells in lymphoid tissues despite being well represented in other sites including the peripheral blood and in the epithelial and mucosal layers in the respiratory and gastrointestinal (GI) tract [38, 39]. The role of γδ T cells in the CNS has not been functionally well-defined, despite studies showing their potential importance in diminishing the neurovirulence of West Nile Virus (WNV) [40] and modulating the progression of neurocysticercosis in TCR-δ chain-deficient mice [41]. In the case of viral infections, γδ T cells can substitute for αβ T cells in a virus model of demyelination [42]. In the neurovirulent Sindbis virus model, animals deficient in αβ, but not γδ T cells have lower mortality rates, indicating the differential contribution of these cell types to the outcome of the brain infection [25].
Live-attenuated VEE vaccines
Following upon the success of the 17D yellow fever vaccine by Theiler [43], VEEV was attenuated by 83 serial passages in guinea pig heart cells to produce the TC-83 strain [44]. TC-83 was first tested extensively in equids during the 1971 Texas VEE epizootic/epidemic, where it may have contributed to limiting the spread northward. Although the vaccine produces viremia, fever and leucopenia in horses, robust neutralizing antibodies are generated as well as protection from VEEV challenge [45]. The TC-83 strain continues to be manufactured in Mexico and Colombia for use as a live vaccine in equids, but is currently only marketed in inactivated form in the U.S.
The history of serious laboratory infections by VEEV as well as its development as a biological weapon in the U.S. and former USSR prompted the use of TC-83 in humans as an investigational new drug (IND) product. TC-83 produces seroconversion in about 80% of humans (neutralizing antibody titers ≥20) but mild to moderate flu-like symptoms in about 205 of volunteers. Persons who fail to seroconvert in the U.S. Army Special Immunizations program are given boosters of C-84 (inactivated TC-83) [46]. Unlike TC-83, C-84 produces only occasional, mild, reactions. Some rodent studies indicate that TC-83 protects mice better against aerosol challenge than C-84 [47], although neither completely protects nonhuman primates against aerosol exposure [48].
The reactogenicity and limited immunogenicity of TC-83 may be the result of only 2 attenuating mutations among the 12 mutations that accompanied in vitro passage of the Trinidad donkey strain [49]. Presumably, these mutations are subject to reversion in vaccinees, which also presents a risk of epizootic amplification. To produce a more stably attenuated VEEV vaccine candidate, the Trinidad donkey genome was cloned in cDNA form and attenuation was achieved by inserting either point mutations or a PE2 cleavage-signal mutation combined with an E1 gene resuscitating mutation. The latter strain, called V3526, is safe and immunogenic for mice and nonhuman primates, and appears superior to TC-83 in rodents [50–52]. V3526 also appears to have a lower risk for environmental transmission and distribution [53, 54]. Although V3526 elicits neutralizing antibodies in nonhuman primates only against homologous IAB VEEV strains, it protects against aerosol challenges with both IAB and IE strains [55]. Furthermore, it is not neurovirulent when administered intracranially to juvenile rhesus macaques [56].
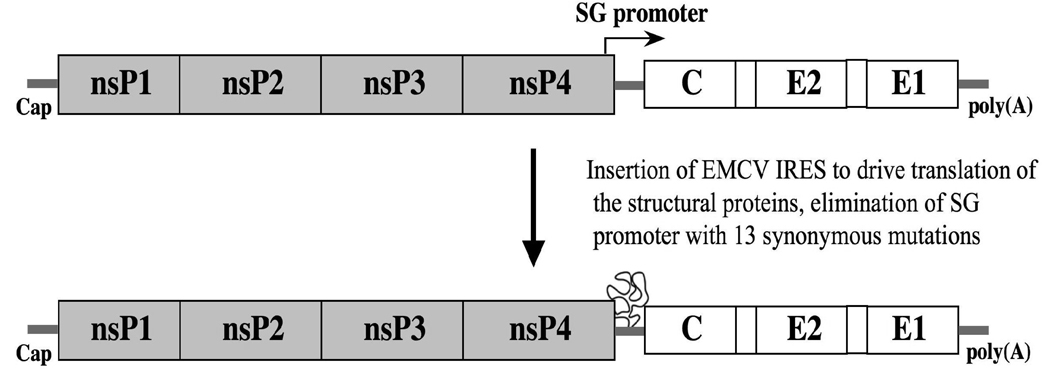
Because TC-83 can be transmitted by mosquito vectors [57] and was isolated in mosquitoes collected in Louisiana during the 1971 VEE epizootic/epidemic [57], efforts were made to improve it safety by preventing its ability to infect insects. Translation of the viral structural proteins and, ultimately, viral replication was made dependent on an internal ribosome entry site of encephalomyelocarditis virus, and the subgenomic promoter was inactivated with 13 synonymous mutations (Fig. 2)[58]. This recombinant virus further attenuated TC-83, but was completely unable to infect mosquito cells or mosquitoes in vivo. Thus, the manipulation of structural protein gene expression may be useful not only as a safety feature of live vaccine strains but also as an attenuation mechanism.
Figure 2.
Mutant strain of TC-83 with the subgenomic promoter inactivated and the translation of the structural protein genes placed under the contol of an encephalomyelocarditis virus internal ribosome entry site (IRES). From reference [58].
Inactivated VEE vaccines
Due to the economic devastation caused by VEE epizootics in regions of Latin American that relied on equids for agriculture and transportation, vaccines were first produced soon after VEEV was isolated in 1938 [59, 60]. Formalin-inactivated preparations were initially made from mouse brain and other animal tissues following infection with wild-type, subtype IAB strains isolated during epizootics [61]. These vaccines were probably efficacious in most animals, but the equid-amplification potential of the parent viruses presented a high risk if residual live virus remained in vaccine lots. Sequencing studies showing conservation among all IAB strains isolated from 1938–1973 [62, 63], as well as the isolation of live virus from at least one human vaccine preparation [64], indicated that this “escape” of VEEV from incompletely inactivated vaccines probably occurred on several occasions. The disappearance of subtype IAB VEEV since 1973, when inactivated vaccines were replaced by the live-attenuated TC-83 strain, supports this conclusion.
Currently, commercial equine vaccines marketed in the U.S. consist of inactivated TC-83, often combined with the other principal alphaviral encephalitides, eastern and western equine encephalitis viruses.
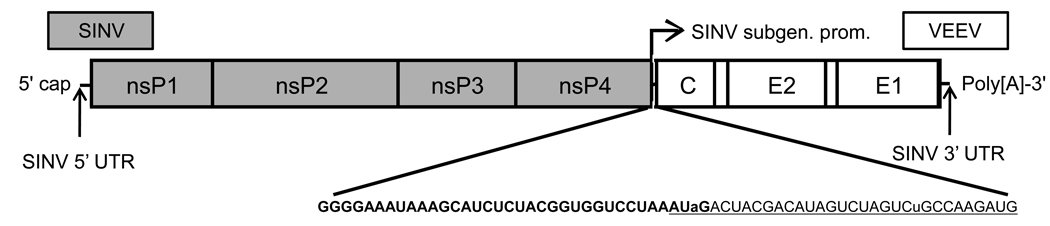
Sindbis virus-based chimeric vaccine approach
Recombinant live-attenuated vaccines and, in particular, an alphavirus-based approach, represent a viable approach to the production of safe, immunogenic and efficacious vaccines against the encephalitis alphaviruses [19, 21, 65–67]. By utilizing as a vector the genome of Sindbis virus (SINV), a relatively nonpathogenic alphavirus in humans, chimeric SIN/VEE virus(es) can be designed to express all of the structural proteins of the virulent alphavirus. These constructs contain the cis-acting RNA elements and non-structural protein genes of the SINV genome, which are required for replication and transcription of the subgenomic RNA, e.g., 5' untranslated region (UTR), 3' UTR, and the subgenomic promoter (Fig. 3).
Figure 3.
Genetic organization of chimeric Sindbis/Venezuelan equine encephalitis virus vaccine candidates described in references [21, 66]. The cis-acting sequences were derived from Sindbis virus strain Toto1101 or AR339, along with the nonstructural protein genes, while the structural protein genes were derived from Venezuelan equine encephalitis virus strain TC-83 or ZPC738. Bold letters represent SINV-specific sequence, and underlined letters represent VEEV-specific sequence. Lowercase letters indicate mutations introduced into the VEEV sequence to make the junction more SINV-like and to preserve the putative secondary structure of the 5’ UTR in the VEEV subgenomic RNA.
The safety of several chimeric SIN/VEE virus vaccine candidates have been tested in mice of different genetic background and age, and via several routes of infection. All were evaluated in parallel with the investigational vaccine, TC83, which is currently used for vaccination of research and military personnel, but which is documented to have significant adverse effects. SIN83 chimeric virus at doses in range of 2 × 104 to 2 × 106 PFUdid not cause any detectable clinical disease in either adult or weanling mice when monitored up to 21 days after either s.c. or i.c. inoculation [66]. When tested at a higher s.c. dose of 5 × 106 PFU, none of the chimeric SIN/VEE virus, e.g., SIN83, SIN/ZPC, or SIN/TRD resulted in morbidity or mortality [21]. This is in contrast to mortality of 10% and 100% for TC83, which were both fatal to newborn outbred (NIH Swiss) mice at comparable doses of 2 × 105 and 5 × 106, respectively [66, 67]. Another VEEV vaccine candidate undergoing preclinical testing, V3526, was 100% fatal to these mice at the lower dose of 1 × 105 [67]. Additional safety studies were performed in inbred mice with selective immunodeficiencies in the T cell compartments (αβ T cell receptor (TCR)-deficient or γδ TCR-deficient mice), in the B cell compartment (µMT-deficient mice), or in their ability to respond to the cytokine interferon gamma (IFN-γR-deficient mice). Vaccines were delivered via two s.c. inoculations (5 × 105 PFU/animal) and survival evaluated for 14 days following the booster dose [19].All alpha-beta (αβ) TCR- and γδ TCR- deficient, and µMT-deficient mice survived vaccination and none of these animals showed any signs of disease.
The chimeric SIN/VEE vaccines were highly efficacious in NIH Swiss as well as in C57BL/6 mice challenged with ZPC738, as described above, irrespective of the challenge method (i.c., i.n., or s.c.) [19, 21, 66], and in immunocompetent C57BL/6 (wild type, WT) mice and their immunodeficient counterparts. Vaccinated γδ TCR-deficient mice and WT mice were protected, with survival of 98%, which was significantly greater (Fisher’s exact test; p = 0.0001) than for vaccinated WT mice (93%). Survival of IFN-γR KO mice was reduced in comparison to vaccinated WT and γδ TCR KO mice, although the survival time was also extended in comparison to mock-vaccinated and vaccinated αβ TCR-deficient mice. The majority of µMT-deficient mice were not protected from challenge (13% survival) and this was not significantly different from mock vaccinated WT mice (Fisher’s exact test; p = 0.2748) [19].
Recent results strongly suggest that VEEV-specific CD4+ T cells are the primary cell population responsible for protection from lethal encephalitis elicited by vaccination with this chimeric live-attenuated vaccine [20]. A minor proportion of µMT mice survive lethal challenge infection following vaccination suggesting that antibody is not absolutely required for protection from VEEV-mediated lethal encephalitis. Passive transfer of hyperimmune serum reactive with VEEV into immunocompetent mice results in a statistically significant increase in survival time from a median of 8 days for the mice treated with hyperimmune serum in comparison to 5.5 days for the placebo (PBS-treated) controls. However, all hyperimmune serum-treated animals succumbed to infection within 12 days (0% survival, 0/8 mice), indicating that antibody alone is not sufficient for protection from infection.
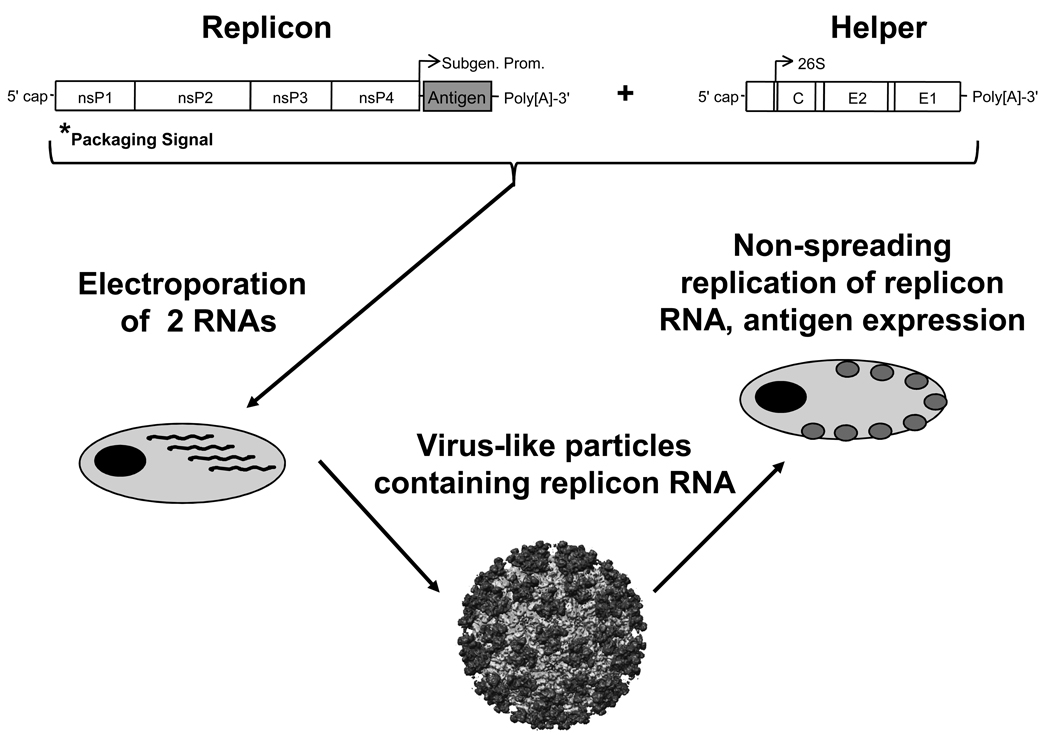
Alphavirus replicons
Because only the nonstructural proteins and cis-acting RNA sequences are required for alphavirus genome replication, the structural protein genes can be replaced and foreign antigens expressed at high levels [68, 69]. These replicon genomes can be packaged into virus-like particles by capsid and envelope proteins provided in trans from a second genetic construct (Fig. 4). To reduce the probability of recombination between replicon and “helper” RNAs, two separate helpers can be used to encode the structural proteins [70]. Packaging cell lines that constitutively express the structural proteins can also be used to produce replicon particles [71]. Even in packaged form, the replicon genomes cannot produce structural proteins, so they express their foreign genes during only one round of replication and cannot spread to other cells. This immunogenicity advantage of antigenic gene replication with the safety advantage of limited spread has resulted in the use of alphavirus replicon systems to express many immunogens from other viruses or proteins [72, 73]. However, these replicons can also be used to immunize against homologous or heterologous alphaviruses without the safety concerns of a live replicating virus. Furthermore, alphavirus replicon particles appear to have intrinsic systemic and mucosal adjuvant activity due to their RNA replication activity [74].
Figure 4.
Genetic organization of alphavirus replicons and helpers used to package them into virus-like particles. In some cases, the helper construct is divided into the capsid and E2/E1 protein to minimize the change of RNA recombination that can produce complete genomes and live virus.
DNA vaccines
Recent studies employed directed molecular evolution to generate cross-reactivity Venezuelan equine encephalitis virus (VEEV) envelope glycoproteins. Dupuy et al. [75] generated libraries of chimeric genes expressing variant envelope proteins and used selected variants to vaccinate mice. Their results indicate that it is possible to improve the immunogenicity and protective efficacy of alphavirus DNA vaccines using directed molecular evolution. Previously, others have shown that vaccinia virus recombinants as well as adenovirus-based approach can be successfully utilized to generate protective immunity against VEEV in the mouse model [17, 76]
Future directions
Development of a vaccine that would induce rapid protection in people and animals remains an important issue. New generation of safe chimeric viruses that are unable to infect mosquitoes is currently in development and preclinical studies are ongoing. This would be a major step toward production of live-attenuated vaccine that is safer for the environment and would minimize the risk for vaccine-born outbreaks as reported in 1970”s for TC83 vaccine. However, additional efficacy trials in non-human primates are required to confirm the protective response for some of the candidates and for initiation of potential clinical trials. Some of the recent experimental data indicates that the immune response against VEEV needed to control the brain infection may differ from the one required to control the peripheral infection. Therefore, vaccines that protect against the natural infection may differ in the future from those that are supposed to protect against high-dose air-borne challenge and may be more attenuated. Our group is also trying to use the most recent pathogenesis data to design a therapeutic vaccine that would reverse already established encephalitis and help clear the virus from the brain.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Strauss EG, Strauss JH. Structure and replication of the alphavirus genome. In: Schlesinger S, Schlesinger M, editors. The Togaviruses and Flaviviruses. New York: Plenum Press; 1986. pp. 35–90. [Google Scholar]
- 2.Strauss JH, Calisher CH, Dalgarno L, Dalrymple JM, Frey TK, Pettersson RF, et al. Togaviridae. In: Murphy FA, Fauquet CM, Bishop DHL, Ghabrial SA, Jarvis AW, Martelli GP, et al., editors. Virus Taxonomy Sixth Report of the International Committee on Taxonomy of Viruses. New York: Springer-Verlag; 1995. pp. 428–433. [Google Scholar]
- 3.Strauss JH, Strauss EG. The alphaviruses: gene expression, replication, and evolution. Microbiol Rev. 1994;58(3):491–562. doi: 10.1128/mr.58.3.491-562.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rice CM, Strauss JH. Nucleotide sequence of the 26S mRNA of Sindbis virus and deduced sequence of the encoded virus structural proteins. Proc Natl Acad Sci U S A. 1981;78(4):2062–2066. doi: 10.1073/pnas.78.4.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paessler S, Pfeffer M. Togaviruses causing encephalitis (Togaviridae) In: Mahy BWJ, Van Regenmortel MHV, editors. Encyclopedia of Virology. 3rd ed. Oxford: Elsevier; 2008. pp. 76–82. [Google Scholar]
- 6.Davis NL, Grieder FB, Smith JF, Greenwald GF, Valenski ML, Sellon DC, et al. A molecular genetic approach to the study of Venezuelan equine encephalitis virus pathogenesis. Arch Virol Suppl. 1994;9:99–109. doi: 10.1007/978-3-7091-9326-6_11. [DOI] [PubMed] [Google Scholar]
- 7.Kundin WD. Pathogenesis of Venezuelan equine encephalomyelitis virus. II. Infection in young adult mice. J Immunol. 1966;96(1):49–58. [PubMed] [Google Scholar]
- 8.Jackson AC, SenGupta SK, Smith JF. Pathogenesis of Venezuelan equine encephalitis virus infection in mice and hamsters. Vet Pathol. 1991;28(5):410–418. doi: 10.1177/030098589102800509. [DOI] [PubMed] [Google Scholar]
- 9.Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, et al. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995;212(1):102–110. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- 10.Schoneboom BA, Catlin KMK, Marty AM, Grieder FB. Inflammation is a component of neurodegeneration in response to Venezuelan equine encephalitis virus infection in mice. J Neuroimmunology. 2000;(109):132–146. doi: 10.1016/s0165-5728(00)00290-3. [DOI] [PubMed] [Google Scholar]
- 11.Schoneboom BA, Fultz MJ, Miller TH, McKinney LC, Grieder FB. Astrocytes as targets for Venezuelan equine encephalitis virus infection. J Neurovirol. 1999;5(4):342–354. doi: 10.3109/13550289909029475. [DOI] [PubMed] [Google Scholar]
- 12.Grieder FB, Davis BK, Zhou XD, Chen SJ, Finkelman FD, Gause WC. Kinetics of cytokine expression and regulation of host protection following infection with molecularly cloned Venezuelan equine encephalitis virus. Virology. 1997 Jul 7;233(2):302–312. doi: 10.1006/viro.1997.8617. [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Tamayo J, Carreno G, Esparza J. Central nervous system alterations as sequelae of Venezuelan equine encephalitis virus infection in rat. J Pathol. 1979;128(128):87–91. doi: 10.1002/path.1711280206. [DOI] [PubMed] [Google Scholar]
- 14.Gorelkin L. Venezuelan equine encephalomyelitis in an adult animal host.An electron microscopic study. Am J Pathol. 1973;73(2):425–442. [PMC free article] [PubMed] [Google Scholar]
- 15.Grieder FB, Davis NL, Aronson JF, Charles PC, Sellon DC, Suzuki K, et al. Specific restrictions in the progression of Venezuelan equine encephalitis virus-induced disease resulting from single amino acid changes in the glycoproteins. Virology. 1995;206(2):994–1006. doi: 10.1006/viro.1995.1022. [DOI] [PubMed] [Google Scholar]
- 16.Ryzhikov AB, Ryabchikova EI, Sergeev AN, Tkacheva NV. Spread of Venezuelan equine encephalitis virus in mice olfactory tract. Arch Virol. 1995;140(12):2243–2254. doi: 10.1007/BF01323243. [DOI] [PubMed] [Google Scholar]
- 17.Phillpotts RJ, O'Brien L, Appleton RE, Carr S, Bennett A. Intranasal immunisation with defective adenovirus serotype 5 expressing the Venezuelan equine encephalitis virus E2 glycoprotein protects against airborne challenge with virulent virus. Vaccine. 2005 Feb 18;23(13):1615–1623. doi: 10.1016/j.vaccine.2004.06.056. [DOI] [PubMed] [Google Scholar]
- 18.Phillpotts RJ, Jones LD, Howard SC. Monoclonal antibody protects mice against infection and disease when given either before or up to 24 h after airborne challenge with virulent Venezuelan equine encephalitis virus. Vaccine. 2002 Feb 22 22;20(11–12):1497–1504. doi: 10.1016/s0264-410x(01)00505-9. [DOI] [PubMed] [Google Scholar]
- 19.Paessler S, Yun NE, Judy BM, Dziuba N, Zacks MA, Grund AH, et al. Alpha-beta T cells provide protection against lethal encephalitis in the murine model of VEEV infection. Virology. 2007 Jul 2;367(2):307–323. doi: 10.1016/j.virol.2007.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yun NE, Peng BH, Bertke AS, Borisevich V, Smith JK, Smith JN, et al. CD4+ T cells provide protection against acute lethal encephalitis caused by Venezuelan equine encephalitis virus. Vaccine. 2009 Jun 19;27(30):4064–4073. doi: 10.1016/j.vaccine.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, et al. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J Virol. 2006 Mar;80(6):2784–2796. doi: 10.1128/JVI.80.6.2784-2796.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bennett AM, Lescott T, Phillpotts RJ. Improved protection against Venezuelan equine encephalitis by genetic engineering of a recombinant vaccinia virus. Viral Immunol. 1998;11(3):109–117. doi: 10.1089/vim.1998.11.109. [DOI] [PubMed] [Google Scholar]
- 23.Jones LD, Bennett AM, Moss SR, Gould EA, Phillpotts RJ. Cytotoxic T-cell activity is not detectable in Venezuelan equine encephalitis virus-infected mice. Virus Res. 2003 Feb;91(2):255–259. doi: 10.1016/s0168-1702(02)00275-7. [DOI] [PubMed] [Google Scholar]
- 24.Thach DC, Kimura T, Griffin DE. Differences between C57BL/6 and BALB/cBy mice in mortality and virus replication after intranasal infection with neuroadapted Sindbis virus. J Virol. 2000;74(13):6156–6161. doi: 10.1128/jvi.74.13.6156-6161.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rowell JF, Griffin DE. Contribution of T cells to mortality in neurovirulent Sindbis virus encephalomyelitis. J Neuroimmunol. 2002 Jun;127(1–2):106–114. doi: 10.1016/s0165-5728(02)00108-x. [DOI] [PubMed] [Google Scholar]
- 26.Ziegler SF. FOXP3: Of Mice and Men. Annu Rev Immunol. 2005 Dec 1; doi: 10.1146/annurev.immunol.24.021605.090547. [DOI] [PubMed] [Google Scholar]
- 27.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003 Feb 14;299(5609):1057–1061. doi: 10.1126/science.1079490. [DOI] [PubMed] [Google Scholar]
- 28.Loser K, Hansen W, Apelt J, Balkow S, Buer J, Beissert S. In vitro-generated regulatory T cells induced by Foxp3-retrovirus infection control murine contact allergy and systemic autoimmunity. Gene Ther. 2005 Sep;12(17):1294–1304. doi: 10.1038/sj.gt.3302567. [DOI] [PubMed] [Google Scholar]
- 29.King NJ, Getts DR, Getts MT, Rana S, Shrestha B, Kesson AM. Immunopathology of flavivirus infections. Immunol Cell Biol. 2007 Jan;85(1):33–42. doi: 10.1038/sj.icb.7100012. [DOI] [PubMed] [Google Scholar]
- 30.Solomon T, Winter PM. Neurovirulence and host factors in flavivirus encephalitis--evidence from clinical epidemiology. Arch Virol Suppl. 2004;(18):161–170. doi: 10.1007/978-3-7091-0572-6_14. [DOI] [PubMed] [Google Scholar]
- 31.Kagi D, Hengartner H. Different roles for cytotoxic T cells in the control of infections with cytopathic versus noncytopathic viruses. Curr Opin Immunol. 1996 Aug;8(4):472–477. doi: 10.1016/s0952-7915(96)80033-1. [DOI] [PubMed] [Google Scholar]
- 32.Griffin DE. Immune responses to RNA-virus infections of the CNS. Nat Rev Immunol. 2003 Jun;3(6):493–502. doi: 10.1038/nri1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma J, Urba WJ, Si L, Wang Y, Fox BA, Hu HM. Anti-tumor T cell response and protective immunity in mice that received sublethal irradiation and immune reconstitution. Eur J Immunol. 2003 Aug;33(8):2123–2132. doi: 10.1002/eji.200324034. [DOI] [PubMed] [Google Scholar]
- 34.Marks L, Levy RB. The cytotoxic potential of regulatory T cells: what has been learned from gene knockout model systems? Transplantation. 2004 Jan 15;77(1 Suppl):S19–S22. doi: 10.1097/01.TP.0000106473.46037.83. [DOI] [PubMed] [Google Scholar]
- 35.Trapani JA. Dual mechanisms of apoptosis induction by cytotoxic lymphocytes. Int Rev Cytol. 1998;182:111–192. doi: 10.1016/s0074-7696(08)62169-5. [DOI] [PubMed] [Google Scholar]
- 36.Shresta S, Pham CT, Thomas DA, Graubert TA, Ley TJ. How do cytotoxic lymphocytes kill their targets? Curr Opin Immunol. 1998 Oct;10(5):581–587. doi: 10.1016/s0952-7915(98)80227-6. [DOI] [PubMed] [Google Scholar]
- 37.Kajino K, Kajino Y, Greene MI. Fas- and perforin-independent mechanism of cytotoxic T lymphocyte. Immunol Res. 1998;17(1–2):89–93. doi: 10.1007/BF02786434. [DOI] [PubMed] [Google Scholar]
- 38.Hayday AC, Roberts S, Ramsburg E. gammadelta cells and the regulation of mucosal immune responses. Am J Respir Crit Care Med. 2000 Oct;162(4 Pt 2):S161–S163. doi: 10.1164/ajrccm.162.supplement_3.15tac4. [DOI] [PubMed] [Google Scholar]
- 39.Hayday AC. [gamma][delta] cells: a right time and a right place for a conserved third way of protection. Annu Rev Immunol. 2000;18:975–1026. doi: 10.1146/annurev.immunol.18.1.975. [DOI] [PubMed] [Google Scholar]
- 40.Wang T, Scully E, Yin Z, Kim JH, Wang S, Yan J, et al. IFN-gamma-producing gamma delta T cells help control murine West Nile virus infection. J Immunol. 2003 Sep 1;171(5):2524–2531. doi: 10.4049/jimmunol.171.5.2524. [DOI] [PubMed] [Google Scholar]
- 41.Cardona AE, Teale JM. Gamma/delta T cell-deficient mice exhibit reduced disease severity and decreased inflammatory response in the brain in murine neurocysticercosis. J Immunol. 2002 Sep 15;169(6):3163–3171. doi: 10.4049/jimmunol.169.6.3163. [DOI] [PubMed] [Google Scholar]
- 42.Dandekar AA, Perlman S. Virus-induced demyelination in nude mice is mediated by gamma delta T cells. Am J Pathol. 2002 Oct;161(4):1255–1263. doi: 10.1016/s0002-9440(10)64402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Theiler M, Smith HH. Use of yellow fever virus modified by in vitro cultivation for human immunization. J Exp Med. 1937;65:787–800. doi: 10.1084/jem.65.6.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berge TO, Banks IS, Tigertt WD. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea pig heart cells. Am J Hyg. 1961;73:209–218. [Google Scholar]
- 45.Walton TE, Alvarez O, Jr, Buckwalter RM, Johnson KM. Experimental infection of horses with an attenuated Venezuelan equine encephalomyelitis vaccine (strain TC-83) Infect Immun. 1972 May;5(5):750–756. doi: 10.1128/iai.5.5.750-756.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996 Mar;14(4):337–343. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- 47.Jahrling PB, Stephenson EH. Protective efficacies of live attenuated and formaldehyde-inactivated Venezuelan equine encephalitis virus vaccines against aerosol challenge in hamsters. J Clin Microbiol. 1984 Mar;19(3):429–431. doi: 10.1128/jcm.19.3.429-431.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pratt WD, Gibbs P, Pitt ML, Schmaljohn AL. Use of telemetry to assess vaccine-induced protection against parenteral and aerosol infections of Venezuelan equine encephalitis virus in non-human primates. Vaccine. 1998;16(9–10):1056–1064. doi: 10.1016/s0264-410x(97)00192-8. [DOI] [PubMed] [Google Scholar]
- 49.Kinney RM, Chang GJ, Tsuchiya KR, Sneider JM, Roehrig JT, Woodward TM, et al. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5'-noncoding region and the E2 envelope glycoprotein. Journal of virology. 1993 Mar;67(3):1269–1277. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pratt WD, Davis NL, Johnston RE, Smith JF. Genetically engineered, live attenuated vaccines for Venezuelan equine encephalitis: testing in animal models. Vaccine. 2003 Sep 8;21(25–26):3854–3862. doi: 10.1016/s0264-410x(03)00328-1. [DOI] [PubMed] [Google Scholar]
- 51.Hart MK, Caswell-Stephan K, Bakken R, Tammariello R, Pratt W, Davis N, et al. Improved mucosal protection against Venezuelan equine encephalitis virus is induced by the molecularly defined, live-attenuated V3526 vaccine candidate. Vaccine. 2000;18(26):3067–3075. doi: 10.1016/s0264-410x(00)00042-6. [DOI] [PubMed] [Google Scholar]
- 52.Ludwig GV, Turell MJ, Vogel P, Kondig JP, Kell WK, Smith JF, et al. Comparative neurovirulence of attenuated and non-attenuated strains of Venezuelan equine encephalitis virus in mice. The American journal of tropical medicine and hygiene. 2001;64(1–2):49–55. doi: 10.4269/ajtmh.2001.64.49. [DOI] [PubMed] [Google Scholar]
- 53.Turell MJ, Ludwig GV, Kondig J, Smith JF. Limited potential for mosquito transmission of genetically engineered, live-attenuated Venezuelan equine encephalitis virus vaccine candidates. The American journal of tropical medicine and hygiene. 1999;60(6):1041–1044. doi: 10.4269/ajtmh.1999.60.1041. [DOI] [PubMed] [Google Scholar]
- 54.Rao V, Hinz ME, Roberts BA, Fine D. Environmental hazard assessment of Venezuelan equine encephalitis virus vaccine candidate strain V3526. Vaccine. 2004 Jun 30;22(20):2667–2673. doi: 10.1016/j.vaccine.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 55.Reed DS, Lind CM, Lackemeyer MG, Sullivan LJ, Pratt WD, Parker MD. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine. 2005 May 2;23(24):3139–3147. doi: 10.1016/j.vaccine.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 56.Fine DL, Roberts BA, Terpening SJ, Mott J, Vasconcelos D, House RV. Neurovirulence evaluation of Venezuelan equine encephalitis (VEE) vaccine candidate V3526 in nonhuman primates. Vaccine. 2008 Jun 25;26(27–28):3497–3506. doi: 10.1016/j.vaccine.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 57.Pedersen CE, Jr, Robinson DM, Cole FE., Jr Isolation of the vaccine strain of Venezuelan equine encephalomyelitis virus from mosquitoes in Louisiana. Am J Epidemiol. 1972 May;95(5):490–496. doi: 10.1093/oxfordjournals.aje.a121416. [DOI] [PubMed] [Google Scholar]
- 58.Volkova E, Frolova E, Darwin JR, Forrester NL, Weaver SC, Frolov I. IRES-dependent replication of Venezuelan equine encephalitis virus makes it highly attenuated and incapable of replicating in mosquito cells. Virology. 2008 Jul 20;377(1):160–169. doi: 10.1016/j.virol.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beck CE, Wyckoff RWG. Venezuelan equine encephalomyelitis. Science. 1938;88(2292):530. doi: 10.1126/science.88.2292.530. [DOI] [PubMed] [Google Scholar]
- 60.Kubes V, Rios FA. The causitive agent of infectious equine encephalomyelitis in Venezuela. Science. 1939;90:20–21. doi: 10.1126/science.90.2323.20. [DOI] [PubMed] [Google Scholar]
- 61.Randall R, Maurer FD, Smadel JE. Immunization of laboratory workers with purified Venezuelan equine encephalomyelitis vaccine. J Immunol. 1949 Nov;63(3):313–318. [PubMed] [Google Scholar]
- 62.Kinney RM, Tsuchiya KR, Sneider JM, Trent DW. Molecular evidence for the origin of the widespread Venezuelan equine encephalitis epizootic of 1969 to 1972. J Gen Virol. 1992;73(Pt 12):3301–3305. doi: 10.1099/0022-1317-73-12-3301. [DOI] [PubMed] [Google Scholar]
- 63.Weaver SC, Pfeffer M, Marriott K, Kang W, Kinney RM. Genetic evidence for the origins of Venezuelan equine encephalitis virus subtype IAB outbreaks. Am J Trop Med Hyg. 1999;60(3):441–448. doi: 10.4269/ajtmh.1999.60.441. [DOI] [PubMed] [Google Scholar]
- 64.Sutton LS, Brooke CC. Venezuelan equine encephalomyelitis due to vaccination in man. J Am Med Assoc. 1954;155(17):1473–1476. doi: 10.1001/jama.1954.03690350015005. [DOI] [PubMed] [Google Scholar]
- 65.Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, et al. Chimeric Sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine. 2007 Oct 23;25(43):7573–7581. doi: 10.1016/j.vaccine.2007.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. Recombinant sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J Virol. 2003 Sep;77(17):9278–9286. doi: 10.1128/JVI.77.17.9278-9286.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ni H, Yun NE, Zacks MA, Weaver SC, Tesh RB, da Rosa AP, et al. Recombinant alphaviruses are safe and useful serological diagnostic tools. Am J Trop Med Hyg. 2007 Apr;76(4):774–781. [PubMed] [Google Scholar]
- 68.Frolov I, Frolova E, Schlesinger S. Sindbis virus replicons and Sindbis virus: assembly of chimeras and of particles deficient in virus RNA. Journal of virology. 1997;71(4):2819–2829. doi: 10.1128/jvi.71.4.2819-2829.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liljestrom P, Garoff H. A new generation of animal cell expression vectors based on the Semliki Forest virus replicon. Biotechnology (N Y) 1991 Dec;9(12):1356–1361. doi: 10.1038/nbt1291-1356. [DOI] [PubMed] [Google Scholar]
- 70.Pushko P, Parker M, Ludwig GV, Davis NL, Johnston RE, Smith JF. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology. 1997;239(2):389–401. doi: 10.1006/viro.1997.8878. [DOI] [PubMed] [Google Scholar]
- 71.Polo JM, Belli BA, Driver DA, Frolov I, Sherrill S, Hariharan MJ, et al. Stable alphavirus packaging cell lines for Sindbis virus and Semliki Forest virus-derived vectors. Proceedings of the National Academy of Sciences of the United States of America. 1999 Apr 13;96(8):4598–4603. doi: 10.1073/pnas.96.8.4598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou X, Berglund P, Rhodes G, Parker SE, Jondal M, Liljestrom P. Self-replicating Semliki Forest virus RNA as recombinant vaccine. Vaccine. 1994 Dec;12(16):1510–1514. doi: 10.1016/0264-410x(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 73.Davis NL, West A, Reap E, MacDonald G, Collier M, Dryga S, et al. Alphavirus replicon particles as candidate HIV vaccines. IUBMB Life. 2002;53(4–5):209–211. doi: 10.1080/15216540212657. [DOI] [PubMed] [Google Scholar]
- 74.Thompson JM, Whitmore AC, Konopka JL, Collier ML, Richmond EM, Davis NL, et al. Mucosal and systemic adjuvant activity of alphavirus replicon particles. Proceedings of the National Academy of Sciences of the United States of America. 2006 Mar 7;103(10):3722–3727. doi: 10.1073/pnas.0600287103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dupuy LC, Locher CP, Paidhungat M, Richards MJ, Lind CM, Bakken R, et al. Directed molecular evolution improves the immunogenicity and protective efficacy of a Venezuelan equine encephalitis virus DNA vaccine. Vaccine. 2009 Jun 24;27(31):4152–4160. doi: 10.1016/j.vaccine.2009.04.049. [DOI] [PubMed] [Google Scholar]
- 76.Phillpotts RJ, Lescott TL, Jacobs SC. Vaccinia virus recombinants encoding the truncated structural gene region of Venezuelan equine encephalitis virus (VEEV) give solid protection against peripheral challenge but only partial protection against airborne challenge with virulent VEEV. Acta Virol. 2000 Oct;44(5):233–239. [PubMed] [Google Scholar]