Abstract
INTRODUCTION
Acute sigmoid volvulus is a well recognised cause of acute large bowel obstruction.
PATIENTS AND METHODS
We reviewed our unit's experience with non-operative and operative management of this condition. A total of 27 patients were treated for acute sigmoid volvulus between 1996 and 2006. In total, there were 62 separate hospital admissions.
RESULTS
Eleven patients were managed with colonoscopic decompression alone. The overall mortality rate for non-operative management was 36.4% (4 of 11 patients). Fifteen patients had operative management (five semi-elective following decompression, 10 emergency). There was no mortality in the semi-elective cohort and one in the emergency surgery group. The overall mortality for surgery was 6% (1 of 15). Five of the seven patients managed with colonoscopic decompression alone who survived were subsequently re-admitted with sigmoid volvulus (a 71.4% recurrence rate). The six deaths in our overall series each occurred in patients with established gangrene of the bowel. With early surgical intervention before the onset of gangrene, however, good outcomes may be achieved, even in patients apparently unsuitable for elective surgery. Eight of the 15 operatively managed patients were considered to be ASA (American Society of Anesthesiologists) grade 4. There was no postoperative mortality in this group.
CONCLUSIONS
Given the high rate of recurrence of sigmoid volvulus after initial successful non-operative management and the attendant risks of mortality from gangrenous bowel developing with a subsequent volvulus, it is our contention that all patients should be considered for definitive surgery after initial colonoscopic decompression, irrespective of the ASA score.
Keywords: Acute sigmoid volvulus, Colonoscopic decompression, Sigmoid resection
Acute sigmoid volvulus is commonest in the Western world among the elderly and the institutionalised. Given the significant co-morbidity in this population and the perceived risks associated with definitive surgery, many surgeons elect to manage this condition conservatively with colonoscopic decompression alone. Non-operative management of acute sigmoid volvulus potentially obviates surgical morbidity in high-risk elderly and frail patients with distended, unprepared bowel. However, because recurrence rates (55–90%) and mortality rates (40%) are high, conservative treatment should be used predominantly to move patients from emergency surgery status to semi-elective surgery status.1–8 Indeed, following initial resuscitation of patients with acute sigmoid volvulus, including an attempt to detort the volvulus colonoscopically where appropriate, definitive surgery may prevent the significant morbidity and mortality associated with subsequent episodes of volvulus. We reviewed our unit's experience with non-operative and operative management of this condition.
Patients and Methods
The records of all patients who underwent emergency non-operative or operative treatment for acute sigmoid volvulus in the Department of Surgery, Mayo General Hospital, during an 11-year period between January 1996 and December 2006, were reviewed retrospectively. The age, gender, co-morbid problems, ASA score, clinical presentation, indication, non-operative or operative procedures, mortality, morbidity, hospitalisation period, and recurrence rates were considered.
Patients were identified from the operating theatre register and admissions office records.
The diagnosis was established on clinical, radiological (abdominal X-ray films, computed tomography), endoscopic or operative findings.
In the emergency treatment of acute sigmoid volvulus, following initial resuscitation, colonoscopic decompression was performed as the initial treatment in patients who were stable or who did not have peritonitis. When successful, this was either the only treatment or was followed by semi-elective surgery. If initial attempts at colonoscopic decompression were unsuccessful or if patients presented with peritonitis or shock, operative management was undertaken. The operation performed (sigmoid colectomy with primary anastomosis, Hartmann's procedure, Paul–Mikulicz procedure) depended on intra-operative findings and surgeon preference. Mortality was defined as death within 30 days of hospitalisation.
Results
A total of 27 patients were treated for acute sigmoid volvulus during the 11-year period between 1996 and 2006 (Table 1). Sixteen patients (59.3%) had more than one admission with acute sigmoid volvulus requiring detorsion. In patients who had more than one admission with acute sigmoid volvulus (n =13), the period between recurrent episodes ranged from 2–35 months. In total, there were 62 separate hospital admissions for acute sigmoid volvulus.
Table 1.
Demographics of patient series
| Age (years; n = 27) | |
| Mean | 73.1 |
| Median | 77 |
| Range | 48–99 |
| Sex M/F 19/8 | |
| Previous episode of sigmoid volvulus (n = 27) | |
| No | 11 (40.7%) |
| Yes | 16 (59.3%) |
| ASA score | Number of patients (n = 27) |
| 1 | 0 |
| 2 | 2 |
| 3 | 7 |
| 4 | 13 |
| 5 | 5 |
| Number of co-morbidities | Number of patients (n = 27) |
| 0 | 2 |
| 1 | 6 |
| 2 | 1 |
| 3 | 6 |
| 4 | 3 |
| 5 | 5 |
| 6 | 4 |
| Residential status | Number of patients (n = 27) |
| Institution | 19 (70.4%) |
| Home | 8 (29.6%) |
The mean patient age was 73.1 years (range, 48–99 years; median, 77 years). Nineteen patients were male (70.4%) and eight patients were female (29.6%).
Twenty-five patients (92.6%) had significant co-morbidity. Nineteen patients (70.4%) had either a chronic psychiatric illness or were resident in a nursing home. The ASA score of all 27 patients is represented in Table 2.
Table 2.
ASA classification of patients according to mode of management
| ASA | Operative | Operative mortality | Non-operative | Non-operative mortality |
|---|---|---|---|---|
| 1–3 | 7 | 0/7 (0%) | 2 | 0/2 (0%) |
| 4–5 | 8 | 1/8 (12.5%) | 9 | 4/9 (44.4%) |
| Total | 15 | 1/15 (6%) | 11 | 4/11 (36.4%) |
Of seventeen patients with an ASA score of 4 or 5, eight had operative management (mean age, 73.5 years; range, 54–99 years; male:female ratio, 5:3) and nine had conservative management (mean age, 78.4 years; range, 65–88 years; male:female ratio, 7:2). All patients presented with clinical features of obstruction. One patient who presented with peritonitis and shock died during the initial resuscitation and did not have any procedure performed. In this particular case, it was the patient's first presentation with acute sigmoid volvulus. The overall management of all 27 patients is represented in Figure 1.
Figure 1.
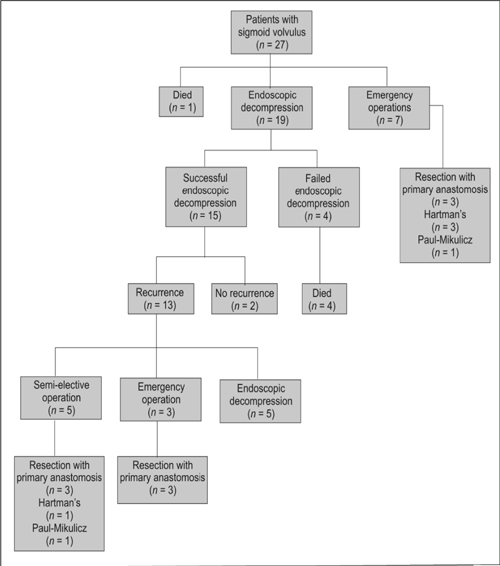
Management of all 27 patients.
Conservative management
Eleven patients were managed with colonoscopic decompression alone, of whom four died on that admission. One of these four patients had had a prior admission for acute sigmoid volvulus and was managed with colonoscopic decompression alone. Five of the seven patients in this group who survived were subsequently admitted with further episodes of sigmoid volvulus and were again treated with decompression (a recurrence rate of 71.4% in this group). Only two patients who had successful reduction of acute sigmoid volvulus by colonoscopy did not have a subsequent admission for a recurrence of the condition. The overall mortality rate for non-operative management was 36.4% (4 of 11 patients). All four of these mortalities occurred within 24 h of admission; in each case, at post mortem examination, a diagnosis of sigmoid volvulus with resultant gangrenous bowel was established.
Surgical management
Fifteen patients were managed operatively. Of these, eight had previously been admitted with acute sigmoid volvulus and been managed with colonoscopic decompression. Five of the 15 patients underwent semi-elective surgery following initial decompression and 10 underwent emergency surgery without prior colonoscopy. Of these, three had a sigmoid colectomy with primary anastomosis, one had a Hartmann's procedure and one had a Paul–Mikulicz's procedure. The latter two patients were noted at laparotomy to have a grossly distended proximal colon and an ischaemic sigmoid colon, respectively.
Of the 10 patients who underwent emergency operation, six had a sigmoid colectomy with primary anastomosis, three had a Hartmann's procedure and one had a Paul–Mikulicz's procedure. Each of these latter four patients were found at laparotomy to have an ischaemic sigmoid colon. Postoperative outcomes of both groups are shown in Table 3. There was no mortality in the semi-elective cohort. One of the 10 patients who had an emergency laparotomy died from endotoxic shock following a Hartmann's procedure for a gangrenous colon. No wound infections occurred in any of the 15 patients; among the nine patients who had a resection with primary anastomosis, there were no anastomotic leaks.
Table 3.
Complications of operative management
| Complications | Semi-elective surgery (n = 5)* | EPA (n = 6) | EHP (n = 3) | Mikulicz (n = 1) |
|---|---|---|---|---|
| None | 2 | 3 | 1 | 1 |
| Death | 0 | 0 | 1 | 0 |
| Sepsis–gangrenous bowel | 0 | 1 | 0 | 0 |
| Parastomal herniation | 0 | 0 | 1 | 0 |
| LRTI | 2 | 2 | 0 | 0 |
| CCF/MI | 1 | 1 | 0 | 0 |
Semi-elective surgery: Mikulicz's (1), RPA (3), Hartmann's (1).
EHP = Emergency Hartmann's procedure
EPA = Emergency primary anastomosis
Of the 15 patients who underwent operative management, 8 (53%) had had colonoscopic decompression during a previous admission for sigmoid volvulus (mean, 4; range, 1–8). Table 4 summarises how many colonoscopies each patient had before surgery.
Table 4.
Number of colonoscopies for patients who underwent operative management
| Number of colonoscopies | Number of patients (n = 8) |
|---|---|
| 1 | 2 |
| 2–3 | 2 |
| 4–6 | 3 |
| > 6 | 1 |
Of the 10 patients who went straight to surgery for peritonitis, three had had previous colonoscopies for sigmoid volvulus; two of these had had the procedure done twice and the other patient eight times.
The overall mortality rate in our series was 22.2% (6 deaths, 27 patients). The overall mortality rate per admission was 9.7% (6 deaths, 62 admissions).
The six deaths in our overall series each occurred in patients with established gangrene of the bowel. With early surgical intervention before the onset of gangrene, however, good outcomes may be achieved, even in patients apparently unsuitable for elective surgery. Eight of the 15 patients who were managed operatively were considered to be ASA grade 4. There was no postoperative mortality in this group.
Discussion
The earliest known description in antiquity of sigmoid volvulus appears in the Ebers Papyrus from Egypt, the oldest preserved medical document, which dates from c.1550 BC.1 The author noted ‘if he does not evacuate it for a twist in the bowel and if the phlegm does not find a way out then it shall rot in the belly’. The condition was also recognised by the ancient Greeks. Hippocrates used a 12-inch long suppository and anal insufflation with air to untwist the bowel.9
Anatomical predispositions, a high-fibre diet, chronic constipation, previous abdominal surgery, neurological or psychiatric illness, pregnancy, high altitude, and megacolon have all been reported in association with development of the condition.10
The most common symptoms of acute sigmoid volvulus are abdominal pain and distension followed by obstipation, while the other complaints include vomiting, nausea, diarrhoea and anorexia. The physical findings are abdominal distension located generally asymmetrically in the upper abdomen, and tenderness, while additional findings include abnormal bowel sounds, tympany, empty rectum, visible peristalsis and an abdominal mass. Presence of rectal melanotic stool or rebound tenderness and guarding may occur in the presence of gangrene or perforation and peritonitis.6,11–13
In sigmoid volvulus, plain abdominal radiographs usually demonstrate a dilated sigmoid colon and/or multiple small or large intestinal air-fluid levels. The diagnostic accuracy of plain abdominal radiography has been put at 65–90% by numerous studies.6,11,14
Findings on computed tomography (CT) may be diagnostic, indicating a whorl pattern in the mesocolon and dilated ahaustral sigmoid colon segments around it.15,16 In a recent series with 25 CT scans, the positive diagnosis rate in sigmoid volvulus was 100%.14
Endoscopy is both a diagnostic method and a therapeutic modality in sigmoid volvulus and is also useful in eliminating other causes of obstruction. A spiral, sphincter-like twist of mucosa shows the torsion in endoscopy.17,18
Spontaneous detorsion of sigmoid volvulus is not common.6 The patients generally have a tendency to hypovolaemic and endotoxic shock caused by closed-loop obstruction and gangrene.12,19,20
While non-operative reduction of sigmoid volvulus generally carries a lower risk than open surgery, recurrence rates are high, and patients may subsequently present with ischaemic bowel and peritonitis, as was the case with three of the patients in our series. Following initial colonoscopic decompression, definitive surgery may be performed with minimal mortality rates. Because the conservative approach is not curative, many surgeons insist on subsequent definitive operative treatment. Pre-operative decompression followed by semi-elective one-stage resection, where possible, enhances optimal surgical outcome in cases of acute sigmoid volvulus.1
The only prospective, randomised study in the literature indicates that a sigmoid resection, done either as a Hartmann's procedure when a gangrenous colon is discovered at laparotomy, or as a one-stage resection with primary anastomosis in the setting of a viable colon, has the lowest rate of recurrence.21
Recent results of series of primary anastomosis in an unprepared bowel, for either malignant or non-malignant colonic obstruction, are encouraging.22,23
Other operative techniques such as sigmoidopexy and, more recently, percutaneous endoscopic colostomy have been used in the management of recurrent sigmoid volvulus. Promising results have been described for percutaneous endoscopic colostomy in selected patients, although the technique is not wide-spread and has not been employed in our unit.24
The overall mortality rate for operatively managed patients in our series was 6% (1 of 15). Surgery may be considered a definitive treatment as no patient was subsequently admitted for acute volvulus. Nineteen patients had colonoscopic decompression, with a mortality rate of 21% (4 of 19). This is not a definitive approach, however, as 13 of the 15 patients initially managed by this means were subsequently admitted with recurrence (87%), with eight of these requiring surgery. When surgery was undertaken as a semi-elective procedure following an initial colonoscopic decompression, there was no mortality (0 of 5).
In two studies of gangrenous and non-gangrenous sigmoid volvulus, the risk factors for mortality identified were: (i) age over 60 years; (ii) presence of shock on admission; and (iii) positive history of a previous episode of volvulus. For the latter, the authors suggested that all patients presenting with non-gangrenous volvulus should have a definitive recurrence preventing procedure carried out in the first attack itself or electively before a subsequent attack.7,13 The present study supports the view that even though a history of previous episodes of volvulus is common, most patients developed gangrene in their first attack13,25,26 and also confirms the view that patients developing gangrene in a recurrent episode suffer a survival disadvantage.27 Our findings also reinforce previous series which suggest maximal survival is achieved by early elective resection following initial decompression.11 During the 10-year period studied, the decision whether or not to manage these patients operatively was at the discretion of the individual surgeon. It is now the policy of our unit to manage acute sigmoid volvulus by resection of the sigmoid colon with or without primary anastomosis depending on intra-operative findings, preferably as a semi-elective procedure after an initial colonoscopic decompression in suitable patients.
Conclusions
In patients with a sigmoid volvulus who do not have peritonitis on presentation, recurrence preventing surgery may be performed with minimal mortality rates. Given the high rate of recurrence of sigmoid volvulus after initial successful non-operative management and the attendant risks of mortality from gangrenous bowel developing with a subsequent volvulus, it is our contention that definitive surgery after initial colonoscopic decompression should be considered for all patients, irrespective of the ASA score.
References
- 1.Kuzu MA, Aslar AK, Soran A, Polat A, Topcu O, Hengirmen S. Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Dis Colon Rectum. 2002;45:1085–90. doi: 10.1007/s10350-004-6364-0. [DOI] [PubMed] [Google Scholar]
- 2.Ballantyne GH, Brandner MD, Beart RW, Jr, Ilstrup DM. Volvulus of the colon: incidence and mortality. Ann Surg. 1985;202:83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung YF, Eu KW, Nyam DC, Leong AF, Ho YH, Seow-Choen F. Minimizing recurrence after sigmoid volvulus. Br J Surg. 1999;86:231–3. doi: 10.1046/j.1365-2168.1999.01034.x. [DOI] [PubMed] [Google Scholar]
- 4.Hines JR, Geurkink RE, Bass RT. Recurrence and mortality rates in sigmoid volvulus. Surg Gynecol Obstet. 1967;124:567–70. [PubMed] [Google Scholar]
- 5.Shepherd JJ. The epidemiology and clinical presentation of sigmoid volvulus. Br J Surg. 1969;56:353–9. doi: 10.1002/bjs.1800560510. [DOI] [PubMed] [Google Scholar]
- 6.Arnold GJ, Nance FC. Volvulus of sigmoid colon. Ann Surg. 1973;177:527–31. doi: 10.1097/00000658-197305000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatnagar BN, Sharma CL. Nonresective alternative for the cure of nongangrenous sigmoid volvulus. Dis Colon Rectum. 1998;41:381–8. doi: 10.1007/BF02237496. [DOI] [PubMed] [Google Scholar]
- 8.Peoples JB, McCafferty JC, Scher KS. Operative therapy for sigmoid volvulus. Identification of risk factors affecting outcome. Dis Colon Rectum. 1990;33:643–6. doi: 10.1007/BF02150737. [DOI] [PubMed] [Google Scholar]
- 9.DiMarino AJ, Benjamin SB. Gastrointestinal disease: an endoscopic approach. New Jersey: Slack; 2002. [Google Scholar]
- 10.Margolin DA, Whitlow CB. The pathogenesis and etiology of colonic volvulus. Semin Colon Rectal Surg. 1999;10:129–38. [Google Scholar]
- 11.Bak MP, Boley SJ. Sigmoid volvulus in elderly patients. Am J Surg. 1986;151:71–5. doi: 10.1016/0002-9610(86)90014-0. [DOI] [PubMed] [Google Scholar]
- 12.Lord SA, Boswell WC, Hungerpiller JC. Sigmoid volvulus in pregnancy. Am Surg. 1996;62:380–2. [PubMed] [Google Scholar]
- 13.Bhatnagar BNS, Sharma CLN, Gautam A, Kakar A, Reddy DC. Gangrenous sigmoid volvulus: a clinical study of 76 patients. Int J Colorect Dis. 2004;19:134–42. doi: 10.1007/s00384-003-0534-8. [DOI] [PubMed] [Google Scholar]
- 14.Atamanalp SS, Yildirgan MI, Basoglu M, Oren D, Aydinli B, et al. Clinical presentation and diagnosis of sigmoid volvulus: outcomes of 40-year and 859-patient experience. J Gastroenterol Hepatol. 2007 doi: 10.1111/j.1440-1746.2007.04946.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Feldman D. The coffee bean sign. Radiology. 2000;216:178–9. doi: 10.1148/radiology.216.1.r00jl17178. [DOI] [PubMed] [Google Scholar]
- 16.Catalano O. Computed tomographic appearance of sigmoid volvulus. Abdom Imaging. 1996;21:314–7. doi: 10.1007/s002619900071. [DOI] [PubMed] [Google Scholar]
- 17.Brothers TE, Strodel WE, Eckhauser FE. Endoscopy in colonic volvulus. Ann Surg. 1987;206:1–4. doi: 10.1097/00000658-198707000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starling JR. Initial treatment of sigmoid volvulus by colonoscopy. Ann Surg. 1979;190:36–9. doi: 10.1097/00000658-197907000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atamanalp SS, Oren D, Basoglu M, Yildirgan MI, Balik AA, et al. Ileosigmoidal knotting: outcome in 63 patients. Dis Colon Rectum. 2004;47:906–10. doi: 10.1007/s10350-004-0528-9. [DOI] [PubMed] [Google Scholar]
- 20.Oren D, Atamanalp SS, Aydinli B, Yildirgan MI, Basoglu M, et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007;50:489–97. doi: 10.1007/s10350-006-0821-x. [DOI] [PubMed] [Google Scholar]
- 21.Bagarani M, Conde AS, Longo R, Italiano A, Terenzi A, Venuto G. Sigmoid volvulus in West Africa: a prospective study on surgical treatments. Dis Colon Rectum. 1993;36:186–90. doi: 10.1007/BF02051177. [DOI] [PubMed] [Google Scholar]
- 22.Naaeder SB, Archampong EQ. One-stage resection of acute sigmoid volvulus. Br J Surg. 1995;82:1635–6. doi: 10.1002/bjs.1800821215. [DOI] [PubMed] [Google Scholar]
- 23.Naraynsingh V, Rampaul R, Maharaj D, Kuruvilla T, Ramcharan K, Pouchet B. Prospective study of primary anastomosis without colonic lavage for patients with an obstructed left colon. Br J Surg. 1999;86:1341–3. doi: 10.1046/j.1365-2168.1999.01230.x. [DOI] [PubMed] [Google Scholar]
- 24.Daniels IR, Lamparelli MJ, Chave H, Simson JN. Recurrent sigmoid volvulus treated by percutaneous endoscopic colostomy. Br J Surg. 2000;87:1419. doi: 10.1046/j.1365-2168.2000.01537.x. [DOI] [PubMed] [Google Scholar]
- 25.Shepherd JJ. Treatment of volvulus of the sigmoid colon: a review of 425 cases. BMJ. 1968;1:280–3. doi: 10.1136/bmj.1.5587.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson JR, Lee D. The management of sigmoid volvulus. Br J Surg. 1981;68:117–20. doi: 10.1002/bjs.1800680217. [DOI] [PubMed] [Google Scholar]
- 27.Melo SM. Megasigmoid and acute volvulus in relation to altitude. Int Surg. 1966;45:504–7. [Google Scholar]


