Abstract
INTRODUCTION
Early carotid endarterectomy (CEA) in symptomatic patients may prevent repeat cerebral events. This study investigates the relationship between waiting time for CEA and the incidence of repeat cerebral events prior to surgery in symptomatic patients.
PATIENTS AND METHODS
A prospective database of consecutive patients undergoing CEA between January 2002 and December 2006 was reviewed. Repeat event rates prior to surgery were calculated using Kaplan–Meier analysis and predictive factors identified using Cox regression analysis.
RESULTS
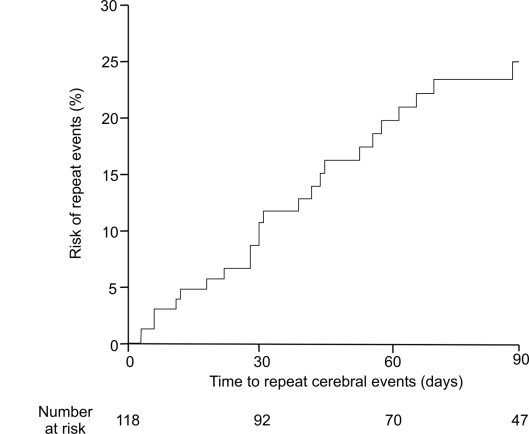
A total of 118 patients underwent CEA for non-disabling stroke, TIA and amaurosis fugax. Repeat cerebral events occurred in 34 of 118 (29%) patients at a median 51 days (range, 2–360 days) after the first event. The estimated risk of repeat events was 2% at 7 days and 9% at 1 month after first event (Kaplan–Meier survival analysis). Age (HR 1.059; 95% CI 1.014–1.106; P = 0.009] was identified as a predictor of repeat events. Patients underwent surgery at median 97 days (range, 7–621 days) after the first event. Eleven of 60 (18%) patients waiting ≤?97 days for surgery and 23 of 58 (40%) patients waiting >?97 days had repeat events. (P = 0.011, chi-squared test).
CONCLUSIONS
Delays in surgery should be reduced in order to minimise repeat cerebral events in patients with symptomatic carotid stenosis, particularly in the elderly population.
Keywords: Carotid endarterectomy, Transient ischaemic attacks, Non-disabling stroke, Amaurosis fugax, Repeat cerebral events
Stroke is one of the leading causes of death in industrialised countries.1 Rapid assessment stroke clinics have been shown to be an effective way of selecting patients for early carotid intervention2 with delays reduced by the early identification of symptoms and efficient direction towards appropriate care.
Carotid endarterectomy (CEA) has been shown to be helpful in prevention of further strokes following a non-disabling cerebral ischaemic event.3,4 The early period after a transient ischaemic attack (TIA) or non-disabling stroke is associated with a high incidence of further cerebral events. Recent data from population-based studies suggest that the risk of sustaining a repeat event following a TIA is 8% at 7 days, 11.5% at 1 month and 17.3% at 3 months and the risk increases slightly following a minor stroke.5 The Oxford Community Stroke Project (OCSP) reported a stroke risk of 8.6% at 7 days and 12% at 1 month after first-ever TIA and 2.4% in the first week after referral rising to 4.9% at 1 month.6 As a result, timing of carotid endarterectomy following cerebral ischaemic event has been a topic of considerable interest.7–11
Carotid endarterectomy is beneficial in reducing risk of stroke in the presence of > 70% carotid stenosis,3,4 with greater absolute risk reduction seen if surgery is carried out within 1–2 weeks of the ischaemic event.11–14 Despite one observational study which suggested an increased risk of peri-operative stroke in those patients operated on within 1 month of the preceding event,15 most clinicians advocate prompt surgical intervention in patients with symptomatic high-grade stenosis. The aim of this study was to investigate the relationship between waiting time for CEA and the incidence of repeat cerebral events prior to surgery.
Patients and Methods
Setting and patients
Consecutive patients from a single vascular unit who had CEA for symptomatic carotid stenosis between January 2002 and December 2006 were identified from a prospectively maintained vascular database and their case notes reviewed retrospectively. All patients underwent bilateral carotid duplex scans carried out by experienced vascular technologists and dates of key events including onset of symptoms, initial presentation, specialist referral and review, carotid duplex and surgery were recorded. Indications for surgery were classified as hemispheric transient ischaemic attacks (TIA), amaurosis fugax and non-disabling stroke (defined as focal neurological deficit persisting for more than 24 h and leading to a slight disability but able to look after own affairs without assistance; equivalent to modified Rankin scale16 of 1 and 2). Any specific reasons for delayed assessment of patients were noted. Requirements for further carotid imaging including computed tomography (CT) scan and magnetic resonance imaging (MRI) in difficult cases, echocardiography and need for a further specialist referral were also noted. Details of repeat cerebral events were obtained from the case notes.
Statistical analysis
All analyses were performed in consultation with a medical statistician using Statistical Package for Social Sciences (SPSS for Windows, v.13.0; Chicago, IL, USA). Repeat events after initial presentation were analysed using Kaplan–Meier survival analysis. Predictive factors for repeat cerebral events were identified using Cox regression analysis; repeat cerebral events and waiting time for surgery were compared with chi-squared test and a P-value less than 0.05 was considered statistically significant.
Results
Initial presentation
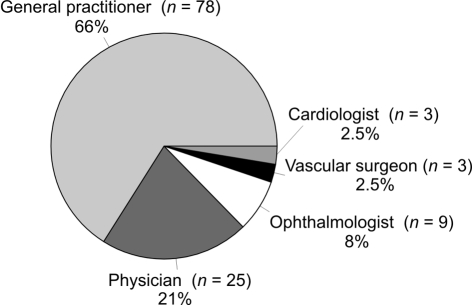
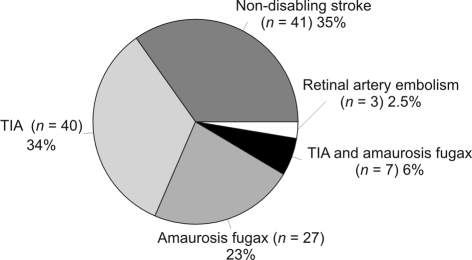
A total of 118 patients underwent carotid endarterectomy during the study period. The median age was 73.5 years (range, 45–88 years) and 72% patients were male (M:F ratio, 85:33). Of these, 78 (66%) patients presented initially to their general practitioner following first symptoms whilst the remaining patients presented to a physician, ophthalmologist, vascular surgeon or cardiologist (Fig. 1A). Median time from the first symptom to initial presentation was 3 days (range, 0–609 days); however, 25% of patients waited over 1 month before seeking medical attention. Of the 118 patients, 69 (58.4%) presented initially within a week of the first symptom and a further 19 patients (16.1%) presented within a month. Initial symptoms were non-disabling stroke (35%), TIA (34%), amaurosis fugax (23%) and TIA and amaurosis fugax (6%). Three patients were found to have retinal artery embolism on routine diabetic screening (Fig. 1B). Times to key events after first symptoms are shown in Table 1. Patients waited for a median 97 days (range, 7–621 days) from initial event to CEA and 21 days (range, 1–156 days) from vascular consultation to CEA. All patients had > 70% internal carotid artery stenosis. In 14 patients, carotid duplex was not conclusive and so the diagnosis was confirmed by carotid CT or MRI.
Figure 1.
(A) Initial presentation; (B) initial symptoms.
Table 1.
Key events from first symptom
| Key events | Median (days) | Range (days) |
|---|---|---|
| Initial event to initial presentation | 3 | 0–609 |
| Initial event to carotid duplex | 41 | 1–615 |
| Initial event to visiting vascular specialist | 58 | 1–609 |
| Initial event to surgery | 97 | 7–621 |
| Initial event to repeat cerebral events | 51 | 2–360 |
Repeat cerebral events
Of the 118 patients, 34 (29%) suffered repeat cerebral events before undergoing CEA; of these, 16 had transient limb weakness, 13 had amaurosis fugax and 5 had transient speech-related symptoms. None of these 34 patients had a disabling stroke. Repeat cerebral events occurred at a median 51 days (range, 2–360 days) after first event. The estimated risk of repeat events prior to surgery was 1.7% at 7 days, 8.9% at 1 month and 25% at 3 months (Kaplan–Meier survival analysis; Fig. 2). Using a Cox regression analysis, patient age (HR 1.059; 95% CI 1.014–1.106; P = 0.009) was identified as a predictor of repeat events (Table 2). Other factors including gender, limb symptoms (motor or sensory), TIA alone, amaurosis fugax and non-disabling stroke were not found to be predictors of repeat events. Of the 60 patients who waited for surgery for ≤ 97 days, 11 (18%) had repeat cerebral events and of the remaining 58 patients who waited for surgery for >97 days, 23 (40%) had repeat cerebral events (P = 0.011, chi-squared test; Table 3).
Figure 2.
Time to repeat cerebral events curve prior to surgery.
Table 2.
Cox regression analysis of risk factors for repeat cerebral events
| Risk factor | Hazard ratio (95% CI) | P-value |
|---|---|---|
| Age | 1.059 (1.014–1.106) | 0.009 |
| Gender | 0.548 (0.264–1.137) | 0.106 |
| Limb symptoms | 1.625 (0.789–3.344) | 0.188 |
| TIA alone | 1.274 (0.557–2.913) | 0.566 |
| TIA and amaurosis fugax | 1.848 (0.575–5.934) | 0.302 |
| Amaurosis fugax alone | 1.004 (0.384–2.620) | 0.994 |
| Non-disabling stroke | 1.227 (0.591–2.549) | 0.583 |
Table 3.
Repeat cerebral events
| Repeat events | Waiting time to surgery in days (%) | P-value* | |
|---|---|---|---|
| ≤ 97 (n = 60) | > 97 (n = 58) | ||
| Yes | 11 (18%) | 23 (40%) | |
| 0.011 | |||
| No | 49 (82%) | 35 (60%) | |
Chi-squared test.
Discussion
This study demonstrates that a prolonged delay between initial presentation and carotid endarterectomy increases the risk of repeat cerebral events. This highlights the importance of prompt referral, efficient investigation and early surgery. It also supports the findings from a pooled data analysis of patients from the European Carotid Surgery Trial (ECST) and North American Symptomatic Carotid Endarterectomy Trial (NASCET) that showed the benefit of performing surgery within the first 2 weeks of last ischaemic cerebral event.12
The estimated risk of repeat cerebral events observed in this study was slightly higher than the risk of recurrent stroke observed in previous studies.5,6 Furthermore, the risk factor analysis in the current study showed that elderly patients waiting longer for surgery are more likely to suffer from repeat cerebral events. This supports the view that repeat events are likely to have different predictive factors and early recognition of these may be useful in preventing any delays in carotid intervention. In contrast to a previous study, initial symptoms such as TIA, amaurosis fugax and limb symptoms including sensory and motor symptoms were not predictive of repeat events in this study which may be a chance finding.17
In this study, carotid endarterectomy was delayed for various reasons which included delayed presentation, referral and waiting times for investigation and surgery. Pre-hospital delays can be reduced by primary care physician education regarding the importance of promptly and fully evaluating patients with TIA. There may be a case for seeing all TIA patients in rapid-access clinics as recommended in the past.18,19 Pre-operative delays may arise for various reasons including delay in initial duplex scan, the need for additional imaging, or further specialist opinion. Attempts to reduce these delays by speeding up definitive investigations after initial presentation, possibly by introducing local treatment pathways and better organisation of referral services, may avoid delays in patients undergoing surgery.
Many patients following an ischaemic cerebral event delay seeking medical attention, as reported previously.20 In our study, 25% of patients waited for more than a month before seeking medical attention which suggests that an effective public education plan needs to be implemented to increase patient knowledge and attitude following TIA or stroke.
It is likely that the risk of repeat cerebral events is much higher than previously thought. The current study focused exclusively on patients who underwent carotid surgery and was not designed to identify patients who were not considered for surgical intervention as a result of fatal or severe cerebrovascular events following initial ischaemic event. It may, therefore, underestimate the risk of repeat stroke whilst awaiting surgery.
Whilst the results are interesting, this study does not give a clear view on an optimum time interval for carotid endarterectomy following a cerebrovascular event. Nonetheless, the risk of repeat cerebral event increased linearly with time from initial event to surgery suggesting that there may be no ‘safe’ period of delay for carotid endarterectomy following TIA, minor stroke or amaurosis fugax. These patients, in many ways, are analogous to those presenting with unstable angina and, accordingly, must be urgently assessed or indeed admitted as an emergency and those with a carotid stenosis of > 70% should be offered surgery as soon as possible. This is in keeping with the UK Department of Health national stroke strategy which recommends that carotid intervention for recently symptomatic severe carotid stenosis should be regarded as an emergency procedure and should ideally be performed within 48 hours of a TIA or minor stroke.21
Acknowledgments
The authors would like to thank M Roidl (clinical research fellow), C Foy (medical statistician, Gloucestershire Research and Development Unit), C Wakely, J Minor and H Metcalfe (vascular scientists) and L Emerson and F Slim (senior nurse practitioners) for their contribution and support.
References
- 1.Warburton E. Stroke management. Clin Evid. 2004;11:240–56. [PubMed] [Google Scholar]
- 2.Widjaja E, Manuel D, Hodgson TJ, Connolly DJ, Coley SC, et al. Sheffield Stroke Prevention Group. Imaging findings and referral outcomes of rapid assessment stroke clinics. Clin Radiol. 2005;60:1076–82. doi: 10.1016/j.crad.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415–25. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 4.European Carotid Surgery Trialists' collaborative group (ECST) Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial. Lancet. 1998;351:445–53. [PubMed] [Google Scholar]
- 5.Coull A, Lovett JK, Rothwell PM, on behalf of the Oxford Vascular Study Early risk of stroke after a TIA or minor stroke in a population-based study. BMJ. 2004;328:326–8. doi: 10.1136/bmj.37991.635266.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lovett JK, Dennis M, Sandercock PAG, Bamford J, Warlow CP, Rothwell PM. The very early risk of stroke after a first transient ischaemic attack. Stroke. 2003;34:138–40. doi: 10.1161/01.STR.0000080935.01264.91. [DOI] [PubMed] [Google Scholar]
- 7.Ballotta E, Da Giau G, Baracchini C, Abbruzzese E, Saladini M, Meneghetti G. Early versus delayed carotid endarterectomy after a nondisabling ischaemic stroke: a prospective randomised study. Surgery. 2002;131:287–93. doi: 10.1067/msy.2002.119987. [DOI] [PubMed] [Google Scholar]
- 8.Eckstein HH, Ringleb P, Dorfler A, Klemm K, Muller BT, et al. The carotid surgery for ischaemic stroke trial: a prospective observational study on carotid endarterectomy in the early period after ischaemic stroke. J Vasc Surg. 2002;36:997–1004. doi: 10.1067/mva.2002.128303. [DOI] [PubMed] [Google Scholar]
- 9.Brandl R, Brauer RB, Maurer PC. Urgent carotid endarterectomy for stroke in evolution. Vasa. 2001;30:115–21. doi: 10.1024/0301-1526.30.2.115. [DOI] [PubMed] [Google Scholar]
- 10.Peiper CH, Nowack J, Ktenidis K, Hopstein S, Keresztury G, Horsch S. Prophylactic urgent revascularisation of the internal carotid artery in the symptomatic patient. Vasa. 2001;30:247–51. doi: 10.1024/0301-1526.30.4.247. [DOI] [PubMed] [Google Scholar]
- 11.Welsh S, Mead G, Chant H, Picton A, O'Neill PA, McCollum CN. Early carotid surgery in acute stroke: a multicenter randomised pilot study. Cerebrovasc Dis. 2004;18:200–5. doi: 10.1159/000079942. [DOI] [PubMed] [Google Scholar]
- 12.Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ, for the Carotid Endarterectomy Trialists Collaboration Effect of endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet. 2004;363:915–24. doi: 10.1016/S0140-6736(04)15785-1. [DOI] [PubMed] [Google Scholar]
- 13.Ricco JB, Illuminati G, Bouin-Pineau MH, Demarque C, Camiade C, et al. Early carotid endarterectomy after a nondisabling stroke: a prospective study. Ann Vasc Surg. 2000;14:89–94. doi: 10.1007/s100169910016. [DOI] [PubMed] [Google Scholar]
- 14.Wolfle KD, Pfadenhauer K, Bruijnen H, Becker T, et al. Early carotid endarterectomy in patients with a nondisabling stroke: results of a retrospective analysis. Vasa. 2004;33:30–5. doi: 10.1024/0301-1526.33.1.30. [DOI] [PubMed] [Google Scholar]
- 15.Rockman CB, Maldonado TS, Jacobowitz GR, Cayne NS, Gagne PJ, Riles TS. Early carotid endarterectomy in symptomatic patients is associated with poorer perioperative outcomes. J Vasc Surg. 2006;44:480–7. doi: 10.1016/j.jvs.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 16.de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of Rankin ‘handicap’ grades after stroke. Stroke. 1995;26:2027–30. doi: 10.1161/01.str.26.11.2027. [DOI] [PubMed] [Google Scholar]
- 17.Kastrup A, Ernemann U, Nagele T, Groschel K. Risk factors for early recurrent cerebral ischemia before treatment of symptomatic carotid stenosis. Stroke. 2006;37:3032–4. doi: 10.1161/01.STR.0000248968.86868.f3. [DOI] [PubMed] [Google Scholar]
- 18.Intercollegiate Working Party for Stroke. National Clinical Guidelines for Stroke. London: Royal College of Physicians; 2000. [Google Scholar]
- 19.Department of Health. National service framework for older people. London: DH; 2001. < www.dh.gov.uk>. [Google Scholar]
- 20.Castaldo JE, Nelson JJ, Reed JF, 3rd, Longenecker JE, Toole JF. The delay in reporting symptoms of carotid artery stenosis in an at-risk population. The Asymptomatic Carotid Atherosclerosis Study experience: a statement of concern regarding watchful waiting. Arch Neurol. 1997;54:1267–71. doi: 10.1001/archneur.1997.00550220067016. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health. National stroke strategy. London: DH; 2007. < www.dh.gov.uk>. [Google Scholar]