Abstract
Objective
To explore effects of various recruitment strategies on randomized clinical trial (RCT)-entry characteristics for patients with eating disorders within an everyday health-plan practice setting.
Methods
Randomly selected women, aged 25-50, in a Pacific Northwest HMO were invited to complete a self-report binge-eating screener for two treatment trials. We publicized the trials within the health plan to allow self-referral. Here, we report differences on eating-disorder status by mode and nature of recruitment (online, mail, self-referred) and assessment (comprehensive versus abbreviated) and on possible differences in enrollee characteristics between those recruited by strategy (self-referred versus study-outreach efforts).
Results
Few differences emerged among those recruited through outreach who responded by different modalities (internet versus mail), early-versus-late responders, and those enrolling under more comprehensive or abbreviated assessment. Self-referred were more likely to meet binge-eating thresholds and reported higher average BMI than those recruited by outreach and responding by mail; however, in most respects the groups were more similar than anticipated. Fewer than 1% of those initially contacted through outreach enrolled.
Conclusions
Aggressive outreach and screening is likely not feasible for broader dissemination in everyday practice settings and recruits individuals with more similar demographic and clinical characteristics to those recruited through more abbreviated and realistic screening procedures than anticipated.
Keywords: recruitment, eating disorders, binge eating, clinical trials
Across domains of mental health and health behavior interventions, there has been increasing concern and recognition of a gap between the context in which research is carried out and the everyday practice settings in which we hope such findings are applied (1-9). Many researchers and policy makers have noted that the ultimate dissemination and usability of evidence-based interventions are as important as is the tight scientific control (internal validity) under which many of the early clinical trials are conducted. As one distinguished health researcher noted, “If we want more evidence-based practice, then we need more practice-based evidence” (10) Similar to interventions developed to address many mental health and behavioral health conditions, treatment research in eating disorders has relied almost entirely on self-selected volunteers or provider referrals to tertiary care specialty settings to recruit participants (11;12). Given the recognition that there are many more individuals with eating disorders than those presenting for treatment (13;14), that many who present for treatment might not volunteer for participation in clinical trials, and the availability of effective treatments for these disorders(15;16), one could argue that a more aggressive outreach and screening is needed. Although there have been a limited number of studies examining possible sampling biases among those participating in eating disorders research(17;18), we could find no studies focused on examining the effect of using recruitment procedures consistent with what might be found in everyday practice settings. Rather, these studies either have examined non-clinical samples’ response to surveys under the frame of an eating disorder-focused study or more general survey(17) or a compared the characteristics of clinical trial participants of different ethnicities(18).
It is our intent to address five fundamental questions about practice-based trials with this paper. First, how realistic is it to instigate an intensive outreach and screening effort to identify patients who may potentially benefit from eating disorder treatment? Second, how closely do those self-referred for treatment and those identified through more intensive outreach resemble one another? Third, among those recruited through study outreach efforts, do different modalities of response (mail versus online) represent different types of respondents? Fourth, among those recruited through study outreach efforts, how important is persistence of outreach to ensure inclusion of a broader, more diverse population? Finally, we examine whether the use of more abbreviated but realistic screening procedures for real world settings results in the enrollment of a less impaired patient population.
METHODS
Study Design
The principal aim of the overall project was to determine the acceptability as well as clinical and cost effectiveness of a cognitive behavioral therapy-based guided self-help program (CBT-GSH) when delivered to a community population of adults with binge eating disorders following large-scale outreach (screening) efforts. We sought to evaluate an intervention that could reach large numbers of adults with eating disorders at a reasonable cost within an everyday health plan practice setting in which such screening and low-intensity treatment provision was most likely to be utilized. We describe here the recruitment efforts for two related randomized clinical trials.
Setting
The study was conducted at the Center for Health Research (CHR), a multidisciplinary research organization located within a large Health Maintenance Organization (HMO) in the Northwest (Kaiser Permanente — KPNW). The research center is scientifically autonomous and has conducted academic, public domain health research for 45 years. KPNW is the third largest (N=450,000) of 12 semiautonomous Kaiser Permanente divisions, the world’s largest nongovernmental health care provider. It is a federally qualified prepaid group practice HMO. The HMO facilities and services currently include inpatient and outpatient clinics, the full range of medical specialists and other health professionals, and educational, screening, diagnostic, treatment, and rehabilitation services. All member contacts within the system and all services referred outside the system are recorded in a single, comprehensive electronic medical record. As a division of the HMO, CHR has access to the KPNW administrative databases for research purposes. All members are informed of this research access when they enroll. If they wish, members may preemptively decline all research contacts. The HMO Institutional Review Board approved all study procedures.
Participants
Recruitment for the randomized clinical trial (RCT) portion of this study proceeded in two waves preceded by a pilot of the recruitment procedures and intervention. Both waves of recruitment focused on women between 25 and 50 years of age - our highest yielding subpopulation during our pilot (although eligible self-referred men and younger women [18-24 years of age] were accepted into the study). In the first wave (July 2005 through June 2006), all those who responded and were eligible per the initial screener were invited to complete a much more comprehensive assessment to determine eligibility for the RCT. Thus, we identify this as the “comprehensive assessment” phase of the study.
In contrast to the first wave of recruitment (“assessment”), those individuals screening eligible in the second wave (August 2006 through June 2007) completed a more abbreviated self-report assessment battery followed by a secondary telephone interview to determine eligibility for the RCT. This process likely more closely reflects the type of screening and treatment referral process feasible for execution in an everyday practice setting. We label this the “abbreviated assessment” phase through the remainder of the article.
Table 1 shows a comparison of eligibility criteria, screening procedures, and assessment instruments for those recruited during these two distinct waves (trials) of the research study. All those between 18 and 50 years of age, with a body mass index less than 45, and reporting at least one objective binge episode per week on average over the past three months were eligible to participate. In both trials, individuals in the targeted age range were randomly selected from the HMO Electronic Medical Records data base (EMR) and sent an invitational postcard to complete a brief survey questionnaire about body image and eating behaviors. The postcard was followed by a mailing of the initial screening survey questionnaire. Recruitment materials emphasized that the program was designed to help participants gain control over their eating and more generally to better understand individuals’ eating habits and body image concerns. Respondents had the option of completing a paper and pencil version of the screener and returning it by mail via a prepaid return envelope or completing an online version. In order to motivate quick response, those individuals completing the screener online were mailed a $5 coffee shop coupon for their efforts (no compensation was provided for response by mail). During the comprehensive assessment trial, non-responders were mailed another questionnaire after 15 days (this practice was discontinued during the abbreviated assessment trial). We based this interval between mailings on pilot findings, which demonstrated that responses fell off sharply after 15 days suggesting that those who were likely to respond had done so within this time frame. Excluded from the mailings for both of these trials were individuals whose medical records indicated severe cognitive or psychiatric impairment (e.g., mental retardation, psychosis), or those currently receiving treatment for a severe physical illness such as cancer. Also excluded were approximately 100 plan members whose records indicated that they had pre-emptively opted out of involvement in research. In addition, those who reported body mass indexes exceeding 45 upon initial screening were not included in further assessments as the low intensity nature of the treatment was not considered sufficient for severely obese individuals. Finally, we displayed posters and brochures at the health plan primary care clinics to encourage those interested to self-refer to the project.
Table 1.
Comparison of Participant Characteristics in Two Related Trials Evaluating A Binge Eating Disorder Interventiona
| Comprehensive Assessment Phase (trial #1) |
Abbreviated Assessment Phase (trial #2) |
|
|---|---|---|
|
Target Population for Recruitment Mailingb |
Women, 25 – 50 years of age | Women, 25-50 years of age |
| Initial Screening | Modified version of PHQ eating disorders module |
Modified version of PHQ eating disorders module |
|
Persistence of Screening Effort |
Nonrespondents to mailed survey sent a second copy after 15 days |
No second survey mailed |
| Incentives Provided | $5 for online completion of screening questionnaire; $50 for baseline assessment (1-2 hrs phone interview) |
No incentive for online completion of screening questionnaire; $25 for baseline assessment (10-15 minute pencil and paper measure) |
|
Determination of RCT Eligibility |
Eating Disorders Examination (EDE) and Structured Clinical Interview for DSM Disorders (SCID) |
Eating Disorders Examination — Questionnaire (EDE-Q) and secondary telephone screening |
Although instruments assessing RCT eligibility differed across the two study phases/trials, criteria were consistent across both. Samples included in this paper were limited to women between 25 and 50 years of age who reported one or more objective bulimic episode per week over the past three months.
self-referred men and younger (18-24 year old) women were were eligible for participation but their data is not included in this report
Measures
Initial screening survey questionnaire
The initial screening survey questionnaire, used in both trials, was designed to collect demographic information and measure eating disorder symptomatology, functional impairment, and health and well-being. To assess eating disorder symptoms, a modified version of the Patient Health Questionnaire (PHQ; Spitzer et al. 1999(19)) eating disorder module was used. This module included binary (yes/no) response items concerning binge eating and compensatory behaviors. To assess binge eating, participants were asked to indicate if they often feel that they can’t control what or how much they eat and if they often eat, within any 2-hour period, what most people would regard as an unusually large amount of food. If participants responded ‘yes” to both of these items, they were then asked to indicate if the behaviors in question occurred as often as twice a week in the last 3 months. These frequency and duration criteria align with those currently required by the DSM in order to establish a research diagnosis of Binge Eating Disorder (BED).
In order to identify participants who met our specific inclusion criterion (recurrent binge eating at least once per week), we added an item asking participants whether binge eating occurred as often as once a week in the past 3 months. To assess potential functional impairment due to binge eating, participants who responded “yes” to the binge eating items were also asked to rate on a 4-point scale the extent to which the eating behavior(s) made it difficult (ranging from “not at all difficult” to “extremely difficult”) for them to do their work, take care of things at home, or get along with other people. Participants who indicated that their eating behaviors made it at least “somewhat difficult” for them in their daily living tasks were coded as having eating disorder related impairment. In addition, participants were asked their current height and weight to determine body mass index and a number of demographic questions (age, gender, race/ethnicity, level of education, marital status, and household income).
Eating Disorders Examination Interview (EDE; Fairburn & Cooper, 1993(21))
This standardized, semi-structured, investigator-based interview measures the severity of the core clinical features of eating disorders, generates operationalized diagnoses of eating disorders, and is considered the “gold standard” method for assessing disordered eating-related psychopathology. The diagnostic portion of the interview was utilized in the comprehensive assessment phase (trial #1)study to determine whether participants met diagnostic criteria for a binge eating disorder (BN, BED, or RBE) and, hence, were eligible for participation.
Structured Clinical Interview for DSM-IV (SCID; First et al, 1995(22); 1997(23))
During the comprehensive assessment phase (trial #1), the SCID was administered to determine presence or absence of nonED axis I psychiatric disorders as well as Borderline Personality Disorder (assessed using SCID-II). Those individuals whose responses indicated a current or past psychotic disorder or current alcohol/drug abuse were excluded from further participation in the first trial. Although the SCID was not used to screen for these exclusionary criteria during the second trial, review of potential participants’ electronic medical records allowed us to exclude individuals with these indications from our recruitment pool.
Eating Disorders Examination Questionnaire (EDE-Q; Fairburn & Beglin, 1994(24))
The EDE-Q is a 36-item self-report version of the EDE and was administered to all participants in both trials who, on the PHQ, reported binge eating once a week or more over the past three months as a continuous measure of eating disorder symptomatology; for those in the abbreviated assessment trial (where we did not use the EDE), the EDE-Q was used as a further assessment of trial eligibility. EDE-Q items yield an overall score of eating disturbance as well as four subscale scores including Restraint, Eating Concern, Weight Concern and Shape Concern. Those who responded to each subscale with an average value of “4” or greater were categorized as evidencing clinically significant symptom levels on the subscale in question (Fairburn & Beglin, 1993).
Secondary Telephone Screening to Assess for Binge Eating
For participants in the abbreviated assessment phase (trial #2), who met eligibility criteria on the PHQ and the EDE-Q, a follow-up telephone screening was completed to ensure that the magnitude of the referenced binge episodes was sufficient to meet criteria for “objective bulimic episodes,” (i.e., the amount of food consumed during the binge was “definitely larger than most people would eat during a similar period of time and under similar circumstances” during which the person is experiencing a sense of loss of control(25), and that the frequency of such objective bulimic episodes was at least once/week during the past three months.. Telephone interview questions were adapted from the relevant section of the EDE.
Data analyses
Descriptive statistics were derived for comparisons of characteristics of the different types of respondents. Chi-square analyses were used to test for differences across groups for categorical variables and t-tests and analysis of variance for continuous variables. The effect size reported was Number Needed to Take (NNT) for categorical variables. NNT is the answer to the question: “How many cases do you have to see to find one more ‘bad outcome’ than if you had observed their matched controls?” However, in the present study, “bad outcome” refers to reporting presence of a given behavior (e.g., eating disorder scores) or baseline characteristic. NNT was used because it takes into account base rates of each of the conditions of interest (26;27). Following Kraemer and Kupfer (26), a NNT less than 4 was considered a “strong” effect; a NNT between 4 and 9 was considered a “moderate” effect; and an NNT over 9 was considered a “weak” effect.
RESULTS
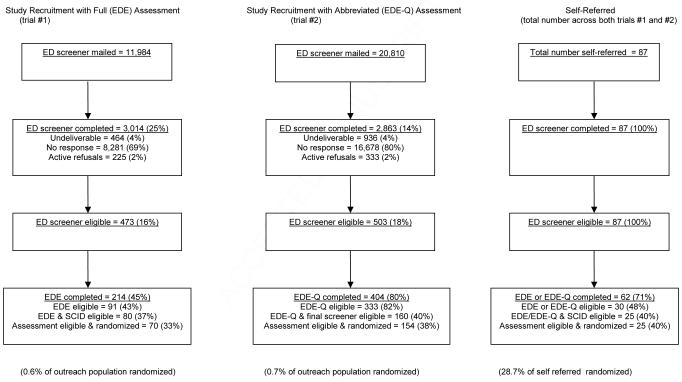
Figure 1 summarizes the recruitment process for those participating in the “comprehensive” (full EDE assessment) and “abbreviated” (abbreviated EDE-Q assessment) phases of the project, respectively, as well as compares these individuals contacted through study outreach efforts to those who self-referred to the study. In both phases a minority of those contacted completed this initial screening (25% in comprehensive assessment phase, 14% in abbreviated assessment phase) yet there were few active refusals (<2% in both phases). The proportion of respondents who met initial eligibility based on their responses to binge eating questions was comparable in the two phases (16% in the comprehensive- and 18% in the abbreviated assessment phase) but substantially lower than those who self-referred to the study, 100% of whom met initial eligibility criteria. Although a larger proportion of those in the abbreviated assessment phase participated in the baseline assessment (80% for EDE-Q versus 45% when full EDE interview administered), the overall proportion from the two phases that were assessment eligible and randomized was similar (33% in comprehensive- phase versus 38% in abbreviated assessment phase). Interestingly, despite all of those who self-referred to the study meeting the initial eligibility criteria, a comparable more modest proportion of them (40%) were assessment eligible and randomized into one of the two studies. Only a small proportion of those initially contacted through study outreach about the potential opportunity to participate in the program to help gain control over eating (0.6% for comprehensive- and 0.7% for abbreviated assessment phase) were randomized into the trial in comparison to 28.7% of those who self-referred to the study.
Figure 1.
Recruitment Process for All Modes of Recruitment
Table 2 compares the characteristics of those participants initially identified for study outreach contact who responded to the screening by mail, online, and those who self-referred to the study across both trials. Those who self-referred were more likely to meet both thresholds for binge eating than were EMR-identified individuals (as shown from the NNT); specifically, for every two participants who were self-referrals, one more was expected to meet the study’s binge eating criteria than for every two individuals who responded either by mail or online). Among those reporting binge eating, those who self-referred reported modestly more ED-related impairment (77.65%) than those recruited through study outreach who responded either by mail (63.29%) or online (58.31%). There were also significant differences in the prevalence of obesity (BMI ≥ 30) in the different groups with a substantially larger proportion of those self-referred meeting obesity criteria (61%) than those study outreach participants responding by mail (34%). An intermediate prevalence of obesity (47%) was reported among those study outreach participants responding online. Self referred participants tended to report higher incomes than those reported by study outreach participants responding either by phone or online. There appeared to be no racial or ethnic differences between online, mail and self-referred respondents. Finally, although there were significant differences in the proportions of those with advanced education among the three groups, effect size estimates suggested that the differences were not meaningful.
Table 2.
Characteristics of those responding by mail, online, or self-referred (trials #1 and #2 combined)
| Responded by Mail1 (N = 3,443) |
Responded Online (N = 2,434) |
Self-Referred (N = 87) |
p-value | Effect Size Estimate: M vs. O |
Effect Size Estimate: M vs. SR |
Effect Size Estimate: O vs. SR |
|
|---|---|---|---|---|---|---|---|
| Eating Disorder Scores | |||||||
| Binge 1× per week over last 3 months |
16.12% | 26.34% | 93.51% | < .0001 | 10 | 2 | 2 |
| Binge 2× per week over last 3 months |
13.53% | 22.68% | 84.42% | < .0001 | 11 | 2 | 2 |
| ED-related Impairment2 | 63.29% | 58.31% | 77.65% | < .0001 | 21 | 7 | 6 |
|
Prevalence of Obesity (BMI ≥ 30) |
34.07% | 47.41% | 60.92% | < .0001 | 8 | 4 | 8 |
| Demographics | |||||||
| Age | 39.52a (7.21) | 38.46b (7.25) | 36.69b (7.34) | < .0001 | N/A | N/A | N/A |
| Race/Ethnicity | |||||||
| White/Non-Hispanic | 96.88% | 96.77% | 93.22% | ||||
| Other | 3.12% | 3.23% | 6.78% | .2881 | 910 | 28 | 29 |
| Highest Grade Completed | 19.67% | 14.33% | 9.20% | ||||
| Up to high school grad | 80.33% | 85.67% | 90.80% | < .0001 | 19 | 10 | 20 |
| Some college & higher | |||||||
| Marital Status | |||||||
| Married | 66.55% | 68.83% | 65.52% | ||||
| Widowed | 0.73% | 0.46% | 1.15% | ||||
| Divorced | 11.09% | 8.59% | 16.09% | ||||
| Separated | 1.61% | 1.49% | 2.30% | .0640 | N/A | N/A | N/A |
| Never Married | 11.94% | 12.70% | 8.05% | ||||
| Unmarried Couple | 8.09% | 7.93% | 6.90% | ||||
| Income | |||||||
| $49,999 or less | |||||||
| $50,000 or more | 39.71%60.29% | 36.61%63.39% | 55.42%44.58% | .0004 | 32 | 7 | 6 |
Includes 6 early respondents who were screened by telephone
Total N for responded by mail = 899; total N for responded online = 909; Total N for self-referred = 85
Note: a, b and c superscripts denote groups that are statistically different using multiple comparison procedures; M=mail/phone response, O=online response, and SR = self-referred
Because second mailings of the eating disorders screening questionnaire to initial nonrespondents were only sent during the comprehensive assessment phase, Table 3 is limited to those study outreach participants in trial #1. Modest differences were observed in the proportion of respondents meeting the stricter binge eating criteria (two times per week on average) with those responding more quickly reporting higher levels of binge eating. However, despite other differences in the groups that were statistically significant, effect size estimates suggested that the differences were not meaningful.
Table 3.
Characteristics of early and late responders to ED screener during comprehensive assessment case identification phase
| Response time 15 days or less (N=1,890) |
Response time more than 15 days (N=1,124) |
p-value | Effect Size Estimate (number needed to treat) |
|
|---|---|---|---|---|
| Eating Disorder Scores | ||||
| Binge 1× per week over last 3 months |
18.84% | 14.68% | .0035 | 25 |
| Binge 2× per week over last 3 months |
16.40% | 12.01% | .0010 | 8 |
| ED Impairment1 | 61.17% | 54.81% | .0822 | 16 |
|
Prevalence of Obesity (BMI ≥ 30) |
35.98% | 32.30% | .0398 | 28 |
| Demographics | ||||
| Age | 38.79 (7.57) | 39.01 (7.50) | .4359 | N/A |
| Race/Ethnicity | ||||
| White/Non-Hispanic | 98.60% | 97.06% | 0.127 | 65 |
| Other | 1.40% | 2.94% | ||
| Highest Grade Completed | ||||
| high school or less | 17.13% | 19.88% | 0.591 | 37 |
| Some college & higher | 82.87% | 80.12% | ||
| Marital Status | ||||
| Married | 68.18% | 66.31% | ||
| Widowed | 0.70% | 0.54% | ||
| Divorced | 9.57% | 10.15% | .2462 | N/A |
| Separated | 1.50% | 2.25% | ||
| Never Married | 12.14% | 14.11% | ||
| Unmarried Couple | 7.91% | 6.65% | ||
| Income | 40.36% | 40.46% | ||
| $49,999 or less | 59.64% | 59.54% | .9574 | 1000 |
| $50, or more | ||||
Total N for responded in 15 days or less = 546; total N for responded after 15 days or more = 274
Finally, Table 4 shows the comparison of characteristics among those who met full study eligibility criteria and were randomized into either of the two trials. Those who self referred were younger on average and were more likely to report shape and weight concerns. However, there was no indication that the groups systematically varied by reported frequency of binge eating (one versus two times per week on average), perceived impairment related to disordered eating practices, rates of obesity, the likelihood of reporting dietary restraint nor other demographic characteristics.
Table 4.
Comparison of baseline characteristics of those randomized using study outreach (comprehensive and abbreviated ED assessments) to those self-referred for treatment
| Study outreach / comprehensive assessment (N =70 ) |
Study outreach / abbreviated assessment (N =152) |
Self-Referred / mixed assessment (N =25) |
p-value | Effect Size Estimate: F vs. A |
Effect Size Estimate: F vs. SR |
Effect Size Estimate: A vs. SR |
|
|---|---|---|---|---|---|---|---|
| Eating Disorder Scores | |||||||
| Binge 1× per week over last 3 months |
91.43% | 92.86% | 96.00% | .7488 | 70 | 22 | 32 |
| Binge 2× per week over last 3 months |
82.86% | 81.82% | 80.00% | .9489 | 97 | 35 | 55 |
| ED Impairment | 79.71% | 74.17% | 75.00% | .6697 | 19 | 22 | 121 |
| EDE Restraint | 21.74% | 26.80% | 29.17% | .6652 | 20 | 14 | 43 |
| EDE Shape/Weight Concern |
82.61% | 89.54% | 100.0% | .0584 | 15 | 6 | 10 |
|
Prevalence of Obesity (BMI ≥ 30) |
60.00% | 57.14% | 60.00% | .9061 | 35 | N/A | 35 |
| Demographics | |||||||
| Age | 40.96a (5.99) | 39.41a (6.40) | 34.24b (7.16) | < .0001 | N/A | N/A | N/A |
| Race/Ethnicity | 98.21% | 96.03% | 94.12% | ||||
| White/Non-Hispanic | 1.79% | 3.97% | 5.88% | .6536 | 46 | 25 | 53 |
| Other | |||||||
| Highest Grade Completed | |||||||
| Up to high school grad | 24.29% | 15.58% | 12.00% | ||||
| Some college & higher | 75.71% | 84.42% | 88.00% | .2103 | 12 | 9 | 28 |
| Marital Status | |||||||
| Married | 68.57% | 68.63% | 80.00% | ||||
| Divorced | 21.43% | 10.46% | 4.00% | ||||
| Separated | 0.00% | 1.31% | 4.00% | .1132 | N/A | N/A | N/A |
| 2003;Never Married | 5.71% | 12.42% | 4.00% | ||||
| Unmarried Couple | 4.29% | 7.19% | 8.00% | ||||
| Income | |||||||
| $49,999 or less | 40.58% | 37.33% | 54.17% | ||||
| More than $49,999 | 59.42% | 62.67% | 45.83% | .2920 | 31 | 8 | 6 |
Note: a, b and c superscripts denote groups that are statistically different using multiple comparison procedures; M=mail/phone response, O=online response, and SR = self-referred
DISCUSSION
In summary, among those recruited using intensive outreach methods (study invitation), we found few differences among those responding by different modalities (Internet versus mail), early and late responders, and those enrolling in the clinical trials when more comprehensive or abbreviated assessment was utilized. Some modest differences emerged between respondents who had been invited into the studies by outreach efforts and those who were self-referred. Those who self referred were more likely to meet binge eating thresholds and reported a higher average BMI than those recruited through study outreach who responded by mail. However, in many respects the groups were more similar than anticipated and there were no discernible differences in perceived functional impairments related to disordered eating patterns. Hence, the intensive efforts employed in this study did not yield a more demographically diverse group of patients than would have been assembled by self-referral in response to brochures or posters displayed at the health plan clinics. Similarly, based on differences observed between early and later responders our findings suggest that persistence of outreach efforts (while increasing the overall number of participants) results in few differences in recruited participants. This is consistent with an earlier report by Mond and colleagues (28) which found no difference in eating disorder psychopathology between those responding relatively quickly and those responding only after several reminders were made. Importantly, using an abbreviated eating disorders assessment did not appear to result in a less impaired sample than that recruited through a more comprehensive assessment. This suggests that, compared to a more labor-intensive and burdensome assessment approach, an assessment method that is more likely to be acceptable to everyday health care settings (reduced demand on staff time and lower burden on patients) still identifies patients with comparable levels of eating disorder-related pathology.
One cautionary note from the reported findings is the very large outreach sample that was necessary for this two-step screening process to identify interested individuals for participation in these randomized clinical trials — percentages (less than 1%) that were virtually identical regardless of recruitment response modality (mail or online) or the burden of the initial assessment process. While the point prevalence of diagnostic threshold binge eating disorders is modest (approximately 1%; (29-31)), there may be individuals who could be identified in everyday practice settings who would be interested and benefit from low intensity (guided self-help) clinical treatment such as the one offered in these trials but who are unwilling to participate in a clinical trial. Our finding suggests that such an intensive outreach and screening as that employed for the current study would not be feasible for broader dissemination in everyday practice settings. In a recent study examining the beliefs of the public concerning the helpfulness of interventions for bulimia nervosa (32), respondents indicated that they believed that seeing a general practitioner would be more helpful than seeing a mental health specialist. This suggests that screening and follow-up initiated explicitly within the primary care setting may be most likely to be successful in identifying those who would benefit and be willing to receive treatment for a binge eating disorder. We are not able to address the question of whether there was sampling bias due to the self-help nature of the intervention used in our trials, because this type of intervention may have failed to appeal to potential participants interested in more extensive treatment. Yet, we advertised for a brief binge eating treatment that was as low-intensity as many of the psychoeducational treatments/programs available through the health plan; we therefore expect that systematic differences were unlikely between our recruited samples and those who would enroll for such services in everyday practice settings. We believe that the large and representative sample of potential participants makes this a particularly important study in which to evaluate recruitment strategies and implications for eating disorders treatment in everyday practice settings. Although the shifting of recruitment methods makes some elements difficult to compare directly, the overall findings of lack of difference in respondent/participant characteristics across different modes and persistence of recruitment and screening is important. Although based on our findings, it doesn’t appear to be realistic to launch broad screening outreach for binge eating disorders per se within everyday practice settings, this may be feasible if done as one part of a larger mental health/behavioral health screener administered by a health plan with appropriate services for a variety of conditions (e.g., depression/anxiety, substance use, eating disorders). Evaluating such a process would be an important next research step.
Acknowledgments
We thank Lynette Rogers, Kristina Booker, Emily Ach, Y. May Chao, and Alexis May. Without their assistance, this study could not have been conducted. This study was supported by NIH Research Grant No. MH066966 (Principal Investigator: Ruth Striegel-Moore, Wesleyan University) funded by the National Institute of Mental Health (NIMH) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), awarded to Kaiser Foundation Research Institute. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH, NIMH, NIDDK, or Kaiser Foundation Research Institute. Guided Self-Help Treatment for Binge Eating Disorders registered with ClinicalTrials.gov (Identifier: NCT000158340). The first author, Dr. DeBar had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was supported by NIH Research Grant No. MH066966 (Principal Investigator: Ruth Striegel-Moore, Wesleyan University) funded by the National Institute of Mental Health (NIMH) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), awarded to Kaiser Foundation Research Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- (1).Glasgow RE. RE-AIMing research for application: ways to improve evidence for family medicine. J Am Board Fam Med. 2006;19(1):11–19. doi: 10.3122/jabfm.19.1.11. [DOI] [PubMed] [Google Scholar]
- (2).Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- (3).Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Schoenwald SK, Hoagwood K. Effectiveness, transportability, and dissemination of interventions: what matters when? Psychiatr Serv. 2001;52(9):1190–1197. doi: 10.1176/appi.ps.52.9.1190. [DOI] [PubMed] [Google Scholar]
- (5).McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- (6).Zerhouni E. Medicine. The NIH Roadmap. Science. 2003;302(5642):63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- (7).Farquhar CM, Stryer D, Slutsky J. Translating research into practice: the future ahead. Int J Qual Health Care. 2002;14(3):233–249. doi: 10.1093/oxfordjournals.intqhc.a002615. [DOI] [PubMed] [Google Scholar]
- (8).Institute of Medicine, Committee on quality of health care in America . Crossing the quality chasm: a new health system for the 21st Century. Institute of Medicine Committee on quality of health Care in America. National Academy of Press; Washington (DC): 2001. Ref Type: Report
- (9).Humphreys K, Weingardt KR, Horst D, Joshi AA, Finney JW. Prevalence and predictors of research participant eligibility criteria in alcohol treatment outcome studies, 1970-98. Addiction. 2005;100(9):1249–1257. doi: 10.1111/j.1360-0443.2005.01175.x. [DOI] [PubMed] [Google Scholar]
- (10).From efficacy to effectiveness to community and back: evidence-based practice vs. practice-based evidence. National Institutes of Diabetes, Digestive, and Kidney Diseases. 2004.
- (11).Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):337–348. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- (12).Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):321–336. doi: 10.1002/eat.20372. [DOI] [PubMed] [Google Scholar]
- (13).Fairburn CG, Cooper Z, Bohn K, O’Connor ME, Doll HA, Palmer RL. The severity and status of eating disorder NOS: implications for DSM-V. Behav Res Ther. 2007;45(8):1705–1715. doi: 10.1016/j.brat.2007.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Mond JM, Hay PJ, Rodgers B, Owen C. Health service utilization for eating disorders: findings from a community-based study. Int J Eat Disord. 2007;40(5):399–408. doi: 10.1002/eat.20382. [DOI] [PubMed] [Google Scholar]
- (15).Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. 2007;40(4):293–309. doi: 10.1002/eat.20369. [DOI] [PubMed] [Google Scholar]
- (16).Wilson GT, Grilo CM, Vitousek KM. Psychological treatment of eating disorders. Am Psychol. 2007;62(3):199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- (17).Moss EL, von Ranson KM. An experimental investigation of recruitment bias in eating pathology research. Int J Eat Disord. 2006;39(3):256–259. doi: 10.1002/eat.20230. [DOI] [PubMed] [Google Scholar]
- (18).Grilo CM, Lozano C, Masheb RM. Ethnicity and sampling bias in binge eating disorder: Black women who seek treatment have different characteristics than those who do not. Int J Eat Disord. 2005;38(3):257–262. doi: 10.1002/eat.20183. [DOI] [PubMed] [Google Scholar]
- (19).Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- (20).Wilfley DE, Bishop ME, Wilson GT, Agras WS. Classification of eating disorders: toward DSM-V. Int J Eat Disord. 2007;40(Suppl):S123–S129. doi: 10.1002/eat.20436. [DOI] [PubMed] [Google Scholar]
- (21).Fairburn CG, Cooper Z. The eating disorders examination. In: Fairburn CG, Cooper Z, editors. Binge Eating and Bulimia Nervosa: Distribution and Determinants. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- (22).First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- (23).First MB, Spitzer RL, Gibbon MA, Williams JBW. Structured clinical interview for DSM-IV personality disorders (SCID-II) New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- (24).Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–370. [PubMed] [Google Scholar]
- (25).American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV. 4 ed. American Psychiatric Association; Washington D.C.: 1994. [Google Scholar]
- (26).Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry. 2006;59(11):990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- (27).Grissom RJ, Kim JJ. Review of assumptions and problems in the appropriate conceptualization of effect size. Psychol Methods. 2001;6(2):135–146. doi: 10.1037/1082-989x.6.2.135. [DOI] [PubMed] [Google Scholar]
- (28).Mond JM, Rodgers B, Hay PJ, Owen C, Beumont PJ. Nonresponse bias in a general population survey of eating-disordered behavior. Int J Eat Disord. 2004;36(1):89–98. doi: 10.1002/eat.20007. [DOI] [PubMed] [Google Scholar]
- (29).Hudson JI, Hiripi E, Pope HG, Jr., Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Hay P. The epidemiology of eating disorder behaviors: an Australian community-based survey. Int J Eat Disord. 1998;23(4):371–382. doi: 10.1002/(sici)1098-108x(199805)23:4<371::aid-eat4>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- (31).Hoek HW, van HD. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34(4):383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- (32).Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Beliefs of the public concerning the helpfulness of interventions for bulimia nervosa. Int J Eat Disord. 2004;36(1):62–68. doi: 10.1002/eat.20004. [DOI] [PubMed] [Google Scholar]