Abstract
Drug-induced liver injury is a significant and still unresolved clinical problem. Limitations to knowledge about the mechanisms of toxicity render incomplete the detection of hepatotoxic potential during preclinical development. Several xenobiotics are lipophilic substances and their transformation into hydrophilic compounds by the cytochrome P-450 system results in production of toxic metabolites. Aging, preexisting liver disease, enzyme induction or inhibition, genetic variances, local O2 supply and, above all, the intrinsic molecular properties of the drug may affect this process. Necrotic death follows antioxidant consumption and oxidation of intracellular proteins, which determine increased permeability of mitochondrial membranes, loss of potential, decreased ATP synthesis, inhibition of Ca2+-dependent ATPase, reduced capability to sequester Ca2+ within mitochondria, and membrane bleb formation. Conversely, activation of nucleases and energetic participation of mitochondria are the main intracellular mechanisms that lead to apoptosis. Non-parenchymal hepatic cells are inducers of hepatocellular injury and targets for damage. Activation of the immune system promotes idiosyncratic reactions that result in hepatic necrosis or cholestasis, in which different HLA genotypes might play a major role. This review focuses on current knowledge of the mechanisms of drug-induced liver injury and recent advances on newly discovered mechanisms of liver damage. Future perspectives including new frontiers for research are discussed.
Keywords: Adverse effects, Apoptosis, Drug toxicity, Liver diseases, Microsomes, Mitochondria, Necrosis
INTRODUCTION
Drug-induced liver injury is the leading cause of acute liver failure and transplantation in western countries. The detection of subtle mechanisms that lead to potential drug hepatotoxicity is of key importance and remains a major challenge in clinical practice.
The frequent involvement of the liver in drug-induced toxicity depends on its anatomical location (the liver is the primary port of entry for ingested drugs) and its physiological and biochemical functions because of the abundance of metabolizing enzymes.
The spectrum of injury secondary to drug reaction ranges from mild damage to massive hepatic destruction. However, if one considers the large consumption of drugs, the latter possibility is rather infrequent[1]. While direct toxic damage is dose-dependent, predictable and experimentally reproducible, idiosyncratic damage is rather supported by the innate and the adaptive immune system. With few exceptions of intrinsic hepatotoxicity, most cases of drug-induced liver injury are idiosyncratic. Toxicity can be experimentally tested by administering the compound at increasing doses, in the presence of metabolic inducers or inhibitors or toxicity enhancers, with depletion of protective systems, or by co-administering the drug with a known toxic compound. In general, in vitro tests precede in vivo experiments. Intracellular organelles and their functions are often the primary targets of hepatotoxicity[2]. Not only hepatocytes, but also cholangiocytes, Kupffer cells, Ito cells and sinusoidal endothelial cells can be involved in the process of drug-induced hepatotoxicity. Some drugs can induce cholestasis by impairing bile secretion or by causing obstruction of extrahepatic bile ducts[3].
This review deals with the main mechanisms associated with drug-induced hepatic injury, by discussing current views on intra- and extracellular mechanisms of damage and cell death with respect to different drugs. Future perspectives on emerging problems, namely liver steatosis and genetic polymorphisms, are also discussed.
RISK FACTORS
As toxicity is exerted mostly through metabolites rather than the parent drugs, factors affecting metabolite formation are of key importance. Accordingly, genetic polymorphisms and environmental influences on metabolizing enzymes play an important role. Of note, drug-induced hepatotoxicity occurs mainly in women[4], and this points to the existence of hormonal conditioning factors. Additional genetic, metabolic and immunological factors also may have a role in idiosyncratic hepatotoxicity. All such mechanisms can occur if specific metabolic pathways are activated and previous exposure has sensitized the organ with the formation of specific antibodies (e.g. halothane). In addition, the intrinsic toxicity of some molecules can depend on the expression of genetic variants, as occurs for paracetamol[5]. Although preexisting liver disease generally is believed to play a minor role as a risk factor for hepatotoxicity, there are some well-documented exceptions. Hepatotoxicity caused by isoniazid, for example, is more common among patients with viral hepatitis and/or human immunodeficiency virus (HIV) infection[6]. Patients undergoing antiretroviral treatment for HIV infection are at higher risk for severe hepatotoxicity when co-infected with hepatitis B or C viruses, particularly if therapy includes protease inhibitors[7]. Fatty liver is another condition that is particularly prone to stress damage[8]. Further studies are needed urgently in this respect, linking toxic injury to liver steatosis, which is becoming an emerging health problem, because of the increasing epidemic of obesity and diabetes as part of the metabolic syndrome[9].
GENERAL MECHANISMS OF DAMAGE
Although major pathways leading to drug-induced liver injury include necrosis and/or apoptosis, a net distinction between these two processes is sometimes difficult and both events often coexist in the same microscopic field[10]. Several factors may influence the hepatocyte response to a toxic insult and the extent of damage results from the intervention of intrinsic and extrinsic cell factors. A combination of age, sex, genetics, hormones, cell energetic status, underlying liver disease, environmental factors, and local O2 supply, strongly contributes to the expression of cell death mediators[11]. Less frequently, hepatocyte injury follows on from vascular damage as a consequence of the occlusion of the centrilobular vein (i.e. azathioprine, estrogens, progesterone, pyrrolidine alkaloids). Generally, hepatocytes react to toxic aggression by activating defense mechanisms that include hypertrophy of the endoplasmic reticulum, induction of protective systems (glutathione, GSH), and synthesis of heat shock and acute phase proteins.
Apoptosis and necrosis initially may follow common metabolic pathways. When the injury affects the maintenance of functional cell programs, hepatocytes preferentially die via apoptosis, thus limiting the extent of the injury. Necrotic damage generally begins at the cytoplasmic level and thus involves mitochondria and the nucleus in determining swelling and loss of plasma membrane integrity. It becomes irreversible when cytosolic Ca2+ concentration increases[12,13] for increased release by mitochondria and endoplasmic reticulum, or increased extracellular influx. Apoptosis determines cytoplasmic and nuclear condensation and fragmentation without loss of membrane integrity. Drug-induced apoptosis is generally spotty, whereas necrosis is zonal.
The mechanisms of damage include interference with hepatic transport proteins (i.e. organic anion transporting polypeptides), bile salt export pump, or with the nuclear receptor-mediated regulation of drug metabolism and transport[14,15].
MECHANISMS OF CELL DEATH
Hepatocyte death typically follows an apoptotic or necrotic pathway[16], mainly depending on predisposing factors[10]. General mechanisms of hepatotoxicity include reactive metabolite formation, antioxidant depletion, and protein alkylation. Intracellularly generated signaling can activate B-cell CLL/lymphoma 2 (Bcl-2) family members (Bax and Bid) which form pores in the outer mitochondrial membrane. This condition favors the release of intramembrane proteins and promotes chromatin condensation and DNA fragmentation. Alternatively, mitochondrial dysfunction, through reactive oxygen species (ROS) delivery and peroxynitrite formation, triggers membrane permeability transition and leads to membrane potential collapse with decrease of energy production and release of nucleases[17].
Apoptosis
Apoptosis results from an ATP-dependent death program that is characterized by activation of specific pathways involving death ligands and death receptors (e.g. Fas ligand with Fas) with activation of the caspase cascade (Figure 1). There are two different activating pathways of drug-induced hepatocyte apoptosis. The “intrinsic way” is triggered by intracellular signals scattered directly by the drug or its metabolites, with activation of a cascade of reactions that damage nuclear and/or mitochondrial DNA directly. Single-stranded DNA subsequently will stimulate intracellular sensor systems and induce the expression of the effector p53. In the “extrinsic way”, new surface antigens on hepatocyte membranes work as receptors. The interaction with ligands, such as tumor necrosis factor alpha (TNF-α) or Fas, activates cytotoxic T cells and liver non-parenchymal cells, with release of cytokines[18] that engage death receptors on the cell surface[19]. After binding, the receptor trimerizes and leads to a clustering of death domains. Intrinsic and extrinsic ways finally promote the activation of interleukin (IL)-1β converting enzyme, which activates caspases and nucleases.
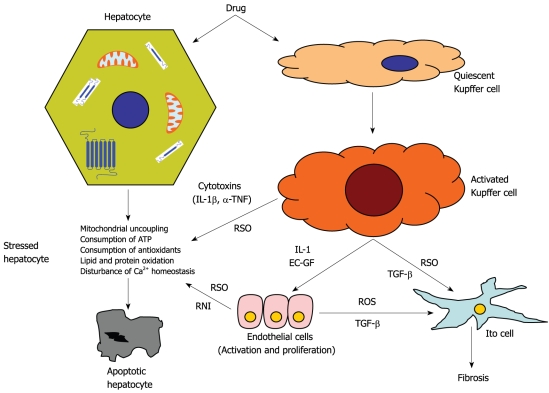
Figure 1.
Schematic representation of subtoxic damage of hepatocyte in response to moderate dose of drug. Drug molecule activates Kupffer cells is metabolically processed by hepatocytes. These events may result in hepatocyte stress which is worsened by the intervention of reactive oxygen species (ROS) and nitrogen species from activated endothelial cells. Final result is apoptotic death and Ito cells activation with promotion of fibrosis. EC-GF: Endothelial cell growth factor; IL1: Interleukin 1; IL1β: Interleukin 1β; RNI: Reactive nitrogen intermediates; ROS: Reactive oxygen species; TGF-β: Transforming growth factor β; TNF: Tumor necrosis factor α.
Generally, hepatocytes are resistant to TNF-α-induced cytotoxicity[20]. In fact, under normal conditions, the activation of membrane receptors stimulates the synthesis of anti-apoptotic molecules and enzymes (e.g. Bcl-2, NO synthase), mediated by the intervention of the nuclear transduction factor nuclear factor-κB (NF-κB). Therefore, increased cell sensitivity to TNF-α or to other specific ligands is required to trigger subsequent events[21]: a strong signaling response with activation of the executioner caspases[22], and the involvement of mitochondria to amplify death mechanisms in the presence of a poor caspase activation[23].
Necrosis
Drug-induced cell necrosis results from an intense and massive perturbation of cell homeostasis, with ATP depletion (Figure 2) associated with cytoskeletal alterations, cellular swelling and bleb formation[16]. The next steps include lysosomal breakdown, bleb rupture, and irreversible collapse of electrical and ion gradients.
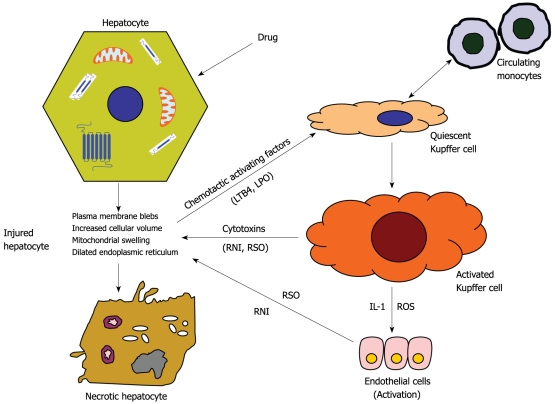
Figure 2.
Schematic representation of toxic damage of hepatocyte in response to high dose of drug. High drug amount is processed by hepatocytes with production of reactive metabolites which induce cell injury. Toxic products and chemotactic factors released by damaged hepatocytes stimulate the activation of Kupffer and endothelial cells with a subsequent delivery of reactive oxygen (ROS) and nitrogen species. The intracellular damages result in necrotic death. LPO: Lipid peroxidation; LTB4: Leukotriene B4.
When a high amount of toxicant reaches the liver, necrosis occurs because of dramatic intracellular alterations, or as a consequence of oxygen and nitrogen radical attack from activated Kupffer and endothelial cells[24]. On this occasion, drugs are oxidized by the cytochrome P-450 (CYP-450) enzymes, with release of a large amount of reactive metabolites, with promotion of lipid and protein oxidation and depletion of GSH. Oxidized proteins and protein adducts may have immunogenic properties and activate Kupffer and polymorphonuclear cells, with subsequent release of ROS. The formation of protein disulfides results in increased permeability of the inner mitochondrial membrane, with loss of membrane potential, decrease of ATP synthesis, inhibition of Ca2+-dependent ATPase, decreased capability to sequester Ca2+, oxidation of actin, microfilament breakage, and membrane bleb formation[25].
Abnormal control of cell volume is a major factor that promotes hepatocyte necrosis. Oxidative stress, very fast consumption of cellular energy, and mitochondrial dysfunction activate anaerobic glycolysis, which results in decreased intracellular pH. The incoming acidosis is contrasted partially by H+/Na+ and Na+/HCO3- exchanges with influx of Na+. As a result of low ATP availability, Na+ cannot be further exchanged and accumulates within the cell. The consequent osmotic load results in cell swelling and blocks the apoptotic process, which requires a reduction of the cell volume. This osmotic stress is worsened by the increase of cytosolic Ca2+ and results in plasma membrane rupture[26].
Additional mechanisms include nucleotide alterations and protein synthesis disruption. In most cases, these actions follow drug-induced mitochondrial injury. However, discriminatory nucleotide alterations and oxidation of protein sulfhydryls (γ-glutamyl synthetase and glucose 6-phosphate dehydrogenase) are promoted selectively by some drugs; one example is the damage to the ATPase complex observed after cisplatin intoxication[27].
CELLULAR AND INTRACELLULAR TARGETS OF DRUG HEPATOCELLULAR INJURY
Aspects to discuss include non-parenchymal hepatic cells, microsomes, mitochondria, and nuclear receptors. Much evidence suggests the participation of non-parenchymal hepatic cells in drug-induced hepatocellular injury[28], which depends on factors such as the intrinsic characteristics of the drug, its dose, its metabolites, and the local O2 supply[29]. Activation of Kupffer cells results in the release of inflammatory mediators and ROS, and modulates hepatocyte injury[30]. It has been shown that inhibition of macrophage activation or administration of TNF-α antagonists protects hepatocytes against paracetamol toxicity[31], and that depletion of Kupffer cells attenuates thioacetamide hepatotoxicity[32]. Indeed, both Kupffer and endothelial cells can be activated secondarily by chemotactic factors (i.e. leukotriene B4) released by injured hepatocytes[24,33], which in turn, can be damaged by TNF-α and IL-1β released from activated non-parenchymal cells. Examples of drug hepatotoxicity that involves non-parenchymal cells are that seen with methotrexate (activation of hepatic stellate cells to myofibroblasts, and liver fibrosis may develop even in the absence of liver enzyme elevation); bosentan (inhibition of transport proteins including the bile salt export pump[34]); sulindac (competitive inhibition of canalicular bile salt transport, a contributing factor to cholestatic liver injury[35]); cyclophosphamide and azathioprine (sinusoidal obstruction syndrome, veno-occlusive disease, follows a severe depletion of GSH in sinusoidal endothelial cells. This damage results in fibrosis of the hepatic sinusoids).
Microsomes are another target of hepatocellular damage induced by drugs. Biotransformation of lipophilic drugs via CYP-450 metabolic pass and the subsequent excretion of their metabolites are essential to avoid intracellular accumulation of toxic compounds. Less than 10 CYP-450 enzymes accounts for > 90% of all drug oxidation. Most adverse drug reactions depend on the release of reactive metabolites and ROS, which may overwhelm lethal insult, sensitize the innate immune system, or haptenize, thus eliciting immunoallergic reactions[36]. If metabolites have a particularly high reactivity, they can even bind and inactivate the metabolic enzymes[37]. This occurs with drugs that show a narrow therapeutic index (e.g. terfenadine and astemizole). Several factors may affect the efficiency of the microsomal metabolism: namely aging, liver disease, enzyme induction and inhibition, genetics (existence of slow and fast acetylators), and O2 supply. Changes in the level of CYPs may have a dramatic impact on drug metabolism. P-450 enzymes are subjected to multiple levels of regulation and expression; the latter being dominant in zone 3 just surrounding the centrilobular vein. Expression of P-450 isoforms varies with age; therefore, the capacity for drug metabolism is a function of age[38,39]. Polymorphisms in P-450s or induction/inhibition account for the appearance of adverse reactions. In this regard, it has been noted that the constitutive androstane receptor (CAR) binds drugs and regulates the expression of the genes that code for CYP3A and CYP2B[40]. Also, induction or inhibition of CYPs by herbal remedies accounts for the increasing number of case reports of hepatotoxicity[41]. In fact, some herbal components are converted to toxic metabolites by P-450 enzymes; this is the case of aristolochis acid, which generates the highly reactive cyclic nitrenium ions[42]. Upregulation of specific P-450 enzymes has been described during rifampicin treatment[43] in experimental models of obesity and fatty liver[44] and in humans with nonalcoholic fatty liver disease (NAFLD)[45].
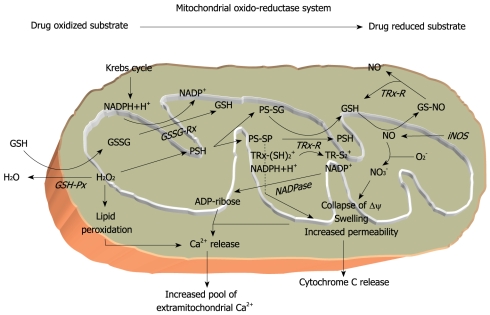
Mitochondria are often a major target of drug toxicity, and therefore mitochondrial dysfunction represents a major determinant of hepatotoxicity[46,47] (Figure 3). Indeed, mitochondria are the gateway at which signals that initiate cell death converge[3,48]. By integrating signaling networks, mitochondria have an active role in several metabolic pathways[49]. Signals may damage mitochondria directly or act indirectly by activating death receptors. In particular, reactive metabolite formation, GSH depletion and protein alkylation are associated with mitochondrial dysfunction, and represent critical initiating events for drug-induced toxicity. Opening of pores in the outer mitochondrial membrane, release of proteins and cytochrome c, imbalance in intracellular Ca2+ homeostasis, and intracellular accumulation of Na+ are essential steps in hepatocyte death[17,50]. In this context, the maintenance of the mitochondrial GSH pool[21,51] is important to detoxify ROS and maintain the reduced status of membrane protein sulfhydryls, including the ATP synthase complex and the Ca2+-dependent ATPase. A fall of total cellular GSH below 15% (< 1 μmol/g) inevitably is associated with lethal cell damage by involving the mitochondrial stores[52,53]. Common events that lead to apoptosis and necrosis act through mitochondrial permeabilization and dysfunction. In particular, it seems that the number of mitochondria that undergo pore opening is associated with apoptosis or necrosis, according to ATP availability or deficiency[47]. Some drugs exert toxic effects on mitochondria only after their metabolic activation at the microsomal level (isoniazid/rifampicin), after inducing endoplasmic reticulum stress (paracetamol) or even lysosomal dysfunction. The study of these mechanisms has revealed intriguing relationships between mitochondria and other intracellular organelles[54-56].
Figure 3.
Schematic representation of mitochondrial oxido-reductase system. Several drug molecules directly or after metabolic release of toxic intermediates can cause mitochondrial alterations at different levels. The following impairment of the energetic and redox balance finally triggers apoptotic or necrotic processes according to a poor or sufficient ATP level. Important regulatory mechanisms rely on the glutathione dependent redox status of proteins. GSH: Reduced glutathione; GSSG: Oxidized glutathione; GSH-Px: Glutathione peroxidase; GSSG-RX: Glutathione reductase; iNOS: Inducible nitric oxide synthetase; NO: Nitric oxide; PSH: Protein sulphydrils; PS-SG: Protein mixed disulfides; PS-SP: Protein-protein disulfides; TRx: Thioredoxin; TRx-R: Thioredoxin reductase; TR-S2: Oxidized thioredoxin.
Recent advances in molecular biology have revealed that nuclear receptors such as the pregnane X receptor (PXR) and CAR act as intracellular sensors for lipophilic compounds by encoding proteins and regulating the expression of enzymes[57,58] that are involved in drug oxidative metabolism, disposition and transport[15]. Their incorrect activation may result in drug metabolism disturbance. PXR can be activated or inhibited by a variety of structurally different drugs. Its activation is associated with downregulation of several genes[59] that influence mitochondrial ketogenesis[60] and favor mitochondrial imbalance and hepatic steatosis[61]. These receptors also represent important drug targets. In fatty livers, peroxisome proliferator-activated receptor (PPAR) activation/deactivation is particularly important, not only for the switch from simple steatosis to steatohepatitis, but also for maintaining the efficiency of specific metabolic drug pathways[62]. PPARs and other oxidative stressors can be activated also by macrophage-released molecules (i.e. Stat-3 and NF-κB)[63]. The existence of single-nucleotide polymorphisms is associated in humans with drug transport alterations as a predisposing factor for drug-induced cholestasis[14].
COMMON PATHWAYS OF DRUG-INDUCED LIVER DAMAGE
Immune system
The liver is a site of intense immunological activity and represents a tolerogenic immune organ for lymphocytes. Activation of Kupffer cells, and recruitment of macrophages and immune cells result in inflammation and injury caused by cytokines release[64]. These events are major factors in initiating and maintaining drug-induced liver injury[65].
The drug itself and its metabolites can activate an immune response in the liver: the molecule is processed by antigen-presenting cells in the central lymphoid tissue directly, or after the appearance of haptens or new antigens on the hepatocyte membrane. The latter case follows a covalent binding of the drug molecule with membrane constituents or intracellular proteins[66]. This hypothesis is supported by the observation that neutrophil depletion protects against paracetamol toxicity[67]. Also, idiosyncratic reactions are more likely to occur in the presence of an inflammatory state[68]. Effectors are dendritic cells, which act by sensing pathogens and triggering adaptive immune responses. These responses are characterized by activation of B lymphocytes, which release immunoglobulins and kinines and activate the complement cascade, and of T lymphocytes, which produce lymphokines (CD4) or determine direct cytotoxicity (CD8) via surface-molecule expression and the release of mediators (e.g. perforin and granzyme)[69]. As a consequence, inhibition of lymphocyte activation reduces the extent of drug-induced hepatocyte injury[70].
The local O2 supply has an important role in the progression of immune-mediated toxic liver injury. For example, metabolism of halothane under the anaerobic conditions of the reductive pathway may result in mild hepatitis, whereas, in the presence of a high O2 supply, the oxidative pathway may induce massive liver necrosis[29]. These different effects may be explained by the higher immunogenicity of oxidized metabolites that form adducts with proteins. This example suggests the potential capacity of some drugs to trigger autoimmune hepatitis in some patients. In fact, statins, hydralazine and procainamide may trigger autoimmune reactions in predisposed patients[71]. Most of these patients are positive for HLA-DR3, 4 or 7, which are known to be associated with increased risk of autoimmunity. Halothane toxicity rarely occurs after first exposure; but antibodies against CYP 2E1-mediated trifluoroacetylated metabolite-protein adducts can be detected after frequent exposures to halothane.
Direct toxicity
Paracetamol hepatotoxicity is the classical example of direct liver injury. Given at recommended doses, paracetamol is generally safe, but its intrinsic toxicity at higher doses represents the most important cause of acute liver failure and transplantation. Predominantly metabolized by conjugation with sulfate and glucuronide (metabolites are excreted into bile by Mrp2 and extruded into blood through Mrp3), only a small amount is degraded by CYP 2E1 to the highly reactive metabolite N-acetyl-benzoquinoneimide (NAPQI). NAPQI is, in turn, detoxified by binding with GSH. If the amount of paracetamol that reaches the liver exceeds 12-15 g, the conjugating capacity is overwhelmed and the remaining unbound NAPQI covalently binds to cellular and mitochondrial proteins, which leads to cell necrotic death. In the presence of CYP 2E1 hypertrophy and/or decreased GSH availability (e.g. chronic alcoholism, malnutrition, and prolonged intake of barbiturates), NAPQI formation is increased even at therapeutic doses, and after overwhelming the GSH stores, it may cause severe liver injury[72,73].
Events start with disturbances of intracellular Ca2+ homeostasis, with an increase in cytosolic Ca2+ levels, Bax and Bid translocation into mitochondria, and mitochondrial oxidative changes with accumulation of oxidized GSH and peroxynitrite[74,75]. The latter induces membrane permeability transition, with collapse of mitochondrial membrane potential, inability to synthesize ATP, release of mitochondrial proteins with calpain activation, and release of cytochrome C and endonucleases. ATP deficiency prevents caspase activation but induces nuclear DNA damage, and activates intracellular proteases that lead to cell membrane rupture and hepatocyte necrosis[76,77]. These intracellular events explain the massive cell death and liver failure observed after paracetamol poisoning[17]. The recent observation that paracetamol toxicity is modulated by CAR gives rise to new concepts that are important for the general understanding of drug-induced liver injury[78]. Accordingly, the presence of gene polymorphisms may explain inter-individual differences in susceptibility to paracetamol toxicity. Finally, a role for hepatic non-parenchymal cells in paracetamol-induced hepatocellular injury also has been suggested. In fact, the chemical elimination of Kupffer cells by gadolinium chloride has been observed to reduce the extent of paracetamol-induced liver injury[31].
Direct toxicity of the liver is also induced by another drug, valproate, a branched medium-chain fatty acid with eight carbon atoms. Its chronic intake is associated with weight gain and it causes insulin resistance and NAFLD in 61% of treated patients[79]. Mechanisms of toxicity rely on mitochondrial β oxidation inhibition followed by the appearance of microvesicular steatosis[80]. Mitochondrial dysfunction follows the microsomal production of toxic metabolites (4-ene-valproate, 2,4-diene-valproate)[81], decreased activity of complex IV of the respiratory chain, and depletion of coenzyme A (CoA) and carnitine[80]. Preexisting mitochondrial impairment or deficiency of cofactors involved with valproate metabolism (e.g. carnitine) may represent risk factors for hepatotoxicity[82].
Idiosyncratic reactions
Unpredictable idiosyncratic reactions can follow the administration of virtually any drug. As a consequence, an enormous number of hepatic reactions have been registered for practically all drug classes. Several mechanisms have been elucidated, including TNF-α-induced apoptosis, inhibition of mitochondrial function, and neoantigen formation. Here, we report some of the most representative cases. Hepatotoxicity associated with the non-steroid anti-inflammatory drug (NSAID) nimesulide has led recently to its commercial withdrawal in some countries[83]. The mechanism is unknown, although liver histology has shown centrilobular and bridging necrosis[84]. Diclofenac potentially leads to zone 3 necrosis, autoimmune hepatitis, or even cholestasis[85] in predisposed individuals. The major pathway of diclofenac metabolism is through 40-hydroxylation by CYP 2C9[86]. Diclofenac also undergoes oxidative metabolism by CYP 2C8 to form reactive diclofenac acyl glucuronide and 5-hydroxydiclofenac[87]. Nucleophilic displacement can then replace the glucuronic acid moiety to form adducts with free cysteine thiols[88], and act as a potential hapten that triggers autoimmunity. Studies with diclofenac-protein conjugates have shown that diclofenac-treated hepatocytes carry antigens that are recognized by T-cell- and non-T-cell-enriched splenocytes[89]. As a consequence, changes in the activity of CYP 2C8, its haplotype distribution, or impairment in the clearance of acyl glucuronide may potentially increase the risk of hepatotoxicity. Polymorphisms, such as the presence of UGT2B7*2 allele, favor the development of diclofenac hepatotoxicity[90].
EXAMPLES OF LIVER DAMAGE INDUCED BY COMMONLY USED DRUGS
Aspirin induces hepatotoxicity that is different from that of other NSAIDs. Aspirin is hydrolyzed into salicylic acid, which is transformed actively by mitochondria into its salicyl-coenzyme A derivative. This compound indirectly inhibits the β oxidation of long-chain fatty acids and increases NADH availability, thus resulting in increased capacity of mitochondria to decarboxylate branched chain amino acids[91,92]. The negative effect on mitochondrial β oxidation probably is augmented by concomitant viral infection that affects mitochondrial function. This combination may determine microvesicular steatosis known as Reye’s syndrome[93].
Nefazodone, a triazolopyridine trazodone, an antidepressant drug, recently has been withdrawn from the market because of hepatotoxicity. Mechanisms include inhibition of mitochondrial respiratory complex I and IV, associated with accelerated glycolysis. This effect leads to mitochondrial membrane potential collapse, GSH depletion and oxidative stress[94].
Hepatotoxicity exerted by isoniazid, an anti-tuberculosis drug is related to its metabolite monoacetyl hydrazine, which is activated at the CYP-450 level and detoxified by N-acetyltransferase 2. These enzymes undergo genetic variability and environmental alterations; slow acetylator status and CYP 2E1 genetic polymorphism are risk factors for isoniazid hepatotoxicity[95,96]. Concomitant therapy with rifampicin, a CYP-450 inducer, significantly increases the risk of liver injury[56].
Amiodarone is a commonly used antiarrhythmic drug that consists of a benzofuran ring coupled with two iodine and diethyl-ethanolamine side chains substituted with a p-OH-benzene structure. Amiodarone accumulates within mitochondria and causes toxicity by inhibiting state 3 glutamate and palmitoyl-CoA oxidation and by decreasing mitochondrial respiration[55]. Electron transport chain complexes and β oxidation are also inhibited by amiodarone[96]. The chemical structure of benzarone resembles that of amiodarone. Benzarone, a non-halogenated benzbromarone derivative, is used for the treatment of vascular disorders. It decreases mitochondrial membrane potential, as well as state 3 oxidation and respiratory control ratio, uncouples oxidative phosphorylation, and inhibits β oxidation. Benzarone increases the production of ROS, as well as the leakage of cytochrome C, with final induction of mitochondrial permeability transition[97].
Troglitazone, a PPAR agonist, causes hepatocyte injury by dissipating the mitochondrial transmembrane potential, which favors superoxide generation, thioredoxin oxidation and activation of the kinase-1-dependent apoptosis signaling pathway[98].
HIV-1 protease inhibitors are essential components of antiretroviral therapy. However, mitochondrial toxicity represents a serious problem for patients taking antiretroviral drugs. It occurs most often with administration of a full dose of ritonavir and saquinavir[7]. Genetic HLA variants of the immune system seem to participate in the hepatotoxicity induced by abacavir, another antiretroviral drug. Co-infection with hepatitis viruses is known to increase the risk of mitochondrial toxicity induced by these nucleoside compounds[6].
CHOLESTASIS
Hepatic clearance of drugs depends on the activity of transport proteins that are located on the hepatocyte canalicular membrane. Alterations of these transporters by drugs or genetic polymorphisms increase the susceptibility to cholestatic injury[14]. As a consequence, cholestasis is one of the most important features of drug-induced hepatotoxicity[99]. Substrates for hepatic transport proteins include indomethacin, statins, digoxin, enalapril, midazolam, tamoxifen, diclofenac, methotrexate, and troglitazone. Selective inhibition of ATP-dependent bile salt transport proteins represents an additional mechanism of damage; therefore, co-administration of drugs at this level may enhance the risk of cholestasis. Examples are troglitazone plus lisinopril, itraconazole and verapamil, bosentan and glyburide[100,101]. Changes in the expression of drug transporters in conditions of chronic liver disease can also result in marked alterations in drug disposition[102]. Examples are increased bioavailability of drugs with high hepatic extraction, and decreased hepatic clearance of drugs with a low hepatic extraction and of those with biliary excretion[103]. Finally, cholangiocytes can also be damaged directly by drugs. Flucloxacillin, an isoxazolyl-penicillin, can cause cholestasis by injuring bile duct epithelial cells[104].
FUTURE PERSPECTIVES
Drug-induced liver injury occurs when the organ defense systems are overwhelmed. Preexisting conditions may contribute to the extent of damage. Two examples in this respect are the existence of fatty liver disease (liver steatosis), and genetic polymorphisms.
The mechanisms that favor high sensitivity of fatty liver to drug toxicity and necrotic cell death are depicted in Table 1. It is known that fatty liver has a reduced tolerance towards stress conditions, i.e. ischemia-reperfusion, prolonged fasting, and exposure to t-butyl-hydroperoxide[105,106]. Potential mechanisms that favor increased susceptibility of steatotic liver to drug-induced toxicity include mitochondrial imbalance[107], increased mitochondrial ROS production[108], and deficient repair capacity[109]. Indeed, a high incidence of hepatotoxicity has been observed in patients with type 2 diabetes[110], a condition that is associated inevitably with fatty liver[111]. Therefore, it is conceivable that hepatotoxic drugs might produce injury even at non-toxic doses in patients with fatty liver, although in a recent study[112], steatosis appeared to protect against paracetamol toxicity through preserving microcirculatory alterations. Defective hepatobiliary transport as well as the downregulation of Mrp2, as observed in rats with fatty liver, may represent additional predisposing factors for damage in these organs[113].
Table 1.
Mechanisms that favor high sensitivity of fatty liver to drug toxicity and necrotic cell death
| Initial change | Intermediate effects | Consequences |
| Increased bioactivation (microsomal CYP 450s) | Higher amount of toxic metabolites | Consumption of antioxidants |
| Increased release of ROS | Lipid peroxidation | |
| Mitochondrial dysfunction | Decreased energy production (ATP) and cytochrome c content | Over-expression of uncoupling protein 2 |
| Increased Ca2+ efflux | ||
| Increased release of ROS and NO derivatives | Protein oxidation and nitration | |
| Pores opening and increased membrane permeability | Expression of FAS ligands | |
| Calpain activation and protein cleavage | ||
| Impaired intracellular signaling and trafficking | Alterations of nuclear receptors and sensors | Defective transcription of repair mechanisms |
| Increased DNA fragmentation rate | ||
| Activation of non-parenchymal cells (Kupffer cells) and enzymes | Increased release of transforming growth factor-β1, p53, TNF-α | Inflammation and pro-oxidant attack |
| Increased NADPH oxidase activity |
ROS: Reactive oxygen species; TNF: Tumor necrosis factor.
Genetic polymorphisms are another important issue. Polymorphisms of CYP-450s account, at least in part, for the variability of efficacy and for the occurrence of adverse drug reactions, and may explain the variety of effects exerted by the same drug in different subjects. Genetic variations in the glutathione S-transferases (GSTT1 and GSTM1) have been associated with drug-induced hepatotoxicity[114]. Subjects who display mutations in some alleles that code for manganese superoxide dismutase have a higher risk of developing drug-induced liver injury[115]. Genetic mitochondrial abnormalities are a major determinant of the high susceptibility towards idiosyncratic liver injury caused by drugs that target mitochondria, especially in aged and female subjects[116]. Genetic polymorphisms associated with alteration of hepatobiliary transporters have implications in drug-induced cholestasis[14].
CONCLUSION
The search for the underlying mechanisms of damage is expected to lead to new intriguing perspectives for diagnosing and treating toxic liver injury. Today, certain microsomal and mitochondrial metabolic pathways can be assessed easily in vivo by performing breath tests with substrates that release CO2 during their metabolism. Methionine and α-ketoisocaproate breath tests assess mitochondrial functions and are altered after exposure to alcohol or drugs, thus reflecting specific metabolic alterations induced by exogenous compounds[92,117]. Such noninvasive diagnostic tools may guide evaluation of the effect of therapeutic strategies.
Future issues might include the use of cytokine and death receptor antagonists, strategies directed at factors that cause mitochondrial damage, and approaches that promote survival gene expression that may overcome drug-induced cell death. In this regard, toxicogenomics, a combination of toxicology and genomics, attempts to identify the effects of drugs on gene expression, and the role of genetic polymorphisms in drug-induced liver injury. However, although recent developments in genetics and toxicology have provided some new insights into drug hepatotoxicity, the complex interactions of hepatotoxins with genetic and environmental risk factors responsible for the onset of toxic injury have yet to be elucidated. Severe drug-induced liver diseases therefore remain unpredictable for most drugs. The identification of new risk factors and a better understanding of pathogenetic mechanisms will certainly have implications for health care and pharmaceutical developments in the near future.
Footnotes
Peer reviewer: Yukihiro Shimizu, MD, PhD, Kyoto Katsura Hospital, 17 Yamada-Hirao, Nishikyo, Kyoto 615-8256, Japan
S- Editor Li LF L- Editor Kerr C E- Editor Yin DH
References
- 1.Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:474–485. doi: 10.1056/NEJMra021844. [DOI] [PubMed] [Google Scholar]
- 2.Kaplowitz N. Biochemical and cellular mechanisms of toxic liver injury. Semin Liver Dis. 2002;22:137–144. doi: 10.1055/s-2002-30100. [DOI] [PubMed] [Google Scholar]
- 3.Kass GE. Mitochondrial involvement in drug-induced hepatic injury. Chem Biol Interact. 2006;163:145–159. doi: 10.1016/j.cbi.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Ostapowicz G, Fontana RJ, Schiødt FV, Larson A, Davern TJ, Han SH, McCashland TM, Shakil AO, Hay JE, Hynan L, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–954. doi: 10.7326/0003-4819-137-12-200212170-00007. [DOI] [PubMed] [Google Scholar]
- 5.Zhang J, Huang W, Chua SS, Wei P, Moore DD. Modulation of acetaminophen-induced hepatotoxicity by the xenobiotic receptor CAR. Science. 2002;298:422–424. doi: 10.1126/science.1073502. [DOI] [PubMed] [Google Scholar]
- 6.Kontorinis N, Dieterich D. Hepatotoxicity of antiretroviral therapy. AIDS Rev. 2003;5:36–43. [PubMed] [Google Scholar]
- 7.Sulkowski MS. Hepatotoxicity associated with antiretroviral therapy containing HIV-1 protease inhibitors. Semin Liver Dis. 2003;23:183–194. doi: 10.1055/s-2003-39949. [DOI] [PubMed] [Google Scholar]
- 8.Grattagliano I, Vendemiale G, Caraceni P, Domenicali M, Nardo B, Cavallari A, Trevisani F, Bernardi M, Altomare E. Starvation impairs antioxidant defense in fatty livers of rats fed a choline-deficient diet. J Nutr. 2000;130:2131–2136. doi: 10.1093/jn/130.9.2131. [DOI] [PubMed] [Google Scholar]
- 9.Clark JM, Diehl AM. Hepatic steatosis and type 2 diabetes mellitus. Curr Diab Rep. 2002;2:210–215. doi: 10.1007/s11892-002-0085-3. [DOI] [PubMed] [Google Scholar]
- 10.Farber E. Programmed cell death: necrosis versus apoptosis. Mod Pathol. 1994;7:605–609. [PubMed] [Google Scholar]
- 11.Pessayre D, Larrey D. Acute and chronic drug-induced hepatitis. Baillieres Clin Gastroenterol. 1988;2:385–422. doi: 10.1016/0950-3528(88)90009-7. [DOI] [PubMed] [Google Scholar]
- 12.Carini R, Autelli R, Bellomo G, Albano E. Alterations of cell volume regulation in the development of hepatocyte necrosis. Exp Cell Res. 1999;248:280–293. doi: 10.1006/excr.1999.4408. [DOI] [PubMed] [Google Scholar]
- 13.Lauterburg BH. Early disturbance of calcium translocation across the plasma membrane in toxic liver injury. Hepatology. 1987;7:1179–1183. doi: 10.1002/hep.1840070602. [DOI] [PubMed] [Google Scholar]
- 14.Bohan A, Boyer JL. Mechanisms of hepatic transport of drugs: implications for cholestatic drug reactions. Semin Liver Dis. 2002;22:123–136. doi: 10.1055/s-2002-30099. [DOI] [PubMed] [Google Scholar]
- 15.Liddle C, Goodwin B. Regulation of hepatic drug metabolism: role of the nuclear receptors PXR and CAR. Semin Liver Dis. 2002;22:115–122. doi: 10.1055/s-2002-30098. [DOI] [PubMed] [Google Scholar]
- 16.Malhi H, Gores GJ, Lemasters JJ. Apoptosis and necrosis in the liver: a tale of two deaths? Hepatology. 2006;43:S31–S44. doi: 10.1002/hep.21062. [DOI] [PubMed] [Google Scholar]
- 17.Jaeschke H, Bajt ML. Intracellular signaling mechanisms of acetaminophen-induced liver cell death. Toxicol Sci. 2006;89:31–41. doi: 10.1093/toxsci/kfi336. [DOI] [PubMed] [Google Scholar]
- 18.Scaffidi C, Fulda S, Srinivasan A, Friesen C, Li F, Tomaselli KJ, Debatin KM, Krammer PH, Peter ME. Two CD95 (APO-1/Fas) signaling pathways. EMBO J. 1998;17:1675–1687. doi: 10.1093/emboj/17.6.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Latta M, Künstle G, Leist M, Wendel A. Metabolic depletion of ATP by fructose inversely controls CD95- and tumor necrosis factor receptor 1-mediated hepatic apoptosis. J Exp Med. 2000;191:1975–1985. doi: 10.1084/jem.191.11.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatano E, Bennett BL, Manning AM, Qian T, Lemasters JJ, Brenner DA. NF-kappaB stimulates inducible nitric oxide synthase to protect mouse hepatocytes from TNF-alpha- and Fas-mediated apoptosis. Gastroenterology. 2001;120:1251–1262. doi: 10.1053/gast.2001.23239. [DOI] [PubMed] [Google Scholar]
- 21.Colell A, García-Ruiz C, Miranda M, Ardite E, Marí M, Morales A, Corrales F, Kaplowitz N, Fernández-Checa JC. Selective glutathione depletion of mitochondria by ethanol sensitizes hepatocytes to tumor necrosis factor. Gastroenterology. 1998;115:1541–1551. doi: 10.1016/s0016-5085(98)70034-4. [DOI] [PubMed] [Google Scholar]
- 22.Hampton MB, Orrenius S. Dual regulation of caspase activity by hydrogen peroxide: implications for apoptosis. FEBS Lett. 1997;414:552–556. doi: 10.1016/s0014-5793(97)01068-5. [DOI] [PubMed] [Google Scholar]
- 23.Lemasters JJ, Qian T, Bradham CA, Brenner DA, Cascio WE, Trost LC, Nishimura Y, Nieminen AL, Herman B. Mitochondrial dysfunction in the pathogenesis of necrotic and apoptotic cell death. J Bioenerg Biomembr. 1999;31:305–319. doi: 10.1023/a:1005419617371. [DOI] [PubMed] [Google Scholar]
- 24.Li J, Billiar TR. Nitric Oxide. IV. Determinants of nitric oxide protection and toxicity in liver. Am J Physiol. 1999;276:G1069–G1073. doi: 10.1152/ajpgi.1999.276.5.G1069. [DOI] [PubMed] [Google Scholar]
- 25.Vendemiale G, Grattagliano I, Altomare E, Turturro N, Guerrieri F. Effect of acetaminophen administration on hepatic glutathione compartmentation and mitochondrial energy metabolism in the rat. Biochem Pharmacol. 1996;52:1147–1154. doi: 10.1016/0006-2952(96)00414-5. [DOI] [PubMed] [Google Scholar]
- 26.Barros LF, Stutzin A, Calixto A, Catalán M, Castro J, Hetz C, Hermosilla T. Nonselective cation channels as effectors of free radical-induced rat liver cell necrosis. Hepatology. 2001;33:114–122. doi: 10.1053/jhep.2001.20530. [DOI] [PubMed] [Google Scholar]
- 27.Anderson ME, Naganuma A, Meister A. Protection against cisplatin toxicity by administration of glutathione ester. FASEB J. 1990;4:3251–3255. doi: 10.1096/fasebj.4.14.2227215. [DOI] [PubMed] [Google Scholar]
- 28.Laskin DL. Nonparenchymal cells and hepatotoxicity. Semin Liver Dis. 1990;10:293–304. doi: 10.1055/s-2008-1040485. [DOI] [PubMed] [Google Scholar]
- 29.Gut J, Christen U, Huwyler J. Mechanisms of halothane toxicity: novel insights. Pharmacol Ther. 1993;58:133–155. doi: 10.1016/0163-7258(93)90047-h. [DOI] [PubMed] [Google Scholar]
- 30.Roberts RA, Ganey PE, Ju C, Kamendulis LM, Rusyn I, Klaunig JE. Role of the Kupffer cell in mediating hepatic toxicity and carcinogenesis. Toxicol Sci. 2007;96:2–15. doi: 10.1093/toxsci/kfl173. [DOI] [PubMed] [Google Scholar]
- 31.Laskin DL, Gardner CR, Price VF, Jollow DJ. Modulation of macrophage functioning abrogates the acute hepatotoxicity of acetaminophen. Hepatology. 1995;21:1045–1050. [PubMed] [Google Scholar]
- 32.Andrés D, Sánchez-Reus I, Bautista M, Cascales M. Depletion of Kupffer cell function by gadolinium chloride attenuates thioacetamide-induced hepatotoxicity. Expression of metallothionein and HSP70. Biochem Pharmacol. 2003;66:917–926. doi: 10.1016/s0006-2952(03)00443-x. [DOI] [PubMed] [Google Scholar]
- 33.Laskin DL, Pendino KJ. Macrophages and inflammatory mediators in tissue injury. Annu Rev Pharmacol Toxicol. 1995;35:655–677. doi: 10.1146/annurev.pa.35.040195.003255. [DOI] [PubMed] [Google Scholar]
- 34.Mano Y, Usui T, Kamimura H. Effects of bosentan, an endothelin receptor antagonist, on bile salt export pump and multidrug resistance-associated protein 2. Biopharm Drug Dispos. 2007;28:13–18. doi: 10.1002/bdd.527. [DOI] [PubMed] [Google Scholar]
- 35.Bolder U, Trang NV, Hagey LR, Schteingart CD, Ton-Nu HT, Cerrè C, Elferink RP, Hofmann AF. Sulindac is excreted into bile by a canalicular bile salt pump and undergoes a cholehepatic circulation in rats. Gastroenterology. 1999;117:962–971. doi: 10.1016/s0016-5085(99)70356-2. [DOI] [PubMed] [Google Scholar]
- 36.Kassahun K, Pearson PG, Tang W, McIntosh I, Leung K, Elmore C, Dean D, Wang R, Doss G, Baillie TA. Studies on the metabolism of troglitazone to reactive intermediates in vitro and in vivo. Evidence for novel biotransformation pathways involving quinone methide formation and thiazolidinedione ring scission. Chem Res Toxicol. 2001;14:62–70. doi: 10.1021/tx000180q. [DOI] [PubMed] [Google Scholar]
- 37.Masubuchi Y, Horie T. Toxicological significance of mechanism-based inactivation of cytochrome p450 enzymes by drugs. Crit Rev Toxicol. 2007;37:389–412. doi: 10.1080/10408440701215233. [DOI] [PubMed] [Google Scholar]
- 38.Schuetz JD, Beach DL, Guzelian PS. Selective expression of cytochrome P450 CYP3A mRNAs in embryonic and adult human liver. Pharmacogenetics. 1994;4:11–20. doi: 10.1097/00008571-199402000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Egger SS, Rätz Bravo AE, Hess L, Schlienger RG, Krähenbühl S. Age-related differences in the prevalence of potential drug-drug interactions in ambulatory dyslipidaemic patients treated with statins. Drugs Aging. 2007;24:429–440. doi: 10.2165/00002512-200724050-00006. [DOI] [PubMed] [Google Scholar]
- 40.Kawamoto T, Sueyoshi T, Zelko I, Moore R, Washburn K, Negishi M. Phenobarbital-responsive nuclear translocation of the receptor CAR in induction of the CYP2B gene. Mol Cell Biol. 1999;19:6318–6322. doi: 10.1128/mcb.19.9.6318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Russmann S, Barguil Y, Cabalion P, Kritsanida M, Duhet D, Lauterburg BH. Hepatic injury due to traditional aqueous extracts of kava root in New Caledonia. Eur J Gastroenterol Hepatol. 2003;15:1033–1036. doi: 10.1097/00042737-200309000-00015. [DOI] [PubMed] [Google Scholar]
- 42.Zhou SF, Xue CC, Yu XQ, Wang G. Metabolic activation of herbal and dietary constituents and its clinical and toxicological implications: an update. Curr Drug Metab. 2007;8:526–553. doi: 10.2174/138920007781368863. [DOI] [PubMed] [Google Scholar]
- 43.Upadhyay G, Kumar A, Singh MP. Effect of silymarin on pyrogallol- and rifampicin-induced hepatotoxicity in mouse. Eur J Pharmacol. 2007;565:190–201. doi: 10.1016/j.ejphar.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Salazar DE, Sorge CL, Corcoran GB. Obesity as a risk factor for drug-induced organ injury. VI. Increased hepatic P450 concentration and microsomal ethanol oxidizing activity in the obese overfed rat. Biochem Biophys Res Commun. 1988;157:315–320. doi: 10.1016/s0006-291x(88)80049-4. [DOI] [PubMed] [Google Scholar]
- 45.Portincasa P, Grattagliano I, Lauterburg BH, Palmieri VO, Palasciano G, Stellaard F. Liver breath tests non-invasively predict higher stages of non-alcoholic steatohepatitis. Clin Sci (Lond) 2006;111:135–143. doi: 10.1042/CS20050346. [DOI] [PubMed] [Google Scholar]
- 46.Krähenbühl S. Mitochondria: important target for drug toxicity? J Hepatol. 2001;34:334–336. doi: 10.1016/s0168-8278(00)00106-9. [DOI] [PubMed] [Google Scholar]
- 47.Pessayre D, Mansouri A, Haouzi D, Fromenty B. Hepatotoxicity due to mitochondrial dysfunction. Cell Biol Toxicol. 1999;15:367–373. doi: 10.1023/a:1007649815992. [DOI] [PubMed] [Google Scholar]
- 48.Susin SA, Zamzami N, Kroemer G. Mitochondria as regulators of apoptosis: doubt no more. Biochim Biophys Acta. 1998;1366:151–165. doi: 10.1016/s0005-2728(98)00110-8. [DOI] [PubMed] [Google Scholar]
- 49.Kass GE, Price SC. Role of mitochondria in drug-induced cholestatic injury. Clin Liver Dis. 2008;12:27–51, vii. doi: 10.1016/j.cld.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 50.Miller TJ, Knapton A, Adeyemo O, Noory L, Weaver J, Hanig JP. Cytochrome c: a non-invasive biomarker of drug-induced liver injury. J Appl Toxicol. 2008;28:815–828. doi: 10.1002/jat.1347. [DOI] [PubMed] [Google Scholar]
- 51.Haouzi D, Lekehal M, Tinel M, Vadrot N, Caussanel L, Lettéron P, Moreau A, Feldmann G, Fau D, Pessayre D. Prolonged, but not acute, glutathione depletion promotes Fas-mediated mitochondrial permeability transition and apoptosis in mice. Hepatology. 2001;33:1181–1188. doi: 10.1053/jhep.2001.24235. [DOI] [PubMed] [Google Scholar]
- 52.Colell A, García-Ruiz C, Morales A, Ballesta A, Ookhtens M, Rodés J, Kaplowitz N, Fernández-Checa JC. Transport of reduced glutathione in hepatic mitochondria and mitoplasts from ethanol-treated rats: effect of membrane physical properties and S-adenosyl-L-methionine. Hepatology. 1997;26:699–708. doi: 10.1002/hep.510260323. [DOI] [PubMed] [Google Scholar]
- 53.Lauterburg BH, Mitchell JR. Toxic doses of acetaminophen suppress hepatic glutathione synthesis in rats. Hepatology. 1982;2:8–12. doi: 10.1002/hep.1840020103. [DOI] [PubMed] [Google Scholar]
- 54.Macanas-Pirard P, Yaacob NS, Lee PC, Holder JC, Hinton RH, Kass GE. Glycogen synthase kinase-3 mediates acetaminophen-induced apoptosis in human hepatoma cells. J Pharmacol Exp Ther. 2005;313:780–789. doi: 10.1124/jpet.104.081364. [DOI] [PubMed] [Google Scholar]
- 55.Berson A, De Beco V, Lettéron P, Robin MA, Moreau C, El Kahwaji J, Verthier N, Feldmann G, Fromenty B, Pessayre D. Steatohepatitis-inducing drugs cause mitochondrial dysfunction and lipid peroxidation in rat hepatocytes. Gastroenterology. 1998;114:764–774. doi: 10.1016/s0016-5085(98)70590-6. [DOI] [PubMed] [Google Scholar]
- 56.Chowdhury A, Santra A, Bhattacharjee K, Ghatak S, Saha DR, Dhali GK. Mitochondrial oxidative stress and permeability transition in isoniazid and rifampicin induced liver injury in mice. J Hepatol. 2006;45:117–126. doi: 10.1016/j.jhep.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 57.Maglich JM, Stoltz CM, Goodwin B, Hawkins-Brown D, Moore JT, Kliewer SA. Nuclear pregnane x receptor and constitutive androstane receptor regulate overlapping but distinct sets of genes involved in xenobiotic detoxification. Mol Pharmacol. 2002;62:638–646. doi: 10.1124/mol.62.3.638. [DOI] [PubMed] [Google Scholar]
- 58.Xie W, Uppal H, Saini SP, Mu Y, Little JM, Radominska-Pandya A, Zemaitis MA. Orphan nuclear receptor-mediated xenobiotic regulation in drug metabolism. Drug Discov Today. 2004;9:442–449. doi: 10.1016/S1359-6446(04)03061-2. [DOI] [PubMed] [Google Scholar]
- 59.Zhou J, Zhai Y, Mu Y, Gong H, Uppal H, Toma D, Ren S, Evans RM, Xie W. A novel pregnane X receptor-mediated and sterol regulatory element-binding protein-independent lipogenic pathway. J Biol Chem. 2006;281:15013–15020. doi: 10.1074/jbc.M511116200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nakamura K, Moore R, Negishi M, Sueyoshi T. Nuclear pregnane X receptor cross-talk with FoxA2 to mediate drug-induced regulation of lipid metabolism in fasting mouse liver. J Biol Chem. 2007;282:9768–9776. doi: 10.1074/jbc.M610072200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee JH, Zhou J, Xie W. PXR and LXR in hepatic steatosis: a new dog and an old dog with new tricks. Mol Pharm. 2008;5:60–66. doi: 10.1021/mp700121u. [DOI] [PubMed] [Google Scholar]
- 62.George J, Liddle C. Nonalcoholic fatty liver disease: pathogenesis and potential for nuclear receptors as therapeutic targets. Mol Pharm. 2008;5:49–59. doi: 10.1021/mp700110z. [DOI] [PubMed] [Google Scholar]
- 63.McMillian M, Nie A, Parker JB, Leone A, Kemmerer M, Bryant S, Herlich J, Yieh L, Bittner A, Liu X, et al. Drug-induced oxidative stress in rat liver from a toxicogenomics perspective. Toxicol Appl Pharmacol. 2005;207:171–178. doi: 10.1016/j.taap.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 64.Tu Z, Bozorgzadeh A, Crispe IN, Orloff MS. The activation state of human intrahepatic lymphocytes. Clin Exp Immunol. 2007;149:186–193. doi: 10.1111/j.1365-2249.2007.03415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Szabo G, Mandrekar P, Dolganiuc A. Innate immune response and hepatic inflammation. Semin Liver Dis. 2007;27:339–350. doi: 10.1055/s-2007-991511. [DOI] [PubMed] [Google Scholar]
- 66.Liu ZX, Govindarajan S, Kaplowitz N. Innate immune system plays a critical role in determining the progression and severity of acetaminophen hepatotoxicity. Gastroenterology. 2004;127:1760–1774. doi: 10.1053/j.gastro.2004.08.053. [DOI] [PubMed] [Google Scholar]
- 67.Liu ZX, Han D, Gunawan B, Kaplowitz N. Neutrophil depletion protects against murine acetaminophen hepatotoxicity. Hepatology. 2006;43:1220–1230. doi: 10.1002/hep.21175. [DOI] [PubMed] [Google Scholar]
- 68.Deng X, Stachlewitz RF, Liguori MJ, Blomme EA, Waring JF, Luyendyk JP, Maddox JF, Ganey PE, Roth RA. Modest inflammation enhances diclofenac hepatotoxicity in rats: role of neutrophils and bacterial translocation. J Pharmacol Exp Ther. 2006;319:1191–1199. doi: 10.1124/jpet.106.110247. [DOI] [PubMed] [Google Scholar]
- 69.Swain MG. Hepatic NKT cells: friend or foe? Clin Sci (Lond) 2008;114:457–466. doi: 10.1042/CS20070328. [DOI] [PubMed] [Google Scholar]
- 70.Speck RF, Schranz C, Lauterburg BH. Prednisolone stimulates hepatic glutathione synthesis in mice. Protection by prednisolone against acetaminophen hepatotoxicity in vivo. J Hepatol. 1993;18:62–67. doi: 10.1016/s0168-8278(05)80010-8. [DOI] [PubMed] [Google Scholar]
- 71.Alla V, Abraham J, Siddiqui J, Raina D, Wu GY, Chalasani NP, Bonkovsky HL. Autoimmune hepatitis triggered by statins. J Clin Gastroenterol. 2006;40:757–761. doi: 10.1097/00004836-200609000-00018. [DOI] [PubMed] [Google Scholar]
- 72.Lauterburg BH, Velez ME. Glutathione deficiency in alcoholics: risk factor for paracetamol hepatotoxicity. Gut. 1988;29:1153–1157. doi: 10.1136/gut.29.9.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lauterburg BH. Analgesics and glutathione. Am J Ther. 2002;9:225–233. doi: 10.1097/00045391-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 74.Cover C, Mansouri A, Knight TR, Bajt ML, Lemasters JJ, Pessayre D, Jaeschke H. Peroxynitrite-induced mitochondrial and endonuclease-mediated nuclear DNA damage in acetaminophen hepatotoxicity. J Pharmacol Exp Ther. 2005;315:879–887. doi: 10.1124/jpet.105.088898. [DOI] [PubMed] [Google Scholar]
- 75.Knight TR, Kurtz A, Bajt ML, Hinson JA, Jaeschke H. Vascular and hepatocellular peroxynitrite formation during acetaminophen toxicity: role of mitochondrial oxidant stress. Toxicol Sci. 2001;62:212–220. doi: 10.1093/toxsci/62.2.212. [DOI] [PubMed] [Google Scholar]
- 76.Kim JS, He L, Lemasters JJ. Mitochondrial permeability transition: a common pathway to necrosis and apoptosis. Biochem Biophys Res Commun. 2003;304:463–470. doi: 10.1016/s0006-291x(03)00618-1. [DOI] [PubMed] [Google Scholar]
- 77.Liu X, Van Vleet T, Schnellmann RG. The role of calpain in oncotic cell death. Annu Rev Pharmacol Toxicol. 2004;44:349–370. doi: 10.1146/annurev.pharmtox.44.101802.121804. [DOI] [PubMed] [Google Scholar]
- 78.Watkins PB, Seeff LB. Drug-induced liver injury: summary of a single topic clinical research conference. Hepatology. 2006;43:618–631. doi: 10.1002/hep.21095. [DOI] [PubMed] [Google Scholar]
- 79.Luef GJ, Waldmann M, Sturm W, Naser A, Trinka E, Unterberger I, Bauer G, Lechleitner M. Valproate therapy and nonalcoholic fatty liver disease. Ann Neurol. 2004;55:729–732. doi: 10.1002/ana.20074. [DOI] [PubMed] [Google Scholar]
- 80.Krähenbühl S, Mang G, Kupferschmidt H, Meier PJ, Krause M. Plasma and hepatic carnitine and coenzyme A pools in a patient with fatal, valproate induced hepatotoxicity. Gut. 1995;37:140–143. doi: 10.1136/gut.37.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ponchaut S, van Hoof F, Veitch K. In vitro effects of valproate and valproate metabolites on mitochondrial oxidations. Relevance of CoA sequestration to the observed inhibitions. Biochem Pharmacol. 1992;43:2435–2442. doi: 10.1016/0006-2952(92)90324-c. [DOI] [PubMed] [Google Scholar]
- 82.Knapp AC, Todesco L, Beier K, Terracciano L, Sägesser H, Reichen J, Krähenbühl S. Toxicity of valproic acid in mice with decreased plasma and tissue carnitine stores. J Pharmacol Exp Ther. 2008;324:568–575. doi: 10.1124/jpet.107.131185. [DOI] [PubMed] [Google Scholar]
- 83.Maciá MA, Carvajal A, del Pozo JG, Vera E, del Pino A. Hepatotoxicity associated with nimesulide: data from the Spanish Pharmacovigilance System. Clin Pharmacol Ther. 2002;72:596–597. [PubMed] [Google Scholar]
- 84.Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs, antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22:169–183. doi: 10.1055/s-2002-30102. [DOI] [PubMed] [Google Scholar]
- 85.Aithal GP, Day CP. Nonsteroidal anti-inflammatory drug-induced hepatotoxicity. Clin Liver Dis. 2007;11:563–575, vi-vii. doi: 10.1016/j.cld.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 86.Leemann T, Transon C, Dayer P. Cytochrome P450TB (CYP2C): a major monooxygenase catalyzing diclofenac 4'-hydroxylation in human liver. Life Sci. 1993;52:29–34. doi: 10.1016/0024-3205(93)90285-b. [DOI] [PubMed] [Google Scholar]
- 87.Tang W. The metabolism of diclofenac--enzymology and toxicology perspectives. Curr Drug Metab. 2003;4:319–329. doi: 10.2174/1389200033489398. [DOI] [PubMed] [Google Scholar]
- 88.Boelsterli UA, Zimmerman HJ, Kretz-Rommel A. Idiosyncratic liver toxicity of nonsteroidal antiinflammatory drugs: molecular mechanisms and pathology. Crit Rev Toxicol. 1995;25:207–235. doi: 10.3109/10408449509089888. [DOI] [PubMed] [Google Scholar]
- 89.Kretz-Rommel A, Boelsterli UA. Cytotoxic activity of T cells and non-T cells from diclofenac-immunized mice against cultured syngeneic hepatocytes exposed to diclofenac. Hepatology. 1995;22:213–222. doi: 10.1002/hep.1840220132. [DOI] [PubMed] [Google Scholar]
- 90.Daly AK, Aithal GP, Leathart JB, Swainsbury RA, Dang TS, Day CP. Genetic susceptibility to diclofenac-induced hepatotoxicity: contribution of UGT2B7, CYP2C8, and ABCC2 genotypes. Gastroenterology. 2007;132:272–281. doi: 10.1053/j.gastro.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 91.Deschamps D, Fisch C, Fromenty B, Berson A, Degott C, Pessayre D. Inhibition by salicylic acid of the activation and thus oxidation of long chain fatty acids. Possible role in the development of Reye's syndrome. J Pharmacol Exp Ther. 1991;259:894–904. [PubMed] [Google Scholar]
- 92.Lauterburg BH, Grattagliano I, Gmür R, Stalder M, Hildebrand P. Noninvasive assessment of the effect of xenobiotics on mitochondrial function in human beings: studies with acetylsalicylic acid and ethanol with the use of the carbon 13-labeled ketoisocaproate breath test. J Lab Clin Med. 1995;125:378–383. [PubMed] [Google Scholar]
- 93.Fromenty B, Pessayre D. Inhibition of mitochondrial beta-oxidation as a mechanism of hepatotoxicity. Pharmacol Ther. 1995;67:101–154. doi: 10.1016/0163-7258(95)00012-6. [DOI] [PubMed] [Google Scholar]
- 94.Dykens JA, Jamieson JD, Marroquin LD, Nadanaciva S, Xu JJ, Dunn MC, Smith AR, Will Y. In vitro assessment of mitochondrial dysfunction and cytotoxicity of nefazodone, trazodone, and buspirone. Toxicol Sci. 2008;103:335–345. doi: 10.1093/toxsci/kfn056. [DOI] [PubMed] [Google Scholar]
- 95.Huang YS, Chern HD, Su WJ, Wu JC, Chang SC, Chiang CH, Chang FY, Lee SD. Cytochrome P450 2E1 genotype and the susceptibility to antituberculosis drug-induced hepatitis. Hepatology. 2003;37:924–930. doi: 10.1053/jhep.2003.50144. [DOI] [PubMed] [Google Scholar]
- 96.Spaniol M, Bracher R, Ha HR, Follath F, Krähenbühl S. Toxicity of amiodarone and amiodarone analogues on isolated rat liver mitochondria. J Hepatol. 2001;35:628–636. doi: 10.1016/s0168-8278(01)00189-1. [DOI] [PubMed] [Google Scholar]
- 97.Kaufmann P, Török M, Hänni A, Roberts P, Gasser R, Krähenbühl S. Mechanisms of benzarone and benzbromarone-induced hepatic toxicity. Hepatology. 2005;41:925–935. doi: 10.1002/hep.20634. [DOI] [PubMed] [Google Scholar]
- 98.Lim PL, Liu J, Go ML, Boelsterli UA. The mitochondrial superoxide/thioredoxin-2/Ask1 signaling pathway is critically involved in troglitazone-induced cell injury to human hepatocytes. Toxicol Sci. 2008;101:341–349. doi: 10.1093/toxsci/kfm273. [DOI] [PubMed] [Google Scholar]
- 99.Grattagliano I, Portincasa P, Palmieri VO, Palasciano G. Contribution of canalicular glutathione efflux to bile formation. From cholestasis associated alterations to pharmacological intervention to modify bile flow. Curr Drug Targets Immune Endocr Metabol Disord. 2005;5:153–161. doi: 10.2174/1568008054064931. [DOI] [PubMed] [Google Scholar]
- 100.Fattinger K, Funk C, Pantze M, Weber C, Reichen J, Stieger B, Meier PJ. The endothelin antagonist bosentan inhibits the canalicular bile salt export pump: a potential mechanism for hepatic adverse reactions. Clin Pharmacol Ther. 2001;69:223–231. doi: 10.1067/mcp.2001.114667. [DOI] [PubMed] [Google Scholar]
- 101.Gitlin N, Julie NL, Spurr CL, Lim KN, Juarbe HM. Two cases of severe clinical and histologic hepatotoxicity associated with troglitazone. Ann Intern Med. 1998;129:36–38. doi: 10.7326/0003-4819-129-1-199807010-00008. [DOI] [PubMed] [Google Scholar]
- 102.Lickteig AJ, Fisher CD, Augustine LM, Aleksunes LM, Besselsen DG, Slitt AL, Manautou JE, Cherrington NJ. Efflux transporter expression and acetaminophen metabolite excretion are altered in rodent models of nonalcoholic fatty liver disease. Drug Metab Dispos. 2007;35:1970–1978. doi: 10.1124/dmd.107.015107. [DOI] [PubMed] [Google Scholar]
- 103.Delcò F, Tchambaz L, Schlienger R, Drewe J, Krähenbühl S. Dose adjustment in patients with liver disease. Drug Saf. 2005;28:529–545. doi: 10.2165/00002018-200528060-00005. [DOI] [PubMed] [Google Scholar]
- 104.Lakehal F, Dansette PM, Becquemont L, Lasnier E, Delelo R, Balladur P, Poupon R, Beaune PH, Housset C. Indirect cytotoxicity of flucloxacillin toward human biliary epithelium via metabolite formation in hepatocytes. Chem Res Toxicol. 2001;14:694–701. doi: 10.1021/tx0002435. [DOI] [PubMed] [Google Scholar]
- 105.Caraceni P, Domenicali M, Vendemiale G, Grattagliano I, Pertosa A, Nardo B, Morselli-Labate AM, Trevisani F, Palasciano G, Altomare E, et al. The reduced tolerance of rat fatty liver to ischemia reperfusion is associated with mitochondrial oxidative injury. J Surg Res. 2005;124:160–168. doi: 10.1016/j.jss.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 106.Grattagliano I, Caraceni P, Portincasa P, Domenicali M, Palmieri VO, Trevisani F, Bernardi M, Palasciano G. Adaptation of subcellular glutathione detoxification system to stress conditions in choline-deficient diet induced rat fatty liver. Cell Biol Toxicol. 2003;19:355–366. doi: 10.1023/b:cbto.0000013341.73139.fc. [DOI] [PubMed] [Google Scholar]
- 107.Vendemiale G, Grattagliano I, Caraceni P, Caraccio G, Domenicali M, Dall'Agata M, Trevisani F, Guerrieri F, Bernardi M, Altomare E. Mitochondrial oxidative injury and energy metabolism alteration in rat fatty liver: effect of the nutritional status. Hepatology. 2001;33:808–815. doi: 10.1053/jhep.2001.23060. [DOI] [PubMed] [Google Scholar]
- 108.Petrosillo G, Portincasa P, Grattagliano I, Casanova G, Matera M, Ruggiero FM, Ferri D, Paradies G. Mitochondrial dysfunction in rat with nonalcoholic fatty liver Involvement of complex I, reactive oxygen species and cardiolipin. Biochim Biophys Acta. 2007;1767:1260–1267. doi: 10.1016/j.bbabio.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 109.Donthamsetty S, Bhave VS, Mitra MS, Latendresse JR, Mehendale HM. Nonalcoholic fatty liver sensitizes rats to carbon tetrachloride hepatotoxicity. Hepatology. 2007;45:391–403. doi: 10.1002/hep.21530. [DOI] [PubMed] [Google Scholar]
- 110.Wang T, Shankar K, Ronis MJ, Mehendale HM. Mechanisms and outcomes of drug- and toxicant-induced liver toxicity in diabetes. Crit Rev Toxicol. 2007;37:413–459. doi: 10.1080/10408440701215100. [DOI] [PubMed] [Google Scholar]
- 111.Portincasa P, Grattagliano I, Palmieri VO, Palasciano G. Nonalcoholic steatohepatitis: recent advances from experimental models to clinical management. Clin Biochem. 2005;38:203–217. doi: 10.1016/j.clinbiochem.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 112.Ito Y, Abril ER, Bethea NW, McCuskey MK, McCuskey RS. Dietary steatotic liver attenuates acetaminophen hepatotoxicity in mice. Microcirculation. 2006;13:19–27. doi: 10.1080/10739680500383423. [DOI] [PubMed] [Google Scholar]
- 113.Pizarro M, Balasubramaniyan N, Solís N, Solar A, Duarte I, Miquel JF, Suchy FJ, Trauner M, Accatino L, Ananthanarayanan M, et al. Bile secretory function in the obese Zucker rat: evidence of cholestasis and altered canalicular transport function. Gut. 2004;53:1837–1843. doi: 10.1136/gut.2003.037689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Agúndez JA, Ladero JM. Glutathione S-transferase GSTT1 and GSTM1 allozymes: beyond null alleles. Pharmacogenomics. 2008;9:359–363. doi: 10.2217/14622416.9.3.359. [DOI] [PubMed] [Google Scholar]
- 115.Huang YS, Su WJ, Huang YH, Chen CY, Chang FY, Lin HC, Lee SD. Genetic polymorphisms of manganese superoxide dismutase, NAD(P)H:quinone oxidoreductase, glutathione S-transferase M1 and T1, and the susceptibility to drug-induced liver injury. J Hepatol. 2007;47:128–134. doi: 10.1016/j.jhep.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 116.Boelsterli UA, Lim PL. Mitochondrial abnormalities--a link to idiosyncratic drug hepatotoxicity? Toxicol Appl Pharmacol. 2007;220:92–107. doi: 10.1016/j.taap.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 117.Grattagliano I, Russmann S, Palmieri VO, Jüni P, Bihl F, Portincasa P, Palasciano G, Lauterburg BH. Low membrane protein sulfhydrils but not G6PD deficiency predict ribavirin-induced hemolysis in hepatitis C. Hepatology. 2004;39:1248–1255. doi: 10.1002/hep.20208. [DOI] [PubMed] [Google Scholar]