Abstract
Monitoring disparities over time is complicated by the varying disparity definitions applied in the literature. This study used data from the 1996-2005 Medical Expenditure Panel Survey (MEPS) to compare trends in disparities by three definitions of racial/ethnic disparities and to assess the influence of changes in socioeconomic status (SES) among racial/ethnic minorities on disparity trends. This study prefers the Institute of Medicine’s (IOM) definition, which adjusts for health status but allows for mediation of racial/ethnic disparities through SES factors. Black-White disparities in having an office-based or outpatient visit and medical expenditure were roughly constant and Hispanic-White disparities increased for office-based or outpatient visits and for medical expenditure between 1996-1997 and 2004-2005. Estimates based on the independent effect of race/ethnicity were the most conservative accounting of disparities and disparity trends, underlining the importance of the role of SES mediation in the study of trends in disparities.
Keywords: racial disparities, medical expenditure, trends, statistical adjustment for health status
Aconsensus has emerged that disparities by race and ethnicity exist in many areas of health care (Agency for Healthcare Research and Quality [AHRQ], 2003, 2004, 2005b, 2006b, 2007; Institute of Medicine, 2002; U.S. Department of Health and Human Services [USDHHS], 2000). Attention is now turning to the question of whether racial/ethnic disparities in health care are increasing or diminishing. Research has established that changes in health care organization, the rate of innovation (Goldman & Smith, 2005; Groeneveld, Laufer, & Garber, 2005), and patterns of immigration (Alegria et al., 2007), among other factors, affect disparities. The net effect of these forces over time, along with any explicit policies designed to reduce disparities, is not clear. Thus, tracking disparities over time is a crucial component of the national research agenda for ensuring an equitable distribution of health care services.
To track disparities, methods and definitions need to be applied consistently over time. Disparity connotes unfair differences across racial/ethnic groups, but it is often not explicitly defined in empirical work. The major definitions of disparity identify different components of the difference as a disparity. We categorize methods used in previous studies of racial/ethnic health care disparities into one of the following three groups, each with an implicit or explicit definition of disparity.
Definition 1: AHRQ—A Disparity Is the Total Difference Between Racial/Ethnic Groups
The AHRQ, in the 2004 National Healthcare Disparities Report (NHDR), defined racial disparity in the same way as Healthy People 2010 (USDHHS, 2000):
In pursuit of the overarching goal of eliminating health disparities, all differences among populations in measures of health and healthcare are considered evidence of disparities. (p. 7)
The AHRQ compares health care utilization, quality of care, and access to care among racial/ethnic groups by comparing differences in means and making the assessment of disparities and the tracking of disparity trends a straightforward analytical task not requiring the use of statistical modeling.
It is not clear, however, that fairness-based health policy should be concerned with all differences. Disparities are about the parts of differences that are unfair, and not all are. Blacks are younger than Whites on average, and differences due to lower health needs from being younger do not represent unfair differences or a concern for public policy. On the other hand, at comparable ages, Blacks have lower health status than Whites (National Center for Health Statistics, 2005), and therefore only if Blacks had higher average use than Whites at the same age would health care be distributed according to need. Thus, the difference definition of disparities may be simple to implement but does not measure differences that are unfair. It is not even an upper bound because the adjustment for health status could go either way when comparing Whites with Blacks or another group.
Moy, Dayton, and Clancy (2005, p. 377) advocated the AHRQ approach using unadjusted means on practical grounds, arguing that the available data are not adequate to adjust for patient needs and preferences, as would be called for in implementing the Institute of Medicine’s (IOM) approach (discussed below). While we agree that preference data are poor and problematic, many national data sets include good measures of health status that might improve on the total difference estimate of disparities.
Results from the NHDR are that Blacks and Hispanics are less likely on average to have insurance, a usual source of care, and an outpatient or office-based visit in the past year (AHRQ, 2007). Because the NHDR has been publishing for 5 years and uses data dating back to 1998 (1992 for cancer incidence and treatment disparities), analysis of disparities trends are possible. The authors find that disparities have diminished slowly for Blacks, but the majority of disparities for quality and access have widened for Hispanics (AHRQ, 2007; Clancy, 2006).1
Starting in 2004, the AHRQ included stratified and multivariate analyses to “disentangle the independent effects of different SES measures on racial and ethnic disparities” (AHRQ, 2004, p. 13). The multivariate analyses were conducted using logistic regression models controlling for age, gender, household income, education, insurance, and residence location. These analyses were meant to estimate the contribution of these variables to the disparity. The AHRQ definition and method for measuring the disparities were left unchanged.
Other studies also use a simple difference measure of disparities. Kirby, Taliaferro, and Zuvekas (2006) applied Oaxaca-Blinder decomposition methods on Medical Expenditure Panel Survey (MEPS) data to assess which factors (including community-level factors) account for the total difference between groups, and they used the terms difference and disparity equivalently.2
Definition 2: Residual Direct Effect (RDE) of Race/Ethnicity
An alternative definition of racial disparities is any difference between racial/ethnic groups, after controlling for as many other factors affecting use as are available in the data. While not always overtly stated, this is the definition implied by studies focusing on the race/ethnicity coefficient in a multivariate regression model. Because the race coefficient measures the effect of race after adjusting for all other variables in the model, this method can be called the residual direct effect.3
Typical of the previous studies that use RDE-based methods are analyses that estimate race effects with and without controlling for socioeconomic variables (Fiscella, Franks, Doescher, & Saver, 2002; Guevara, Mandell, Rostain, Zhao, & Hadley, 2006; Trivedi, Zaslavsky, Schneider, & Ayanian, 2005; Vaccarino et al., 2005) or present results from models that adjust for socioeconomic variables (AHRQ, 2005b, 2006b). Identifying the change in the race/ethnicity coefficient between a base model and a more fully specified model is a common method of measuring the mediation of variables (Baron & Kenny, 1986). If race effects disappear when socioeconomic variables are added to a base model, the RDE-based definition implies that there are no racial/ethnic disparities though there may be disparities by socioeconomic status (SES).
Two recent studies focus on the residual race effect when studying trends in disparities. Trivedi et al. (2005) tracked disparities in health care effectiveness data and information set (HEDIS) measures of performance for Medicare managed care health plans by fitting linear models of quality performance and evaluating the significance of the race/year interaction variable for data from 1997 to 2004. Three models of performance on HEDIS quality measures were estimated. The first adjusted for age and sex. The second added rural residence and health plan, and the third added variables for Medicaid eligibility and zip code-level variables for income and education. Disparities in all models narrowed over time for seven of the nine HEDIS measures. Vaccarino et al. (2005) used a similar strategy, evaluating the significance of race, year, and sex interaction coefficients from logistic regressions of the use of evidence-based acute myocardial infarction (AMI) management. Three separate models were used. Model 1 included all interactions and main effects of the variables race, year, and sex. Model 2 added demographic and clinical factors, and Model 3 added hospital characteristics. No evidence was found that disparities in AMI management had moderated between 1994 and 2002.
Definition 3: IOM—A Disparity Is All Difference Except Those Due to Health Status
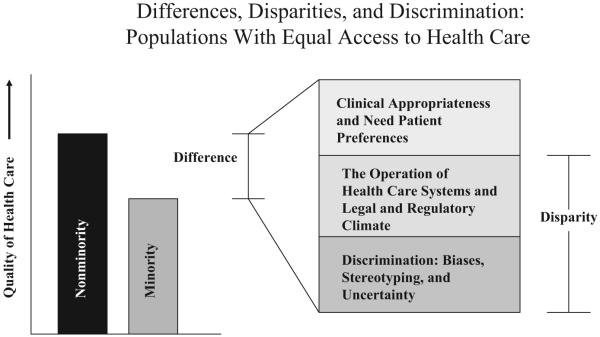
We propose (and prefer) a third method of defining a disparity that is based on the IOM definition of racial/ethnic healthcare disparities (IOM, 2002; reproduced as Figure 1 here). In Unequal Treatment (IOM, 2002), the IOM defined disparity to be any difference not due to clinical need or preferences for health care services. Differences that are considered to be disparities include differences due to the operation of health care systems, the legal and regulatory climate, discrimination, or other factors.
Figure 1. The Institute of Medicine’s Definition of Racial/Ethnic Health Care Disparities.
Source: Institute of Medicine (2002).
To apply the IOM definition to analyses of large, national health care data sets, the researcher must decide whether variables used in the analysis are related to clinical need or preferences. Clinical need can be measured using health status variables and variables highly correlated with health status such as age and sex. Identifying variables related to preferences is more problematic. These variables are typically not measured at all or measured imperfectly in national surveys. Furthermore, patients are rarely fully informed about their clinical options when deciding to access health care (Ashton et al., 2003; IOM, 2002). Braddock et al. (1999) found that only 9% of clinical decisions were considered to be made with patient-informed decision making. Minority patients may be even less likely than Whites to have fully informed preferences for health care because of language and cultural barriers to care and communication difficulties with providers. Further complicating the treatment of preferences is that they may themselves have been influenced by contributors to disparities such as past discrimination (Cooper-Patrick et al., 1997). Without accounting for the association between preferences, SES, and previous discrimination, the inclusion and adjustment of preferences in disparities models may lead to biased disparity estimates.
Differences due to the operation of health care systems and the legal and regulatory climate (considered to contribute to disparities according to the IOM definition) can be captured by SES variables. For example, individuals of lower SES may have more difficulty paying for health care and navigating the health care system. If this leads to poorer health care, and minorities are disproportionately represented in lower SES categories, then the operation of the health care system impacts disparities through SES. Moreover, race may independently influence health care through discriminatory practices by providers or health services organizations that lead to disparate access to care and rates of utilization.
The IOM definition of health care disparities can be summarized as all differences not due to health status. Interpreting the definition in this way assumes that health status is a reasonable summary of clinical need and appropriateness and concedes that the difficulty of identifying preferences precludes them from use in the disparity measurement. On the other hand, differences due to SES, health care system factors, and race (via racial discrimination) can be considered to be unfair and should be incorporated into the disparity calculation.
The most basic factors affecting health status are age and gender, and we consider studies about trends in disparities that adjust for age and gender, but not SES or other factors, in keeping with the spirit of the IOM definition. Escarce and McGuire (2004) replicated methodology in Escarce, Epstein, Colby, and Schwartz (1993) to compare Black and White rates of procedure use in Medicare between 1986 and 1997. Identical clinical algorithms and definitions were applied to 5% of the national Part B data from the traditional (fee-for-service) Medicare program for the two time periods. Rates were adjusted by age and gender. Black-White differences persisted over this time period, but the differences narrowed. For all but 4 of the 30 procedures and tests measured, there was a statistically significant decrease in the Black-White disparity.
Jha, Fisher, Li, Orav, and Epstein (2005) also used Part B data from traditional Medicare to measure differences between Blacks and Whites, adjusted for age and gender, for nine major surgical procedures. Between 1992 and 2001, the difference increased significantly for five out of the nine procedures and narrowed significantly for only one procedure. The methods and data in this recent study were the same as Escarce and McGuire, except for the partial overlap in time periods. Assembly of a longer time series in Medicare would be necessary to reconcile the apparent differences in the findings of the two studies.
Empirical Distinctions Among the Definitions
The distinction between the IOM and the AHRQ definitions of disparity is that the IOM counts as a disparity only the differences that persist after accounting for the contribution of health status. The IOM and the AHRQ definitions both allow SES to mediate the relationship between race and quality of care. Individuals of lower SES may have more difficulty paying for care and navigating health care services and the legal and regulatory infrastructure. If minorities are disproportionately represented in lower SES categories, then this failure to serve lower-SES groups contributes to racial disparities.
The distinction between the IOM and RDE-based definitions is the IOM’s inclusion of SES-mediated disparities. It is natural for empirical researchers to build the most fully specified model possible to explain differences between groups, estimating the independent effect of the many factors influencing utilization. The question of what is the right empirical model, however, is distinct from what are the components of the model that contribute to a disparity. Within a fully specified model, the researcher must still choose to estimate disparities based on a coefficient or coefficients indicating race/ethnicity or allowing for mediating factors.
Figure 2 depicts the distinctions between these three definitions of disparity in empirical terms. The AHRQ definition counts the full difference between groups, irrespective of the source. The IOM counts all differences except those due to health status, and the RDE counts only the direct effect of race. Clearly, a statistical model is necessary to implement either the IOM or RDE definition, but not the AHRQ approach.
Figure 2. Three Definitions of Racial Disparities.
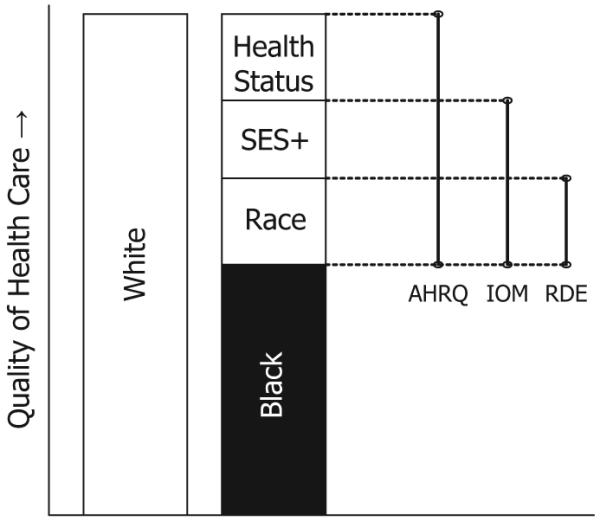
Note: Bars on the right of figure represent differences included in racial disparities definitions according to the AHRQ in the National Healthcare Disparities Reports, the IOM, and the RDE method used in other health services literature. SES+ = socioeconomic status (SES) variables plus two variables that are highly correlated with SES: health insurance type and region of country; AHRQ = Agency for Healthcare Research and Quality; IOM = Institute of Medicine; RDE = residual direct effect.
The choice of a disparity definition generally affects the size of the estimated disparity. Much of the disparities research is about measuring the magnitudes of disparities, and the policy importance of disparities is premised on a significant magnitude of unfair differences. With this at stake, arguments have been made in support of different definitions. On one side, critics fault both the AHRQ and IOM reports for not isolating the independent effect of race/ethnicity from other factors, in effect, advocating for the RDE method of measurement, adjusting for all SES and health status covariates. Klick and Satel (2006) questioned the IOM position, stating that claims of racial disparities are only warranted in those areas where residual differences remain after controlling for SES and all other confounding variables (many of which, the authors pointed out, have been unmeasured in retrospective studies). Drafts of the first NHDR ran into the same criticism. According to Bloche (2004), critics of the draft claimed that the research literature “failed to show that race mattered by itself, apart from social class and insurance status” (p. M1). Bloche’s response, consistent with the IOM approach, points out that racial/ethnic disparities are still unfair, and worthy of policy attention, even if they arise through differences in income, wealth, or insurance.
The debate comes down to whether the definition of racial disparity should include effects mediated through other factors, such as SES, insurance, or geography. Suppose we found income was all that mattered in a regression determining access, Blacks have worse access than Whites as they have lower income on average. Are there racial disparities in health care access? If one focused on race as the cause of disparities, the answer would have to wait for further research to see if race caused the lower income. If one focused on describing the situation and answering the question, “Do Blacks have worse access than Whites?” the answer would be yes. Both the AHRQ and IOM definitions include SES-mediated disparities; the RDE-based definition does not.
In sum, the literature on trends in disparities has not come to a clear resolution of the question of the direction of trends for either Blacks or Hispanics. Inconsistent definitions of disparity hinder unified interpretation of the studies. In this article, we compare trends in two overall measures of health care disparities applying three alternative definitions of disparity to data from the MEPS, an ongoing national survey widely used for disparities assessment. The purpose of this article is threefold:
To introduce a rigorous methodology of disparities measurement using the IOM definition and apply it to the measurement of trends.
To compare the preferred IOM definition to two other definitions typically used in the literature.
To measure how trends in SES account for disparity trends.
New Contribution
First, we contribute to the literature by conducting an empirical analysis of trends in health care disparities using a definition of disparities proposed by the IOM and the most recently available, nationally representative health care utilization and expenditure data. We use the MEPS for the years 1996 to 2005, extending both forward and backward the 1999-2004 MEPS data used in the NHDR (AHRQ, 2003, 2004, 2005b, 2006b, 2007). In addition to expanding the number of years covered, we also report on trends in disparities with a global outcome from the MEPS data, total spending on health care.
Second, we compare the IOM definition to other definitions to track disparity trends, highlighting the empirical importance of the adjustment of health status variables and the mediation of SES variables. We believe that adjusting for health status isolates the unfair portion of differences that should be relevant to policy makers.
Third, we decompose disparity trends to estimate the contribution of SES trends to trends in disparities. Because the IOM definition considers differences mediated by SES to be included in disparity measurements, changing patterns of employment, uninsurance, or immigration can affect disparities. It is important for purposes of policy to know, for example, if Hispanic-White disparities are widening, if this is due to the changing sociodemographics of the underlying populations or to changes in the functioning of the health care system.
Data
The data are from the MEPS, which contains variables related to individuals’ health care expenditures, utilization, demographic, SES, and health status characteristics. To measure trends during this time period, models were fit using MEPS data from two pooled time periods (1996-1997 and 2004-2005). Two years were used in the early and late periods to increase the precision of estimates. The change in disparities was thus estimated over an 8-year period. Unadjusted analyses used data from 1996 to 2005. The dependent variables we studied were any office or outpatient visit and total medical expenditures in each calendar year. The first of these variables is equivalent to one of the dependent variables used in the NHDR. The total medical expenditure variable supplements the NHDR analysis by providing a global health care utilization measure with greater variation than binary variables. Total expenditure was constructed by summing all direct payments for care provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources.4 Data were taken from responses to the Medical Provider and Household Components of the MEPS as reported on the MEPS public use files. Prices were adjusted to 2005 dollars using the gross domestic product (GDP) deflator. The GDP deflator is a broader measure than the more commonly used consumer price index (CPI). The CPI covers only about 60% of the economy and omits investment goods, rural consumers, and, most importantly in the context of health care spending, government purchases.
Covariates used in our model were classified into two broad categories to implement the IOM definition of disparity: SES variables and health status variables. The SES variables include education level (less than high school, high school graduate, any college, college graduate), income level (below federal poverty level [FPL], near poverty [100%-125% FPL], low income [125%-200% FPL], middle income [200%-400% FPL], and high income [≥400% FPL]), region of the country (Northeast, South, Midwest, and West), and insurance coverage (private, Medicare, Medicaid or other public insurance, and uninsured). Health status variables include gender, age (18-24, 25-34, 35-44, 45-54, 55-64, 65-74, 75+), having any functional limitation, and self-assessed health scores (excellent, very good, good, fair, poor). These variables are nearly equivalent to the variables used in the multivariate analyses of the NHDR. The NHDR includes location of residence, whereas we include geographic region, and we add marital status, any limitation of activity, and self-reported health status. Census categories were used for questions about race and ethnicity. Individuals of any race claiming to be of Hispanic origin were identified as Hispanic in our study. Other respondents were classified as Black or White by responses to the question about race.
Method
Applying Definitions of Disparity
We applied the three major definitions of disparities, recognizing that each answers a distinct empirical question. Measuring all differences except those due to health status, as recommend by the IOM, calls for an explicit empirical counterfactual. The counterfactual we pose is as follows: What would Blacks (or Hispanics) have used if they had the same health status as Whites but retained their own racial and SES characteristics? This counterfactual was compared with the actual White usage, and the difference is the disparity.5 We calculate this for time periods pooled from the endpoints of our data, 1996-1997 and 2004-2005, and test if the disparity changed over time. We adjusted for all available health status-related characteristics and allowed differences mediated by SES to enter into disparity calculations. Specifics about these adjustment methods are provided below after our empirical model is set out.
The question addressed by the AHRQ total difference measure is as follows: How does the average use of Whites compare with the average for Blacks (or Hispanics)? All group averages were observed directly, and no empirical counterfactual is needed to interpret the measured difference. We tested for trends in this total difference.
Finally, we calculated the RDE, for each racial/ethnic group at each time period, to assess the independent effect of race. The RDE captures the unmediated effect of race/ethnicity in models that include all available covariates, including interactions. Specifically, we calculated the independent effect of race/ethnicity by fitting a regression model, switching all Black race indicators from 0 to 1, and then using model coefficients to predict outcomes in the White (with a positive Black race indicator) subpopulation for each time period. A similar calculation estimates the Hispanic RDE by generating model predictions for the White (with a positive Hispanic race indicator) subpopulation for each time period. This measure also addresses a counterfactual: What would Whites have used in each time period if they kept all their characteristics (SES, health status, etc.) except were Black (or Hispanic)? Then, the disparity is the difference between the actual White use and this counterfactual use, and the disparity trend is the difference in disparity over time. The isolation of the effect of race/ethnicity over time is analogous to the method used in studies determining the existence of a disparity trend based on a significant Race × Time interaction coefficient, controlling for all other variables.
Estimation
The IOM and RDE definitions of disparity call for predictions based on statistical modeling. For the dichotomous variable of any outpatient or office-based visit, we used a multivariate logistic regression model similar to those used in the NHDR. Because we were estimating differences in racial/ethnic differences over two pooled time periods (1996-1997 and 2004-2005), main effects of race/ethnicity and year as well as a Race × Year interaction term were used as predictors. Other predictors used were a vector of health status variables and a vector of SES variables. To account for the differential return by race of SES and health status variables, significant SES × Race and Health Status × Race interactions were added to the model.
| (1) |
where f is the inverse logistic function, Yit is the utilization by individual and time, Healthi is the vector of health status indicator variables, SESi is the vector of SES characteristics, including poverty status and education, and Yeart is the vector of year indicator variables.
For the continuous medical expenditure variable, we used the same set of covariates from Equation 1 in a generalized linear model (GLM) with quasi likelihoods (McCullagh & Nelder, 1989), a form of nonlinear least squares modeling. Expected expenditures E(y|x) were modeled directly as μ(x’β), where x are the predictors and μ is the link between the observed raw scale of expenditure y and the linear predictor x’β. The conditional variance of y is a power of expected expenditures. Thus,
| (2) |
where μ is a log transformation, and λ is 2, making the distribution of the variance equivalent to a gamma distribution of the expected expenditures.
All model estimates were weighted to reflect sample design and survey nonresponse.
Adjustment for Health Status
To apply the IOM definition of racial disparities in the context of the model described above, health status variables were adjusted using a method described in Cook (2007) and McGuire, Alegria, Cook, Wells, and Zaslavsky (2006). Actual White average use was compared to a counterfactual minority group with White health status characteristics and minority SES characteristics and race. To create this counterfactual, the entire distribution of minority health values (not just the mean) was transformed. Our approach generalizes the Oaxaca-Blinder mean replacement method commonly used with linear models (Hargraves & Hadley, 2003; Kirby et al., 2006; Weinick, Zuvekas, & Cohen, 2000; Zuvekas & Taliaferro, 2003).6
The health status variables used in this study are dichotomous or ordinal. We adjusted self-reported health status, age, and having any functional limitation by transforming the minority distribution to match White distributions, while attempting to preserve the correlation structure among these variables within the minority group. First, a health status composite z-score was calculated for each variable by x - x‾/σx; each variable was scored so that a positive z-score was an indicator of better health. An individual’s z-scores for all health status variables were then added to create the composite score, which was used as the ranking mechanism to determine which of the minority individuals would have their health status indicator changed. Starting with poor health status, we switched minority individuals with the highest composite health status score from poor to fair (an individual is never shifted twice) until the minority proportion of each of the categories was equated with the White proportion. We repeated this method for the other self-reported health status categories. For age, we made minority individuals with the lowest composite health status score one age group older (again, an individual is never shifted twice) until proportions were equal. For functional limitation, we switched the functional limitation indicator from 0 to 1 for minority individuals with the lowest composite health status score.
Gender was also transformed so minority distributions matched White distributions. However, the composite score was not used to switch outcome indicators to match distributions. Rather, if x‾Minority > x‾White, then minorities with positive health status indicators were switched at random until x‾Minority = x‾White. Likewise, if x‾Minority < x‾White, then minorities with negative health status indicators were switched at random until x‾Minority = x‾White.
Once these distribution adjustments were made, coefficients from the previously generated model were used in combination with the adjusted health status values to calculate predicted disparities in health care expenditures.
The Contribution of SES to Disparity Trends
We assessed the contribution to disparities of trends in SES factors using a similar methodology. Specifically, we ask, what would disparities be for Blacks and Hispanics in 2004-2005 if these groups had the same SES characteristics as they did in 1996-1997? For this purpose, we used the rank and replace methodology described above, transforming marital status, poverty status, education, health insurance, and region for Blacks and Hispanics in 2004-2005 to their 1996-1997 values. Our counterfactual is then as follows: What Blacks (Hispanics) would have used had they had the same health status as Whites, but the SES characteristics of Blacks (Hispanics) in 1996-1997. This was compared against the White actual use to estimate what disparities would have been had the SES characteristics minority of the populations not changed.
Variance Estimation
Variance estimates for model coefficients and unadjusted rates account for the complex sample design, and stratum and primary sampling unit variables are standardized across pooled years (AHRQ, 2005a). Variance estimates for difference-in-difference comparisons were calculated using a balanced-repeated-replication (BRR) procedure (Wolter, 1985). This method of measuring standard errors repeats the estimation process used on the full sample on a group of subsamples of the population, each of which is half of the full sample size. Difference-in-difference estimates were calculated for each of the 64 subsamples provided by AHRQ, and the variation of these estimates was calculated (AHRQ, 2006a).
Results
Table 1 presents unadjusted means by race and year for variables used in models in this article. Medical care spending on Whites and Blacks increased significantly between 1996-1997 and 2004-2005, whereas spending on Hispanics increased little. The same trend was found for any office-based or outpatient visit with increased White and Black rates and little change in Hispanic rates. The percentage of respondents reporting excellent health status declined for all groups over this period, though no trends in self-reported health status were significantly different by race/ethnicity. The percentage of Hispanics having any functional limitation only slightly increased over this period, a significant difference from the increasing trend among Whites. Over time, Blacks were less likely to live in poverty, more likely to be in the high-income category, and less likely to be uninsured, although these trends were not significantly different from Whites. Fewer Hispanics lived in poverty in 2004-2005 than in 1996-1997, a significantly different trend than Whites. The percentage of Hispanics who graduated from college remained stable over this time period, a significant difference from the increasing trend among Whites.
Table 1. 1996-1997 and 2004-2005 Medical Expenditure Panel Survey’s (n = 72,106) Weighted Population Characteristics for Blacks, Hispanics, and non-Hispanic Whites Age ≥ 18a.
| White |
Black |
Hispanic |
||||
|---|---|---|---|---|---|---|
| 1996-1997 (%) |
2004-2005 (%) |
1996-1997 (%) |
2004-2005 (%) |
1996-1997 (%) |
2004-2005 (%) |
|
| Total expenditures (US$2005) |
$2,929.44 | $4,502.73 | $2,023.20 | $3,569.53 | $1,767.75 | $2,184.14b |
| Any office-based or outpatient visit |
76.1 | 79.3 | 61.9 | 65.9 | 57.0 | 56.2b |
| Age | ||||||
| 18-24 | 11.3 | 10.7 | 15.9 | 15.2 | 18.5 | 17.4 |
| 25-34 | 18.5 | 16.3 | 22.8 | 20.4 | 28.3 | 26.5 |
| 35-44 | 22.1 | 18.4 | 23.9 | 21.5 | 23.5 | 23.8b |
| 45-54 | 17.7 | 19.6 | 16.7 | 19.2 | 13.4 | 15.4 |
| 55-64 | 11.7 | 15.6 | 8.9 | 11.9 | 8.1 | 8.9b |
| 65-74 | 10.2 | 9.9 | 7.3 | 6.9 | 5.3 | 4.9 |
| 75+ | 8.4 | 9.4 | 4.5 | 4.8 | 2.9 | 3.0 |
| Gender | ||||||
| Female | 52.0 | 52.1 | 55.7 | 56.1 | 49.0 | 49.9 |
| Marital status | ||||||
| Married | 60.6 | 58.9 | 36.0 | 34.5 | 55.3 | 54.7 |
| Health status | ||||||
| Excellent | 31.7 | 28.5 | 27.2 | 23.0 | 25.2 | 24.2 |
| Very Good | 32.2 | 33.6 | 27.7 | 28.9 | 28.1 | 29.1 |
| Good | 24.2 | 25.6 | 27.9 | 29.7 | 28.5 | 30.8 |
| Fair | 8.5 | 8.7 | 12.4 | 14.5 | 13.9 | 12.5 |
| Poor | 3.4 | 3.6 | 4.9 | 4.0 | 4.2 | 3.4 |
| Limitation of activity | ||||||
| Any | 25.5 | 29.7 | 21.9 | 28.0 | 17.9 | 18.7b |
| Poverty status | ||||||
| Below poverty line |
7.9 | 8.1 | 22.1 | 21.7 | 22.5 | 17.4b |
| Near poverty | 3.5 | 3.1 | 6.5 | 5.9 | 8.2 | 7.6 |
| Low income | 12.3 | 11.1 | 18.2 | 17.8 | 21.4 | 21.4 |
| Middle income | 33.4 | 31.0 | 31.3 | 31.6 | 30.7 | 32.7b |
| High income | 42.8 | 46.7 | 21.9 | 22.9 | 17.1 | 20.8 |
| Education | ||||||
| <HS | 15.5 | 13.4 | 22.9 | 23.5 | 42.5 | 43.9 |
| HS graduate | 33.9 | 32.9 | 38.0 | 35.9 | 29.4 | 28.4 |
| Some college | 24.2 | 24.5 | 24.5 | 25.3 | 17.0 | 16.6 |
| College graduate | 26.4 | 29.2 | 14.6 | 15.4 | 11.1 | 11.1b |
| Health insurance | ||||||
| Private insurance | 81.1 | 78.7 | 60.3 | 60.0 | 51.2 | 49.3 |
| Medicare | 20.3 | 21.3 | 14.9 | 15.6 | 9.5 | 9.5 |
| Medicaid | 5.6 | 6.4 | 18.8 | 20.0 | 16.7 | 16.0 |
| Uninsured | 9.4 | 9.6 | 18.3 | 17.5 | 30.9 | 32.9 |
| Region | ||||||
| Northeast | 20.7 | 19.6 | 17.8 | 16.0 | 16.4 | 14.4 |
| Midwest | 26.8 | 26.7 | 18.0 | 18.2 | 7.1 | 8.1 |
| South | 33.2 | 34.1 | 55.2 | 56.7 | 33.7 | 36.5 |
| West | 19.3 | 19.6 | 9.1 | 9.1 | 42.8 | 41.1 |
| Urbanicity | ||||||
| Living in MSA |
77.8 | 79.5 | 84.7 | 87.9 | 91.3 | 92.4 |
| Not living in MSA |
22.2 | 20.5 | 15.3 | 12.1 | 8.7 | 7.6 |
Note: HS = High school; MSA = metropolitan statistical area.
Calculations are weighted to be representative of the entire U.S. population.
Difference in trends for minority group is significantly different than difference in trends for Whites.
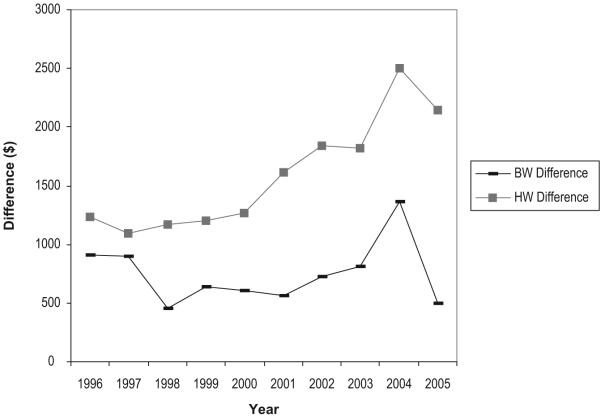
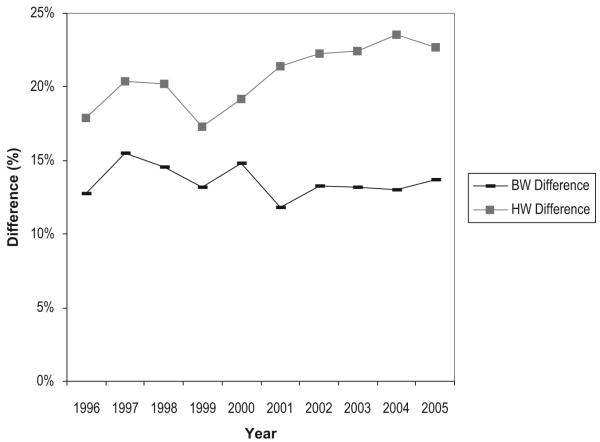
Figure 3 presents, in 2005 dollars, the difference in Black-White and Hispanic-White total medical expenditures for the years 1996-2005, corresponding to the AHRQ definition of disparity. Both Hispanic-White and Black-White disparities increased sharply in 2004 and dropped in 2005. From 1996 to 2005, the Hispanic-White disparity increased steadily over time whereas the Black-White disparity remained relatively stable during that time period. Figure 4 shows unadjusted Hispanic-White and Black-White disparity trends for having any outpatient or office-based visit in the past year. For the years 1996-2005, Hispanic-White disparities generally increased over time, whereas Black-White disparities were roughly constant.
Figure 3. Unadjusted Black-White (BW) and Hispanic-White (HW) Differences in Total Medical Expenditures (US$2005).
Figure 4. Unadjusted Black-White (BW) and Hispanic-White (HW) Difference in Any Outpatient or Office-Based Visit.
Table 2 presents model coefficients for having an outpatient or office-based visit and total medical expenditures in the past year. Interaction terms were centered by subtracting the mean value so that main effects are readily interpretable (Kraemer & Blasey, 2002). Black and Hispanic coefficients show a significantly lower probability of a doctor visit and lower total medical expenditures than Whites, controlling for all other factors. No significant interaction effects with time were found for Blacks. Hispanics showed a significantly negative interaction effect with time in both medical expenditure and having any doctor visit in the past year, one indicator of growing Hispanic-White disparities in both of these measures. Significant predictors were generally similar in the two models. Positive predictors include being female, older age, having any functional limitation, being married, poorer health status, higher education, and being insured especially in Medicaid and Medicare.
Table 2. Models of Total Medical Expenditures (US$2005) and Any Doctor Visit in the Past Year on Race and Time With Demographic, SES, and Health Status Variables Used as Independent Controls (n = 72,106)a,b.
| Expenditures (US$2005) |
Doctor Visit in Past Year |
|||
|---|---|---|---|---|
| Coefficient | SE | Coefficient | SE | |
| Race (referent White) | ||||
| Black | -0.29* | .05 | -0.49* | .05 |
| Hispanic | -0.35* | .05 | -0.46* | .04 |
| Year (referent 1996-1997) | ||||
| 2004-2005 | 0.32* | .03 | 0.08* | .03 |
| 2004-2005 Black | 0.09 | .07 | -0.003 | .07 |
| 2004-2005 Hispanic | -0.14* | .07 | -0.17* | .07 |
| Gender (referent male) | ||||
| Female | 0.38* | .03 | 0.97* | .02 |
| Age (referent 35-44) | ||||
| 18-24 | -0.21* | .05 | 0.002 | .04 |
| 25-34 | -0.11* | .04 | -0.05 | .03 |
| 44-55 | 0.21* | .04 | 0.22* | .04 |
| 55-64 | 0.53* | .04 | 0.61* | .05 |
| 65-74 | 0.38* | .08 | 0.58* | .12 |
| 75+ | 0.59* | .09 | 0.76* | .13 |
| Limitation of activity (referent no limitation) | ||||
| Any | 0.71* | .03 | 0.71* | .04 |
| Marital status (referent not married) | ||||
| Married | 0.10* | .03 | 0.16* | .03 |
| Self-reported health status (referent excellent) | ||||
| Very good | 0.19* | .04 | 0.31* | .03 |
| Good | 0.47* | .04 | 0.54* | .03 |
| Fair | 0.84* | .05 | 1.07* | .05 |
| Poor | 1.21* | .05 | 1.42* | .10 |
| Poverty status (referent below poverty) | ||||
| Near poverty | -0.02 | .08 | 0.03 | .07 |
| Low income | -0.05 | .06 | 0.12* | .05 |
| Middle income | -0.02 | .06 | 0.25* | .05 |
| High income | 0.15* | .07 | 0.47* | .05 |
| Education (referent less than high school) | ||||
| HS graduate | 0.11* | .04 | 0.19* | .03 |
| Some college | 0.20* | .04 | 0.43* | .04 |
| College graduate | 0.28* | .04 | 0.70* | .05 |
| Health insurance (referent private insurance) | ||||
| Medicaid | 0.40* | .07 | 0.17* | .05 |
| Medicare | 0.34* | .08 | 0.56* | .11 |
| Other public | -0.03 | .16 | 0.15 | .24 |
| Uninsured | -0.93* | .05 | -1.00* | .04 |
| Region (referent Northeast) | ||||
| Midwest | 0.04 | .04 | -0.02 | .05 |
| South | -0.04 | .03 | -0.05 | .04 |
| West | 0.03 | .04 | -0.02 | .05 |
| Urbanicity (referent not living in an MSA) | ||||
| Living in MSA | 0.05 | .03 | -0.03 | .04 |
| Constant | 7.00* | .05 | 0.40* | .06 |
Note: HS = high school; MSA = metropolitan statistical area.
Logit coefficients and standard errors take into account sampling weights and stratification used to make Medical Expenditure Panel Survey sample representative of U.S. population.
In this table, we do not present Race × Gender, Race × Age, Race × Self-Reported Health Status, Race × Poverty, or Race × Education interactions that were included in the model. Race, year, education, and income coefficients are centered on the means so that regression coefficients on a given characteristic can be directly interpreted as the difference by race from the overall mean of the characteristic.
p < .05.
Table 3 presents our main results. Trends in disparities for having any doctor visit in the past year and total medical expenditure were estimated using the three definitions of racial disparity. The left-most columns present estimates based on the AHRQ definition measuring unadjusted differences. (This is the result graphed in Figures 3 and 4 except that the 2 years at the beginning of the period were pooled and the 2 years at the end were pooled to make these estimates comparable to the model-based estimates.) The middle columns show the implementation of the IOM definition of racial disparities adjusting for health status. The right-most columns present RDE estimates of disparities adjusting for both health status and SES variables.
Table 3. Trends in Disparities Using Three Definitions for Any Doctor Visit and Total Expenditurea.
| AHRQ |
IOM |
Independent Race Effect |
||||
|---|---|---|---|---|---|---|
| Unadjusted |
HS Adjustment With SES Mediationb |
Adjustment of All Variablesc |
||||
| Definition of Disparities | Predicted Disparity |
SEd | Predicted Disparity |
SEd | Predicted Disparity |
SEd |
| Black-White | ||||||
| Any doctor visit | ||||||
| 2004-2005 (%) | -13.4* | 1.0 | -13.6* | 0.8 | -7.6* | 0.8 |
| 1996-1997 (%) | -14.2* | 1.1 | -14.3* | 0.9 | -8.2* | 1.0 |
| Difference in disparity (%) | 0.8 | 1.5 | 0.7 | 1.2 | 0.6 | 1.2 |
| Total medical expenditure (US$) | ||||||
| 2004-2005 | -933.20* | 195 | -1,053.52* | 210 | -922.93* | 235 |
| 1996-1997 | -906.22* | 148 | -868.50* | 157 | -813.28* | 170 |
| Difference in disparity | -26.98 | 245 | -185.03 | 232 | -109.64 | 248 |
| Hispanic-White | ||||||
| Any doctor visit | ||||||
| 2004-2005 (%) | -23.1* | 1.2 | -19.8* | 0.9 | -8.1* | 1.0 |
| 1996-1997 (%) | -19.2* | 1.2 | -16.4* | 0.8 | -5.8* | 1.0 |
| Difference in disparity (%) | -3.9* | 1.6 | -3.4* | 1.1 | -2.3* | 1.0 |
| Total medical expenditure (US$) | ||||||
| 2004-2005 | -2,318.60* | 152 | -1,818.83* | 136 | -1,455.56* | 247 |
| 1996-1997 | -1,161.70* | 123 | -1,011.44* | 97 | -609.58* | 182 |
| Difference in disparity | -1,156.90* | 195 | -807.40* | 171 | -845.99* | 225 |
Note: Data are from 1996/1997 and 2004/2005 Medical Expenditure Panel Survey. AHRQ = Agency for Healthcare Research and Quality; IOM = Institute of Medicine; HS = health status; SES = socioeconomic status.
Figures shown are Black-White and Hispanic-White differences and disparities in any doctor visit and total medical expenditure.
Health status-related variables used in adjustment are age, sex, marital status, activity limitation, and self-reported health status.
Variables used in adjustment model are health status-related variables, poverty status, education, health insurance, and region.
Standard errors are calculated using balanced-repeated-replication methodology.
p < .05.
We first focus on the results from the analysis based on the IOM definition, our preferred method. Black-White disparities in any doctor visit and total medical expenditures in the past year did not change between 1996-1997 and 2004-2005. For Blacks, disparities within the periods were similar. Blacks had about 14% lower likelihood of making a doctor visit in both time periods. The Black-White disparity in expenditures rose from US$869 in 1996-1997 to US$1,054 in 2004-2005, but the difference was not statistically significant.
Hispanic-White disparities in any doctor visits and total medical expenditures increased between 1996-1997 and 2004-2005. In 1996-1997, Hispanics were 16% less likely to see a doctor and had US$1,011 less in expenditures in comparison to Whites, slightly greater disparities than experienced by Blacks during the same period. By 2004-2005, disparities for Hispanics had gotten much worse. In the case of spending, the Hispanic-White gap almost doubled to US$1,819, nearly twice the Black-White spending difference.
Comparing the three definitions, we found that for most analyses measuring disparities at a point in time, the AHRQ unadjusted approach estimated the largest disparities, and the RDE measured the smallest disparities. For example, within both time periods, the RDE-based method found disparities in doctor visits approximately 40% less than the other two methods. Similarly, the AHRQ method measured the largest widening of Hispanic-White disparities over time whereas the RDE method estimated the smallest widening of disparities over time. All six estimates for the increase in disparities for Hispanics were statistically significant. The within-year estimates and the estimates of change in disparities, however, differed according to definition.
We applied our estimated models to address the question of how much of the change in disparities between 1996-1997 and 2004-2005 was due to changes in SES of minority groups. To do so, we used the IOM approach to measuring disparities. (The question of how much SES contributes to disparities trends does not make sense within the RDE approach, but it could be asked in the AHRQ definition.) Our method was similar in spirit to the adjustment for health status in the IOM definition. To check for the contribution of SES changes to disparities changes, we transformed the 2004-2005 minority distribution of SES variables to be the same as they were in 1996-1997. We used this doubly transformed model (health status like contemporaneous Whites and SES like 1996-1997 minority) to project minority utilization and compared with actual White utilization to refigure disparities. The difference in the change using this projection for 2004-2005 tells us the effect of SES changes between the two time periods on disparities.
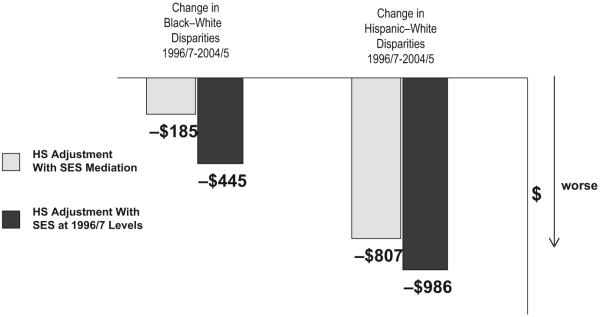
As shown in Table 4, recalculating 2004-2005 disparities after resetting Black SES to 1996-1997 values worsened Black-White disparity trends in having any doctor visit by 0.8% (0.7% to -0.1%) and expenditure by US$260 (from -US$185 to -US$445). Resetting Hispanic SES to 1996-1997 values had no effect on Hispanic-White disparities in having any doctor visit and increased expenditure disparities by US$178 (from -US$807 to -US$986). Figure 5 graphs the results for changes in disparities in medical expenditure, showing the estimated widening over time of disparities in total spending (-US$185 for Blacks and -US$807 for Hispanics) based on the IOM definition, and the even greater widening of disparities that would result if SES remained at 1996-1997 values (-US$445 for Blacks and -US$986 for Hispanics). Disparities would have grown more (gotten even worse) if SES improvements for Blacks and Hispanics had not occurred (see Table 1 for changes in education and income). Other factors, therefore, aside from SES changes, must be operating to lead to the constancy of Black-White disparities and the exacerbation of Hispanic-White disparities over this period.
Table 4. Comparing Health-Adjusted Black and Hispanic Disparity Trends for Any Doctor Visit and Total Expenditure With SES Differences as Mediator and SES Differences and Change in SES Differences as Mediatorsa.
| HS Adjustment With SES Mediationb |
HS Adjustment With SES at 1997 Levelsc |
|
|---|---|---|
| Black-White | ||
| Any doctor visit | ||
| 2004-2005 | -13.6% | -14.4% |
| 1996-1997 | -14.3% | -14.3% |
| Difference in disparity | 0.7% | -0.1% |
| Total medical expenditure (US$) | ||
| 2004-2005 | -1,053.52 | -1,313.15 |
| 1996-1997 | -868.50 | -867.68 |
| Difference in disparity | -185.03 | -445.47 |
| Hispanic-White | ||
| Any doctor visit | ||
| 2004-2005 | -19.8% | -19.9% |
| 1996-1997 | -16.4% | -16.5% |
| Difference in disparity | -3.4% | -3.4% |
| Total medical expenditure (US$) | ||
| 2004-2005 | -1,818.83 | -1,992.43 |
| 1996-1997 | -1,011.44 | -1,006.90 |
| Difference in disparity | -807.40 | -985.53 |
Note: HS = health status; SES = socioeconomic status.
Health status variables used in adjustment are age, sex, marital status, activity limitation, and self-reported health status.
SES mediation estimated from SES differences by race/ethnicity within each time period.
SES mediation estimated from SES differences gives no change in minority SES after 1997.
Figure 5. Assessing the Effect of SES Changes on Change in Medical Expenditure Disparities: 1996/1997 to 2004/2005.
Note: HS = health status; SES = socioeconomic status.
Discussion
According to three approaches to measuring disparities, Hispanic-White disparities for two broad indicators of health care use have grown over the period 1996-1997 to 2004-2005 while Black-White disparities have remained roughly constant.
While all three definitions of disparities tell the same basic story, we find important differences between the definitions in terms of the magnitudes of disparities and changes over time. Adjusting for differences in health status using the IOM method reduces the magnitude of Hispanic-White disparities compared to unadjusted trends. Further adjusting for SES, health insurance, and all other variables in the RDE method reduces the magnitude of Hispanic-White disparities even more and also reduces Black-White disparities.
The SES of Hispanics improved between 1996 and 2005 in a number of indicators. Disparities between Hispanics and Whites would have been slightly worse had these SES improvements not occurred, leaving open the question of why Hispanics are faring badly in comparison to Whites.
Hispanics experience continuing high levels of uninsurance and underinsurance (Alegria et al., 2007; Kaiser Commission on Medicaid and the Uninsured [KCMU], 2000, 2004), and continuing problems with access to care due to language and cultural barriers. These factors impede Hispanics’ access and may be having even a greater effect in more recent years. Also, increasing levels of immigration by Hispanic populations may contribute to increasing disparities in ways not captured by the SES variables in our model. The percentage of the U.S. population that was foreign born from Latin America increased 35% between 1996 and 2003 (4.6% to 6.2%, respectively; Hansen & Faber, 1997; Larsen, 2004). The foreign born are younger, more likely to live in poverty (Larsen, 2004), more likely to be uninsured (KCMU, 2004), and are likely to be disadvantaged in other ways as well.
The absence of improvement against disparities for Blacks and the worsening situation for Hispanics must be regarded as disheartening in light of the massive amount of research and policy attention devoted to disparities in the past 10 years. In broad terms, solutions for disparities could come from the eventual improvement of the SES of minorities in relation to Whites or from a reconfigured health care system that diminish the effect of SES on use in comparison to factors related to health status. Slight improvements in the relative SES of minorities have occurred over this time period, but progress on this front will inevitably be slow. For the measures examined in this analysis, we found no evidence that the health care system was becoming more responsive to health status in comparison to SES.
Trends analysis is limited by data. The 1996 and 1997 MEPS do not have health status data beyond age, sex, functional limitation, and self-reported health status. Beginning in 2000, the MEPS included more measures of health status. To assess the impact of this exclusion on the IOM and RDE estimates, we reestimated 2004-2005 predictions using SF-12, BMI, and 11 health condition measures. This sensitivity test did not significantly change IOM-based estimates or RDE-based estimates of any doctor visit, but it did slightly increase RDE-based estimates of Hispanic and Black medical expenditure. RDE-based medical expenditure disparities may therefore be overestimated within each time period. However, we expect, though cannot be certain, that RDE-based expenditure disparities would have similarly decreased in 1996-1997 given the same set of variables, thereby leaving disparity trends relatively unchanged. Precision of comparisons can improve over time as more years of data become available with more extensive measures of key variables.
Health insurers and government health care programs have recently begun to track disparities for the purpose of monitoring provider and system performance, and to identify interventions that improve the health and health care of minorities. For example, nine of the nation’s largest health insurers are collecting and analyzing data by race/ethnicity on the quality of diabetes care for the National Health Plan Collaborative to Reduce Disparities and Improve Quality in Diabetes Care (Center for Health Care Strategies, 2004). Measuring trends in disparities further increases in importance as pay for performance initiatives may tie provider payments to the reduction of racial disparities. The recently implemented Massachusetts health reform package mandating health insurance for all Massachusetts residents includes an initiative that would make hospital rate increases contingent on reducing health care disparities (State of Massachusetts, 2006).
Our article compares several approaches for measuring disparities and assesses trends in disparities. We compare what we regard to be current best practice—implementing the definition of disparity proposed by the IOM with a rigorous method of adjustment for health status—with an approach based on unadjusted means and an approach based on estimated race/ethnicity coefficients.
Empirical researchers studying disparities at a point in time or trends in disparities must choose a definition of disparity to employ in their work. We recognize that all three definitions have value, and our most fundamental recommendation is that the choice of definition be explicit.
From a practical standpoint, all three approaches are straightforward to implement. The AHRQ means-based definition is very easy. Once a researcher estimates an empirical model of health care use, the IOM and RDE definitions are within reach. We adjusted for health status in this article in an innovative way to come to the IOM measure, but there are other easier methods for approximating the mediating effect of SES and other variables in a nonlinear model of health care use, such as omitting these variables altogether from the model (Balsa, Cao, & McGuire, 2007). The important feature of the IOM definition is the counting of mediation for nonhealth status variables, not the method for quantifying the mediation.
Each definition calls attention to unfair differences in a distinct way, and the choice of definition to employ should be guided by the underlying objective of the investigation. We believe an unadjusted comparison of means is less informative about fairness and, therefore, less useful for policy. The coefficient-based RDE measure picks up racial/ethnic differences not due to other factors in the model; therefore, its interpretation across studies is fluid, depending on what else the researcher is able to measure and include. The RDE measure also runs the risk of implying an absence of racial/ethnic disparities if there is no significant race coefficient. A researcher focused on the causes of group differences and most interested in the effect of race as distinct from SES or other system factors may prefer the RDE approach.
When the goal of a study is to quantify disparities (or change in disparities), we believe the IOM approach is the right one. The definition of unfair differences—differences not due to health status or need—we believe, captures what most researchers and policy makers are concerned about. The IOM approach captures the reality that race and ethnicity matter in direct and in indirect ways affecting access to health care and that all of these are legitimate concerns about the way our health care system serves members of different groups.
Acknowledgments
This research was supported by grants P50 MHO 73469 and R03 MH82312 from the National Institute of Mental Health and P60 MD002261 from the National Center for Minority Health and Disparities. The views expressed in this article are those of the authors, and no official endorsement by the Agency for Healthcare Research and Quality or the US Department of Health and Human Services is intended or should be inferred.
Footnotes
Trends are assessed graphically in the 2004 National Healthcare Disparities Report (NHDR; Agency for Healthcare Research and Quality [AHRQ], 2004); The 2005 NHDR (AHRQ, 2005b) introduces formal tests of trends, measuring the significance (p < .05 is considered significant) of differences between the oldest available and most recent estimates.
For an earlier study using a similar methodology and disparity definition, see Weinick, Zuvekas, and Cohen (2000). This study compared data from the 1996 Medical Expenditure Panel Survey (MEPS) with its predecessor surveys conducted in 1977 and 1987.
The residual direct effect (RDE) is a modification of the use of predictive margins with complex survey data developed by Graubard and Korn (1999). See Cook, McGuire, Zaslavsky, and Meara (In press) for a more thorough conceptual and empirical comparison of the application of the RDE definition and the Institute of Medicine’s (IOM) definition.
The MEPS expenditure variables omit all payments not made at the patient level, including Medicaid Disproportionate Share and Medicare Direct Medical Education subsidies as well as uncollected liability, bad debt, and charitable care (unless provided by a public clinic or hospital). Thus, the expenditure variable may overstate disparities in real health care resource use to the extent that Blacks and Hispanics are more likely to receive services associated with these types of nonpatient-level payment or revenue flows. Our simulations suggest that even under the strongest assumptions about the extent of these flows and uncompensated care, the resulting bias is negligible. The expenditure measure is also based on prices, which vary by geographic area and insurance coverage, rather than real resource costs. It is not clear in which direction using prices that vary by geographic area might bias estimates of disparities in resource use. Variation in prices due to insurance coverage may introduce bias in the expenditure measure of disparities because the mix of health insurance coverage differs substantially by race and ethnicity. However, we believe this potential bias is small relative to the large differences observed for many different types of health care utilization.
An alternative counterfactual would give Blacks the White socioeconomic status (SES) and race and compare that counterfactual distribution with the actual Black distribution, with the difference being an IOM disparity.
See Cook et al. (In press) for more discussion and explicit analytical comparison with Oaxaca-Blinder as well as with propensity score-based methods for making these adjusted comparisons.
Contributor Information
Benjamin Lê Cook, Cambridge Health Alliance/Harvard Medical School, Somerville, MA.
Thomas G. McGuire, Harvard Medical School, Boston, MA
Samuel H. Zuvekas, Agency for Healthcare Research and Quality, Rockville, MD
References
- Agency for Healthcare Research and Quality . National healthcare disparities report, 2003. Author; Rockville, MD: 2003. [Google Scholar]
- Agency for Healthcare Research and Quality . National healthcare disparities report, 2004. Author; Rockville, MD: 2004. [Google Scholar]
- Agency for Healthcare Research and Quality . MEPS HC-036: 1996-2004 pooled estimation file. Author; Rockville, MD: 2005a. [Google Scholar]
- Agency for Healthcare Research and Quality . National healthcare disparities report, 2005. Author; Rockville, MD: 2005b. [Google Scholar]
- Agency for Healthcare Research and Quality . MEPS HC-036BRR: 1996-2004 replicates for calculating variances file. Author; Rockville, MD: 2006a. [Google Scholar]
- Agency for Healthcare Research and Quality . National healthcare disparities report, 2006. Author; Rockville, MD: 2006b. [Google Scholar]
- Agency for Healthcare Research and Quality . National healthcare disparities report, 2007. Author; Rockville, MD: 2007. [Google Scholar]
- Alegria M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of past-year mental health service use among Latinos: Results from the national Latino and Asian American study. American Journal of Public Health. 2007;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, et al. Racial and ethnic disparities in the use of health services: Bias, preferences, or poor communication? Journal of General Internal Medicine. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsa AI, Cao Z, McGuire TG. Does managed health care reduce health care disparities between minorities and Whites? Journal of Health Economics. 2007;27:101–121. doi: 10.1016/j.jhealeco.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bloche MG. Los Angeles Times. Feb 15, 2004. Erasing racial data erased report’s truth; p. M1. [Google Scholar]
- Braddock CH, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: Time to get back to basics. Journal of the American Medical Association. 1999;282:2313–2320. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- Center for Health Care Strategies . National health plan collaborative to reduce disparities and improve quality. Author; Hamilton, NJ: 2004. [DOI] [PubMed] [Google Scholar]
- Clancy CM. AHRQs national healthcare quality and disparities reports: Resources for health services researchers. Health Services Research. 2006;41:xiii–xix. doi: 10.1111/j.1475-6773.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL. Effect of Medicaid managed care on racial disparities in health care access. Health Services Research. 2007;42:124–145. doi: 10.1111/j.1475-6773.2006.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zaslavsky AM, Meara E. Adjusting for health status in nonlinear models of health care disparities. Health Services Outcomes & Research Methodology. doi: 10.1007/s10742-008-0039-6. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe NR, Jenckes MW, Gonzales JJ, Levine DM, Ford DE. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12:431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escarce JJ, Epstein KR, Colby DC, Schwartz JS. Racial differences in the elderly’s use of medical procedures and diagnostic tests. American Journal of Public Health. 1993;83:948–954. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escarce JJ, McGuire TG. Changes in racial differences in use of medical procedures and diagnostic tests among elderly persons: 1986-1997. American Journal of Public Health. 2004;94:1795–1799. doi: 10.2105/ajph.94.10.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care. 2002;40:52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Goldman D, Smith J. Socioeconomic differences in the adoption of new medical technologies. American Economic Review Papers and Proceedings. 2005;95:234–237. doi: 10.1257/000282805774669907. [DOI] [PubMed] [Google Scholar]
- Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries: 1989-2000. Medical Care. 2005;43:320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- Guevara JP, Mandell DS, Rostain AL, Zhao H, Hadley TR. Disparities in the reporting and treatment of health conditions in children: An analysis of the Medical Expenditure Panel Survey. Health Services Research. 2006;41:532–549. doi: 10.1111/j.1475-6773.2005.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen KA, Faber CS. The foreign-born population in the United States: 1997. U.S. Census Bureau; Washington, DC: 1997. [Google Scholar]
- Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Services Research. 2003;38:809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. New England Journal of Medicine. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured . Health insurance coverage in America: 1999 data update. Author; Washington, DC: 2000. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured . Health insurance coverage in America: 2003 data update. Author; Washington, DC: 2004. [Google Scholar]
- Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in health care. Medical Care. 2006;44:164–172. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- Klick J, Satel S. The health disparities myth. American Enterprise Institute; Washington, DC: 2006. [Google Scholar]
- Kraemer HC, Blasey CM. Centering in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2002;13:141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen LJ. The foreign-born population in the United States: 2004. U.S. Census Bureau; Washington, DC: 2004. [Google Scholar]
- McCullagh P, Nelder JA. Generalized linear models. Chapman & Hall; London: 1989. [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: An application to mental health care. Health Services Research. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy E, Dayton E, Clancy CM. Compiling the national healthcare disparities reports. Health Affairs. 2005;24:376–387. doi: 10.1377/hlthaff.24.2.376. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . Health, United States, 2005. With chartbook on trends in the health of Americans. Author; Hyattsville, MD: 2005. [PubMed] [Google Scholar]
- State of Massachusetts . House Bill No. 4850. 2006. [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. New England Journal of Medicine. 2005;353:692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy people 2010: Understanding and improving health. 2nd ed. Author; Washington, DC: 2000. [Google Scholar]
- Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. New England Journal of Medicine. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Medical Care Research and Review. 2000;57:36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- Wolter K. Introduction to variance estimation. Springer-Verlag; New York: 1985. [Google Scholar]
- Zuvekas SH, Taliaferro GS. Pathways to access: Health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Affairs. 2003;22:139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]