Abstract
Background
Effective smoking cessation for youth is urgently needed, but the literature guiding such efforts is nascent. We evaluated the implementation of a proactive intervention for adolescent smoking cessation that incorporated motivational interviewing (MI) and cognitive behavioral skills training (CBST).
Methods
We proactively identified 1058 smokers via classroom survey of enrolled juniors in 25 experimental high schools. After parental consent was obtained, trained counselors telephoned participants to invite their participation and deliver personalized smoking cessation counseling that combined MI and CBST. Implementation quality was assessed via weekly supervision of counselors, monitoring of counselor adherence to protocol via review of 5% of each counselor’s calls, and formal evaluation of counselor fidelity to MI via review of a random sample of 19.8% of counseling calls using the Motivational Interviewing Treatment Integrity Code.
Results
Among identified smokers, 948 (89.6%) were eligible for intervention by age (≥18 years) or parental consent, 736 (70%) agreed to participate in telephone counseling, 691 (65%) completed one or more counseling calls, and 499 (47%) completed all planned calls. Telephone delivery of the personalized MI and CBST counseling intervention to a general population of adolescents was done with greater than 90% adherence to the intervention protocol. Review of the random sample of counselors’ calls demonstrated that more than 85% of counselors’ calls met or exceeded benchmark scores for four of six evaluated behaviors: MI spirit (99.1%), empathy (96.2%), ratio of reflections to questions (97.2%), and MI adherent (85.7%).
Conclusion
An effective proactive telephone counseling intervention consisting of MI and CBST can be successfully implemented with reach and fidelity in a general population of adolescent smokers.
CONTEXT AND CAVEATS
Prior knowledge
Recruitment of adolescent participants in clinical trials of smoking cessation has been difficult because of several effectiveness barriers, including lack of motivation, lack of skills to quit, using smoking to reduce stress, and life transitions.
Study design
A personalized counseling smoking cessation intervention of motivational interviewing and cognitive behavioral skills training by telephone was developed and used on more than 1000 high school senior smokers who were proactively identified as high school juniors in 25 schools. Quality of implementation was evaluated.
Contributions
Of the smokers identified, nearly half completed all intervention calls. The intervention was executed with more than 90% adherence to the intervention protocol and more than 85% of counselors met or exceeded behavioral benchmark scores.
Implications
A smoking cessation intervention of personalized telephone counseling using motivational interviewing and cognitive behavioral skills training can be used in a general population of adolescent smokers.
Limitations
In some cases, counselors failed to initially contact, to recontact and initiate telephone counseling, and to recontact participating smokers.
From the Editors
In an accompanying article in this issue of the Journal, we report the results of the Hutchinson Study of High School Smoking (HS), a group-randomized trial in adolescent smoking cessation. In this trial, a proactive intervention approach that used personalized smoking cessation telephone counseling for smoking cessation reached 65% of all smokers in a general population of adolescents. The HS intervention produced statistically significant positive treatment effects for multiple abstinence endpoints, all measured more than 12 months after randomization, including 6-month prolonged abstinence among daily smokers (1). The magnitudes of the treatment effects achieved for 30- and 7-day abstinence at 12 months of follow-up (1) were roughly three times the overall treatment effect reported in a recent meta-analysis of 48 adolescent smoking cessation trials (2).
In light of the HS intervention's success in reaching teens and increasing smoking cessation, and in response to multiple calls for researchers to describe their methods and report their process results (3–9), we describe the intervention's theoretical rationale and therapeutic basis, present individual intervention strategies aimed at overcoming research-identified barriers to both reach and effectiveness, and report implementation process results. Finally, we discuss how approaches used in this intervention may be more widely used in other interventions for young people.
Barriers to Reach and Effectiveness
One barrier to reach has been the failure to provide privacy or to convince teen smokers that their privacy is protected (5,10–14). Adolescent smokers do not want their smoking status revealed to parents, teachers, and others—a concern that can be exacerbated when parental consent for adolescent participation is required or when cessation programs are conducted during or after school or as group sessions. In these settings, it is impossible to conceal participants’ smoking status from school personnel and to guarantee the confidentiality of what is said within the group (14). Another recruitment barrier is adolescents’ desire for independence and for making their own decisions. For many teens, smoking cessation programs represent “nagging,” “judging,” “preaching,” and “pushing” (13,15)—the antithesis of independence. Finally, many teens lack enthusiasm for, and harbor misperceptions about, potentially helpful cessation strategies, and still others simply do not know that help is available or where to find it (11,13,15–19).
These barriers to recruitment and retention can also limit teens’ willingness to engage in the constructive dialogue essential for interventions to be effective. But there are other impediments to effectiveness, many of which are associated with the unique characteristics of adolescents and their smoking habits. For example, many teens smoke less often than daily and do not think of themselves as smokers or do not view their smoking as a problem requiring assistance (5,7,19,20). They also underestimate the addictive potential of nicotine—evidence suggests that a large proportion of adolescent smokers are dependent on nicotine (21)—and overestimate their ability to quit at any time (22). For these smokers, cessation messages hold little relevance (13,15,19,23,24). Other effectiveness barriers include adolescents’ lack of motivation to quit, their lack of knowledge and skills for quitting, and their use of smoking to manage stress and negative emotions (25). Finally, the life transitions of older adolescence and emerging adulthood—transitions to higher education, jobs, independent living arrangements, new social networks, and “adult” relationships and responsibilities—present both opportunities and barriers to smoking abstinence (26–29).
Subjects and Methods
Protection of Human Subjects
The HS intervention design, procedures, and materials met project and Federal requirements for sensitive and respectful treatment of study participants and were reviewed and approved in advance and annually by the Hutchinson Center's Institutional Review Board. The trial is registered on ClinicalTrials.gov, identifier: NCT00115882.
Conceptual Basis of the Smoking Cessation Intervention
Social Cognitive Theory (SCT) (30) guided the development of the HS cessation intervention. SCT describes a dynamic ongoing process in which personal factors (including cognitions), human behavior, and the environment exert influence on each other (30). Personal factors influencing smoking cessation include the adolescent's valuation of quitting, expectations about the positive and negative consequences of smoking and quitting, and belief in her or his own ability to quit, that is, quitting self-efficacy. Behavioral factors influencing cessation include the number and level of refusal and cessation skills that the adolescent has mastered. Environmental influences include family members, peers, and the media that, through modeling, influence the development of an adolescent's own smoking practices, attitudes, and perceptions of social norms. Consistent with SCT, the HS intervention seeks to change participants’ smoking and quitting outcome expectancies, quitting self-efficacy, quitting outcome expectations, behavioral capability, and perceptions of social norms (31–34).
Intervention Therapeutic Modalities
Acknowledging that both motivation and skills are critical for achieving behavior change, the HS intervention incorporates two therapeutic modalities: motivational interviewing (MI) and cognitive behavioral skills training (CBST).
Motivational Interviewing.
Because the HS trial aimed to proactively recruit all at-least-monthly smokers to the intervention, it was important to consider the motivation of infrequent smokers and those not interested in quitting. MI was chosen as the primary therapeutic modality for the HS cessation intervention because of its emphasis on the client and a minimally prescriptive style that seemed appropriate for adolescents who value their independence and want their choices to be respected. As defined by its originators, MI is “a client-centered directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence” (35,36). It seeks to mobilize the client's inner resources to help her or him resolve ambivalence about behavior change and trigger a decision to change and to empathically and strategically support and strengthen the client's commitment to change (35,36). The HS telephone counseling intervention used a broad menu of MI strategies (eg, reflective listening, open-ended questions, summarizing) appropriate for exploring concerns about smoking, avoiding conflict with clients, minimizing resistance, supporting self-efficacy and optimism for change, and strategically exploring cognitive discrepancies. The aims were to emphasize the importance of quitting, increase participants’ confidence in their ability to do so, resolve ambivalence, and trigger a quit attempt. These core MI processes are used to target multiple SCT mechanisms. For example, outcome expectancies for quitting (ie, the values that the individual places on quitting) are addressed by assessing importance for stopping smoking, creating discrepancy, and using reflective statements, including strategic reflection of feelings and values, to promote intrinsic motivations and self-initiated rewards for quitting.
Cognitive Behavioral Skills Training.
CBST was used to help those participants who want to quit but lack the skills and/or the confidence to do so. CBST seeks to help individuals build skills for quitting and preventing relapse through such counseling processes as suggesting self-talk strategies, offering strategies to cope with anticipated internal (eg, stress) and external (eg, friends’ smoking) triggers to smoke, and collaborating on a plan for stopping (37). Skills training was used primarily to target the SCT processes of behavioral capability (ie, the individual's knowledge and skills for quitting) and quitting self-efficacy (ie, the individual's confidence in her or his ability to quit). In the HS intervention, CBST was applied in a manner consistent with MI's strategies and empathic therapeutic style; for example, maladaptive cognitions are gently challenged, often by reference to the adolescent's own, other statements (38,39), and advice is offered only with the participant's permission. Maintaining MI's empathic, respectful, and caring style allows adolescents control over their treatment, helps increase their self-efficacy, and reinforces their accomplishments—all of which contribute to sustaining long-term change (39). Furthermore, the intervention's use of MI with skills training complies with current guidelines for treatment of tobacco dependence among unmotivated smokers (40), is consistent with the intervention's conceptual framework, and strategically addresses barriers to intervention reach and effectiveness.
Intervention Components and Sequence
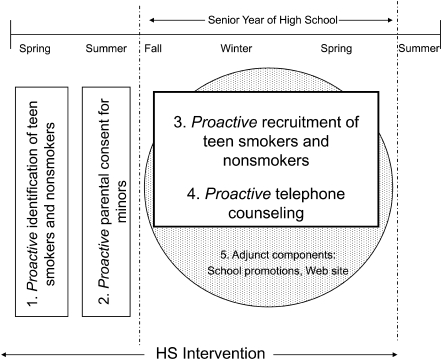
To increase intervention reach and effectiveness, the main components and sequence of the HS intervention encompassed 1) identification of all smokers within the general population of teens, 2) obtaining active consent from parents of minors, 3) recruitment of (experimental) smokers to the HS intervention, and 4) delivery of proactive telephone counseling (Figure 1). These four intervention components were designed to be conducted proactively to maximize reach and participation. Two adjunct intervention components supported the telephone counseling: school-based promotional (print) materials and an informational smoking cessation Web site for teens.
Figure 1.
Intervention components and sequence. HS = high school smoking.
Proactive Identification of Smokers.
The HS intervention began with the proactive identification of all (at-least-monthly) smokers among enrolled 11th graders in the 50 participating high schools (Figure 1). As previously described (41,42), students’ smoking status was determined by their responses to a (baseline) classroom survey administered by project staff to all juniors in the spring of their junior year. Staff informed students, “Some of you may be invited to participate in future research activities.” Also, the last page of the survey, which asked for future contact information, read, “We may invite some of you to take part in another activity” and “We’ll use the information below to contact you to see if you want to take part.” The strategy of partnering with schools was adopted to increase intervention reach: Schools provided the enrolled students’ contact information and were the setting for administration of the classroom survey. Proactive identification of smokers ascertains the number of smokers in the population, thus providing a critical denominator for assessing intervention reach. It also facilitates recruitment outreach and can yield participation rates higher than those achieved using standard methods that rely on teens to self-select for cessation counseling (42).
So that intervention contact and participation would not automatically label a teen as a smoker (14), a targeted sample of nonsmokers was also selected as eligible for intervention (41). Including nonsmokers also allowed the program to capitalize on, and build, peer support for quitting (16,43). This strategy has been endorsed by teens, who report being receptive to procedures that are inclusive of the general population, rather than restricted just to smokers (13).
Proactive Parental Consent.
Active parental consent was required for intervention participation by teens who were younger than 18 years (Figure 1). Parental consent was conducted after the baseline survey and before the scheduled senior-year intervention contact with teens. To ensure that parents actually received parental consent requests and had the opportunity to easily communicate their wishes, requests for written parental consent were mailed directly to parents. The request emphasized the intervention's inclusion of both nonsmokers and smokers and the confidential nature of all intervention conversations. Project staff telephoned parents who failed to return their postage-paid consent form to invite their questions and allow them to provide (or decline) verbal consent for their teen's participation.
This proactive parental consent procedure differs from common practice in three important respects: First, for the HS intervention, parental consent was conducted before rather than after any intervention recruitment with adolescents. This procedure eliminated the problem of recruited teens losing interest or dropping out after learning their parents must be consulted. Second, in obtaining parental consent, there was no involvement by school personnel or adolescents, thus ensuring that parents were notified, reducing the incentive for student forgery of consent documents, and not adding to the administrative burden of school systems. Third, consent via telephone was proactively pursued and accepted as an alternative to written consent. The failure of parents to respond to written requests for active parental consent has been associated with poor recruitment and loss of marginalized or high-risk populations (14,44–49). In contrast, use of researcher-initiated follow-up telephone calls to parents who do not respond to requests for written consent has been shown to improve parental consent response rates (45,50) and is acceptable to many schools and institutional review boards (51). Further supporting this procedure are studies showing that the majority of parents who fail to return written parental consent materials are latent consenters (44,52).
Proactive Recruitment of Teen Smokers and Nonsmokers.
Eligible for intervention during their senior year were all identified smokers (and selected nonsmokers) in the experimental high schools who were at least 18 years old or whose parents consented. To more easily manage intervention delivery, participants were assigned to one of six follow-up batches and individual participants within each batch were randomly assigned to counselors. The intervention start dates for each batch were then staggered, with a new batch released to counselors every 4 weeks, beginning at the start of the school year. When a participant became eligible for intervention, he or she was mailed an information letter and brochure describing the HS intervention. Within 2 weeks of this mailing, a trained counselor called the participant (Figure 1) to invite participation. During this call, teens were invited to share their frank and personal opinions and insights about smoking and nonsmoking and details of their unique situation with regard to smoking. The counselor conducted informed consent using a documented procedure, emphasizing that participation was voluntary and confidential, and inviting questions. The counselor stressed the value of learning each teen's honest opinions and experiences and emphasized that participation was not about being pressured to quit smoking, but that if a smoker became interested in quitting, the counselor would provide help and support. The strategies of recruiting teens through counselor-initiated telephone calls, and including program goals relevant to all teens regardless of their smoking status or readiness to quit (eg, learning each teen's opinions and experiences), were aimed at overcoming many teens’ reluctance to initiate smoking cessation counseling (13,15); ensuring privacy; and making participation easy, accessible, and relevant.
Proactive Telephone Counseling.
The centerpiece of the HS cessation intervention is proactive personalized telephone counseling. Delivery of smoking cessation counseling via the telephone has been found to be effective among adults (53–55) and, when used with teens, it addresses multiple well-documented recruitment and retention barriers: Telephone delivery makes smoking cessation counseling easily accessible to large numbers of teens—95% of US households have telephones (56). The telephone allows for private, confidential, one-to-one counseling, without involvement by parents, teachers, or other teens (3). Consistent with MI's emphasis on the client and supporting his or her personal choice goals and values (57), telephone delivery allows counselors to explore and focus on smoking cessation facilitators and barriers specific to the smoker, which is difficult to do in a group therapy setting. Finally, because the counselor does not share the smoker's possible ambivalence about initiating or following through with planned calls (58), proactive telephone outreach captures even precontemplative or infrequent smokers who would not initiate cessation counseling on their own (13,15,23).
Despite the many advantages of using the telephone to deliver smoking cessation counseling to teens, reaching participants by telephone has proved to be challenging in past studies (eg, 59,60). Therefore, the counseling protocol includes strategies aimed at increasing reach including scheduling appointments for “the next call,” not limiting the number of call attempts counselors can make to reach a participant, and using call record information to strategically time call attempts to participants who have missed appointments.
The HS Telephone Counseling Protocol.
The MI plus CBST telephone counseling intervention was adapted from the work of Miller and Rollnick (35,36), Marlatt and Gordon (37), and Baer et al. (38), and documented in a comprehensive semi-structured counseling protocol. The HS protocol outlines required call elements and provides a menu of options for successfully executing each element while focusing on the individual needs of the participant. For example, counselors can choose from lists of strategies for helping infrequent smokers; smokers addicted to nicotine; or smokers who use their smoking to control their emotions, manage stress, or treat negative affect. Use of a documented protocol provided constant and consistent clinical guidance to counselors while also providing them the flexibility needed to personalize the intervention to each participant. It also facilitated consistent program delivery across multiple counselors and provided standards for program evaluation and replication. (An abbreviated list of topics covered in the HS telephone counseling protocol, derived from the table of contents, is shown in Appendix 1.)
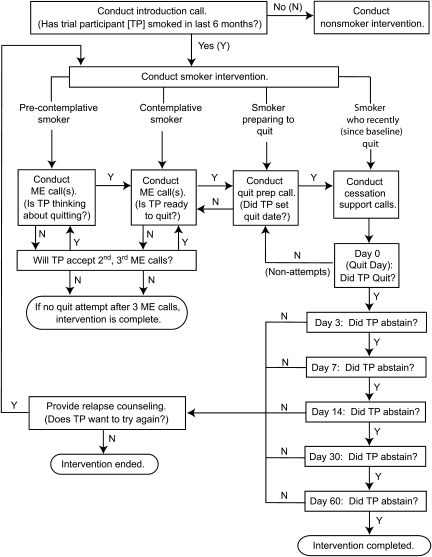
Once a teen agreed to participate, counseling typically began immediately during the initial (recruitment) call. The counselor assessed the participant's current smoking status (eg, “It would help me to know, do you currently smoke cigarettes?” and “When did you last smoke a cigarette?”) and, for smokers, readiness to quit (“Are you thinking about stopping in the next 6 months?” If yes, “Do you think you’ll be ready to stop in the next 30 days?”). Using this information on current smoking status, the counselor matched the individual to the appropriate phase of the telephone counseling, as directed by the protocol (Figure 2).
Figure 2.
Telephone counseling sequence and assignment to motivation enhancement (ME) and cessation support calls. N = no; Y = yes.
Current smokers who were not ready to quit were eligible to receive up to three consecutive motivation enhancement calls, designed to help them build intrinsic motivation and confidence to quit. Using MI, the counselor strategically led discussions with the goal of moving the smoker toward making a quit attempt; however, there was no preset timeline for the attempt to occur. The pace was set by the participant, as was the decision to quit. If after three consecutive motivational enhancement calls a smoker had not committed to making a quit attempt, his or her intervention was considered complete. The counselor thanked the participant, referred him or her to the HS Web site for additional information and help, and encouraged a call back (using the project's toll-free number) if the teen were to decide to quit during the current school year.
If during any intervention call, the smoker wanted to make a quit attempt, the counselor's focus shifted from building motivation and confidence to helping the smoker prepare to quit. At this point, the smoker was eligible for a quit preparation call, designed to strengthen commitment to change and build skills for smoking cessation. During a quit preparation call, the counselor used both MI and CBST to help the smoker build commitment to quitting and develop an action plan. The counselor and smoker brainstormed strategies for quitting and for coping with withdrawal or anticipated difficult situations (37). Following a quit preparation call, the counselor mailed the participant a quit kit, which contained a personal letter outlining the agreed upon plan for quitting, and materials designed to facilitate and inform the quit attempt: a copy of “BUTTsOUT-2,” a self-help guide to quitting smoking (developed and used successfully by the California Smokers’ Helpline), a water bottle, a Frisbee, a stress ball, and sugarless chewing gum and hard candy.
Once a quit attempt was scheduled (or the participant was found to already be actively engaged in quitting), the counselor began a series of up to six cessation support (CS) calls. CS calls incorporated both MI and CBST and followed a relapse-sensitive schedule (61) designed to support the smoker during the period in which physical and psychological withdrawal symptoms and cravings are strongest and the probability of relapse is greatest. The call schedule suggests calls to quitters on day 0 (the quit day), 3, 7, 14, 30, and 60 but was adjusted to the participant's schedule as needed. CS calls focused on building relapse prevention skills (37) while maintaining motivation and commitment for the quit attempt. In CS calls, the counselor encouraged the participant to report the extent to which she or he used the action plan, to evaluate its effectiveness, and to modify the plan as needed. The counselor helped the participant recognize successes and attribute them to his or her actions. To boost self-esteem, resolve any lingering ambivalence about quitting, and help the participant develop a self-image as a nonsmoker, counselors revisited motivation, confidence, and other issues as needed in response to participant feedback.
Any participant who reported at the initial counseling call that he or she did not currently smoke and had last smoked a cigarette 6 months ago or longer, received a nonsmoker call designed to provide positive reinforcement of the participant's abstinence choice and help build motivation and skills for supporting peers’ efforts to quit smoking. Although one counseling call was the norm, counselors would call back at the participant's request or would ask permission to call back if they judged the participant's commitment to remaining abstinent was weak.
Consistent with the principles of MI, the assignment of individuals to a smoker call vs a nonsmoker call was based on the smoking status information provided during the first telephone contact, rather than their smoking status reported approximately 9 months earlier on the baseline survey. Thus, some baseline smokers received the nonsmoker intervention and some baseline nonsmokers, found to be smoking at the first call, received the smoker intervention.
As guided by the protocol, the counselor mailed a brief personal letter (with the participant's permission and to the address of his or her choice) after each call, outlining major discussion points and planned next steps. Each letter was unique and included self-help materials as appropriate. For example, teens who set a quit date were sent a quit kit. Personalized written feedback and tailored print materials have demonstrated effectiveness as adjuncts to other intervention components (62,63); they enhance relevancy and provide a physical reminder to the smoker of the counseling conversation and of his or her responsibility for and control over the change process (64).
Adjunct Intervention Components.
In accordance with SCT's emphasis on the role of environmental influences, including peers, on the development of an adolescent's own smoking attitudes and practices (30), a (minimal) school-wide component was delivered to promote nonsmoking norms and encourage intervention participation (Figure 1). A staff member visited each experimental high school to inform the student leadership council and school faculty about their school's participation in the HS trial and to distribute and encourage student leaders’ use of project-supplied posters, brochures, and electronic media. These materials were designed to foster social norms supportive of tobacco-free choices. The school materials advertised the URL of the project's Web site for teens, designed to reinforce counseling messages, motivate and prepare for quit attempts, and provide relapse prevention assistance. Consistent with SCT, the Web site targeted smoking and quitting outcome expectancies, quitting self-efficacy, quitting outcome expectations, behavioral capability, and perceptions of social norms. Counselors routinely referred participants to the Web site. Message development for the intervention print materials and the Web site was guided by MI's client-centered approach, and both components incorporated CBST strategies.
Counselor Requirements, Training, and Supervision
Counselors were chosen in part for their suitability to work with older adolescents—their demonstrated respect for the privacy and rights of study participants, ability to easily and quickly develop rapport over the phone, genuine enjoyment in working with teens, and appreciation for teens’ capacity for change. All counselors had university bachelor's degrees and three had master's degrees (in social work or counseling). None had previous MI experience. Annual counselor staffing averaged 1.5 full-time-equivalent staff throughout implementation. Counselors typically worked half-time, with an average caseload of 165 participants per school year.
Each counselor completed 120 hours of in-house training, which was conducted by licensed clinical psychologists and senior staff. Psychologists and staff involved with MI training were members of the Motivational Interviewing Network of Trainers. Training covered brief MI, with a focus on establishing rapport and enhancing motivation, and CBST, as well as research participant rights and protections, the counseling process, adolescent patterns of tobacco use, nicotine dependence and withdrawal, other forms of tobacco use, and procedures for responding to teens in crisis. Training was interactive and made use of games and role playing and also required self-study in addition to the classroom hours.
Clinical supervision was provided by licensed clinical psychologists, who were members of Motivational Interviewing Network of Trainers and were experts in MI. Day-to-day supervision, including the monitoring of counselor productivity and timelines, was done by an experienced project manager. The team of counselors and supervisors met weekly throughout the trial to hone clinical skills, address participant issues, and assess progress. Selected audio recordings of counseling calls (recorded with participants’ permission) were reviewed for supervisor and counselor-peer discussion and feedback.
Protocol Adherence.
To supplement weekly supervision, during each intervention period, a minimum 5% random sample of each counselor's audio-recorded counseling calls was evaluated by the project manager for protocol adherence and completeness of process data collection. The random sample of 131 (7.7%) of the 1696 recorded calls included 12 initial calls, 44 motivation enhancement calls, 10 quit preparation calls, 18 CS calls, and 47 nonsmoker calls.
Evaluation of MI Fidelity.
To evaluate counselor fidelity to MI, a random sample of 106 recorded calls with 99 current smokers (44.4% women; 79.7% white; 51.1% were baseline daily smokers) was reviewed and coded by a trained independent rater using the Motivational Interviewing Treatment Integrity (MITI) Code, version 2.0 (65). The MITI code is an established tool for evaluating competence in the use of MI. It has been shown to be a good measure of treatment integrity for MI and is considered to be superior to existing measures when indicators of client behavior are not needed (66,67). It has two components: global assessments of counselor empathy and the spirit of MI, using an anchored 7-point Likert scale, and counts of MI-specific behaviors. A list of the measures used in the MITI code and their definitions are found in Appendix Table 1.
For global measures, the median and range were computed. For counts of MI-specific behaviors, the mean number of MI-relevant behaviors per call and the SD and range were computed. As recommended by the authors of the MITI Code (65), summary scores were computed from the frequency counts to assess treatment fidelity. All summary scores and global assessment scores were evaluated against established benchmarks for MI quality (65).
To monitor intrarater reliability and prevent coding drift, the rater—blind to her original codes—recoded a minimum 15% random sample of calls every 2 weeks, for a total of 21 (19.8%) previously coded calls recoded for quality control. The recodes were compared with original codes and reviewed with the project manager for discussion and resolution of differences. Intrarater reliability was estimated by computing intraclass correlation coefficients between the original codes and the recodes based on recommendations by Cicchetti (68). This analysis (data not shown) demonstrated that the rater's coding was reliable: 100% of global scores for empathy and MI spirit were within one point of the original score on recode and 74% matched exactly; 67% of behavior count coding was in the excellent range and 33% was in the good range, using Cicchetti's scoring system for evaluating the usefulness of intraclass correlation coefficients in clinical instruments (68).
Statistical Methods
Most of the statistics presented are simple descriptive values, for example, mean, median, and SD. Possible differences in intervention recruitment and retention rates by sex, baseline smoking frequency, and baseline smoking cessation stage of change were evaluated using the Cochrane–Armitage trend test (69). Confidence intervals (CIs) for evaluating possible differences by sex in call length were calculated using the t test for equality of means.
Implementation Process Results
Intervention Reach
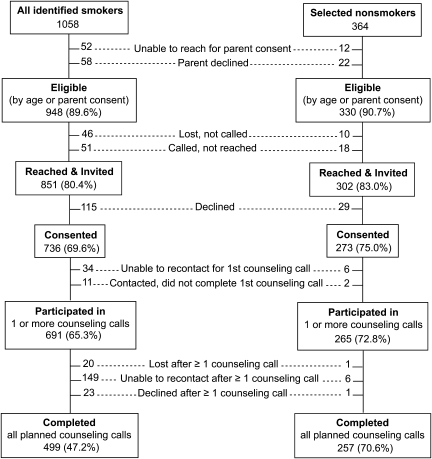
In the 25 experimental schools, 6144 (92.9%) of the 6616 enrolled high school juniors completed a baseline survey and 1058 (17.2%) of the 6144 did not decline future activities and identified themselves as smokers (42). Among those not declining, all identified smokers and 364 selected nonsmokers were targeted for intervention. Nearly three-quarters of identified smokers (779/1058) and selected nonsmokers (257/364) were younger than 18 years and thus required active parental consent for intervention participation. Consent was obtained from parents of 669 (85.9%) of the 779 minor-age smokers. Fewer than 10% of parents responded to written consent requests; the vast majority (77.9%) provided verbal consent in response to telephone outreach. As a result of the parental consent procedures, 89.6% (948/1058) of the targeted smokers and 90.7% (330/364) of nonsmokers were eligible for intervention.
Counselors successfully contacted 851 (89.8%) of the 948 intervention-eligible baseline smokers; 736 (86.5%) of the 851 contacted smokers agreed to participate, and 499 (72.2%) of the 691 of those participating in counseling completed all scheduled counseling calls (Figure 3). There was no evidence that rates of adolescent contact, consent, or participation differed by adolescent sex, baseline smoking frequency, or baseline stage of change in agreement with previous results (42). Intervention completion rates also did not differ by sex; however, there was a trend of lower intervention completion associated with higher baseline smoking frequency (P < .001) and increased intervention completion with baseline stage of change (P = .008), as evaluated and previously reported (42) using the Cochrane–Armitage trend test (69).
Figure 3.
Recruitment and participation by baseline smoking status.
The mean elapsed time between the baseline survey and the start of telephone counseling was 279 days (SD = 84.4) or about 9 months (Figure 1). Because smoking status can change over 9 months, the intervention was personalized to the participants’ smoking status at the first counseling call, instead of their baseline status. Among the 691 baseline smokers who started the intervention, 252 (36.5%) reported at their initial call that they had not smoked in the past 6 months; accordingly, they received the nonsmoker intervention. Similarly, among 266 baseline nonsmokers who received intervention, 20 (7.5%) reported smoking at the initial call and received the smoker intervention.
Characteristics of Phone Calls
Despite multiple strategies aimed at increasing reach, contacting teens by telephone required perseverance. The median elapsed time between when a participant became eligible for counseling and when he or she was reached by a telephone counselor was 21 days (mean ± SD, 41 ± 51.6 days). The rate of counseling call completion per telephone call attempt was only 9%. Also, 24.5% of participating baseline smokers (Figure 3) did not complete their intervention because counselors were unable to recontact them for scheduled calls or their telephone number became inactive and a new number could not be identified.
As previously described, intervention dose (number of scheduled counseling calls) was personalized to the participant's current smoking status, readiness to quit, and progress toward quitting. Participating smokers received an average of 2.83 calls (range: 1–9; median = 3), with a mean total intervention length of 36.58 minutes (SD = 30.17). Nonsmokers received an average of 1.18 calls (range: 1–3; median = 1), with a mean total intervention length of 9.54 minutes (SD = 5.47). There was no difference in mean or median number of telephone calls completed according to sex, and little difference in length of calls: Average length of calls to female and male smokers was 14.36 and 13.56 minutes, respectively, difference = 48 seconds (95% CI = −16 to 113 seconds). Because all HS counselors were female, no information is available about the relationship between counselor sex and call characteristics.
Mean length of calls to smokers was 13.93 minutes, SD = 9.34. Nonsmoker calls were intentionally shorter, with a mean length of 8.78 minutes, SD = 4.93. Overall, the mean length of individual intervention calls was 12.54 minutes, SD = 8.57. Calls to smokers varied in length by type of call. The longest calls were those involving quit preparation: Mean call lengths for an initial call transitioning to quit preparation and a motivational enhancement call transitioning to quit preparation were 20.42 minutes (SD = 12.34) and 24.69 minutes (SD = 14.49), respectively. Subsequent CS calls averaged 10.78 minutes (SD = 8.39). Mean length for motivational enhancement calls was 13.33 minutes (SD = 8.16).
Intervention Fidelity
Protocol Adherence.
Review of a random sample of the audio-recorded counseling calls (131 of 1696 calls) showed that counselors accurately assessed readiness to change in 92.9% of reviewed calls and administered the correct call type in 96.2% of calls. Counselors were found to have avoided protocol-prohibited behaviors in greater than 99% of reviewed calls. Counselors were rated as successfully engaged with participants in 98.5% of reviewed calls; they actively listened without pressuring the participant in 98.5% of calls and were found to have quickly established rapport in 96.9% of calls. Counselors mailed follow-up letters after 91.1% of calls. Their calls were on time for 73.2% of scheduled appointments.
Tone of call was assessed by rating the participant's level of engagement in the counseling conversation. In 93.9% of the reviewed calls, participants were actively engaged in counseling, willing to answer open questions and freely self-disclose. In none of the reviewed calls were the participants openly resistant (although this type of behavior was occasionally encountered during intervention implementation). In 6.1% of calls, participants were willing to provide answers to open questions but did not freely disclose personal information or seem effectively engaged.
Adherence to CBST-specific protocol guidelines was assessed among the sampled quit preparation and CS calls. Among 10 quit preparation calls reviewed, counselors established that the participant was ready for the quit attempt in 100% of calls, helped smokers set goals and assess abstinence challenges in 90% of calls, and helped smokers develop action plans in 80% of calls. Counselors helped the smoker set a quit date in 60% of the reviewed calls. Evaluation of adherence to protocol for the 18 CS calls demonstrated that counselors assessed participants’ progress with quitting in 100% of reviewed calls and assessed withdrawal symptoms in 78.9% of calls. They normalized withdrawal symptoms for 50% of participants reporting symptoms. Counselors helped participants evaluate the effectiveness of their quit strategies in 92.3% of calls, addressed refusal skills deficits in 68.4% of the calls, and examined slips and relapse situations in 100% of calls. Among the CS calls reviewed, 88% adhered to the relapse-sensitive call schedule.
Among the 47 nonsmoker calls in the sample, counselors supported and reinforced the participant's abstinence choice in 97.8% of calls, built motivation for helping peers to stop smoking in 93.3% of calls, and helped nonsmokers develop helping skills in 70.5% of calls.
Evaluation of MI Fidelity.
Evaluation of MI fidelity using the MITI Code is presented in Table 1; shown for both the global scores and the behavior summary scores are the benchmark scores, the average ratings of fidelity, and the percentage of reviewed calls achieving or exceeding the fidelity benchmarks. For the two global scores, 96.2% of calls achieved or exceeded the proficiency benchmark for empathy and 99.1% achieved or exceeded benchmark for MI spirit. Median ratings for empathy and MI spirit were 6, indicating advanced proficiency. For the four summary behavior scores, 97.2% of calls achieved or exceeded the benchmark for ratio of reflections to questions and 85.7% of calls achieved or exceeded benchmark for percent MI adherent. Much fewer calls met the benchmarks for percent open questions (25.2%) and percent complex reflections (18.9%).
Table 1.
Achievement of motivational interviewing quality benchmarks*
| Behavior indicator | Benchmark† | Rating | Calls achieved or exceeded benchmark, % (N = 106) |
| Empathy | 5 | 6 (median) | 96.2 |
| Spirit | 5 | 6 (median) | 99.1 |
| Ratio of reflections to questions‡ | 1 | 2.74 | 97.2 |
| % Open questions§ | 50 | 43.2 | 25.2 |
| % Complex reflections║ | 40 | 26.4 | 18.9 |
| % MI adherent¶ | 90 | 89.2 | 85.7 |
CQ = closed questions; CR = complex reflections; MI = motivational interviewing; MiA = MI adherent; MiNa = MI nonadherent; OQ = open questions; Q = questions; R = reflections; SR = simple reflections.
Benchmarks shown are for “beginning proficiency” and are as per the Motivational Interviewing Treatment Integrity Code, version 2.0 (65).
Rz(CQ + OQ).
OQ/(CQ + OQ).
CR/(SR + CR).
MiA/(MiA + MiNa). MiA code is reserved for instances where an utterance was an especially good example of MI adherent behavior such that it substantially contributed to the counselor–participant exchange. MiNa code is used to capture those counselor behaviors that are inconsistent with an MI approach, for example, advising, confronting, and directing.
Discussion
Building on the important work of earlier adolescent smoking cessation studies, the HS intervention addressed barriers to intervention reach and effectiveness. The trial successfully recruited more than 65% of targeted smokers in a general population of adolescents compared with the 2%–10% of smokers who are typically recruited to school-based smoking cessation programs (5). The HS intervention was implemented via telephone by trained counselors, with fidelity to core principles of MI and adherence to the MI plus CBST treatment protocol, and yielded statistically significant increases in smoking abstinence at 12 months postintervention eligibility (1).
This trial's positive results from an intervention with a major MI component contribute to the field of MI intervention research. At the time this intervention was being developed, studies of MI in brief telephone counseling for smoking cessation had been tested successfully with both contemplative and precontemplative adults (70,71) and showed promise for use with adolescents (64,72). Since then, results of studies of MI for adolescent and young adult smoking cessation have been mixed: In a trial of 85 non–treatment-seeking adolescent daily smokers, Colby et al. (73) reported statistically significant increases in 7-day abstinence at 6-month follow-up with one session of MI compared with standard brief advice. However, three other adolescent cessation trials (74–76) and one trial of young adult smokers (77) testing MI reported no statistically significant differences in cessation rates. Prokhorov et al. (78) tested MI with expert system-generated feedback against standard advice in a randomized trial of 426 daily-smoking college students; higher 7-day quit rates at 10-month follow-up were suggestive of a treatment effect (P = .068). Hollis et al. (79) also tested an expert system consisting of behavioral counseling that incorporated MI in a trial of 2526 adolescents (589 smokers) and observed statistically significantly higher 30-day abstinence rates at the 1- and 2-year follow-ups in the intervention arm. Results of a large randomized trial by the California Smokers’ Helpline, comparing telephone counseling that integrated MI and cognitive behavioral therapy with written materials vs written materials alone, showed that statistically significantly more clients in the telephone counseling group than in the control group quit and remained abstinent for 6 months (80). More recently, Pbert et al. (81,82) reported statistically significant 6-month treatment effects for 30-day abstinence in their trial of 2711 adolescent smokers and nonsmokers who received a smoking prevention or cessation intervention based on the 5A model that incorporated MI and cognitive behavioral therapy compared with those who received usual pediatric care. Now the HS trial has reported statistically significant treatment effects for multiple abstinence outcomes, including 6-month prolonged abstinence among baseline daily smokers (P = .02) (1). This trial's results, combined with the long-term results of the trials by Pbert et al. (81) and Hollis et al. (79), support the effectiveness of adolescent smoking cessation incorporating MI.
That the telephone counseling was delivered with fidelity to MI core elements enhances the internal validity of the intervention. Few studies of MI report evaluations of treatment fidelity (83). One possible reason may be that most MI interventions evaluated to date have tested MI in combination with other treatment modalities, for example, providing problem feedback or skills training (83). When the integrity of such interventions is examined, limited resources may preclude evaluation of all components. It is often the component considered most central to the intervention, such as the 5A model as described in Pbert et al. (82), that is assessed, rather than the core elements of MI (67). Unfortunately, without evaluations of adherence to MI, accurate conclusions cannot be drawn regarding the efficacy of MI interventions nor can their contributions to behavior change be fully understood.
For reasons beyond those established at the outset of the trial, including the nonsmoker intervention proved valuable. The irregular smoking patterns of adolescent smokers (5,7,20,22–24) and their proclivity for spontaneously starting and stopping smoking is well documented (eg, 84). Perhaps because of these characteristics, and the 9-month lapsed time between the trial's baseline survey and intervention contact, 36% of the baseline smokers subsequently reported at their initial counseling call that they currently did not smoke and had not smoked in the past 6 months. Possible explanations for the change in reported status include that participants had 1) accurately reported quitting since their baseline survey; 2) not reported their smoking status accurately, either to the counselors or on their baseline survey; or 3) smoked but because of the infrequency of their smoking did not consider themselves to be smokers. Regardless of the cause for the discrepancy, it proved important that there was a nonsmoker intervention available for these baseline smokers turned nonsmokers. For this reason, and because including nonsmokers in the intervention can help prevent stigmatization of smokers, researchers should consider the potential benefits of including a nonsmoker component when developing adolescent smoking cessation interventions.
Limitations specific to intervention design and implementation include counselor failure to initially contact 97 (10.2%) of the 948 eligible smokers, failure to recontact and initiate telephone counseling with 34 (3.6%) consented smokers, and failure to recontact 169 (17.8%) participating smokers for some of their scheduled calls. Further efforts are needed to continue to improve methods for contacting, engaging, and keeping adolescents in effective interventions. Another possible limitation is the 9-month gap, because of study design, between determination of the adolescents’ baseline smoking status and start of their intervention, during which time changes in adolescents’ smoking status occurred. Finally, that counselors did not achieve benchmark quality scores on two of six core behaviors of MI may limit somewhat our conclusions about MI fidelity.
Many of the approaches used successfully in this trial may be transferable to other interventions for young people and to other settings. For example, the methods for collection of active parental consent can be applied widely to other interventions involving minors. The proactive identification and recruitment of adolescents within a specific population, used with schools in this trial, can be applied in other settings as well: Both Hollis et al. (79) and Pbert et al. (81) proactively identified and recruited teen smokers and nonsmokers in health-care settings. Proactive telephone counseling and use of MI plus skills training, used in the HS intervention, can be used in other settings and for other behavior change applications. Evaluations of such use are strongly encouraged.
It will be important to follow up these promising results with additional research. First, it is essential to replicate the results of this intervention in other populations and settings and to evaluate modifications that could strengthen the intervention, both for reach and for effectiveness. Second, learning whether MI and CBST counseling processes predict smoking cessation outcomes would also be scientifically useful. Third, intervention modifications should be studied that would facilitate wide dissemination, for example, evaluation of a more limited counselor training protocol with both professional and lay counselors and evaluation of additional methods for proactively identifying smokers for cessation counseling. Similarly, before the HS intervention is considered for use with adolescents by existing tobacco quitlines, evaluation of the MI plus CBST telephone counseling component in a reactive quitline setting may be useful. Because counselor behavior that is consistent with MI has been shown to be positively associated with therapeutic alliance and treatment engagement (85), another possible future area of investigation is examination of effect of counselor behavior on intervention recruitment and retention.
Experience with the HS intervention demonstrates that telephone-based smoking cessation interventions that address research-identified challenges and barriers can be developed and successfully implemented with adolescent smokers. Moreover, proactive implementation of such interventions can extend intervention reach and achieve statistically significant rates of smoking abstinence in a large general population of adolescent smokers, thus contributing to national public health goals to reduce smoking among the US population of adolescents and young adults.
Funding
National Cancer Institute (CA082569 to A.V.P.).
Appendix 1:
Topics Addressed in the High School Smoking Telephone Counseling Protocol
- Background
- Overview of the Hutchinson Study of High School Smoking
- Intervention premises and goals
- Intervention challenges and strategies
- Approaches and models used in the intervention
- Smoking acquisition among high school students
The Proactive Telephone Counseling Intervention
Successfully contacting trial participants
Counselor mailings to participants
Building interest, rapport, motivation for future calls
- Initial call
- Informed consent
- Seeking personal opinions and insights
- Assessing current smoking and readiness to quit
- Motivation enhancement (ME) calls
- Assess participant's unique smoking situation
- Building importance and confidence
- Recognizing readiness to change
- Cessation support: Preparing to Quit (aka Quit Preparation or QP)
- Assess participant's unique smoking situation
- Strengthening commitment to change
- Negotiate an action plan
- Cessation support: Relapse Preventions (CS)
- Assess quit status/progress
- Discuss and normalize withdrawal symptoms
- Examine slip/relapse situations
- Evaluate effectiveness of coping strategies; revise action plan as needed
- Revisit (as needed) self-efficacy, motivation, confidence, social support, costs/benefits, self-image
- Non-attempts
- Intervention for nonsmokers
- Support participant's choice to be smoke-free
- Enhance motivation; build skills for helping smoking peers to quit
- Protection of Human Subjects in Research
- Training in human subjects protections
- Informed consent (parental consent, student consent)
- Confidentiality and limits of confidentiality
Procedures for response to imminent and nonimminent risk situations
Appendix Table 1.
Definitions of measures used in MI fidelity assessment*
| Measure | Definition |
| Empathy | The extent to which the therapist understands and/or makes an effort to grasp the client's perspective. |
| Spirit | The therapist's overall competence in using motivational interviewing, particularly with regard to the characteristics of evocation, collaboration, and autonomy. |
| Giving information | Therapist gives information, educates, provides feedback, or discloses personal information in the course of counseling the participant. |
| Giving protocol-specific information† | Therapist gives information or asks questions that are required by the research intervention protocol, for example, asks if participant has enough privacy to talk on the phone about his or her smoking. |
| Open questions | Questions that allows a wide range of possible answers. |
| Closed questions | Questions that can be answered with a “yes” or “no” response or with a very limited range of responses. |
| Closed clarifying questions† | Questions asked immediately following a reflection, used to confirm its accuracy in the absence of visual cues. (New category added to track use of this counselor behavior when working with teens over the phone.) |
| Reflections turned into closed questions (R to Q)† | Statements that otherwise meet the criteria for a reflection but are spoken with an inflection at the end so that they “sound like” questions. (New category added to track use of this counselor behavior when working with teens over the phone.) |
| Simple reflections | Reflective listening statements that convey understanding or facilitate communication but add little or no meaning or emphasis. |
| Complex reflections | Reflective listening statements that add meaning or emphasis to what clients have said. |
| MI adherent‡ | Coding category reserved for coding counselor utterances that are especially good examples of the 10 designated MI behaviors in that they substantially contribute to some aspect of the counselor–participant exchange; good MiA behaviors that do not meet the high threshold are coded using the 10 behavior codes. |
| MI nonadherent‡ | Coding category used to capture those counselor behaviors that are inconsistent with a motivational interviewing approach, for example, advising, confronting, and directing. |
MI = motivational interviewing; Q = questions; R = reflections; MiA = MI adherent.
Adaptations to the Motivational Interviewing Treatment Integrity Code specific to this study.
Because of high threshold for use of this code, it was not used for every call.
Footnotes
The sponsors took no role in the study design, the collection or analysis of the data, the interpretation of the results, the preparation of the manuscript, or the decision to submit the manuscript for publication.
We acknowledge with deep appreciation the high school seniors (now young adults) who participated in this intervention and are grateful for their willingness to share their unique insights and opinions about smoking and not smoking and for allowing us to support their efforts to quit smoking. We also acknowledge the advice and guidance provided by Consultant Shu-Hong Zhu, PhD, during development of the telephone counseling intervention and the skills and exceptional dedication of the counselors who delivered it: Melissa M. Phares, MSW, Jennifer Mullane, MEd, Sarah Stivers, and Karin R. Riggs, MSW.
References
- 1.Peterson AV, Kealey KA, Mann SL, et al. Group-randomized trial of a proactive, personalized telephone counseling intervention for adolescent smoking cessation. J Natl Cancer Inst. 2009 doi: 10.1093/jnci/djp317. doi:10.1093/jnci/djp317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychol. 2006;25(5):549–557. doi: 10.1037/0278-6133.25.5.549. [DOI] [PubMed] [Google Scholar]
- 3.Backinger CL, Michaels CN, Jefferson AM, Fagan P, Hurd AL, Grana R. Factors associated with recruitment and retention of youth into smoking cessation intervention studies—a review of the literature. Health Educ Res. 2008;23(2):359–368. doi: 10.1093/her/cym053. doi:10.1093/her/cym053. [DOI] [PubMed] [Google Scholar]
- 4.Sussman S. Effects of sixty-six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tob Induc Dis. 2002;1(1):35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Backinger CL, McDonald P, Ossip-Klein DJ, et al. Improving the future of youth smoking cessation. Am J Health Behav. 2003;27(suppl 2):S170–S184. [PubMed] [Google Scholar]
- 6.McDonald P, Colwell B, Backinger CL, Husten C, Maule CO. Better practices for youth tobacco cessation: evidence of review panel. Am J Health Behav. 2003;27(suppl 2):S144–S158. doi: 10.5993/ajhb.27.1.s2.5. [DOI] [PubMed] [Google Scholar]
- 7.Mermelstein R, Colby SM, Patten C, et al. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine Tob Res. 2002;4(4):395–403. doi: 10.1080/1462220021000018470. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, GA: USDHHS, PHS, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994. [Google Scholar]
- 9.Sussman S, Dent CW, Lichtman KL. Project EX: outcomes of a teen smoking cessation program. Addict Behav. 2001;26(3):425–438. doi: 10.1016/s0306-4603(00)00135-0. [DOI] [PubMed] [Google Scholar]
- 10.McCormick LK, Crawford M, Anderson RH, Gittelsohn J, Kingsley B, Upson D. Recruiting adolescents into qualitative tobacco research studies: experiences and lessons learned. J Sch Health. 1999;69(3):95–99. doi: 10.1111/j.1746-1561.1999.tb07215.x. [DOI] [PubMed] [Google Scholar]
- 11.Massey CJ, Dino GA, Horn KA, Lacey-McCracken A, Goldcamp J, Kalsekar I. Recruitment barriers and successes of the American Lung Association's Not-On-Tobacco Program. J Sch Health. 2003;73(2):58–63. doi: 10.1111/j.1746-1561.2003.tb03573.x. [DOI] [PubMed] [Google Scholar]
- 12.Gillespie A, Stanton W, Lowe JB, Hunter B. Feasibility of school-based smoking cessation programs. J Sch Health. 1995;65(10):432–437. doi: 10.1111/j.1746-1561.1995.tb08208.x. [DOI] [PubMed] [Google Scholar]
- 13.Balch GI. Exploring perceptions of smoking cessation among high school smokers: input and feedback from focus groups. Prev Med. 1998;27(5, pt 2):A55–A63. doi: 10.1006/pmed.1998.0382. [DOI] [PubMed] [Google Scholar]
- 14.Moolchan ET, Mermelstein R. Research on tobacco use among teenagers: ethical challenges. J Adolesc Health. 2002;30(6):409–417. doi: 10.1016/s1054-139x(02)00365-8. [DOI] [PubMed] [Google Scholar]
- 15.Balch GI, Tworek C, Barker DC, Sasso B, Mermelstein RJ, Giovino GA. Opportunities for youth smoking cessation: findings from a national focus group study. Nicotine Tob Res. 2004;6(1):9–17. doi: 10.1080/1462200310001650812. [DOI] [PubMed] [Google Scholar]
- 16.Patten CA, Lopez K, Thomas J, et al. Reported willingness among adolescent nonsmokers to help parents, peers, and others to stop smoking. Prev Med. 2004;39(6):1099–1106. doi: 10.1016/j.ypmed.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 17.Leatherdale ST, McDonald PW. What smoking cessation approaches will young smokers use? Addict Behav. 2005;30(8):1614–1618. doi: 10.1016/j.addbeh.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald S, Rothwell H, Moore L. Getting it right: designing adolescent-centered smoking cessation services. Addiction. 2007;102(7):1147–1150. doi: 10.1111/j.1360-0443.2007.01851.x. [DOI] [PubMed] [Google Scholar]
- 19.Amos A, Wiltshire S, Haw S, McNeill A. Ambivalence and uncertainty: experiences of and attitudes towards addiction and smoking cessation in the mid-to-late teens. Health Educ Res. 2006;21(2):181–191. doi: 10.1093/her/cyh054. [DOI] [PubMed] [Google Scholar]
- 20.Mermelstein R. Teen smoking cessation. Tob Control. 2003;12(suppl 1):i25–i34. doi: 10.1136/tc.12.suppl_1.i25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colby SM, Tiffany ST, Shiffman S, Niaura RS. Are adolescent smokers dependent on nicotine? A review of the evidence. Drug Alcohol Depend. 2000;59(suppl 1):S83–S95. doi: 10.1016/s0376-8716(99)00166-0. [DOI] [PubMed] [Google Scholar]
- 22.Al-Delaimy WK, White MM, Pierce JP. Adolescents’ perceptions about quitting and nicotine replacement therapy: findings from the California Tobacco Survey. J Adolesc Health. 2006;38(4):465–468. doi: 10.1016/j.jadohealth.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Baillie L, Lovato CY, Johnson JL, Kalaw C. Smoking decisions from a teen perspective: a narrative study. Am J Health Behav. 2005;29(2):99–106. doi: 10.5993/ajhb.29.2.1. [DOI] [PubMed] [Google Scholar]
- 24.Kishchuk N, Tremblay M, Lapierre J, Heneman B, O’Loughlin J. Qualitative investigation of young smokers’ and ex-smokers’ views on smoking cessation methods. Nicotine Tob Res. 2004;6(3):491–500. doi: 10.1080/14622200410001696565. [DOI] [PubMed] [Google Scholar]
- 25.Mermelstein R. The Tobacco Control Network Writing Group. Explanations of ethnic and gender differences in youth smoking: a multi-site, qualitative investigation. Nicotine Tob Res. 1999;1(suppl 1):S91–S98. doi: 10.1080/14622299050011661. [DOI] [PubMed] [Google Scholar]
- 26.Bricker JB, Peterson AV, Jr, Leroux BG, Andersen MR, Rajan KB, Sarason IG. Prospective prediction of children's smoking transitions: role of parents’ and older siblings’ smoking. Addiction. 2006;101(1):128–136. doi: 10.1111/j.1360-0443.2005.01297.x. [DOI] [PubMed] [Google Scholar]
- 27.Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD, Schulenberg JE. Smoking, Drinking, and Drug Use in Young Adulthood: The Impacts of New Freedoms and New Responsibilities. Mahwah, NJ: Lawrence Erlbaum Associates; 1997. [Google Scholar]
- 28.Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- 29.Tercyak KP, Rodriguez D, Audrain-McGovern J. High school seniors’ smoking initiation and progression 1 year after graduation. Am J Public Health. 2007;97(8):1397–1398. doi: 10.2105/AJPH.2006.094235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 31.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: W.H. Freeman & Co; 1997. [Google Scholar]
- 33.Mackay PW, Donovan DM, Marlatt GA. Cognitive behavioral approaches to alcohol abuse. In: Frances RJ, Miller SI, editors. Clinical Textbook of Addictive Disorders. New York, NY: Guilford Press; 1991. pp. 452–481. [Google Scholar]
- 34.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research and Practice. 3rd ed. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 35.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: The Guilford Press; 1991. [Google Scholar]
- 36.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 37.Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behavior. New York, NY: The Guilford Press; 1985. [Google Scholar]
- 38.Baer JS, Kivlahan DR, Donovan DM. Integrating skills training and motivational therapies: Implications for the treatment of substance dependence. J Subst Abuse Treat. 1999;17(1–2):15–23. doi: 10.1016/s0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- 39.DiClemente CC, Velasquez MM. Motivational interviewing and the stages of change. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: The Guilford Press; 2002. pp. 209–216. [Google Scholar]
- 40.Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. [Google Scholar]
- 41.Liu J, Peterson AV, Kealey KA, Mann SL, Bricker JB, Marek PM. Addressing challenges in adolescent smoking cessation: design and baseline characteristics of the HS group-randomized trial. Prev Med. 2007;45(2–3):215–225. doi: 10.1016/j.ypmed.2007.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kealey KA, Ludman EJ, Mann SL, et al. Overcoming barriers to recruitment and retention in adolescent smoking cessation. Nicotine Tob Res. 2007;9(2):257–270. doi: 10.1080/14622200601080315. [DOI] [PubMed] [Google Scholar]
- 43.Stanton WR, McGee R. Adolescents’ promotion of nonsmoking and smoking. Addict Behav. 1996;21(1):47–56. doi: 10.1016/0306-4603(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 44.Baker JR, Yardley JK, McCaul K. Characteristics of responding-, nonresponding- and refusing-parents in an adolescent lifestyle choice study. Eval Rev. 2001;25(6):605–618. doi: 10.1177/0193841X0102500602. [DOI] [PubMed] [Google Scholar]
- 45.Dent CW, Sussman SY, Stacy AW. The impact of a written parental consent policy on estimates from a school-based drug-use survey. Eval Rev. 1997;21(6):698–712. doi: 10.1177/0193841X9702100604. [DOI] [PubMed] [Google Scholar]
- 46.Esbensen FA, Miller MH, Taylor TJ, He N, Freng A. Differential attrition rates and active parental consent. Eval Rev. 1999;23(3):316–335. doi: 10.1177/0193841X9902300304. [DOI] [PubMed] [Google Scholar]
- 47.Pokorny SB, Jason LA, Schoeny ME, Townsend SM, Curie CJ. Do participation rates change when active consent procedures replace passive consent? Eval Rev. 2001;25(5):567–580. doi: 10.1177/0193841X0102500504. [DOI] [PubMed] [Google Scholar]
- 48.Severson HH, Ary DV. Sampling bias due to consent procedures with adolescents. Addict Behav. 1983;8(4):433–437. doi: 10.1016/0306-4603(83)90046-1. [DOI] [PubMed] [Google Scholar]
- 49.Severson H, Biglan A. Rationale for the use of passive consent in smoking prevention research: politics, policy and pragmatics. Prev Med. 1989;18(2):267–279. doi: 10.1016/0091-7435(89)90074-1. [DOI] [PubMed] [Google Scholar]
- 50.Moberg DP, Piper DL. Obtaining active parental consent via telephone in adolescent substance abuse prevention research. Eval Rev. 1990;14(3):315–323. [Google Scholar]
- 51.Ellickson PL. Getting and keeping schools and kids for evaluation studies. J Community Psychol. 1994;(CSAP special issue):102–116. [Google Scholar]
- 52.Ellickson PL, Hawes JA. An assessment of active vs passive methods for obtaining parental consent. Eval Rev. 1989;13(1):45–55. doi: 10.1177/0193841X8901300104. [DOI] [PubMed] [Google Scholar]
- 53.Rabius V, McAlister AL, Geiger A, Huang P, Todd R. Telephone counseling increases cessation rates among young adult smokers. Health Psychol. 2004;23(5):539–541. doi: 10.1037/0278-6133.23.5.539. [DOI] [PubMed] [Google Scholar]
- 54.Stead LF, Perea R, Lancaster T. Telephone counseling for smoking cessation [review] Cochrane Database Sys Rev. 2006 doi: 10.1002/14651858.CD002850.pub2. (3):CD002850. doi:10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 55.An LC, Zhu S-H, Nelson DB, et al. Benefits of telephone care over primary care for smoking cessation: a randomized trial. Arch Intern Med. 2006;166(5):536–542. doi: 10.1001/archinte.166.5.536. [DOI] [PubMed] [Google Scholar]
- 56.U.S. Census Bureau. American Community Survey. 2005. Detailed Tables. http://factfinder.census.gov. Accessed November 27, 2006. [Google Scholar]
- 57.Baer JS, Peterson PL. Motivational interviewing with adolescents and young adults. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: The Guilford Press; 2002. pp. 320–332. [Google Scholar]
- 58.Zhu S-H, Tedeschi GJ, Anderson CM, Pierce JP. Telephone counseling for smoking cessation: what's in a call? J Couns Dev. 1996;75(2):93–102. [Google Scholar]
- 59.Elder JP, Woodruff SI, Eckhardt L. Participation in a telephone-based tobacco use prevention program for adolescents. Am J Health Promot. 1994;9(2):92–96. doi: 10.4278/0890-1171-9.2.92. [DOI] [PubMed] [Google Scholar]
- 60.Smith PM, Cameron R, McDonald PW, Kawash B, Madill C, Brown KS. Telephone counseling for population-based smoking cessation. Am J Health Behav. 2004;28(3):231–241. doi: 10.5993/ajhb.28.3.4. [DOI] [PubMed] [Google Scholar]
- 61.Zhu S-H, Pierce JP. A new scheduling method for time-limited counseling. Prof Psychol Res Pr. 1995;26(6):624–625. [Google Scholar]
- 62.Curry SJ, Wagner EH, Grothaus LC. Evaluation of intrinsic and extrinsic motivation interventions with a self-help smoking cessation program. J Consult Clin Psychol. 1991;59(2):318–324. doi: 10.1037//0022-006x.59.2.318. [DOI] [PubMed] [Google Scholar]
- 63.Skinner CS, Campbell MK, Rimer BK, Curry SJ, Prochaska JO. How effective is tailored print communication? Ann Behav Med. 1999;21(4):290–298. doi: 10.1007/BF02895960. [DOI] [PubMed] [Google Scholar]
- 64.Lawendowski LA. A motivational intervention for adolescent smokers. Prev Med. 1998;27(5, pt 2):A39–A46. doi: 10.1006/pmed.1998.0424. [DOI] [PubMed] [Google Scholar]
- 65.Moyers TB, Martin T, Manuel JK, Miller WR. The Motivational Interviewing Treatment Integrity (MITI) Code (version 2.1), 2003. http://www.motivationalinterviewing.org/. Accessed August 17, 2006. [Google Scholar]
- 66.Pierson HM, Hayes SC, Gifford EV, et al. An examination of the Motivational Interviewing Treatment Integrity Code. J Subst Abuse Treat. 2007;32(1):11–17. doi: 10.1016/j.jsat.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 67.Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 68.Cicchetti DV. Guidelines, criteria and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. [Google Scholar]
- 69.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11(3):375–386. [Google Scholar]
- 70.Zhu S-H, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64(1):202–211. doi: 10.1037//0022-006x.64.1.202. [DOI] [PubMed] [Google Scholar]
- 71.Curry SJ, McBride C, Grothaus LC, Louie D. A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol. 1995;63(6):1005–1014. doi: 10.1037//0022-006x.63.6.1005. [DOI] [PubMed] [Google Scholar]
- 72.Colby SM, Monti PM, Barnett NP, et al. Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psychol. 1998;66(3):574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- 73.Colby SM, Monti PM, Tevyaw TO, et al. Brief motivational intervention for adolescent smokers in medical settings. Addict Behav. 2005;30(5):865–874. doi: 10.1016/j.addbeh.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 74.Kelly AB, Lapworth K. The HYP program—targeted motivational interviewing for adolescent violations of school tobacco policy. Prev Med. 2006;43((6)):466–471. doi: 10.1016/j.ypmed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 75.Horn K, Dino G, Hamilton C, Noerachmanto N. Efficacy of an emergency department-based motivational interviewing teenage smoking intervention. Prev Chronic Dis. 2007;4(1):1–12. www.cdc.gov/pcd/issues/2007/jan/06_0021.htm. Accessed September 1, 2008. [PMC free article] [PubMed] [Google Scholar]
- 76.Brown RA, Ramsey SE, Strong DR, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tob Control. 2003;12(suppl IV) doi: 10.1136/tc.12.suppl_4.iv3. iv3–iv10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McCambridge J, Strang J. Development of a structured generic drug intervention model for public health purposes: a brief application of motivational interviewing with young people. Drug Alcohol Rev. 2003;22(4):391–399. doi: 10.1080/09595230310001613903. [DOI] [PubMed] [Google Scholar]
- 78.Prokhorov AV, Yost T, Mullin-Jones M, et al. “Look at your Health”: outcomes associated with a computer-assisted smoking cessation counseling intervention for community college students. Addict Behav. 2008;33(12):757–771. doi: 10.1016/j.addbeh.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hollis JF, Polen MR, Whitlock EP, et al. Teen reach: outcomes from a randomized, controlled trial of a tobacco reduction program for teens seen in primary medical care. Pediatrics. 2005;115(4):981–989. doi: 10.1542/peds.2004-0981. doi: 10.1542/peds.2004-0981. [DOI] [PubMed] [Google Scholar]
- 80.Tedeschi GJ, Zhu S-H, Anderson CM, Cummins S, Ribner NG. Putting it on the line: telephone counseling for adolescent smokers. J Couns Dev. 2005;83(4):416–424. [Google Scholar]
- 81.Pbert L, Flint AJ, Fletcher KE, Young MH, Druker S, DiFranza JR. Effect of a pediatric practice-based smoking prevention and cessation intervention for adolescents: a randomized controlled trial. Pediatrics. 2008;121(4):738–747. doi: 10.1542/peds.2007-1029. [DOI] [PubMed] [Google Scholar]
- 82.Pbert L, Fletcher KE, Flint AJ, Young MH, Durker S, DiFranza JR. Smoking prevention and cessation intervention delivery by pediatric providers, as assessed with patient exit interviews. Pediatrics. 2006;118(3):810–824. doi: 10.1542/peds.2005-2869. [DOI] [PubMed] [Google Scholar]
- 83.Burke BL, Arkowitz H, Dunn C. The efficacy of motivational interviewing and its adaptations. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: The Guilford Press; 2002. pp. 217–250. [Google Scholar]
- 84.Pallonen UE. Transtheoretical measures for adolescent and adult smokers: similarities and differences. Prev Med. 1998;27(5, pt 3):A29–A38. doi: 10.1006/pmed.1998.0423. [DOI] [PubMed] [Google Scholar]
- 85.Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? J Subst Abuse Treat. 2005;31(4):329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]