Abstract
Background and aim: To present our experience with unexpected findings during hernia surgery, either unusual hernial contents or pathologic entities, like neoplastic masses, masquerading as a hernia.
Patients and methods: We studied retrospectively 856 patients with inguinal hernia who were admitted to our surgical department over a 9-year period. In addition, our study included patients complaining of inguinal protrusion, even without a definitive diagnosis of inguinal hernia upon admission.
Results: Five patients presented with unusual hernial contents. Three of them had a vermiform appendix in their sac. Acute appendicitis (Amyands hernia) was found in only one case. One patient had epiploic appendagitis related with a groin hernia. Moreover, an adult woman was diagnosed with ovarian and tubal inguinal hernia. Finally, we report a case of a massive extratesticular intrascrotal lipoma, initially misdiagnosed as a scrotal hernia.
Conclusion: a hernia surgeon may encounter unexpected intraoperative findings. It is important to be prepared to detect them and apply the appropriate treatment.
Keywords: Amyand's hernia, epiploic appendagitis, ovarian and tubal hernia, inguinal mass, intrascrotal lipoma
Inguinal hernia repair is one of the most common operations in surgical practice. Yet, in spite of its great incidence, hernias often pose a surgical dilemma, even for the skilled surgeon1. The unexpected hernial content constitutes one of these cases. We report our experience with unusual hernial contents such as ovary, fallopian tube, epiploic appendagitis, vermiform appendix and acute appendicitis (Amyand's hernia). In addition, many pathologic entities can masquerade as inguinal hernia. It is important to be prepared to detect them and take the appropriate surgical decisions.
A retrospective review of the case histories of 856 inguinal hernia patients who were admitted to our department between 1998 and 2007 was undertaken. Information was obtained from their medical records and the documented operative findings. In addition, our study included patients complaining of inguinal protrusion, even without a definitive diagnosis of inguinal hernia upon admission, in an effort to present all the unexpected findings, true hernias or not, that a hernia surgeon may confront during her/his practice.
Cases description
Vermiform appendix in inguinal hernia sac
Vermiform appendix as a hernial sac content was identified in 3 patients (0.38%). One of them had acute appendicitis (Amyand's hernia) and presented as incarcerated right groin hernia. The two patients with normal appendix had a mesh hernia repair without appendicectomy. In the case of Amyands hernia, the patient underwent simultaneous appendicectomy and Bassini's suture hernia repair. Notably, since appendix seemed inaccessible through the neck of the sac, the hernia incision was extended superiorly. No postoperative infection or recurrence was reported.
Epiploic appendagitis in inguinal hernia sac
Epiploic appendagitis due to chronic torsion and inflammation secondary to an inguinal hernia occurred in one patient (0.12%) who was admitted with a 4-month history of a left groin lump. It caused only irritation symptoms and mass formation, without cough impulse. Intraoperatively, a thick hernia sac was found and opened. An inflamed, swollen epiploic appendage of the sigmoid colon, was identified (Figure 1). The sigmoid colon had normal appearance and was not found in the hernia sac. The epiploic appendage was resected and mesh-plug repair followed.
Figure 1: An inflamed appendage epiploica of the sigmoid colon, as a hernia sac content.

Ovary and fallopian tube in inguinal hernia sac
A 39-year-old woman was diagnosed having an ovarian and tubal inguinal hernia. It presented as irreducible indirect groin hernia. Surgical exploration revealed an edematous but still viable left fallopian tube and a normal ovary in the hernia sac (Figure 2). The tube and the ovary were replaced into the peritoneal cavity and mesh-plug repair was performed.
Figure 2: Ovarian and tubal inguinal hernia in an adult patient.

A massive extratesticular intrascrotal lipoma masquerading as an inguinal hernia
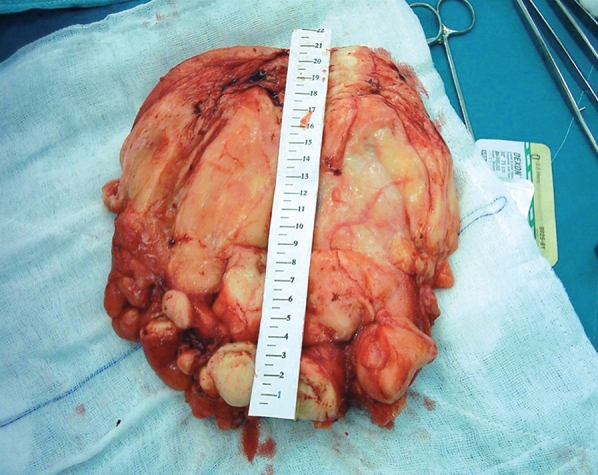
Another peculiar case was that of a massive primary lipoma of the scrotum, initially misdiagnosed as an inguinoscrotal hernia. Patient's chief complaint was swelling which was already present for the last eight years. Believing that he had a hernia, he did not seek any medical attention until its increase to a large-size mass. At clinical examination, an elastic, irreducible soft mass was palpated, without tenderness or transillumination. No bowel sounds were detected within the scrotum. Ultrasound and CT imaging demonstrated a solid mass, most probably a lipoma. The lesion was resected (Figure 3). It was adherent to the scrotal wall but easily separable from it. Testis, epididymis and spermatic cord were intact. The removed specimen measured 20166 cm and was enveloped into a membrane (Figure 4). The histopathology revealed a lipoma.
Figure 3: Massive intrascrotal extratesticular lipoma.

Figure 4: Massive intrascrotal extratesticular lipoma. The removed specimen.
Discussion
Although rare, a hernia sac may contain vermiform appendix and, exceptionally, acute appendicitis. De Garengeot first reported this finding in a femoral hernia sac2,in 1731. Subsequently, a voluminous literature evolved in which anatomists and surgeons recorded the availability of the appendix within the hernia sac. The first recorded appendicectomy was performed by Claudius Amyand in 1736 through a right inguinal hernia sac3–5. The patient was an 11-year-old boy with an appendiceal abscess in the scrotum. The operation was unsuccessful because of recurrent sepsis following the removal of the appendix and its contained foreign bodies.
Acute appendicitis within an inguinal hernia accounts for 0.1 % of all cases6. Inflammation of the appendix is attributed to the external compression of the appendix at the neck of the hernia. The inflammatory status of the vermiform appendix determines the surgical approach and the type of hernia repair. In the case of appendicitis due to the infective and inflammatory process, hernia repair should be performed without synthetic meshes and plugs within the defect. In the case of a normal appendix incidentally found within the sac, the addition of prophylactic appendicectomy to the hernia repair is not favoured. Appendicectomy adds the possibility of infection to an otherwise clean procedure. Superficial wound infection adds morbidity; deep infection may contribute to recurrence. In addition, surgical efforts to achieve visualization of the entire appendix, by enlarging the hernial defect or distending the neck of the sac, increase the possibility of recurrence, by weakening of the anatomic buttress around a rupture5.
The epiploic appendages are 2-5 cm long, fat-containing outpouchings of peritoneum of the large bowel, arranged to the tenia libera medially and to the tenia omentalis laterally. Epiploic appendages may be involved in a number of disease processes such as epiploic appendagitis due to torsion or venous occlusion or acute and chronic inflammation secondary to diverticulitis. When found in the inguinal hernia sac, the epiploic appendages may appear normal, hypertrophied, inflamed with diverticulitis, or strangulated with necrosis. Epiploic appendagitis as an inguinal hernia content is very rare. Only two cases have been reported in MEDLINE, one from Turkey7 and the other one from Russia8. Earlier cases on relation of epiploic appendages and hernia have been reported from USA as early as the 1920s7,9. Although epiploic appendagitis is a self-limiting condition, many times operation is unavoidable in order to rule out a possible incarcerated hernia. Imaging tools like ultrasonography may not be helpful in discriminating an inflamed epiploic appendage from the partly superposed colon. The mass could be misdiagnosed as a bowel loop and the pathological entity as an incarcerated bowel loop. In addition, an apparent inguinal mass must be excised, because many pathologic conditions (some of them malignant) can masquerade as inguinal hernia. So, the treatment consists of excision of the epiploic appendage with an attention to avoid opening of a concominant diverticulum. Tension-free repair of the hernia follows.
Entrapment of the adnexa in an indirect inguinal hernia is rare in adult women. Most reported cases concern the pediatric population, in which ovarian and tubal herniation have long been recognized as an entity10,11. Almost 30% of all reported cases are related to adolescents or women of reproductive age12. Embryogenic derangements are associated with this condition10,12. During embryogenesis, the gubernaculums and broad ligament suspend the ovary and prevent its descent through the canal of Nuck (processus vaginalis peritonei) to the base of the labium major. The canal of Nuck is obliterated on the 8th week of fetal life and the ovary is then suspended between the cornu of the uterus and the internal inguinal ring. If it remains patent, the ovary and the fallopian tube may be forced through the canal to a congenital hernia sac. When ovarian and fallopian tube inguinal hernias are found, they are commonly associated with anomalies in the development of the genital tract, such as vaginal atresia, bicornuate uterus and renal anomalies. The treatment in these cases is surgical13 with high ligation of the hernia sac, closure of the patent inguinal ring with the insertion of a plug and abdominal wall reinforcement with a patch using several interrupted sutures. Reduction of the hernia sac should only be attempted if no ovarian or tubal abnormality is present and the blood supply is not impaired.
Intrascrotal lipoma is not high in the differential diagnosis of an inguinoscrotal mass. Benign lipomatous tumors are not common in the scrotum. Although not found in a hernia sac, they can mimic irreducible groin hernias. Scrotal lipomas are classified into 3 types depending on their site of origin and spread: those arising from the fatty tissue within the spermatic cord and spreading to the scrotum, those originating and developing within the spermatic cord and those originating and developing within the scrotal walls (primary lipoma of the scrotum). The second type is the most common and account for about half of all cord tumors, while the third type, the primary lipoma of the scrotum, is rare14,15. In our case, the lipoma seemed to originate from the subcutaneous tissues posterior to the spermatic cord and spread into the scrotum. Despite to similar to our already reported cases, giant tumors, as the one described here, are not common15,16. In conclusion, a hernia surgeon may encounter unexpected intraoperative findings. It is important to be prepared to detect them and apply the appropriate treatment.
References
- 1.Rutkow IM, Robbins AW. Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am. 1993;73:413–426. doi: 10.1016/s0039-6109(16)46027-5. [DOI] [PubMed] [Google Scholar]
- 2.Akopian G, Alexander M. de Garengeot Hernia: Appendicitis within a femoral hernia. Am Surg. 2005;71:526–527. [PubMed] [Google Scholar]
- 3.Amyand C. Of an inguinal rupture, with a pin in the appendix caeci, incrusted with stone; and some observations on wounds in the guts. Philosophical Transactions of the Royal Society of London. 1736;39:329–336. [Google Scholar]
- 4.Hutchinson R. Amyands hernia. J R Soc Med. 1993;86:104–105. [PMC free article] [PubMed] [Google Scholar]
- 5.Solecki R, Matyja A, Milanowski W. Amyands hernia: a report of two cases. Hernia. 2003;7:50–51. doi: 10.1007/s10029-002-0093-x. [DOI] [PubMed] [Google Scholar]
- 6.Gurer A, Ozdogan M, Ozlem N, Yildirim A, Kulacoglu H, Aydin R. Uncommon content in groin hernia sac. Hernia. 2006;10:152–155. doi: 10.1007/s10029-005-0036-4. [DOI] [PubMed] [Google Scholar]
- 7.Kulacoglu H, Tumer H, Aktimur R, Kusdemir A. Epiploic appendicitis in inguinal hernia sac presenting an inguinal mass. Hernia. 2005;9:288–290. doi: 10.1007/s10029-004-0306-6. [DOI] [PubMed] [Google Scholar]
- 8.Abdulzhavadov IM. Volvulus of the epiploic appendices of the sigmoid in strangulated inguinal hernia (in Russian) Klin Med (Mosk) 1989;67:126–127. [PubMed] [Google Scholar]
- 9.Klingenstein P. Some phases of the pathology of the appendices epiploicae. Surg Gynecol Obstet. 1924;38:376–383. [Google Scholar]
- 10.Heineck AP. Hernias of the ovary, of the fallopian tube, and of the ovary and the fallopian tube: An analytical review of all undoubted cases of this nature reported in the French, German, and English medical literature from 1890 to 1910, inclusive, with a report of unpublished cases. Surg Gynecol Obstet. 1912;15:63–71. [Google Scholar]
- 11.Mayer V, Templeton FG. Inguinal ectopia of the ovary and fallopian tube. Review of the literature and report of the case of an infant. Arch Surg. 1941;43:397–408. [Google Scholar]
- 12.Bradshaw KD, Carr BR. Ovarian and tubal inguinal hernia. Obstet Gynecol. 1986;68:50–52. [PubMed] [Google Scholar]
- 13.Amarin ZO, Hart McK. Inguinal ovary and fallopian tube-an unusual hernia. Int J Gynecol Obstet. 1988;27:141–143. doi: 10.1016/0020-7292(88)90103-8. [DOI] [PubMed] [Google Scholar]
- 14.Florante J, Leyson J, Doroshow LW. Extratesticular lipoma: report of 2 cases and a new classification. J Urol. 1976;116:324–326. doi: 10.1016/s0022-5347(17)58801-1. [DOI] [PubMed] [Google Scholar]
- 15.Zeng L, Xia T, Kong X, Gu F. Massive lipoma of the scrotum. Chin Med J (Engl) 1999;112:84–85. [PubMed] [Google Scholar]
- 16.Greeley DJ, Jr, Sullivan JG, Wolfe GR. Massive primary lipoma of the scrotum. Am Surg. 1995;61:954–955. [PubMed] [Google Scholar]


