Abstract
AIM: To investigate glue extrusion after endoscopic N-butyl-2-cyanoacrylate injection on gastric variceal bleeding and to evaluate the long-term efficacy and safety of this therapy.
METHODS: A total of 148 cirrhotic patients in our hospital with esophagogastric variceal bleeding (EGVB) were included in this study. N-butyl-2-cyanoacrylate was mixed with lipiodol in a 1:1 ratio and injected as a bolus of 1-3 mL according to variceal size. Patients underwent endoscopic follow-up the next week, fourth week, second month, fourth month, and seventh month after injection and then every 6 mo to determine the cast shape. An abdominal X-ray film and ultrasound or computed tomographic scan were also carried out in order to evaluate the time of variceal disappearance and complete extrusion of the cast. The average follow-up time was 13.1 mo.
RESULTS: The instantaneous hemostatic rate was 96.2%. Early re-bleeding after injection in 9 cases (6.2%) was estimated from rejection of adhesive. Late re-bleeding occurred in 12 patients (8.1%) at 2-18 mo. The glue cast was extruded into the lumen within one month in 86.1% of patients and eliminated within one year. Light erosion was seen at the injection position and mucosa edema in the second week. The glue casts were extruded in 18 patients (12.1%) after one week and in 64 patients (42.8%) after two weeks. All kinds of glue clumping shapes and colors on endoscopic examination were observed in 127 patients (86.1%) within one month, including punctiform, globular, pillar and variform. Forty one patients (27.9%) had glue extrusion after 3 mo and 28 patients (28.9%) after six months. The extrusion time was not related to the injection volume of histoacryl. Obliteration was seen in 70.2% (104 cases) endoscopically. The main complication was re-bleeding resulting from extrusion. The prognosis of the patients depended on the severity of the underlying liver disease.
CONCLUSION: Endoscopic injection of cyanoacrylate is highly effective for gastric varices bleeding. The glue clump shape is correlated with anatomic structure of vessels. The time of extrusion was not related to dosage of the glue.
Keywords: Gastric variceal bleeding, Glue extruded, N-butyl-2-cyanoacrylate, Portal hypertension
INTRODUCTION
Although the outcome of variceal hemorrhage has improved over the past two decades, variceal hemorrhage is still the most serious complication of portal hypertension and chronic liver disease[1-3]. Gastric varices (GV) and their association with portal hypertension were first described in 1913[4]. Since then, there have been reports on different aspects of gastric varices including prevalence, bleed tendency and treatment options. Gastric varices occur in 20% of patients with portal hypertension either in isolation or in combination with esophageal varices (EV)[5-6]. GV possibly bleed less frequently than EV, but GV bleeding is typically difficult to control, and is associated with a high risk for re-bleeding and high mortality. Fundal varices, large GV (> 5 mm), presence of a red spot, and Child’s C liver status are associated with a high risk for bleeding[7-8]. gastro-esophageal varices type 1 (GOV1) have a much lower risk for bleeding. A portosystemic pressure gradient of > 12 mmHg is not necessary for GV bleeding, probably related to the high frequency of spontaneous gastrorenal shunts in these patients[9]. There is no consensus for the optimum treatment of GV including drugs, endoscopy, and surgery. Optimal management of GV requires a multidisciplinary approach and close cooperation between gastroenterologists, interventional radiologists and the surgical team.
Histoacryl (N-butyl-cyanoacrylate) is the only endoscopic treatment that has been shown to be effective. Sohendra et al[10] first reported in 1986 that bleeding from GV could be controlled by sclerotherapy using the tissue adhesive agent butyl cyanoacrylate. Since then several authors have used different sclerosing agents to achieve hemostasis in bleeding gastric varices, including N-butyl-2 cyanoacrylate (histoacryl)[11,12], 2-octyl cyanoacrylate[13], ethanolamine oleate injection[14], gastric variceal banding[15], thrombin[1] and sodium tetradecyl sulfate[16]. However, N-butyl 2 cyanoacrylate (NBC) is the only promising agent. Cyanoacrylate injection can achieve primary hemostasis in 70% to 95% of patients with acute GV bleeding, with an early re-bleeding rate ranging from 0% to 28% within 48 h[17-19].
To date, there are many studies on the efficacy and hemostasis rate of NBC injection on gastric variceal bleeding. However, there are no reports on detailed gel extrusion after injection. In this study, we investigated the glue extrusion after endoscopic NBC injection for gastric variceal bleeding and evaluated the long-term efficacy and safety of this therapy to define its role in initial treatment.
MATERIALS AND METHODS
Materials preparation
A 1:1 (v/v) mixture of N-butyl-2-cyanoacrylate (Histoacryl blue; B. Braun-Melsungen, Germany, 0.5 mL per ampoule) and lipiodol (Laboratoire Guerbet, Aulnay-Sous-Bois, France) was prepared just before injection. An endoscopic injector (hemostasis catheter) with a 23-gauge needle (Optiflo, Boston Scientific, Boston, USA) was used.
Patients
From June 2007 to December 2008, total of 148 cirrhotic patients with or without concomitant hepatocellular carcinoma (HCC) who presented to our hospital with acute gastrointestinal bleeding, or who were already hospitalized and developed acute gastrointestinal bleeding, were subjected to injection of the mixture, except those with severe encephalopathy, severe hemodynamic instability, pregnancy, or those who refused treatment. Active hemorrhage was defined as bleeding or oozing of blood from a gastric varix, a clot or blackish ulcer or rent over a gastric varix, or the presence of distinct large GV and absence of EV or other causes of gastrointestinal (GI) bleeding. Liver function was classified according to the Child-Pugh classification criteria. The most common cause of GV was viral hepatitis-related cirrhosis (74.5%). The modality and location of the GV were classified according to the system proposed by Hashizume et al[19]; the modality was classified into 3 types: tortuous (F1), nodular (F2), and tumorous (F3); and location, 5 areas: anterior (La), posterior (Lp), lesser (Ll) and greater curvature (Lg) of the cardia, and the fundic area (Lf). Most of the GV were large. Associated EV were usually small or absent. The most common locations of these GV were the fundus (Lf) and the most proximal body on the posterior wall (Lp) (94.4%).
The location of GV was determined according to the classification described by Sarin et al[20] and divided into gastroesophageal varices type 1 (GOV-1), GV continuing as an extension of EV on the lesser curve of the stomach), gastro-esophageal varices type 2 (GOV-2) on the greater curvature or fundal varices communicating with EV, isolated gastric varices type 1 (IGV-1) and fundal varices within a few centimeters of the gastric cardia, or isolated gastric varices type 2 (IGV-2) and isolated ectopic gastric varices.
NBC was mixed with lipiodol in a 1:1 ratio and injected as a bolus of 1 to 3 mL according to variceal size. Thirty patients had isolate GV, 38 had postoperative residual GV, and 72 had dominant GV. The actual volume of the injection was based on the variceal appearance. The injection was stopped when the varices became engorged. Lipiodol was used to flush the injection needle before and after the injection. The tip of the endoscope and the accessory channel were treated with silicone oil to prevent endoscopic damage. All patients received octreotide infusion (50 mg/h) at admission and was continued for 3 d. All patients were given a proton pump inhibitor, initially intravenously for 48 h and then orally for 4-6 wk.
Indices to evaluate the extrusion rule of glue
Indices to evaluate the extrusion rule of glue are as follows: (1) Information on each patient’s gender, age, Child-Pugh classification, stage of GV, number of treatments, dosage of cyanoacrylate, outcome of GV, diameter of main portal tract, liver function and routine blood tests were collected; (2) An X-ray film was obtained three days after injection to determine the contour of the histoacryl cast. A chest X-ray was also obtained to ascertain whether any embolic material had migrated into the chest. Ultrasound and/or computed tomographic scan of the abdomen were carried out within one week; (3) Patients underwent endoscopic follow-up the next week, fourth week, second month, fourth month, and seventh month after injection and then every 6 mo to determine the cast shape. An abdominal X-ray film and ultrasound or computed tomographic scan were also obtained in order to evaluate the time of variceal disappearance and complete extrusion of the cast; (4) The instant hemostasis rate, obliteration rate and re-bleeding rate were analyzed. Initial hemostasis was defined as a condition in which the vital signs were stable and no recurrent bleeding was noted for 48 h after the first injection. The definition of re-bleeding from GV included the following endoscopic conditions: spurting or oozing bleeding from GV or blood pools in the stomach accompanied by a fibrin cap on the GV. Primary success was defined as the absence of recurrent bleeding after the first histoacryl injection and during the entire follow-up period. Secondary success was defined as the absence of recurrent bleeding after the reinjection of histoacryl for recurrent bleeding. Definitive hemostasis included both primary and secondary success. Treatment failure was defined as failure to obtain definitive hemostasis.
Complications
Major complications included fever, chest pain, esophageal stricture, septicemia, mediastinum inflammation, pulmonary embolism, cerebral infarction, portal vein embolization, aspirated pneumonia and re-bleeding. The average follow-up time was 13.1 mo.
Statistical analysis
Statistical interpretation of data was performed using Statistical Program for Social Sciences (SPSS) version 13. Results were expressed as mean ± SD, median (MD) for all continuous variables (e.g. age, gender, hospital stay, units of packed cells etc) and numbers (percentage) for categorical data (e.g. gender, Child’s class, etc). Analysis was performed using the independent t-test, χ2 test and Fisher’s exact test wherever appropriate. P < 0.05 was considered statistically significant.
RESULTS
A total of 148 patients with liver cirrhosis and EGV at our hospital from June 2007 to December 2008 were subjected to the injection. This was a retrospective review of their records.
Clinical condition
According to Sarin’s classification of GV, GOV-1 was detected in 68 patients (45.9%), GOV-2 in 49 (33.1%), IGV-1 in 30 (20.3%) and IGV-2 in 1 (0.67%). The common cause of GOV was liver cirrhosis and was segmental portal hypertension without liver disease in IGV. The majority of injections in this series were executed in selective cases, with the exception of 25 cases with acute bleeding who received emergent injections. The primary hemostatic rate was 96.2% (142/148). Among the 148 patients, 6 patients did not achieve hemostasis. The average number of sessions required to eradicate the GV was 2.9 ± 1.2. It was observed that at follow-up (1-18 mo) the injected glue was rejected from GV, resulting in eradication. Early re-bleeding after injection in 9 cases (6.2%) was estimated from rejection of the adhesive. Late re-bleeding occurred in 12 patients (8.1%) at 2-18 mo. Some patients were treated with a second injection to successfully control the bleeding (Tables 1 and 2).
Table 1.
Baseline characteristics of the patients
| Variables at baseline | n (%) |
| Total number | 148 |
| Median age (yr) | 50.13 ± 13.55, (14-78) |
| Sex ratio (M:F) | 108:40 |
| Underlying cause | |
| Viral hepatitis B | 87 (58.8) |
| Viral hepatitis C | 7 (4.7) |
| Alcoholic cirrhosis | 14 (9.4) |
| Primary biliary cirrhosis | 6 (4.1) |
| Drug-induced liver cirrhosis | 2 (1.3) |
| Budd-Chiari syndrome | 3 (2.0) |
| CTPV | 4 (2.7) |
| Wilson’s disease | 1 (0.67) |
| Unknown etiology | 24 (16.2) |
| Association with other diseases | |
| Type-2 diabetes | 16 (10.8) |
| Primary hepatic carcinoma | 12 (8.1) |
| Hypertensive disease | 9 (6.1) |
| Portal vein thrombogenesis | 3 (2.0) |
| Clinical classification | |
| Isolated GV | 30 (20.3) |
| EGV received EVS or EVL | 72 (48.6) |
| Residual GV after EVS or EVL | 20 (13.5) |
| GV bleeding after disconnection | 18 (12.2) |
| Other condition | 8 (5.4) |
| Sarin’s category (%) | |
| GOV-1 | 68 (45.9) |
| GOV-2 | 49 (33.1) |
| IGV-1 | 30 (20.3) |
| IGV-2 | 1 (0.67) |
| Child-Pugh class | |
| A/B/C | 42/73/33 |
GV: Gastric varices; EGV: Esophagogastric variceal; GOV: Gastroesophageal varices; IGV: Isolated gastric varices; CTPV: Cavernous transformation of the portal vein.
Table 2.
Results of histoacryl injection
| Variables | n = 148 (%) |
| Number of bleeding times | |
| One time | 49 (33.1) |
| Two times | 38 (25.6) |
| Three times | 18 (12.2) |
| Four times | 9 (6.1) |
| Five times | 6 (4.1) |
| ≥ six times | 17 (11.5) |
| Unidentified | 11 (7.4) |
| Emergency endoscopy | 25 (16.9) |
| Active gastric variceal bleeding | 21 (14.2) |
| Rescue endotherapy | 16 (10.8) |
| Number of injections | 164 |
| Volume of the first glue injection (mL) | |
| 1.0 | 43 (29.1) |
| 2.0 | 59 (39.8) |
| 3.0 | 23 (15.5) |
| 4.0 | 18 (12.2) |
| 5.0 | 4 (2.7) |
| 6.0 | 1 (0.7) |
| Location of the first injection | |
| Inferior esophagus | 8 (5.4) |
| Cardia of stomach | 36 (24.3) |
| Fundus of stomach | 103 (69.6) |
| Descending segment of duodenum | 1 (0.7) |
| Multiple injections required | 15 (10.1) |
| Primary hemostasis rate | 142 (96.2) |
| Re-bleeding rate | 21 (14.1) |
| Obliteration rate | 104 (70.2) |
Vascular structure
Three-dimensional computed tomography was used in ten patients after injection in order to understand the vascular structure of GV. There were two types: one was composed of one blood vessel without obvious branches. The diameter of the influent vein and effluent vein were almost identical. The other was composed of many blood vessels with complex branches. Endoscopic feature of GV were related to their vascular structure. The former was common in regional GV (86%) and the latter in GV with a diffuse pattern (91%).
Glue extrusion
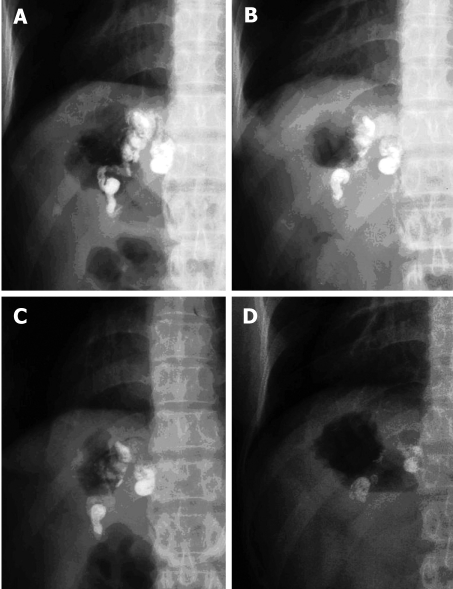
At follow-up (1-18 mo), it was observed that the injected glue was rejected from GV. The cast of glue was extruded into the lumen after one or two weeks, generally without resultant hemorrhage. An X-ray film was obtained three days after the injection to determine the contour of the histoacryl cast. It showed that all the GV were full of the histoacryl and lipiodol mixture, and 13 patients had mixture in the inferior segment of the esophagus. There were all kinds of glue clumping shapes including globular, trabs and flower shapes. The contrast was smaller after one month in 132 patients and disappeared in 138 patients within one year as shown on X ray examination (Figure 1).
Figure 1.
This 47-year-old female patient has isolated gastric varices. Expulsion of tissue glue on X-ray view. A: One day after injection; B: Two weeks after injection; C: One month after injection; D: Three months after injection. Lipiodal mass (intravascular) was in the stomach only and became smaller gradually. This indicated the extrusion process of glue.
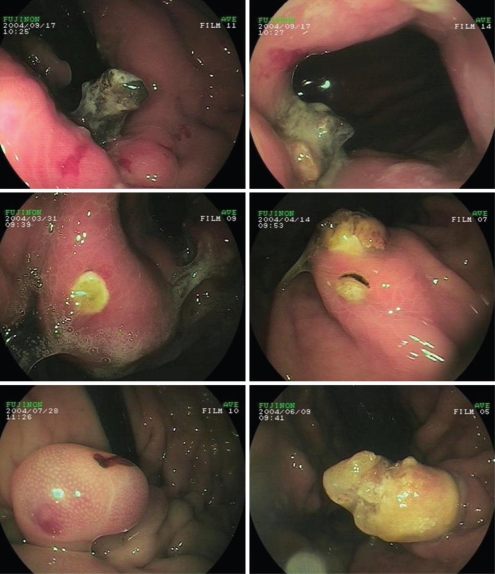
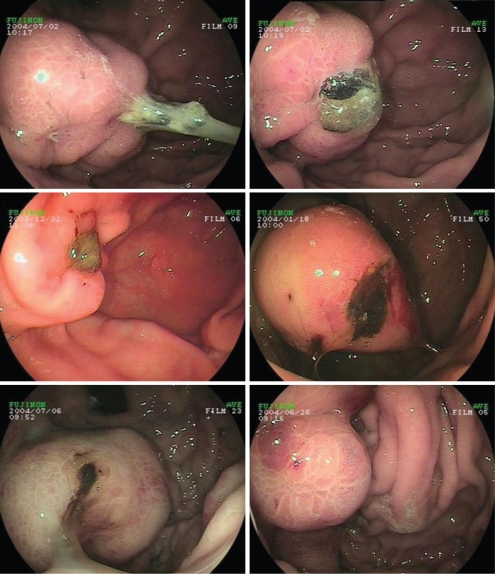
One hundred and twenty eight patients underwent endoscopic follow-up in the second week, fourth week, second month, fourth month, and seventh month after injection and every 6 mo thereafter to determine the cast shape. Light erosion was seen at the injection position and mucosa edema in the second week. The glue casts were extruded in 18 patients (12.1%) after one week and in 64 patients (42.8%) after two weeks. All kinds of glue clumping shapes and colors on endoscopic examination were observed in 127 patients (86.1%) within one month, including punctiform, globular, pillar and variform. Forty one patients (27.9%) had glue extrusion after three months and 28 patients (28.9%) after six months. The extrusion time was not related to injection volume of histoacryl (Tables 3 and 4, Figures 2 and 3).
Table 3.
Extrusion time of glue in 148 patients
| Time of extrusion | Cumulative glue extrusion rate in numbers (%) |
| One week | 18 (12.2) |
| Two weeks | 64 (43.2) |
| One month | 127 (85.8) |
| Three months | 41 (27.7) |
| Six months | 28 (18.9) |
Table 4.
The glue clumping shape on X ray examination and endoscopic examination in the fourth week
| The glue clumping shape | n (%) |
| X ray examination | |
| Globular | 28 (18.9) |
| Cord | 96 (64.8) |
| Flower | 24 (16.3) |
| Endoscopy examination | |
| Punctiform | 36 (24.3) |
| Globular | 88 (59.4) |
| Cord | 24 (16.3) |
| The color of extrusion in endoscopy | |
| Black | 23 (15.5) |
| Yellow | 77 (52.1) |
| Brown | 48 (32.4) |
Figure 2.
Different colors and shapes of contrast on endoscopic examination. A gastric mucosal defect can be seen with expulsion of the adhesive plug from the thrombosed gastric varix several weeks after endoscopic treatment with N-2-butyl-cyanoacrylate.
Figure 3.
Different colors and shapes of contrast on endoscopic examination.
Prognosis
Twenty one patients (14.1%) had re-bleeding. Five patients died from re-bleeding, hepatic failure or HCC aggravation. Lipiodol was seen flowing into lung vessels during injection in 1 with no serious cough or signs of ectopic embolism. The obliteration rate was 70.2% (104 cases) as shown on endoscopic examination. The determining factor for long-term survival was the underlying disease leading to portal hypertension.
DISCUSSION
The majority of patients with cirrhosis will develop varices during their lifetime. Once the diagnosis of cirrhosis has been made, the incidence of new varices is 5% per year and these will progress from small to large varices at a rate of 10 to 15% per year. Growth seems to be influenced by the progression of liver failure. At least one-third of these patients will bleed from their varices and despite significant improvements in treatment and diagnosis, the mortality rate still remains high (30%).
China is one of the countries with the highest incidence of gastric variceal hemorrhage. Esophagogastric variceal bleeding (EGVB) is a serious and emergent condition and hemorrhage control in order to decrease death rate is important. Variceal bleeding results in considerable morbidity and mortality. Although GV bleeding occurs less frequently than EV bleeding[20], whenever bleeding occurs it tends to be more severe and requires more red blood cell transfusions and has a higher mortality rate than EV bleeding[21]; after control of acute bleeding, GV has a high re-bleeding rate of 34% to 89%[22,23]. The principle of initial treatment is to achieve hemostasis and prevent bleeding-related complications such as renal failure, infection, and hepatic decompensation. Cyanoacrylate injection has been proved in large series to be a safe and effective therapy for gastric variceal bleeding.
A total 148 cirrhotic patients with EGV at our hospital from June 2007 to December 2008 were subjected to this treatment. Cyanoacrylate was injected intravariceally in a 1:1 mixture with lipiodal. Each patient underwent scheduled or emergent endoscopic injection of cyanoacrylate and were counterchecked on the 7th day, 1st month and 3rd month after the first treatment, respectively. Cyanoacrylate is a liquid with a consistency similar to water, which rapidly polymerizes on contact with blood. Although the adhesive is injected in a manner similar to sclerosants, extra precautions must be taken before its use to prevent damaging the endoscope. Silicone oil, oil-based contrast agents, simethicone or even olive oil should be used to flush the tip of the endoscope as well as the entire biopsy channel[24,25]. The glue was rejected into the gastric cavity after one or two weeks without re-bleeding. The cast of glue was extruded into the lumen as a foreign body. Glue was extruded in 86.1% of patients within one month with all kinds of shapes and colors of contrast. The rejection had no adverse effects. The glue was extruded in 18 patients (12.1%) within one week and in 64 patients (42.8%) within two weeks. All kinds of glue clumping shapes and colors were seen on endoscopic examination in 127 patients (86.1%) within one month, including punctiform, globular, pillar and variform. Forty one patients (27.9%) had glue extrusion after three months and 28 patients (28.9%) after six months. The extrusion time was not related to the injection volume of histoacryl. We didnot observe contrast due to glue in six patients as a result of mucosal crimple.
We found re-bleeding in 9 patients due to glue extrusion. These patients were examined by endoscopy and erosion and ulcer at the injection site were noted. However, the volume of blood was not large. Time to re-bleeding was about one or two months. We administered antacid drugs, and in some, endoscopy therapy. All the patients recovered. Both follow up and supplementary treatment are important in maintaining and improving long-term outcomes. Repeated sclerotherapy using NBC is effective for remnant GV. The formation of collateral veins around the cardia region after obliteration of gastric short veins or the posterior gastric vein may lead to new EV, which can be managed by conventional endoscopic or surgical measures.
Endoscopic injection of cyanoacrylate is highly effective in the treatment of gastric variceal hemorrhage, with only a few acute and long-term complications. This treatment modality may be referred to as the first choice for bleeding GV.
COMMENTS
Background
Esophagogastric variceal bleeding (EGVB) is a serious and emergent condition of portal hypertension and results in considerable morbidity and mortality. Gastric varices (GV) occur in 20% of patients either in isolation or in combination with esophageal varices (EV). GV possibly bleed less frequently than EV, but GV bleeding is typically difficult to control, and is associated with a high risk for re-bleeding and high mortality. There is no consensus on the optimum treatment of GV including drugs, endoscopy, and surgery. Optimal management of GV requires a multidisciplinary approach and close cooperation between gastroenterologists, interventional radiologists and the surgical team. Sohendra et al first reported in 1986 that bleeding from GV could be controlled by sclerotherapy using the tissue adhesive agent butyl cyanoacrylate.
Research frontiers
Cyanoacrylate injection can achieve primary hemostasis in 70% to 95% of patients with acute GV bleeding, with an early re-bleeding rate ranging from 0% to 28% within 48 h. To date, there are many studies on the efficacy and hemostasis rate of N-butyl-2-cyanoacrylate injection on gastric variceal bleeding. However, there are no reports on detailed gel extrusion after injection.
Innovations and breakthroughs
Gastric variceal bleeding can be challenging to the clinician. Tissue adhesives can control acute bleeding in over 80% of patients, with re-bleeding rates of 20%-30%, and should be the first-line therapy where available. In this study, we investigated the glue extrusion after endoscopic N-butyl-2-cyanoacrylate injection for gastric variceal bleeding and evaluated the long-term efficacy and safety of this therapy to define its role in the initial treatment.
Applications
By understanding how the glue is extruded and the long-term efficacy and safety of endoscopic N-butyl-2-cyanoacrylate injection, this study may represent a better therapeutic intervention in the treatment of patients with gastric variceal bleeding.
Terminology
Gastroesophageal varices type 1 (GOV-1) are GV continuing as an extension of EV on the lesser curve of the stomach, gastro-esophageal varices type 2 (GOV-2) are found on the greater curvature or fundal varices communicating with EV. Isolated gastric varices type 1 (IGV-1) and fundal varices are found within a few centimeters of the gastric cardia, or isolated gastric varices type 2 (IGV-2) and isolated ectopic gastric varices.
Peer review
Looking at the rate of glue extrusion and its association with re-bleeding is quite a novel way of reporting the success of an old technique in arresting gastric variceal bleeding.
Footnotes
Peer reviewer: Andrew Seng Boon Chua, MD, Department of Gastroenterology, Gastro Centre Ipoh, 1, lorong Rani, 31, lebuhraya Tmn Ipoh, Ipoh Garden South, IPOH 30350, Malaysia
S- Editor Tian L L- Editor Webster JR E- Editor Yin DH
References
- 1.Marques P, Maluf-Filho F, Kumar A, Matuguma SE, Sakai P, Ishioka S. Long-term outcomes of acute gastric variceal bleeding in 48 patients following treatment with cyanoacrylate. Dig Dis Sci. 2008;53:544–550. doi: 10.1007/s10620-007-9882-5. [DOI] [PubMed] [Google Scholar]
- 2.Bhasin DK, Siyad I. Variceal bleeding and portal hypertension: new lights on old horizon. Endoscopy. 2004;36:120–129. doi: 10.1055/s-2004-814179. [DOI] [PubMed] [Google Scholar]
- 3.Lunderquist A, Börjesson B, Owman T, Bengmark S. Isobutyl 2-cyanoacrylate (bucrylate) in obliteration of gastric coronary vein and esophageal varices. AJR Am J Roentgenol. 1978;130:1–6. doi: 10.2214/ajr.130.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy. 1986;18:25–26. doi: 10.1055/s-2007-1013014. [DOI] [PubMed] [Google Scholar]
- 5.Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175–1189. doi: 10.1053/j.gastro.2004.01.058. [DOI] [PubMed] [Google Scholar]
- 6.Seewald S, Sriram PV, Naga M, Fennerty MB, Boyer J, Oberti F, Soehendra N. Cyanoacrylate glue in gastric variceal bleeding. Endoscopy. 2002;34:926–932. doi: 10.1055/s-2002-35312. [DOI] [PubMed] [Google Scholar]
- 7.Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol. 2002;97:1010–1015. doi: 10.1111/j.1572-0241.2002.05622.x. [DOI] [PubMed] [Google Scholar]
- 8.Kind R, Guglielmi A, Rodella L, Lombardo F, Catalano F, Ruzzenente A, Borzellino G, Girlanda R, Leopardi F, Pratticò F, et al. Bucrylate treatment of bleeding gastric varices: 12 years' experience. Endoscopy. 2000;32:512–519. doi: 10.1055/s-2000-3817. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen AJ, Baron TH, Burgart LJ, Leontovich O, Rajan E, Gostout CJ. 2-Octyl-cyanoacrylate (Dermabond), a new glue for variceal injection therapy: results of a preliminary animal study. Gastrointest Endosc. 2002;55:572–575. doi: 10.1067/mge.2002.122032. [DOI] [PubMed] [Google Scholar]
- 10.Bureau C, Péron JM, Alric L, Morales J, Sanchez J, Barange K, Payen JL, Vinel JP. "A La Carte" treatment of portal hypertension: Adapting medical therapy to hemodynamic response for the prevention of bleeding. Hepatology. 2002;36:1361–1366. doi: 10.1053/jhep.2002.36945. [DOI] [PubMed] [Google Scholar]
- 11.Kurokohchi K, Maeta T, Ohgi T, Ono M, Yoshitake A, Yachida T, Yoshida M, Mori Y, Kohi F, Kuriyama S. Successful treatment of a giant exposed blood vessel in a gastric ulcer by endoscopic sclerotherapy with N-butyl-2-cyanoacrylate. Endoscopy. 2007;39 Suppl 1:E250. doi: 10.1055/s-2007-967012. [DOI] [PubMed] [Google Scholar]
- 12.Onozato Y, Kakizaki S, Iizuka H, Mori K, Takizawa D, Ohyama T, Arakawa K, Arai H, Ishihara H, Abe T, et al. Ectopic varices rupture in the gastroduodenal anastomosis successfully treated with N-butyl-2-cyanoacrylate injection. Acta Med Okayama. 2007;61:361–365. doi: 10.18926/AMO/32880. [DOI] [PubMed] [Google Scholar]
- 13.Sugimoto N, Watanabe K, Watanabe K, Ogata S, Shimoda R, Sakata H, Eguchi Y, Mizuta T, Tsunada S, Iwakiri R, et al. Endoscopic hemostasis for bleeding gastric varices treated by combination of variceal ligation and sclerotherapy with N-butyl-2-cyanoacrylate. J Gastroenterol. 2007;42:528–532. doi: 10.1007/s00535-007-2041-0. [DOI] [PubMed] [Google Scholar]
- 14.Matsumoto A, Takimoto K. Gastric fundal varices: new aspects of nonsurgical treatment in Japan. Nat Clin Pract Gastroenterol Hepatol. 2006;3:4–5. doi: 10.1038/ncpgasthep0364. [DOI] [PubMed] [Google Scholar]
- 15.Al Hamad A, Kabbani A, Al Kadhi Y. N-butyl-2-cyanoacrylate (Histoacryl) complication: a case report. Ann Saudi Med. 2006;26:71–72. doi: 10.5144/0256-4947.2006.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mumtaz K, Majid S, Shah H, Hameed K, Ahmed A, Hamid S, Jafri W. Prevalence of gastric varices and results of sclerotherapy with N-butyl 2 cyanoacrylate for controlling acute gastric variceal bleeding. World J Gastroenterol. 2007;13:1247–1251. doi: 10.3748/wjg.v13.i8.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noophun P, Kongkam P, Gonlachanvit S, Rerknimitr R. Bleeding gastric varices: results of endoscopic injection with cyanoacrylate at King Chulalongkorn Memorial Hospital. World J Gastroenterol. 2005;11:7531–7535. doi: 10.3748/wjg.v11.i47.7531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kojima K, Imazu H, Matsumura M, Honda Y, Umemoto N, Moriyasu H, Orihashi T, Uejima M, Morioka C, Komeda Y, et al. Sclerotherapy for gastric fundal variceal bleeding: is complete obliteration possible without cyanoacrylate? J Gastroenterol Hepatol. 2005;20:1701–1706. doi: 10.1111/j.1440-1746.2005.03992.x. [DOI] [PubMed] [Google Scholar]
- 19.Hashizume M, Sugimachi K. Classification of gastric lesions associated with portal hypertension. J Gastroenterol Hepatol. 1995;10:339–343. doi: 10.1111/j.1440-1746.1995.tb01105.x. [DOI] [PubMed] [Google Scholar]
- 20.Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244–1249. [PubMed] [Google Scholar]
- 21.Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060–1064. doi: 10.1053/jhep.2001.24116. [DOI] [PubMed] [Google Scholar]
- 22.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 23.Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986;32:264–268. doi: 10.1016/s0016-5107(86)71843-9. [DOI] [PubMed] [Google Scholar]
- 24.Huang YH, Yeh HZ, Chen GH, Chang CS, Wu CY, Poon SK, Lien HC, Yang SS. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160–167. doi: 10.1067/mge.2000.104976. [DOI] [PubMed] [Google Scholar]
- 25.Rengstorff DS, Binmoeller KF. A pilot study of 2-octyl cyanoacrylate injection for treatment of gastric fundal varices in humans. Gastrointest Endosc. 2004;59:553–558. doi: 10.1016/s0016-5107(03)02865-7. [DOI] [PubMed] [Google Scholar]