In the face of concerns raised by citizens about long waits for health care services,1,2 federal and provincial governments in Canada have made the reduction of wait times for key health services – including magnetic resonance imaging (MRI) scanning – a priority.3 Under Ontario’s Wait Times Strategy, launched on 17 November 2004, the provincial government has invested approximately $118 million in capital and operational funding for MRI services through to the end of March 2008 (Steven Johansen, Ontario Ministry of Health and Long-Term Care; personal communication, 2008). Twelve MRI scanners in new locations have been purchased, and seven aging MRI machines at existing sites have been replaced. In addition, the efficiency of existing scanner use has been improved through the funding of additional MRI hours, such that the current availability of MRI has been extended from a baseline of 8 hours on weekdays to 16 or even 24 hours per day, up to 7 days a week.4,5
Previous work has shown that, despite Canada’s system of universal health insurance, some health services (including MRI scanning) have higher rates of use among higher income groups than among Canadians with low incomes, and that these differences are unlikely to be explained by differences in medical need alone.6-9 In this paper we explore whether the recent increase in access to MRI scanning in Ontario has led to a widening of this income-correlated disparity.
In a population-based analysis, we identified all Ontario Health Insurance Plan claims for MRI scans performed between 1 April 2002 and 31 March 2007.10 Inpatient MRI exams were excluded, since they are covered through hospitals’ global budgets. Only one body-part-specific scan per patient per day was counted. Neighbourhood income at the level of the census dissemination area (the smallest geographic areas for which census data are made available by Statistics Canada), was used as a proxy measure of the personal income of patients receiving MRI scans. Neighbourhood income was determined by linking patients’ residential postal code to the Statistics Canada Postal Code Conversion File, which contains neighbourhood income data.11 MRI scanning rates (for Ontario, and within each neighbourhood income quintile) were expressed as the number of MRI scans per 100,000 population and were determined using Statistics Canada population and income data. To adjust for differences in age and sex composition across income groups – factors that could have an important impact on the frequency of MRI scanning – rates of MRI scanning were adjusted for age and sex using direct standardization to Ontario’s 2001 population. Analyses were performed at the Institute for Clinical Evaluative Sciences, which receives core operating funding from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The Ontario MOHLTC had no role in the study design, analysis or interpretation of data, writing of the report, or decision to submit the report for publication. This study was approved by the Sunnybrook Health Sciences Research Ethics Board.
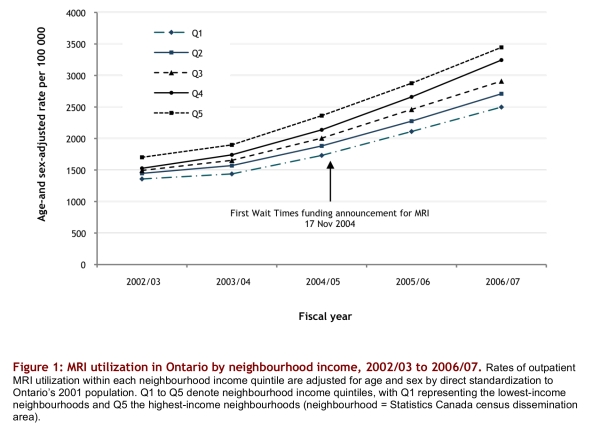
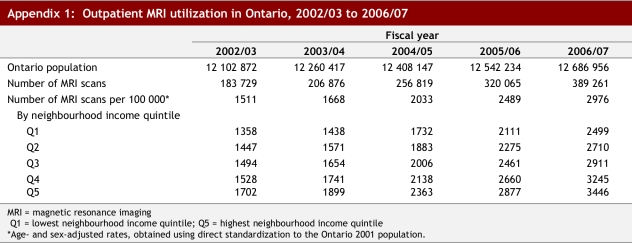
In Ontario, from fiscal years 2002/03 to 2006/07, there were substantial increases in the volume of MRI scans (from 183 729 to 389 261 scans, a 112% increase) and in age- and sex-adjusted population rates of MRI scanning (from 1511 per 100,000 to 2976 per 100,000, a 97% increase). In 2002/03, the rate of scanning among individuals living in neighbourhoods in the wealthiest quintile was 25% greater than among individuals residing in neighbourhoods in the lowest income quintile (age- and sex-adjusted rates of 1702 per 100,000 versus 1358 per 100,000). In the ensuing 5 years, the greatest increases in MRI scanning rates were seen among those living in neighbourhoods in the highest income quintiles (increases of 83%, 87%, 95%, 112%, and 102% for the lowest to highest neighbourhood income quintiles, respectively; see Figure 1 and Appendix 1). Thus, by 2006/07, the relative difference in MRI rates between individuals living in the wealthiest quintile and poorest quintile neighbourhoods had risen to 38%.
Figure 1.
MRI utilization in Ontario by neighbourhood income, 2002/03 to 2006/07
Ontario’s efforts to improve capacity for MRI scanning have been successful: MRI utilization doubled over five years. However, utilization increased disproportionately for those living in the richest neighbourhoods. But does this really mean that individuals with higher incomes have had increasingly better access to MRI over time? There are several potential alternative explanations for our findings. First, we did not have data regarding income at the individual level and used neighbourhood income as a proxy; therefore, some misclassification may have occurred. However, our findings are consistent with the published literature,6-8 and others have found socioeconomic disparities in health services utilization when income is measured at the individual level.9
Could our findings simply reflect a greater need for MRI scans among individuals with higher socioeconomic status? We think this is highly unlikely. Poorer individuals would be expected, on average, to have a greater burden of disease.12,13 Although it could be argued that conditions for which MRI is indicated are more prevalent among individuals living in wealthier neighbourhoods, data from a population-based audit of outpatient MRI scanning in Ontario do not suggest that this is in fact the case.14 Indeed, the argument could be made that conditions such as back and knee pain might be more common among people living in lower income neighbourhoods.15 As well, we observed an increase in the negative correlation between neighbourhood income and access to MRI during the study period, and the prevalence of disease is unlikely to have changed during that time. The proportion of individuals living in rural neighbourhoods is virtually identical across neighbourhood income quintiles (12.5% in the highest and 12.3% in the lowest quintiles (unpublished analyses of Statistics Canada 2001 census data, Institute for Clinical Evaluative Sciences, Toronto, Ont.), and so living in a rural neighbourhood does not explain our findings.
Therefore, it seems unlikely that the disparities we observed can be explained by differences in medical need, and it appears that individuals residing in wealthier neighbourhoods have benefited most, in terms of access, from Ontario’s recent investments in MRI scanning. Whether this translates into better health outcomes is not clear. A study in the United States found that higher rates of diagnostic imaging were associated with less evidence-based care and a trend toward worse outcomes;16,17 however, rates of diagnostic imaging are much higher in the United States than in Ontario.
Why are individuals with higher socioeconomic status more likely to receive MRI scans? It is our impression that many individuals in developed countries appear to equate more testing with better care,18 and that wealthier individuals are more likely to ask their physicians for an MRI scan and are more adept at navigating the health system to gain access to the health services they desire.9,19 Others have found that some physicians have negative perceptions of patients of lower socioeconomic status across several domains,20,21 and that they are more likely to order a diagnostic test for wealthier patients.22 Since we report only on the number of MRI scans actually performed, it is also possible that patients of lower socioeconomic status were ordered MRI scans at a rate similar to wealthier patients, but had a lower proportion of these tests performed because of several barriers, such as difficulties in paying for transportation or in booking time off work. However, it is unlikely that these barriers to accessing MRI services changed during the study period to a degree that would explain the increasing disparities in MRI use that we observed over time.
In conclusion, even in jurisdictions with universal health insurance, decision-makers should be aware that efforts to increase capacity may have the unintended consequence of exacerbating disparities in access according to socioeconomic status. Our findings underscore the need for simultaneous initiatives that aim to target new services according to need and that strive to improve the appropriateness of health services utilization.
Acknowledgments
We thank Dr. Rick Glazier for comments on this manuscript.
Biographies
John J. You, MD, MSc, is an assistant professor of Medicine and of Clinical Epidemiology & Biostatistics at McMaster University, Hamilton, Ontario, Canada, and an adjunct scientist at the Institute for Clinical Evaluative Sciences in Toronto.
Vikram Venkatesh, MD, is a postgraduate trainee in the Department of Radiology at McMaster University.
Andreas Laupacis, MD, MSc, is the Executive Director of the Li Ka Shing Knowledge Institute of St. Michael’s Hospital and a professor of Medicine in the Faculty of Medicine at the University of Toronto, both in Toronto, Ontario, Canada. He is also an adjunct scientist at the Institute for Clinical Evaluative Sciences in Toronto.
Appendix
Appendix 1.
Outpatient MRI utilization in Ontario, 2002/03 to 2006/07
Footnotes
Funding source: John J. You is supported by an Ontario Ministry of Health and Long-Term Care (MOHLTC) Career Scientist Award. The Institute for Clinical Evaluative Sciences receives core operating funds from the Ontario MOHLTC.
Competing interests: None declared.
References
- 1.Chaouilli v. Quebec (Attorney General) 2005.
- 2.Mackie R. Queue-jumping foes fear launch of MRI clinics. Globe and Mail [Toronto] 2002. p. A7.
- 3.First ministers’ meeting on the future of health care: A 10-year plan to strengthen health care. 2004. [accessed 2008 May 29]. www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index_e html.
- 4.Hudson A, Glynn P, Trypuc J. The Wait Time Strategy review of activities, April-August 2005. 2005. [accessed 2008 May 29]. www.health.gov.on.ca/ transformation/wait_times/providers/reports/wt_update_081605.pdf.
- 5.Keller MA. MRI and CT Expert Panel. Phase I Report. 2005. www.health.gov.on.ca/transformation/wait_times/providers/reports/mri_ct.pdf.
- 6.Demeter Sandor, Reed Martin, Lix Lisa, MacWilliam Leonard, Leslie William D. Socioeconomic status and the utilization of diagnostic imaging in an urban setting. CMAJ. 2005;173(10):1173–1177. doi: 10.1503/cmaj.050609. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=16275968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tu JV, Pinfold SP, McColgan P, Laupacis A, editors. Access to Health Services in Ontario: ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 2006. http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=67&morg_id=0&gsec_id=0&item_id=3559&type=atlas. [Google Scholar]
- 8.Alter D A, Naylor C D, Austin P, Tu J V. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341(18):1359–67. doi: 10.1056/NEJM199910283411806. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=10536129&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 9.Alter David A, Iron Karey, Austin Peter C, Naylor C David SESAMI Study Group. Socioeconomic status, service patterns, and perceptions of care among survivors of acute myocardial infarction in Canada. JAMA. 2004;291(9):1100–1107. doi: 10.1001/jama.291.9.1100. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=14996779. [DOI] [PubMed] [Google Scholar]
- 10.Ontario Ministry of Health and Long-Term Care. Ontario Health Insurance Plan (OHIP) Schedule of Benefits and Fees. 2007. [accessed 2008 May 29]. http://www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/d_radiol.pdf.
- 11.Wilkins R. PCCF+ version 4J user’s guide: automated geographic coding based on the Statistics Canada postal code conversion files, including postal codes through September 2006. Ottawa: Statistics Canada; 2007. [Google Scholar]
- 12.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1960;329(2):103–109. doi: 10.1056/NEJM199307083290207. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8510686&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 13.Marmot M G, Smith G D, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-K. http://linkinghub.elsevier.com/retrieve/pii/014067369193068K. [DOI] [PubMed] [Google Scholar]
- 14.You JJ, Purdy I, Rothwell DM, Przybysz R, Fang J, Laupacis A. Indications for and results of outpatient computed tomography and magnetic resonance imaging in Ontario: a population-based study. Can Assoc Radiol J. 2007;59(3):135–143. [PubMed] [Google Scholar]
- 15.Schreuder K J, Roelen C A M, Koopmans P C, Groothoff J W. Job demands and health complaints in white and blue collar workers. Work. 2008;31(4):425–432. [PubMed] [Google Scholar]
- 16.Fisher Elliott S, Wennberg David E, Stukel Thérèse A, Gottlieb Daniel J, Lucas F L, Pinder Etoile L. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. http://www.annals.org/cgi/pmidlookup?view=long&pmid=12585825. [DOI] [PubMed] [Google Scholar]
- 17.Fisher Elliott S, Wennberg David E, Stukel Thérèse A, Gottlieb Daniel J, Lucas F L, Pinder Etoile L. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. http://www.annals.org/cgi/pmidlookup?view=long&pmid=12585826. [DOI] [PubMed] [Google Scholar]
- 18.Leff Bruce, Finucane Thomas E. Gizmo idolatry. JAMA. 2008;299(15):1830–1832. doi: 10.1001/jama.299.15.1830. http://jama.ama-assn.org/cgi/doi/10.1001/jama.299.15.1830. [DOI] [PubMed] [Google Scholar]
- 19.McIsaac W, Goel V, Naylor D. Socio-economic status and visits to physicians by adults in Ontario, Canada. J Health Serv Res Policy. 1997;2(2):94–102. doi: 10.1177/135581969700200207. [DOI] [PubMed] [Google Scholar]
- 20.Woo James K H, Ghorayeb Sahar H, Lee Cheong K, Sangha Harpreet, Richter Suzanne. Effect of patient socioeconomic status on perceptions of first- and second-year medical students. CMAJ. 2004;170(13):1915–1919. doi: 10.1503/cmaj.1031474. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=15210639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O Reilly D, Steele K, Patterson C, Milsom P, Harte P. Might how you look influence how well you are looked after? A study which demonstrates that GPs perceive socio-economic gradients in attractiveness. J Health Serv Res Policy. 2006;11(4):231–234. doi: 10.1258/135581906778476634. [DOI] [PubMed] [Google Scholar]
- 22.Scott A, Shiell A, King M. Is general practitioner decision making associated with patient socio-economic status. Soc Sci Med. 1996;42(1):35–46. doi: 10.1016/0277-9536(95)00063-1. [DOI] [PubMed] [Google Scholar]