Abstract
Objective: A retrospective review of patients with malignant neoplasms of the hypopharynx treated with combined surgery and radiotherapy is presented to highlight the results of treatment and the factors of treatment success for this malignant disease.
Patients and Methods: Between 1995 and 2004 at the University ORL Clinic Nis 89 patients with malignant neoplasms of hypopharynx (85 males, 4 females, and age ranging from 44 to 77 years) were treated. In the 89 patients (stage I, n = 4; stage II, n = 3; stage III, n = 34; stage IV, n = 48), the sites of origin were pyriform sinus (n = 75), postcrycoid (n = 8), posterior pharyngeal wall (n = 3) and superior hypopharynx (n = 3).
Results: Laryngeal preservation surgery was achieved in 11.2% of patients, while 88.8% had laryngectomy with partial or total pharyngectomy. Pyriform sinus was the most common site of origin of hypopharyngeal carcinoma in 84.3%. Totally 93% of patients had neck metastases, and tumors extended beyond the hypopharynx in 41.6% of patients. TNM stage was highly significant parameter of outcome. Five year survival was 100% for stage I, 66.6% for stage II, 53.9% for stage III, and 33.3% for stage IV. Residual disease (5.6%) and recurrent disease (2.2%) were low. Postoperative fistula developed in 16.8% of patients, and in 60% it was closed successfully using local flaps, while in 40% pectoralis flap was needed. Localization of disease was also an important factor of survival. Retrocrycoid carcinoma resulted in very poor survival rate (12.5%), high residual disease, lymph node metastasis, and pharyngocutaneous fistula formation.
Conclusion: Localization and TNM stage are highly significant factors for clinical course, treatment, and outcome of hypopharyngeal carcinoma.
Keywords: hypopharynx, squamous cell carcinoma surgery, five year survival
Hypopharynx is the area of the pharynx that lies below the oropharynx, and it is visually inaccessible by routine office examination. Hypopharyngeal cancers are usually aggressive in behavior, they grow in a region of abundant lymphatic drainage, they do not produce specific early symptoms or signs, and usually occur in people who are nutritionally depleted and immunologically compromised. It is not surprising, then, that the survival rates for these cancers are poor1,2.
The management of malignant neoplasms of hypopharynx and cervical esophagus remains difficult despite recent advances in surgical techniques, as well as multidisciplinary treatment programs. Regardless of the type of therapy employed, high recurrence rates, poor survival, and significant alterations in speech and swallowing functions are common experience for patients with malignancies in these anatomic sites. Despite these facts, patients are potentially curable and must be offered regimens that carefully consider morbidity and outcome within the context of the patients overall medical condition3,4.
A retrospective review of 89 patients with malignant neoplasms of hypopharynx treated with combined surgery and radiotherapy is presented to highlight the results and factors of outcome of treatment for this malignant disease.
Patients and Methods
At the University ORL Clinic Nis in the period between 1995 and 2004 totally 89 previously untreated patients with squamous cell carcinoma of the hypopharynx were included in this study. There were 85 males, and 4 females. The age of patients ranged from 44 to 77 years.
A complete medical history and careful head and neck examination was performed for assessment. Staging was made with help of computed tomography (extent of disease at the primary site, status of lymph nodes in the neck, and evaluation for metastatic disease).
Most of the patients were presented with advanced stage of disease (stage I, n = 4; stage II, n = 3; stage III, n = 34; stage IV, n = 48). The sites of origin were pyriform sinus (n = 75), postcrycoid area (n = 8), posterior pharyngeal wall (n = 3) and superior hypopharynx (n = 3).
Surgery was the primary treatment modality. Laryngeal function preservation was possible in 10 patients, while in others total laryngectomy with partial or total pharyngectomy were performed. All patients had 55-75 Gy radiotherapy after the surgery. Reconstruction of defect was performed using remaining mucosa, and pectoralis flap was used in 5.6% of patients.
The follow up period was five years. Survival rate, residual and recurrent disease, lymph node metastasis, pharyngocutaneous fistula and other changes were noted, and compared statistically. Paired t test was used to investigate the differences between groups of patients (p value less than 0.05 denoted the presence of a statistically significant difference).
Results
The principal signs and symptoms of patients with carcinoma of hypopharynx were dysphagia, hoarseness, odynophagia, neck mass, weight loss, and hemoptysis or hematemesis.
In our study the most common site of origin of malignancies within the hypopharynx was the pyriform sinus in 84.3%. Totally 93% of patients either presented with or developed neck metastases during their course of treatment. Tumors extended beyond the hypopharynx in significant number of patients at initial presentation (41.6%).
TNM stage was very significant parameter of outcome. Five year survival was 100% for stage I, 66.6% for stage II, 53.9% for stage III, and 33.3% for stage IV. Both tumor size and lymph node involvement were significant. Residual disease (5,6%) and recurrent disease (2.2%) were low. However, subsequent lymph node metastasis was frequent, presenting in 22.5%, and was an important factor for decreased five year survival. In three patients massive arterial bleeding occurred. It was successfully treated by urgent revision surgery.
Postoperative fistula developed in 16.8% of patients, only in stage III and IV of disease. In 60% it was closed successfully using local flaps, while in 40% pectoralis flap was used.
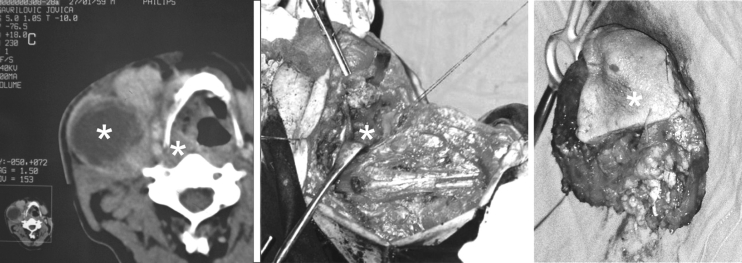
Localization of disease was also an important factor. Since the most of tumors were primarily located in pyriform sinus their characteristics and outcome of therapy predominate. Retrocrycoid carcinoma resulted in very poor survival rate (12.5%), high residual disease, lymph node metastasis, and pharyngocuraneous fistula formation (Table. 1-4, Figure 1-7).
Table 1. Overall results of treatment of hypopharyngeal carcinoma and T stage.
Table 4. Overall results of treatment of hypopharyngeal carcinoma and localization of disease.
Figure 1. Five year survival rate for hypopharyngeal carcinoma and T stage (Kaplan Meir).
Figure 7. Reconstruction of pharyngocutaneous fistula with pectoralis flap: fistula, pectoralis flap, suture with two skin layers, final outlook.
Discussion
Hypopharyngeal cancers have extensive submucosal spread, and high risk of nodal involvement. Treatment approach for hypopharyngeal carcinoma requires a motivated, compliant patient, careful monitoring, and close interdisciplinary cooperation among oncologists1,2.
Despite increasing use of laryngeal preserving protocols, laryngopharyngectomy remains the gold standard treatment for locally advanced hypopharyngeal and upper oesophageal tumours and for salvage following failed chemoradiotherapy. Improved perioperative medical care and experience in reconstruction have reduced mortality and improved functional outcomes5
The standard operative procedure is laryngopharyngoesophagectomy and reconstruction with regional musculocutaneous flaps when needed. Surgical resection for advanced stage primary tumors (T3 or T4) typically requires laryngectomy as part of the procedure. Larynx is removed because of direct or submucosal tumor extension and significant risk of chronic aspiration. Histopathologic studies of hypopharyngeal cancer have shown that assessment of the extent of laryngeal disease based on endoscopic findings in the hypopharynx is inaccurate6. Therefore, laryngeal conservation surgery for hypopharyngeal cancer risks a high incidence of positive margins. However, laryngeal conservation surgery is possible even in T3-4 stage in patients who have no involvement of contralateral larynx, no invasion to esophagus, and no deglutition difficulty, and without decrease of survival rate7-11.
Retrocrycoid carcinoma is particularly difficult to treat. Free jejunal flaps are usually used for reconstruction with early fistulas (33%), and late strictures (33%). On the other side gastric pull-up patients have fewer fistulas but more number of chest complications. Most of the patients with gastric pull-up tolerated solid diet and 43% of them managed oesophageal speech, while the remainder uses an electrolarynx4.
The pectoralis myofascial flap covering the pharyngeal sutures in postradiotherapy laryngectomy is particularly useful in a selected group of patients, such as diabetes mellitus, history of vascular disease or poor nutritional status12. Near-total laryngectomy, circular pharyngectomy with tracheopharyngeal shunt and jejunal free-flap repair offers good voice rehabilitation without impairing swallowing function13. Hypopharyngeal reconstruction with an laryngotracheal flap is effective method with reduced postoperative complications14.
Postoperative radiation therapy has been shown to improve 5-year survival rates, decrease the rates of local and regional recurrence, including peristomal recurrence7,8. Side effects include mucositis, cutaneous reactions, neutropenia, thrombocytopenia, sepsis and death12.
Chemotherapy in the management of hypopharyngeal tumors has evolved in the last decade from palliation to primary combined-modality treatment8,9. Current clinical data support a role for chemotherapy as part of a combination treatment for cure in patients with advanced hypopharyngeal cancer requiring total laryngectomy, or who are unfit for or refuse surgery9. Clinical studies have confirmed better results when chemotherapy and radiotherapy are combined with surgery, than without surgery2,5,7,9,10.
TNM category-based head and neck cancer stage grouping systems have the ability to create clinically relevant prognostic groups of patients with cancer of the hypopharynx. Other staging systems were also proposed for improvement of prognostic ability using hazard consistency, hazard discrimination, percent variance explained, and outcome prediction15. Stage (T-stage, N-stage, over-all stage grouping), and age influence outcome significantly. In some studies the 3-year loco-regional control for T1-T2 disease was 49.7% versus 43.1% for T3-T4 stage. Stage and age remain the most important determinants of outcome2.
No significant differences in 5-year survival, and in disease-free interval was found when using concomitant chemo- and radiotherapy before and after total laryngectomy, partial pharyngectomy, and radical neck dissection, and the patients with surgery and radiotherapy. The prognosis of advanced hypopharyngeal carcinoma remains poor despite treatment with an intensified multimodality protocol. Therefore, the therapeutic strategy should be to individualize treatment with the goal of preserving laryngeal function and optimizing postoperative quality of life3.
Some analyses found that after curative treatment 20% patients had residual disease, recurrences tended to appear in the first year and 50% of first recurrences included metastases. Overall, 47% of patients were disease free at 3 years but eventually 64% of patients died of their cancer11. Dysphagia is the first sign of recurrence and can precede clinically detectable recurrent tumors by several months
The level of cervical lymph node metastasis is the only independent prognostic factor in overall survival, disease-specific survival, and relapse-free survival14. Perineural invasion, vascular invasion, positive nodal status, extracapsular spread, contralateral, bilateral or fixed nodes, level IV to V positive nodes, and N2 disease are all significant predictors of lower survival, higher incidence of neck recurrences, greater risk of distant metastases, and poorer outcome16-19.
Collected current medical references indicate that the survival of patients with carcinoma of the hypopharynx and cervical esophagus remains poor in spite of multimodality treatment. The mean survival following diagnosis is usually less than 20 months and cumulative 5-year survival is less than 20 percent for advanced disease. Failure to control local disease remains a major cause of death in these patients. Locoregional control affects the risk of distant metastases, and tumors of the hypopharynx have a higher probability of micrometastatic dissemination at the time of initial diagnosis. For all head and neck tumor sites, except for the hypopharynx and nasopharynx, improvements in locoregional control are likely to improve survival. Until effective methods to treat disseminated disease and second primary malignancies are developed, improvements in locoregional control will have little effect on ultimate survival for patients with hypopharynx and cervical esophagus malignancies20-23.
For patients with pharyngeal carcinoma, the healthrelated quality of life at diagnosis is an important factor for the prognosis23.
In our study TNM stage and localization of hypopharyngeal carcinoma were highly significant factor for the outcome of disease. Presented data are comparable to other statistics. Prevention and early diagnosis are thus the most important facts ENT surgeons should focus on
Basic investigations in head and neck oncogenesis, such as influence of papilloma virus and other factors, could contribute to prevention of hypopharyngeal malignant tumors24
Conclusion
The most common site of origin of hypopharyngeal carcinoma was the pyriform sinus in 84.3%. Totally 93% of patients either presented with or developed neck metastases. Tumors extended beyond the hypopharynx in 41.6% of patients at initial presentation. TNM stage was very significant parameter of outcome. Five year survival was 100% for stage I, 66.6% for stage II, 53.9% for stage III, and 33.3% for stage IV. Residual disease (5,6%) and recurrent disease (2.2%) were low. Postoperative fistula developed in 16.8% of patients, only in stage III and IV of disease. In 60% it was closed successfully using local flaps, while in 40% pectoralis flap was used. Localization of disease was also an important factor. Retrocrycoid carcinoma resulted in very poor survival rate (12.5%), high residual disease, and lymph node metastasis, and pharyngocutaneous fistula formation.
Figure 2. Five year survival rate for hypopharyngeal carcinoma and N stage (Kaplan Meir).
Figure 3. Five year survival rate for hypopharyngeal carcinoma and stage of disease (Kaplan Meir).
Figure 4. Five year survival rate for hypopharyngeal carcinoma and localisation (Kaplan Meir).
Figure 5. Retrocrycoid carcinoma: CT findings, excised tumor with larynx, intraoperative defect with esophagostoma ready for reconstruction.
Figure 6. Hypopharyngeal carcinoma with cervical metastasis: CT, intraoperative view, excised tumor.
Table 2. Overall results of treatment of hypopharyngeal carcinoma and N stage.
Table 3. Overall results of treatment of hypopharyngeal carcinoma and stage of diseas.
References
- 1.Hinerman RW, Amdur RJ, Mendenhall WM, Villarent DB, Robbins KT, et al. Hypopharyngeal carcinoma. Curr Treat Options Oncol. 2002;3:41, 49. doi: 10.1007/s11864-002-0040-1. [DOI] [PubMed] [Google Scholar]
- 2.Gupta T, Chopra S, Agarwal JP, et al. Squamous cell carcinoma of the hypopharynx: single-institution outcome analysis of a large cohort of patients treated with primary non-surgical approaches. Acta Oncol. 2009;48:541–548. doi: 10.1080/02841860802488839. [DOI] [PubMed] [Google Scholar]
- 3.Windfuhr JP, Andrae M, Chen YS, Makoski HB, Schroder M, Sesterhenn K. Results after intensified therapy for advanced carcinoma of the hypopharynx. Ear Nose Throat J. 2008;87:E11. [PubMed] [Google Scholar]
- 4.Iseli TA, Agar NJ, Dunemann C, Layons BM. Functional outcomes following total laryngopharyngectomy. ANZ J Surg. 2007;77:954, 957. doi: 10.1111/j.1445-2197.2007.04289.x. [DOI] [PubMed] [Google Scholar]
- 5.Lavertu P, Adelstein DJ, Saxton JP, et al. Aggressive concurrent chemoradiotherapy for squamous cell head and neck cancer: an 8-year single-institution experience. Arch Otolaryngol Head Neck Surg. 1999;125:142, 148. doi: 10.1001/archotol.125.2.142. [DOI] [PubMed] [Google Scholar]
- 6.Hirano M, Kurita S, Tanaka H. Histopathologic study of carcinoma of the hypopharynx: implications for conservation surgery. Ann Otol Rhinol Laryngol. 1987;96:625, 629. doi: 10.1177/000348948709600602. [DOI] [PubMed] [Google Scholar]
- 7.Persky MS, Daly JF. Combined therapy vs curative radiation in the treatment of pyriform sinus carcinoma. Otolaryngol Head Neck Surg. 1981;89:87–91. doi: 10.1177/019459988108900119. [DOI] [PubMed] [Google Scholar]
- 8.Arriagada R, Eschwege F, Cachin Y, Richard JM. The value of combining radiotherapy with surgery in the treatment of hypopharyngeal and laryngeal cancers. Cancer. 1983;51:1819–1825. doi: 10.1002/1097-0142(19830515)51:10<1819::aid-cncr2820511011>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 9.Pfister DG, Shaha AR, Harrison LB. The role of chemotherapy in the curative treatment of head and neck cancer. Surg Oncol Clin N Am. 1997;6:749, 768. [PubMed] [Google Scholar]
- 10.Zelefsky MJ, Kraus DH, Pfister DG, et al. Combined chemotherapy and radiotherapy versus surgery and post-operative radiotherapy for advanced hypopharyngeal can-cer. Head Neck. 1996;18:405, 411. doi: 10.1002/(SICI)1097-0347(199609/10)18:5<405::AID-HED3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 11.Hall SF, Groome PA, Irish J, et al. The natural history of patients with squamous cell carcinoma of the hypopharynx. Laryngoscope. 2008;118:1362–1371. doi: 10.1097/MLG.0b013e318173dc4a. [DOI] [PubMed] [Google Scholar]
- 12.Righini C, Lequeux T, Cuisnier O, et al. The pectoralis myofascial flap in pharyngolaryngeal surgery after radiotherapy. Eur Arch Otorhinolaryngol. 2005;262:357–61. doi: 10.1007/s00405-004-0827-8. [DOI] [PubMed] [Google Scholar]
- 13.Temam S, Janot F, Germain M, et al. Functional results with advanced hypopharyngeal carcinoma treated with circular neartotal pharyngolaryngectomy and jejunal free-flap repair. Head Neck. 2006;28:8–14. doi: 10.1002/hed.20286. [DOI] [PubMed] [Google Scholar]
- 14.Chu PY, Chang SY. Reconstruction after resection of hypopharyngeal carcinoma: comparison of the postoperative complications and oncologic results of different methods. Head Neck. 2005;27:901–908. doi: 10.1002/hed.20262. [DOI] [PubMed] [Google Scholar]
- 15.Hall SF, Groome PA, Irish J, et al. TNM-based stage groupings in head and neck cancer: application in cancer of the hypopharynx. Head Neck. 2009;31:1–8. doi: 10.1002/hed.20917. [DOI] [PubMed] [Google Scholar]
- 16.Fagan JJ, Collins B, Barnes L, et al. Perineural invasion in squamous cell carcinoma of the head and neck. Arch Oto-laryngol Head Neck Surg. 1998;124:637–640. doi: 10.1001/archotol.124.6.637. [DOI] [PubMed] [Google Scholar]
- 17.Leibel SA, Scott CB, Mohiuddin M, et al. The effect of localregional control on distant metastatic dissemination in carcinoma of the head and neck: results of an analysis from the RTOG head and neck database. Int J Radiat Oncol Biol Phys. 1991;21:549–556. doi: 10.1016/0360-3016(91)90669-u. [DOI] [PubMed] [Google Scholar]
- 18.Chu PY, Li WY, Chang SY. Clinical and pathologic predictors of survival in patients with squamous cell carcinoma of the hypopharynx after surgical treatment. Ann Otol Rhinol Laryngol. 2008;117:201–206. doi: 10.1177/000348940811700307. [DOI] [PubMed] [Google Scholar]
- 19.Lee MS, Ho HC, Hsiao SH, et al. Treatment results and prognostic factors in locally advanced hypopharyngeal cancer. Acta Otolaryngol. 2008;128:103–109. doi: 10.1080/00016480701387116. [DOI] [PubMed] [Google Scholar]
- 20.Mc Murtrie A, Georgeu GA, Kok K, et al. Novel method of closing a tracheo-oesophageal fistula using a de-epithelialized deltopectoral flap. J Laryngol Otol. 2005;119:129–131. doi: 10.1258/0022215053420086. [DOI] [PubMed] [Google Scholar]
- 21.Ozer E, Grecula JC, Agrawal A, et al. Intensification regimen for advanced-stage resectable hypopharyngeal carcinoma. Arch Otolaryngol Head Neck Surg. 2006;132:385–389. doi: 10.1001/archotol.132.4.385. [DOI] [PubMed] [Google Scholar]
- 22.Santos AB, Cernea CR, Inoue M, et al. Selective neck dissection for node-positive necks in patients with head and neck squamous cell carcinoma: a word of caution. Arch Otolaryngol Head Neck Surg. 2006;132:79–81. doi: 10.1001/archotol.132.1.79. [DOI] [PubMed] [Google Scholar]
- 23.Nordgren M, Jannert M, Boysen M, et al. Health-related quality of life in patients with pharyngeal carcinoma: A five-year follow-up. Head Neck. 2006;28:339–349. doi: 10.1002/hed.20334. [DOI] [PubMed] [Google Scholar]
- 24.Sujanen S. Human papilloma virus (HPV) in head and neck cancer. J Clin Virol. 2005;32:S59–S66. doi: 10.1016/j.jcv.2004.11.017. [DOI] [PubMed] [Google Scholar]