Abstract
Spontaneous haemorrhage is a well known complication of oral anticoagulation therapy. Various sites of bleeding have been reported in the literature, most commonly being the gastrointestinal tract, genitourinary system and central nervous system. Spontaneous haematoma is rarely reported to involve the upper aerodigestive tract, being potentially a life threatening condition. We report a case of a 67 year-old female patient who developed spontaneous heamatoma of the upper aerodigestive tract as a consequence of a rare interaction between acenocoumarol and clindamycin. Reversal of anticoagulation, careful observation, and when necessary prompt intervention to secure the airway are the main aspects of management. We highlight the need for a thorough evaluation of patients who develop new painful or other symptoms while being on anticoagulation therapy. Clinicians should be highly alerted as these could potentially be manifestations of haemorrhagic complications.
Keywords: Drug interaction, anticoagulants, haematoma, clindamycin, acenocoumarol, dysphagia, pharynx, larynx
The main risk of anticoagulation is haemorrhage, which may be spontaneous or may be precipitated by trauma. Over-anticoagulation enhances the risk of haemorrhage. Drug interactions are a major cause of over-anticoagulation. Gastrointestinal tract, genitourinary tract and central nervous system are the most common sites of bleeding. The upper airway may also be affected, occasionally with life threatening sequels1,2. In these subjects securing the airway should be the primary goal of management.
Case report
A 67 year-old female patient was referred on October 2007 to the Otolaryngology Department of AHEPA University Hospital from a District General Hospital with the diagnosis of spontaneous haematoma of the pharynx and aditus of the larynx. Her blood pressure was 130/70 mmHg and she was hemodynamically stable. The patient had been receiving oral anticoagulants (acenocoumarol) for atrial fibrillation. She had also been suffering from hypothyroidism and diabetes mellitus, receiving appropriate per os treatment for these medical conditions.
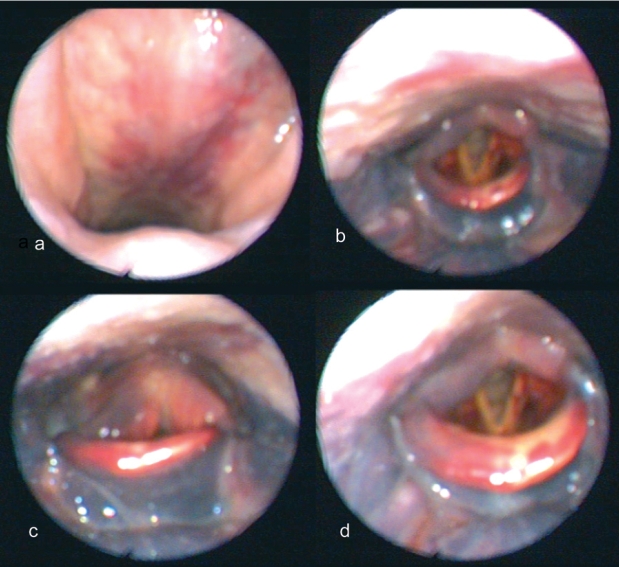
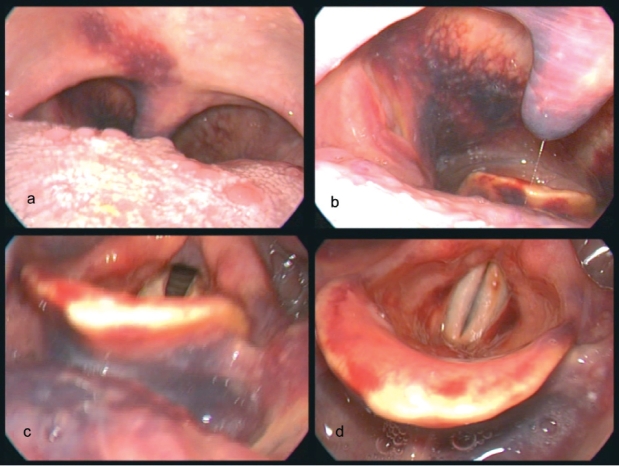
The patient had been well in herself until a week before the admission, when she developed a sore throat. She was diagnosed with lingual tonsillitis and was commenced on clindamycin, 600 mg three times daily, intramuscularly (i.m.). She reported that a few days later she experienced globus sensation in her throat and mild subjective feeling of dysphagia and dyspnoea. At that time a progressive haematoma was noticed to have developed at the site of i.m. injections in the buttocs. Twelve hours before her admission she also developed ecchymosis in her neck. She presented to the Emergency Department of the local District General Hospital where a thorough clinical evaluation was performed. The examination revealed a haematoma extending from the soft palate and nasopharynx to the base of the tongue, valeculla, epiglottis, lateral pharyngeal wall and aditus of the larynx (Figure 1, 2a and 2b). There was no fever. Urea and electolytes were normal except for slightly elevated blood glucose, 130 g/dl. A full blood count revealed anaemia (Hb: 9.4 g/dl) and leukocytosis (WBC: 18,000 mm3). Coagulation tests were grossly abnormal (PT: 117 sec, INR: 10.6, APTT: 115 sec). Vitamin K was administered intravenously (i.v.) with subsequent improvement of the coagulation profile (PT: 23.1 sec, INR: 1.96, APTT: 35.5sec). The patient was referred to the Otolaryngology Department of AHEPA University Hospital for further management. Despite her subjective symptoms, the airway did not necessitate any prompt intervention and she was admitted for observation and further management, should be required. On the fifth day after her admission, the ecchymosis of the neck showed further progress to the most dependent site, whereas the endoscopic examination revealed substantial improvement of the pharyngeal and laryngeal haematoma (Figure 2c, 2d, 3). During her ten-day hospitalization her coagulation profile returned to appropriate values for her atrial fibrillation, and her haematoma gradually subsided.
Figure 1: Pharyngeal and laryngeal haematoma on presentation. a) nasopharynx, b, c, d) superior view of the larynx, valeculla, base of tongue and pyriform sinus.
Figure 2: Echymosis of the neck. a, b) on presentation, c, d) fifth day of admission. Obvious progress to the most dependent site.
Figure 3: Fifth day of admission. Substantial improvement of haematoma. a) soft palate, b) oropharynx, c) valeculla and base of tongue, d) larynx.
Discussion
Coumarin anticoagulants interfere with the posttranslational gamma-carboxylation of vitamin K-dependent clotting factors II, VII, IX and X, by competitively inhibiting the effects of vitamin K. The main risk of oral anticoagulants is haemorrhage. Minor gingival bleeding, traumatic purpura, or trace haematuria may occur even within the therapeutic range of International Normalized Ratio (INR)3. Also, focal pathologic lesions, such as an occult tumour may be unmasked by the therapy. Nevertheless patients being on standard doses of warfarin have a frequency of 2 to 4% per year of clinically significant haemorrhage i.e. requiring transfusion4. Elderly patients or patients with history of stroke, gastrointestinal haemorrhage, first atrial fibrillation episode, concomitant use of aspirin or other co-morbidity i.e. diabetes, anaemia, uraemia or hepatic disease and with infrequent monitoring of the INR, carry higher risk4.
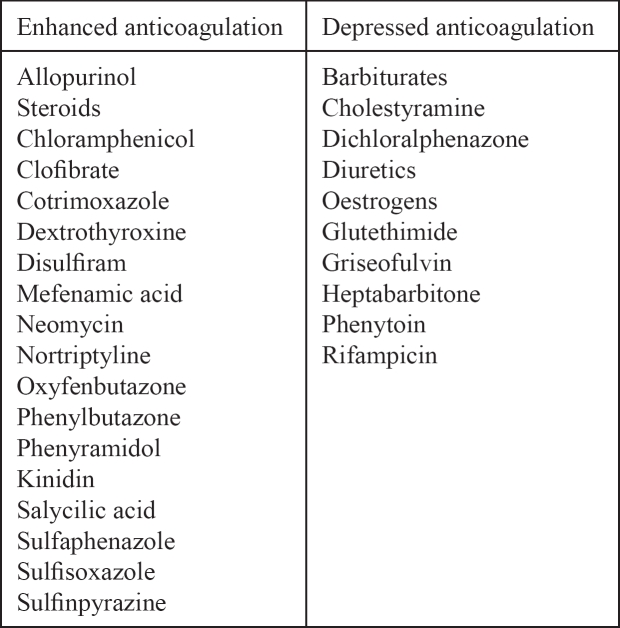
The risk of major bleeding is enhanced with over-anticoagulation. Various factors may alter the effect of coumarin anticoagulants, such as changes in diet, changes in the intake of drugs, hepatic failure and thyrotoxicosis. Over-anticoagulation due to drug interaction is a common cause of spontaneous haemorrhage. Gasse et al reported a 3 to 4.5 fold increase in the risk of serious bleeding in patients being on long term warfarin treatment with the concomitant use of potentially interacting drugs5. Drugs which influence the response to oral anticoagulants are listed in Table 16.
Table 1: Drug interactions of oral anticoagulants.
Interaction between clindamycin and coumarin anticoagulants has been reported in the literature only on few occasions. In 2001, Aldous and Olson described a case of a 47 year-old female patient on warfarin with an INR of 13, after having received clindamycin for 7 days following dental clearance, prior to which a preoperative prophylactic i.v. dose had been administered7. In 2005, Johnson et al, in a retrospective review of paediatric cardiology patients receiving chronic warfarin therapy, among others reported the admission of a 4 year-old child with an INR of 8.5 after having been on oral clindamycin for 6 days8. Decreased gut floral synthesis and decreased absorption of vitamin K have been suggested as the possible mechanisms of this interaction9. A single dose of clindamycin as administered for endocarditis prophylaxis, does not seem to influence the effect of warfarin.
Spontaneous haemorrhage may occur in numerous sites in the body, more commonly in the gastrointestinal tract, genitourinary tract, central nervous system, nose, retroperitoneum, subcutaneous tissues and wounds. Involvement of the upper aerodigestive tract causing obstruction is a rather rare but potentially life threatening complication10. Most reported cases of spontaneous haemorrhage obstructing the upper airway are related to retropharyngeal and laryngeal haematoma10. Sublingual haematoma may cause significant difficulties in securing the airway. Haemorrhage into the sublingual and submaxillary space may compromise the airway by elevating the tongue and floor of the mouth, producing a "pseudo- Ludwig's phenomenon"11. Sore throat is a common early symptom which should alert the highly suspicious clinician. Depending on the site and the significance of haemorrhage other symptoms may be hoarseness, cough, breathing difficulties, globus sensation, 'hot potato' voice and haemoptysis. In general, any painful or other new symptom in patients receiving anticoagulants should be clinically checked as it could be an early manifestation of haemorrhage3. Initially conservative management is suggested and, in most cases, close observation, monitoring, and reversal of anticoagulation result in successful outcome. In more severe cases emergency intervention may be required in order to secure the airway. Surgical drainage of the haematoma is generally not recommended.
Our patient developed spontaneous haematoma secondary to a rather rare interaction between acenocoumarol and clindamycin. Her minor subjective symptoms allowed for conservative management, in particular close observation and reversal of anticoagulation with the i.v. administration of vitamin K. A question could be raised as to whether her initial complaint of sore throat was due to the subsequent diagnosis of lingual tonsillitis or an early manifestation of spontaneous haematoma. However this does not seem to be the case as there were no other factors present to account for the enhanced effect of acenocoumarol prior to the intake of clindamycin. Furthermore, the initial diagnosis was made by a specialist, following thorough examination of the patient.
Conclusion
Spontaneous haematoma of the upper airway in patients receiving anticoagulants is a rather rare but potentially life threatening complication. Close observation, monitoring, reversal of anticoagulation and when necessary emergency intervention to secure the airway is the appropriate management. Interactions between anticoagulants and other drugs should always be taken into account when prescribing new medicines in order to prevent bleeding complications.
References
- 1.Gooder P, Henry R. Impending asphyxia induced by anticoagulant therapy. J Laryngol Otol. 1980;94:347–352. doi: 10.1017/s0022215100088885. [DOI] [PubMed] [Google Scholar]
- 2.Kerr HD, Kwaselow A. Vocal cord hematomas complicating anticoagulant therapy. Ann Emerg Med. 1984;113:552–553. doi: 10.1016/s0196-0644(84)80530-2. [DOI] [PubMed] [Google Scholar]
- 3.Mosher DF. Disorders of blood coagulation. Part XIII: Hematological Diseases. In: Bennett JC, Plum F, editors. Cecil Textbook of Medicine. 20th ed. Philadelphia: WB Saunders Co; 1996. pp. 999–1000. [Google Scholar]
- 4.Harker LA. Antithrombotic Therapy. Part V: Principles of Evaluation & Management. In: Bennett JC, Plum F, editors. Cecil Textbook of Medicine. 20th ed. Philadelphia: WB Saunders Co; 1996. pp. 120–121. [Google Scholar]
- 5.Gasse C, Hollowell J, Meier CR, Haefeli WE. Drug interactions and risk of acute bleeding leading to hospitalization or death in patients with chronic atrial fibrillation treated with warfarin. Thromb Haemost. 2005;94:537–543. doi: 10.1160/TH05-03-0166. [DOI] [PubMed] [Google Scholar]
- 6.Hull RD, Pineo GF, Raskob GE. Thrombosis and Anticoagulation Therapy. In: Stein JH, editor. Internal Medicine, Vol ΙΙ. Greek Edition. Athens: P.C. Paschalides; 1998. 214 pp. [Google Scholar]
- 7.Aldous JA, Olson CJ. Managing patients on warfarin therapy: a case report. Spec Care Dentist. 2001;21:109–112. doi: 10.1111/j.1754-4505.2001.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 8.Johnson MC, Wood M, Vaughn V, Cowan L, Sharkey AM. Interaction of antibiotics and warfarin in pediatric cardiology patients. Pediatr Cardiol. 2005;26:589–592. doi: 10.1007/s00246-005-0819-5. [DOI] [PubMed] [Google Scholar]
- 9.Rice PJ, Perry RJ, Afzal Z, Stockley IH. Antibacterial prescribing and warfarin: a review. Br Dent J. 2003;194:411–415. doi: 10.1038/sj.bdj.4810049. [DOI] [PubMed] [Google Scholar]
- 10.Gonzlez-Garca R, Schoendorff G, Muoz-Guerra MF, Rodrguez-Campo FJ, Naval-Gvas L, Sastre-Prez J. Upper airway obstruction by sublingual haematoma: a complication of anticoagulation therapy with acenocoumarol. Am J Otolaryngol. 2006;27:129–132. doi: 10.1016/j.amjoto.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Cohen AF, Warman SP. Upper airway obstruction secondary to warfarin-induced sublingual hematoma. Arch Otolaryngol Head Neck Surg. 1989;115:718–720. doi: 10.1001/archotol.1989.01860300072020. [DOI] [PubMed] [Google Scholar]